Abstract
Objective
Coronary artery wall magnetic resonance imaging (MRI) has been developed to assess coronary lumen diameter and wall thickness. The purpose of this study was to evaluate the physiological parameters that affect the measures of coronary wall thickness using black-blood MRI pulse sequences.
Methods
Eighty-seven participants (38 men and 49 women) of the Multi-Ethnic Study of Atherosclerosis were enrolled in the coronary artery wall MRI study. Cine 4-chamber imaging was used to determine the coronary artery rest period. Free-breathing whole-heart magnetic resonance angiography with motion adaptor navigator was performed to localize the coronary arteries in 64 participants. Cross-sectional free-breathing black-blood images were acquired using electrocardiogram-gated, turbo spin echo sequence. Imaging parameters were as follows: repetition time = 2 R-R intervals, time to echo = 33 milliseconds, echo train length = 13, bandwidth = 305 Hz/pixel, matrix = 416 × 416, field of view = 420 × 420 mm, and slice thickness = 4 to 5 mm.
Results
Imaging was completed in 215 (92%) of 234 coronary segments; 9 participants had incomplete scans. Mean age was 62.6 ± 8.4 years (range, 45–81 years). Mean body mass index was 29.2 ± 5.9 kg/m2. A higher proportion of images with quality of “good” was seen in the right coronary artery (40.5%) compared to the left main and left anterior descending coronary arteries (31.9% and 26.4%, respectively). There was a very good agreement between observers in the image quality scores (κ = 0.79, P < 0.001). Lower heart rate, male sex, and longer coronary rest period were associated with higher image quality score (P < 0.05). Signal-to-noise ratio was higher in participants with Agatston calcium score of more than 10 in the right coronary and left main arteries (48.5 vs 69.7, P = 0.001; and 53.4 vs 61.6, P = 0.032, respectively).
Conclusion
Improved depiction of the coronary artery wall with MRI is related to coronary rest period and atherosclerotic plaque burden as measured by calcium score and inversely related to heart rate. Because longer coronary artery rest periods are associated with improved image quality both for angiography with MRI and coronary artery wall imaging, heart rate–lowering methods in association with these techniques appear to be a logical application.
Keywords: coronary, magnetic resonance imaging, image quality, MRI, cardiac
Cardiovascular disease is the leading cause of death in the United States, and more than half of cardiovascular disease–related deaths are due to coronary artery disease.1 Coronary black-blood magnetic resonance imaging (MRI) is a method to noninvasively assess the thickness of the coronary arterial wall to assess the extent of atherosclerotic disease. The technique has been validated in ex vivo studies,2 and recent improvements in MRI pulse sequences3,4 have allowed the method to be used in patient investigations.5
Due to motion of the coronary arteries along with small size of the arteries, the coronary artery wall (<1-mm diameter) is at the threshold limit of identification with MRI. Coronary artery wall thickness appears to be overestimated by MRI because of a combination of factors including coronary artery motion and large pixel size.6 It is also likely that factors related to the patient's physiological status (eg, body size, heart rate, breathing pattern, coronary calcifications) may impact on the ability of MRI to obtain high-quality studies of the coronary wall. The purpose of this study was to systematically evaluate patient and MRI acquisition parameters that may impact on the image quality of coronary artery wall MRI and to determine which factors require further study to improve this promising technology.
Materials and Methods
Study Design and Subject Selection
The study was approved by our institutional review board, and informed consent was obtained from all participants. The study was conducted in the context of the Multi-Ethnic Study of Atherosclerosis (MESA).7 For the purposes of this study, 87 randomly selected participants of the Chicago and Baltimore MESA cohorts were invited to participate in the coronary artery wall MRI study. Participants with absence of sinus cardiac rhythm, a heart rate of more than 85 beats per minute, claustrophobia, and contraindications to MRI, such as the presence of ferromagnetic implants, were excluded from the study.
