Abstract
OBJECTIVES
The purpose of this study was to evaluate the relationship of left ventricular (LV) remodeling assessed by cardiac magnetic resonance to various measures of obesity in a large population-based study.
BACKGROUND
Obesity is a well-known risk factor for cardiovascular disease, yet its relationship with LV size and function is poorly understood.
METHODS
A total of 5,098 participants (age 45 to 84 years; 48% men) in the Multi-Ethnic Study of Atherosclerosis who were free of clinically apparent cardiovascular disease underwent cardiac magnetic resonance to assess LV size and function as well as measures of obesity, including body mass index, waist-to-hip ratio and waist circumference, and cardiovascular risk factors. Fat mass (FM) was estimated based on height-weight models derived from bioelectrical impedance studies. The associations of obesity measures with LV size and function were evaluated using linear spline regression models for body mass index and multivariable regression models for other measures of obesity; they were displayed graphically using generalized additive models.
RESULTS
LV mass and end-diastolic volume were positively associated with measures of obesity in both sexes after adjustment for risk factors (e.g., 5.7-g and 6.9-g increase in LV mass per 10-kg increase in FM in women and men, respectively [p < 0.001]). LV mass-to-volume ratio was positively associated with increased body mass index, waist-to-hip ratio, waist circumference, and estimated FM (e.g., 0.02-g/ml and 0.06-g/ml increase in mass-to-volume ratio per 10-kg increase in FM in women and men, respectively [p < 0.001]). The increased mass-to-volume ratio was due to a greater increase in LV mass relative to LV end-diastolic volume. All associations were stronger for men than for women. Ejection fraction showed no significant association with measures of obesity.
CONCLUSIONS
Obesity was associated with concentric LV remodeling without change in ejection fraction in a large, multiethnic cohort study.
Keywords: cardiac magnetic resonance, cardiac morphology, epidemiology, left ventricular function, obesity
Obesity is associated with a spectrum of cardiovascular changes thought to be mediated by altered hemodynamics and an inflammatory state that could result in structural heart changes and heart failure (1,2). In men and women residents of Framingham, Massachusetts, obesity was associated with an increase in wall thickness to a greater extent than the increase in chamber size (3). A similar finding was present in an evaluation of 20 healthy, young obese women (4). However, the pattern of obesity-induced remodeling in relationship to different patterns of adipose tissue distribution and ethnicity is unknown.
Previous studies evaluating obesity and left ventricular (LV) remodeling have relied on echocardiography, which becomes increasing suboptimal as levels of obesity increase due to limited acoustic windows. Moreover, geometric assumptions used in echocardiography to compute LV mass and volumes have limitations that are well documented (5). Cine cardiac magnetic resonance (CMR) has been shown to be highly accurate and reproducible for the assessment of ventricular size and function based on 3-dimensional images of the heart (6,7).
The MESA (Multi-Ethnic Study of Atherosclerosis) study is a large population-based study that used CMR to measure LV structure and function. The aim of this study was to evaluate the association of various measures of obesity and differences in body composition with LV structure and function in a multiethnic population free of clinically apparent cardiovascular disease.
METHODS
Study design and population
MESA has been previously described (8). In brief, between July 2000 and August 2002, 6,814 men and women who identified themselves as white, African-American, Hispanic, or Chinese and were 45 to 84 years old and free of clinically apparent cardiovascular disease were recruited from 6 U.S. communities: Baltimore City and Baltimore County, Maryland; Chicago, Illinois; Forsyth County, North Carolina; Los Angeles County, California; Northern Manhattan and the Bronx, New York; and St. Paul, Minnesota. Consenting participants underwent a CMR scan a median of 16 days after the baseline evaluation; 95% were completed by 11 weeks after the baseline examination. The institutional review boards at all participating centers approved the study, and all participants gave informed consent.
Baseline examination
Participants underwent an extensive baseline evaluation including clinical history, physical examination, anthropometric measurements (weight, height, and waist and hip girth), laboratory tests including 12-h fasting blood glucose, total cholesterol, triglycerides, high-density lipoprotein, and calculated low-density lipoprotein cholesterol from Friedewald’s equation (9). Standardized questionnaires were used to obtain information about smoking history, alcohol intake, exercise, current medications, and physician diagnoses of hypertension and diabetes. Systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or use of antihypertensive medications was classified as hypertension. Diabetes was defined as use of hypoglycemic drugs or fasting blood glucose ≥126 mg/dl.