Coronary MRI Scan
The first 11 participants were evaluated using a 1.5-T whole-body MRI system (Signa CVi; General Electric Medical Systems, Waukesha, Wis) with 40 mT/m gradients and slew rate of 150 T/m per second using a 4-element phased-array coil for signal reception. Subsequently, 76 participants were imaged on a 1.5-T whole-body clinical scanner (Avanto; Siemens Medical Solutions, Erlangen, Germany) operating at a maximum gradient strength of 45 mT/m and slew rate of 200 T/m per second using 6 anterior channels and 6 posterior channels for data acquisition. Three plane scout images were acquired to verify coil positioning and to localize the heart. To monitor motion of the coronary arteries, an electrocardiogram (ECG)-gated, 2-dimensional, single-slice, cardiac 4-chamber view cine steady-state free precession sequence was performed with temporal resolution of 50 milliseconds or less, retrospectively reconstructed at overlapping 20- to 35-millisecond intervals over the cardiac cycle. These images were used to select the optimum delay time corresponding to the coronary artery rest period in systole or diastole, which was determined based on the visual inspection of the right coronary artery (RCA) movement. The RCA rest period is generally shorter and starts later than that of the left coronary artery8; thus the same rest period parameters were able to be applied for all subsequent imaging of either the left or right coronary arteries.
To localize the coronary arteries, a coronary magnetic resonance angiography (MRA) was acquired using either breath-hold technique (n = 23) or free-breathing whole-heart technique (n = 64). Free breathing was performed using a navigator echo technique that measures respiratory-related displacement of the heart, allowing image acquisition only during a small predefined fraction of the respiratory and cardiac cycle to reduce motion.9–11 On the General Electric scanner, a double oblique breath-hold coronary MRA was obtained using a T2-prepared fat-suppressed 3-dimensional steady-state free precession acquisition with the following parameters: repetition time (TR)/time to echo (TE) = 4.7/1.9 milliseconds, flip angle = 65 degrees, readout bandwidth = 970 Hz/pixel, field of view = 280 × 224 mm, matrix = 256 × 192, number of averages = 0.5, slice thickness = 2 mm with interpolation to 1 mm, and number of partitions = 12. On the Siemens scanner, axial whole-heart coronary MRA parameters were as follows: TR/TE = 3.7/1.7 mm, flip angle = 90 degrees, readout bandwidth = 870 Hz/pixel, parallel imaging factor = 2, field of view = 320 mm2, matrix = 288 × 288, number of averages = 1, slice thickness = 3.0 mm with sine interpolation to 1.5 mm, and number of partitions = 40.
Once the coronary arteries were localized, cross-sectional black-blood images of the proximal portions of the coronary arteries were acquired using a breath-hold, ECG-gated, turbo spin echo (TSE) sequence with double inversion pulse preparation to null the blood. Features of the black-blood TSE pulse sequence are explained in detail elsewhere.12,13 A spectrally selective fat-suppression pulse was also used to increase the contrast between the vessel wall and epicardial fat. For the General Electric scanner, imaging parameters were as follows: TR = 2 R-R, TE = 5.1 milliseconds, echo train length = 16, bandwidth = 244 Hz/pixel, matrix = 256 × 192, field of view = 280 × 224 mm, and slice thickness = 4 mm. For the Siemens scanner, the cross-sectional black-blood images were acquired using free-breathing, ECG-gated, TSE sequence imaging with the following parameters: TR = 2 R-R intervals, TE = 33 milliseconds, echo train length = 13, bandwidth = 305 Hz/pixel, matrix = 416 × 416, field of view = 420 × 420 mm, and slice thickness = 5 mm. The free-breathing images acquired were performed using a motion-adapted navigator technique with end-expiratory imaging defined by the dome of the right hemidiaphragm. The motion-adapted navigator technique was performed using a prospective slice following algorithm with a correction factor of 0.6 in the inferior-superior direction. The center position of the navigator acceptance window was adapted to diaphragm drift by immediately changing to higher diaphragm positions (upward drift) and changing to lower diaphragm positions only if the maximum diaphragm position over the last 20 heartbeats was below the acceptance window (downward drift). In all cases, the duration of the echo train length of the TSE sequence was individually optimized not to exceed the coronary rest period duration and to begin after the onset of the coronary rest period based on the 4-chamber cine images.
For black-blood imaging of the coronary arteries, we acquired 3 slices at 5-mm intervals in RCA, 1 slice in the left main (LM) coronary artery, and 3 slices in the left anterior descending (LAD) artery. The best image in each coronary territory was considered for further analysis (Fig. 1). Each cross-sectional image was individually prescribed based on double oblique multiplanar reformations to be orthogonal to the local longitudinal axis of the coronary wall.
FIGURE 1.
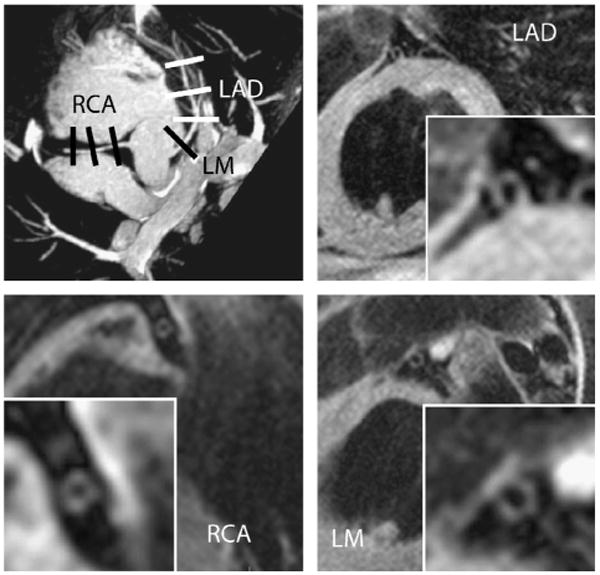
Cross-sectional slice positioning for each coronary artery based on the coronary artery MRI (top left) and corresponding cross-sectional images of the coronary artery wall.
Coronary MRI Analysis
Coronary wall images were analyzed using VesselMASS software (Leiden University Medical Center). Image quality of the coronary arteries was visually assessed by 2 observers (A.A.M. and R.M.) and scored based on a scale of 1 to 5, in which 1 was the poorest image quality (not interpretable) and 5 was the best image quality (Fig. 2). The images were zoomed to 500%, and a region of interest (ROI) tool was used to measure the signal intensity (SI). The signal-to-noise ratio (SNR) was calculated based on the following formula: SNR = SIvessel wall / SDnoise, where SI of the vessel wall was determined by placing the ROI on the vessel wall, and the standard deviation (SD) of the background noise was determined from an ROI placed in the air anterior to the chest wall.
FIGURE 2.
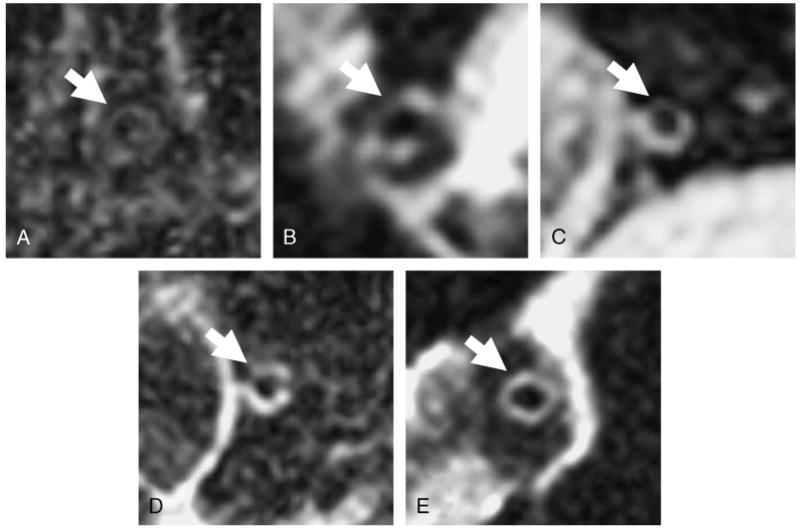
Arteries were visually scored based on the ability of the observer to distinguish all or part of the coronary artery wall from surrounding tissue. A, A score of 1 indicated the observer was unable to distinguish the artery. B, If parts of the artery were visible (<50%) but with hazy borders, it was scored as 2. C, If at least 50% of the wall was identified and the borders were sharp, it was scored as 3. D, If only small portions of the vessel (25%) were not present with well-defined borders, it was scored as 4. E, If the entire coronary wall was visible and well defined, it was scored as 5.
Contrast-to-noise ratio (CNR) was calculated based on the following formula: CNR = SIvessel wall – SIperivascular area / SDnoise. For the purpose of determining the SI of the perivascular area, the ROI was placed in the region between the vessel wall and the myocardium.
Scan Efficiency
The mean of the percentage acceptance rate for the navigator during the axial whole-heart MRA was determined as the scan efficiency.