Assessment of obesity
Body weight, height, waist circumference (WC), and hip circumference were measured to the nearest 0.5 kg, 0.1 cm, and 0.1 cm, respectively. Body mass index (BMI), calculated as weight (kg) divided by height squared (m2), was used as a measure of overall adiposity. Obesity and overweight were defined as BMI ≥30 kg/m2 and between 25 and 30 kg/m2, respectively (10,11). WC was measured using a steel measuring tape (standard 4-oz tension) from midway between the last rib and the iliac crest at normal breathing. Hip circumference was measured from the largest diameter of the hip, and waist-to-hip ratio (WHR) was calculated by dividing the WC by the hip circumference. WC and WHR were used as indexes of abdominal (central, visceral) obesity. The lean body mass of participants was estimated based on height-weight models derived from bioelectrical impedance studies by Kuch et al. (12). Lean body mass was defined as 5.1 × [height (m)1.14] × [weight (kg)0.41] for men and 5.34 × [height (m)1.47] × [weight (kg)0.33] for women. Fat mass (FM) was calculated by subtracting the lean body mass from weight.
CMR and image analysis
Of 6,814 total participants, 5,098 agreed to undergo a CMR examination and signed an informed consent. CMR examinations were performed according to a standard protocol as previously described (13). Briefly, LV mass, volumes, and functional parameters were determined from short-axis fast gradient echo cine images covering the heart from base to apex throughout the cardiac cycle with temporal resolution ≤50 ms. For CMR measurements, the technical error of measurement percentage of the mean was 6% and 4% for LV mass and volume, respectively (13).
Statistical analysis
The characteristics of the study groups are presented as mean ± SD for continuous variables and as percentages for categorical variables. BMI, WC, WHR, and FM were used as continuous variables. The unadjusted magnitude and direction of the associations between various measures of body size and obesity as well as measures of LV size and obesity were determined using Pearson correlation coefficients.
The associations of LV mass, LV end-diastolic volume, mass-to-volume (M/V) ratio, and ejection fraction with BMI, WC, WHR, and FM were displayed graphically using generalized additive models for both sexes. All models were adjusted for age, race/ethnicity, systolic and diastolic blood pressures, use of antihypertensive medications, diabetes, total cholesterol, high-density lipoprotein, triglycerides, use of lipid-lowering medication, family history of heart attack, intentional exercise (the sum of walking for exercise, sports/dancing, and conditioning in metabolic equivalent hours/week) in quartiles, cigarette smoking, and heavy alcohol consumption (current/former drinkers with usual consumption >2 drinks/day). Models examining the association of FM with LV measures were also adjusted for lean body mass.
Significant nonlinearity was present in several of the BMI relationships, and hence a set of linear spline regression models, with prespecified knots at BMI of 25 and 30, were used to evaluate the relationships as a piecewise linear function. The line segments were constrained to be continuous between categories. Within each BMI category, we evaluated the slope for the end point within that range and examined whether the slope differed from 0 and differed by sex. Slopes for other measures of obesity were based on multiple linear regression models. We also tested for interaction between sex and race/ethnicity and each body size measure.
Differences in associations of LV indexes with BMI and FM for participants with and without selected traditional cardiovascular risk factors were also examined separately according to the presence of any of the following: 1) diabetes, abnormal glucose levels, or use of antidiabetic medication; 2) hypertension or use of antihypertensive medication; 3) current or former smoking (≥100 cigarette pack-years in the lifetime); and current or former heavy alcohol use.
All analyses were performed using Stata 10.0 for Windows (StataCorp, College Station, Texas). Values of p < 0.05 were considered as statistically significant. Race/ethnicity interactions were accepted as significant if p < 0.01 due to multiple testing.
RESULTS
Participant characteristics
A total of 5,098 MESA participants underwent CMR (75% of all MESA participants) and 5,004 of them (98%) had technically adequate data and were included in the analysis. The mean age of the participants was 61.5 years (range 45 to 84 years): 52% were female, 13% were Chinese-American, 26% were African-American, 22% Hispanic, and 39% were Caucasian.