Calcium Score Measurements
Computed tomography scanning of the chest was performed with a prospectively ECG-triggered scan acquisition at 50% of the R-R interval with a multidetector computed tomography system (Volume Zoom; Siemens) with 2.5-mm slices in a sequential scan mode. The phantom adjusted average Agatston score was used in all analyses.14
Statistical Analysis
Statistical analysis was performed with SPSS (version 14.0 for Windows; SPSS, Chicago, Ill). For the purpose of the statistical analysis, the averages of the scores of the 2 observers were further categorized to poor (1–3), fair (3.5–4), and good (4.5–5) categories. Continuous data are expressed as mean values with SDs. Unpaired t tests and analysis of variance were performed to evaluate the difference between groups. Categorical data were analyzed by Mann-Whitney non-parametric test. Due to the clustered nature of the data, we performed the statistical analysis separately for each coronary artery. We performed the κ statistic to measure the interobserver agreement.
Results
Study Population
Of 87 participants selected for participation, 49 participants were female (Table 1). The mean age was 62.6 ± 8.4 years (range, 45–81 years). Mean body mass index (BMI) of our population was 29.2 kg/m2 (SD, 5.9 kg/m2). Imaging the coronary arteries was not possible in 9 (10.3%) of the participants, mainly because of inappropriate electrocardiographic gating and irregular respiratory movements. Imaging was completed in 215 (92%) of the 234 remaining coronary segments.
TABLE 1. General Characteristic of the Study Population.
| Demographic Data | n (%) |
|---|---|
| Sex | |
| Men | 38 (43.7) |
| Women | 49 (56.3) |
| Total | 87 (100) |
| Ethnicity | |
| Non-Hispanic White | 44 (50.6) |
| African American | 43 (49.4) |
| Age, yrs | 62.6 ± 8.4 |
| BMI, kg/m2 | 29.2 ± 5.9 |
| Agatston calcium score | |
| ≥10 | 30 (34.5) |
| <10 | 57 (65.5) |
Data are presented as number and mean ± SD. Percentages are in parentheses.
Image Quality Assessment
One hundred twenty-two coronary segments (57%) had subjective ratings of good or fair image quality, whereas 93 (43%) were considered poor. Overall, a higher proportion of images with quality of “good” was seen in the RCA (40.5%) compared to the LM and LAD arteries (31.9% and 26.4%, respectively). Images with poor quality were equally distributed among the 3 coronary artery territories. There was a good agreement between observers in the image quality scores (κ = 0.79, P < 0.001).
The mean SNR and CNR values were 54.9 ± 15.6 and 25.3 ± 11.9, respectively, for all arteries. Higher SNR was associated with higher image quality scores in the RCA and LM artery (Fig. 2A). A similar trend was noted for CNR measurements (Fig. 2B), and this was significant for the RCA.
MRI Scanning Parameters
Eleven of the scans were performed on GE scanners, and the rest of the scans were performed on Siemens scanners. Image quality scores, SNR, and CNR were not significantly different for the images acquired in different scanners, but the power to detect differences between the 2 scanners was low. Scan efficiency was measured in 73 participants who had a whole-heart MRA technique. Mean scan efficiency was 33.9% (SD, 9.1%). There was no relationship between scan efficiency and coronary wall image quality (P = 0.86). Mean total scan time was 46.34 minutes (SD, 16.4 minutes).
Subject Parameters
Image quality score was significantly lower for female participants (P = 0.007). Signal-to-noise ratio and CNR were significantly higher in male participants (57.67 vs 52.0, P = 0.02; and 27.78 vs 22.74, P = 0.007, respectively); also, the calcium score was significantly lower in female participants (log transformed: 1.3 vs 1.9, P = 0.024).
Age was not significantly different for participants in different image quality categories (P = 0.27). There was a trend between increasing BMI and decreasing quality score, but these differences were not statistically significant.
Heart rate was significantly lower in male population (69.8 vs 63.7 beats per minute, P < 0.001), and rest period was significantly higher in male population (183.8 vs 250.4 milliseconds, P < 0.001). Lower heart rate was associated with improved quality score in the RCA (P = 0.001) (Fig. 3). Higher image quality was significantly associated with a longer coronary rest period for all 3 coronary arteries (Fig. 4).
FIGURE 3.
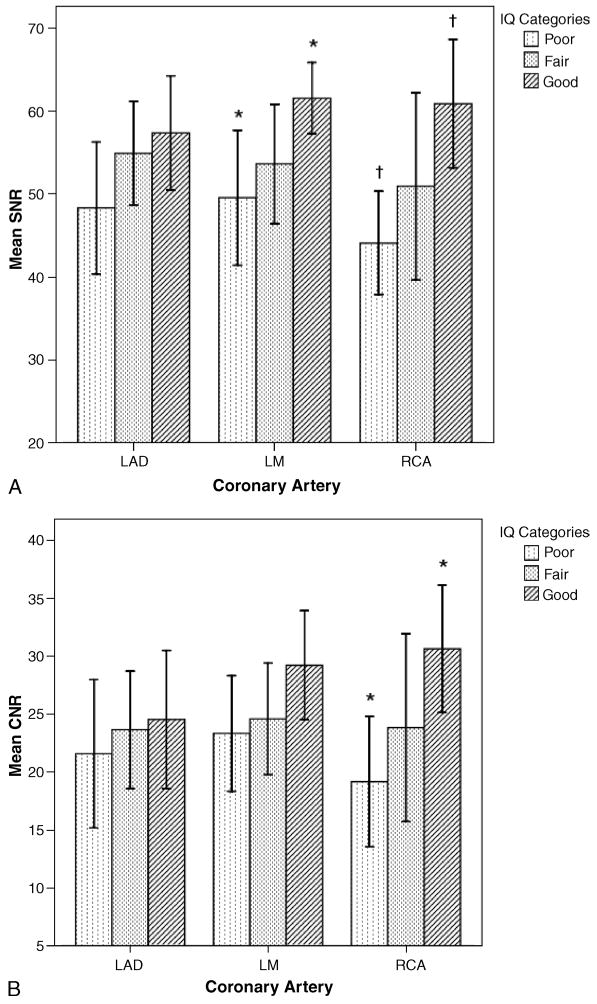
A, Mean SNR values for each coronary artery as a function of the subjective image quality categories (*P = 0.022, †P = 0.013). IQ indicates image quality. T bars represent 95% confidence intervals. B, Mean CNR values for each coronary artery as a function of the subjective image quality categories. The CNR difference between poor and good image quality of the RCA was statistically significant (*P = 0.022). T bars represent 95% confidence interval.
FIGURE 4.
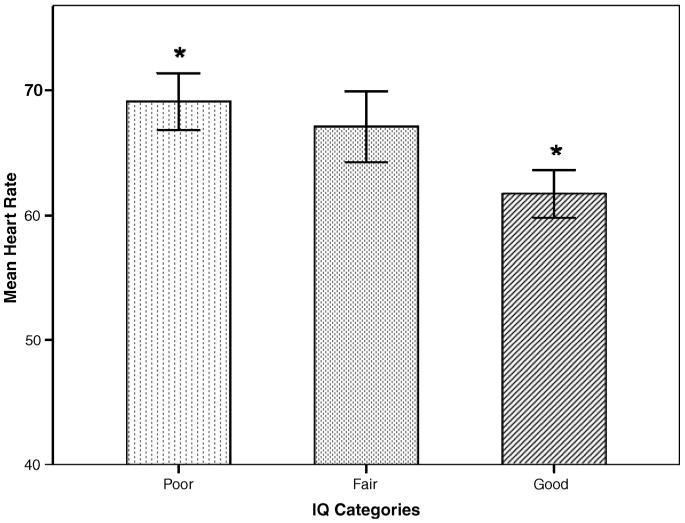
The relationship between heart rate and image quality category for RCA. Asterisk (*) indicates P = 0.001. T bars represent 95% confidence interval.
Calcium score was measured for all participants in the study. The mean Agatston calcium score in our participants was 51.9 units. Signal-to-noise ratio in all coronary arteries was higher in participants with Agatston calcium score of more than 10 (Fig. 5), and this differences were significant in the RCA and LM artery (48.5 vs 69.7, P = 0.001; and 53.4 vs 61.6, P = 0.032, respectively) (Fig. 6).
FIGURE 5.
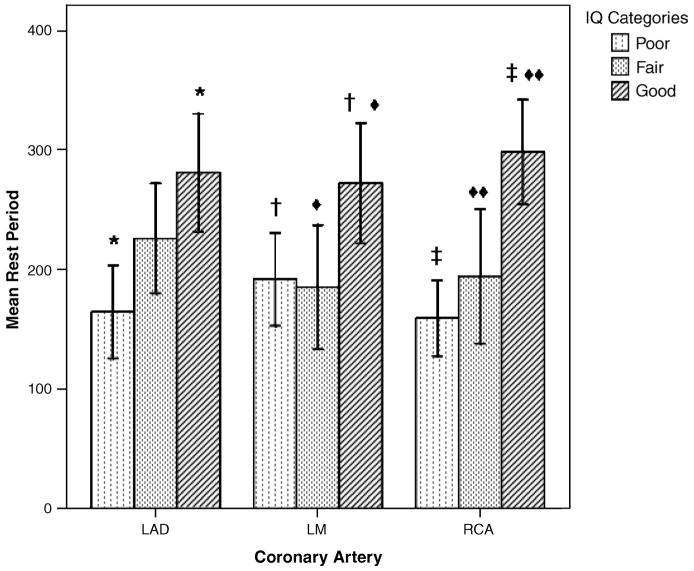
The relationship between coronary artery rest period image quality category for each coronary artery. Image quality increases significantly with increased rest period in all coronary arteries (*P = 0.001, †P = 0.026, ◆P = 0.033, ‡P < 0.001, ◆◆P = 0.017). T bars represent 95% confidence interval.
FIGURE 6.
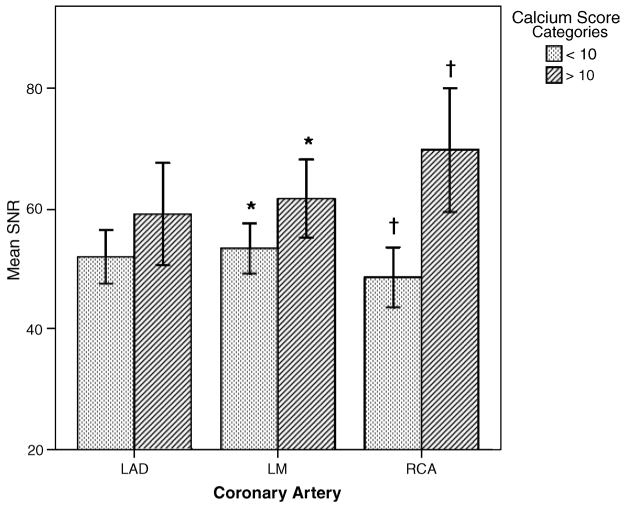
The relationship between SNR and image quality category for each coronary artery stratified by Agatston calcium score. Differences were significant for the LM and RCA (*P = 0.032, †P = 0.001). T bars represent 95% confidence interval.
Discussion
Cross-sectional imaging of the coronary arteries is challenging because of their complex anatomical geometry, small size, and 3-dimensional rapid movement. The effects of heart rate, heart rate variability, and diaphragm movement have been reported previously for CT and magnetic resonance coronary angiography.8,15 However, the subject-specific parameters that impact coronary artery vessel wall imaging with MRI have not previously been reported. In 78 participants who completed the coronary artery wall MRI, improved image quality was significantly associated with lower heart rate and longer coronary artery rest period. These parameters were significant despite MRI scan adjustment for each participant to individually establish the beginning and duration of the coronary rest period and ensure that these values corresponded to timing of the k-space acquisition. Although we detected a decreasing trend in BMI along image quality categories, this trend was not significant. Right coronary artery and LM coronary artery image quality was the highest, and image quality was better in men than women. Image quality generally improved with increasing levels of coronary atherosclerosis as assessed by CT calcium score.
One of the main challenges in imaging the heart structures is freezing the heart movement or imaging the heart at the period of least movement or “rest period.” Besides subject-specific trigger delays and k-space acquisition durations, navigator echoes or breath-holding was used to reduce bulk motion artifacts. The efficiency of the free-breathing MRI scan was determined by the acceptance rate of the navigator during the axial whole-heart MRA. We did not detect any relationship between image quality category and navigator efficiency. This finding suggests that diaphragmatic movement was effectively correlated with heart displacement in the superior-inferior direction.
Previous CT and MRI angiography studies have noted the importance of coronary rest period in relationship to angiogram quality.8,15,16 This study shows that similar relationships hold for cross-sectional imaging of the arterial wall. The coronary artery rest period in the RCA is shorter than the LAD,8,17 and the RCA has a faster and more complex 3-dimensional movement pattern than LAD and LM arteries.17,18 In this study, the onset and duration of the rest period of the RCA were used to image all the coronary arteries. Visual inspection of the cine images did not detect differences between the right and left coronary rest periods, but quantitative analysis could potentially improve this optimization for each artery segment.8,17
Calcium score is considered as a measure of atherosclerosis burden and is highly correlated (r = 0.9) to the atherosclerotic plaque extent.14 Calcium score was significantly related to subjective measure of image quality (SNR) in our study. This is likely related to higher thickness of the coronary artery wall with increasing coronary calcium score. The observers perceived this as improved image quality, because the coronary wall was better seen. This relationship has not been shown before in MRI studies and holds out the future potential for characterization of coronary plaque. Interestingly, image quality was higher in men than women; this may be explained at least in part by higher calcium score in men and thus higher atherosclerotic burden.
Clinical Application
Because longer coronary artery rest periods are associated with improved image quality both for angiography with MRI8,15–18 and coronary artery wall imaging, heart rate–lowering methods in association with these techniques appear to be a logical application.8 Other than pharmacological intervention to increase the rest period and reduce the heart rate, recent advances have been made to detect the cardiac rest period more accurately by myocardial motion–tracking methods in coronary MRA19 and black-blood imaging.20
Limitations
There are several limitations of this study. Although we had a good sample size compared to previous studies, a larger sample size would indicate if certain trends, such as the relationship to BMI and image quality, should be further studied. Voxels were anisotropic, and a slice thickness of 4 to 5 mm was necessary to provide sufficient SNR. Three-dimensional MRI technique can provide near-isotropic spatial resolution21 at the expense of longer acquisition time to sample the right and left coronary arteries. However, the faster 2-dimensional technique that we used allowed cross-sectional images to be easily repeated if necessary. In addition, vessel cross-sections rather than long-axis image acquisition and analysis have previously been shown to be advantageous for atherosclerosis assessment.22 The coronary rest period determination was based on RCA motion only; this simplified image acquisition for the technologist but more optimal rest period assessment could be performed in future studies for each individual coronary artery territory. Finally, we did not specifically obtain images in areas of luminal narrowing/stenosis. Therefore, our finding that there is a correlation between calcium score and higher image quality is more likely due to a generalized diffuse process of atherosclerosis, rather than providing information regarding plaque assessment in areas of luminal narrowing. Signal-to-noise ratio and CNR estimates are less reliable for normal coronary arteries because of their small size, but are likely to be more reliable as the extent of atherosclerosis and wall thickness increase.
Acknowledgments
The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions.
This research was supported by R01 HL78909 and contracts N01-HC-95159 through N01-HC-95169 from the National Heart, Lung, and Blood Institute. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org.
References
- 1.Rosamond W, Flegal K, Friday G, et al. Heart disease and stroke statistics—2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115:e69–e171. doi: 10.1161/CIRCULATIONAHA.106.179918. [DOI] [PubMed] [Google Scholar]
- 2.Larose E, Yeghiazarians Y, Libby P, et al. Characterization of human atherosclerotic plaques by intravascular magnetic resonance imaging. Circulation. 2005;112:2324–2331. doi: 10.1161/CIRCULATIONAHA.105.538942. [DOI] [PubMed] [Google Scholar]
- 3.Katoh M, Spuentrup E, Buecker A, et al. MRI of coronary vessel walls using radial k-space sampling and steady-state free precession imaging. AJR Am J Roentgenol. 2006;186:S401–S406. doi: 10.2214/AJR.04.1864. [DOI] [PubMed] [Google Scholar]
- 4.Botnar RM, Stuber M, Kissinger KV, et al. Free-breathing 3D coronary MRA: the impact of “isotropic” image resolution. J Magn Reson Imaging. 2000;11:389–393. doi: 10.1002/(sici)1522-2586(200004)11:4<389::aid-jmri6>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 5.Kim WY, Astrup AS, Stuber M, et al. Subclinical coronary and aortic atherosclerosis detected by magnetic resonance imaging in type 1 diabetes with and without diabetic nephropathy. Circulation. 2007;115:228–235. doi: 10.1161/CIRCULATIONAHA.106.633339. [DOI] [PubMed] [Google Scholar]
- 6.Schar M, Kim WY, Stuber M, et al. The impact of spatial resolution and respiratory motion on MR imaging of atherosclerotic plaque. J Magn Reson Imaging. 2003;17:538–544. doi: 10.1002/jmri.10287. [DOI] [PubMed] [Google Scholar]
- 7.Bild DE, Bluemke DA, Burke GL, et al. Multi-Ethnic Study of Atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 8.Jahnke C, Paetsch I, Achenbach S, et al. Coronary MR imaging: breath-hold capability and patterns, coronary artery rest periods, and beta-blocker use. Radiology. 2006;239:71–78. doi: 10.1148/radiol.2383042019. [DOI] [PubMed] [Google Scholar]
- 9.Stuber M, Botnar RM, Danias PG, et al. Submillimeter three-dimensional coronary MR angiography with real-time navigator correction: comparison of navigator locations. Radiology. 1999;212:579–587. doi: 10.1148/radiology.212.2.r99au50579. [DOI] [PubMed] [Google Scholar]
- 10.Sommer T, Hofer U, Hackenbroch M, et al. Submillimeter 3D coronary MR angiography with real-time navigator correction in 107 patients with suspected coronary artery disease [in German] Rofo. 2002;174:459–466. doi: 10.1055/s-2002-25121. [DOI] [PubMed] [Google Scholar]
- 11.Plein S, Jones TR, Ridgway JP, et al. Three-dimensional coronary MR angiography performed with subject-specific cardiac acquisition windows and motion-adapted respiratory gating. AJR Am J Roentgenol. 2003;180:505–512. doi: 10.2214/ajr.180.2.1800505. [DOI] [PubMed] [Google Scholar]
- 12.Simonetti OP, Finn JP, White RD, et al. “Black blood” T2-weighted inversion-recovery MR imaging of the heart. Radiology. 1996;199:49–57. doi: 10.1148/radiology.199.1.8633172. [DOI] [PubMed] [Google Scholar]
- 13.Fayad ZA, Fuster V, Fallon JT, et al. Noninvasive in vivo human coronary artery lumen and wall imaging using black-blood magnetic resonance imaging. Circulation. 2000;102:506–510. doi: 10.1161/01.cir.102.5.506. [DOI] [PubMed] [Google Scholar]
- 14.Carr JJ, Nelson JC, Wong ND, et al. Calcified coronary artery plaque measurement with cardiac CT in population-based studies: standardized protocol of Multi-Ethnic Study of Atherosclerosis (MESA) and Coronary Artery Risk Development in Young Adults (CARDIA) study. Radiology. 2005;234:35–43. doi: 10.1148/radiol.2341040439. [DOI] [PubMed] [Google Scholar]
- 15.Hoffmann MH, Shi H, Manzke R, et al. Noninvasive coronary angiography with 16-detector row CT: effect of heart rate. Radiology. 2005;234:86–97. doi: 10.1148/radiol.2341031408. [DOI] [PubMed] [Google Scholar]
- 16.Leschka S, Wildermuth S, Boehm T, et al. Noninvasive coronary angiography with 64-section CT: effect of average heart rate and heart rate variability on image quality. Radiology. 2006;241:378–385. doi: 10.1148/radiol.2412051384. [DOI] [PubMed] [Google Scholar]
- 17.Wang Y, Vidan E, Bergman GW. Cardiac motion of coronary arteries: variability in the rest period and implications for coronary MR angiography. Radiology. 1999;213:751–758. doi: 10.1148/radiology.213.3.r99dc41751. [DOI] [PubMed] [Google Scholar]
- 18.Kim WY, Stuber M, Kissinger KV, et al. Impact of bulk cardiac motion on right coronary MR angiography and vessel wall imaging. J Magn Reson Imaging. 2001;14:383–390. doi: 10.1002/jmri.1198. [DOI] [PubMed] [Google Scholar]
- 19.Ustun A, Desai M, Abd-Elmoniem KZ, et al. Automated identification of minimal myocardial motion for improved image quality on MR angiography at 3 T. AJR Am J Roentgenol. 2007;188:W283–W290. doi: 10.2214/AJR.06.0334. [DOI] [PubMed] [Google Scholar]
- 20.Keegan J, Gatehouse PD, Prasad SK, et al. Improved turbo spin-echo imaging of the heart with motion-tracking. J Magn Reson Imaging. 2006;24:563–570. doi: 10.1002/jmri.20655. [DOI] [PubMed] [Google Scholar]
- 21.Kim WY, Stuber M, Bornert P, et al. Three-dimensional black-blood cardiac magnetic resonance coronary vessel wall imaging detects positive arterial remodeling in patients with nonsignificant coronary artery disease. Circulation. 2002;106:296–299. doi: 10.1161/01.cir.0000025629.85631.1e. [DOI] [PubMed] [Google Scholar]
- 22.Kuszyk BS, Heath DG, Johnson PT, et al. CT angiography with volume rendering for quantifying vascular stenoses: in vitro validation of accuracy. AJR Am J Roentgenol. 1999;173:449–455. doi: 10.2214/ajr.173.2.10430152. [DOI] [PubMed] [Google Scholar]