The risk factor characteristics, body size, and obesity measures of the study group and descriptive results of CMR measures are shown in Table 1. According to BMI categories, 29% of the participants were overweight and 41% were obese. Obese participants were more likely to have hypertension and diabetes and had higher low-density lipoprotein cholesterol and triglyceride levels than normal-weight participants.
Table 1.
Characteristics of MESA Participants With CMR (N = 5,004) by Sex, 2000 to 2002
| Women (n = 2,622), Mean ± SD or n (%) |
Men (n = 2,382), Mean ± SD or n (%) |
p Value | |
|---|---|---|---|
| Risk factors | |||
| Hypertension | 1,147 (43.7) | 973 (40.8) | 0.038 |
| Diabetes | 272 (10.4) | 309 (13.0) | 0.004 |
| Family history of heart attack | 1,143 (43.6) | 853 (35.8) | <0.001 |
| HDL (mg/dl) | 56.8±15.5 | 45.0±11.6 | <0.001 |
| LDL (mg/dl) | 117±31.8 | 117±30.8 | 0.67 |
| Triglycerides (mg/dl) | 129±82.5 | 134±87.9 | 0.019 |
| Ever smoker | 1,044 (39.8) | 1,377 (57.8) | <0.001 |
| Body size measures | |||
| Fat mass (kg) | 28.5±11.8 | 24.5±9.3 | <0.001 |
| Lean body mass (kg) | 43.6±5.0 | 58.3±6.4 | <0.001 |
| Weight (kg) | 72.1±15.7 | 82.9±14.8 | <0.001 |
| BMI category | <0.001 | ||
| Lean (=25) | 853 (32.5) | 693 (29.1) | |
| Overweight (25–30) | 836 (31.9) | 588 (24.7) | |
| Obese (>30) | 933 (35.6) | 1,101 (46.2) | |
| BMI (kg/m2) | 28.0±5.6 | 27.4±4.1 | <0.001 |
| Waist circumference (cm) | 95.2±14.7 | 98±11.3 | <0.001 |
| Hip circumference (cm) | 106±11.7 | 103±8.5 | <0.001 |
| Waist-to-hip ratio | 0.90±0.08 | 0.96±0.07 | <0.001 |
| LV size and function measures | |||
| LV mass (g) | 124±27.4 | 169±37.2 | <0.001 |
| LV end-diastolic volume (ml) | 114±24.4 | 140±32.7 | <0.001 |
| LV end-systolic volume (ml) | 33.1±12.0 | 47.6±18.6 | <0.001 |
| LV ejection fraction (%) | 71.3±6.6 | 66.6±7.5 | <0.001 |
| Stroke volume (ml) | 80.7±17.0 | 92.6±20.8 | <0.001 |
| Cardiac output (l/min) | 5.4±1.4 | 6.0±1.5 | <0.001 |
BMI = body mass index; CMR = cardiac magnetic resonance; HDL = high-density lipoprotein; LDL = low-density lipoprotein; LV = left ventricular; MESA = Multi-Ethnic Study of Atherosclerosis.
Correlation among measures of obesity and between measures of obesity and LV size
Measures of body size and obesity were highly correlated with each other in both women and men (Table 2). Among these measures, WHR had much weaker correlations with other measures of obesity for both sexes.
Table 2.
Correlation Coefficients Between Measures of Body Size and Obesity by Sex in MESA Participants With CMR (N = 5,004)
| Women |
Men |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Weight | BMI | FM | WC | WHR | Weight | BMI | FM | WC | WHR | |
| Weight | 1.00 | 1.00 | ||||||||
| BMI | 0.92 | 1.00 | 0.88 | 1.00 | ||||||
| FM | 0.97 | 0.98 | 1.00 | 0.97 | 0.97 | 1.00 | ||||
| WC | 0.83 | 0.86 | 0.86 | 1.00 | 0.88 | 0.89 | 0.91 | 1.00 | ||
| WHR | 0.27 | 0.36 | 0.32 | 0.69 | 1.00 | 0.40 | 0.48 | 0.45 | 0.67 | 1.00 |
All the correlation coefficients are significantly different from 0 (p < 0.001).
FM = fat mass; WC = waist circumference; WHR = waist-to-hip ratio; other abbreviations as in Table 1.
All measures of obesity, except WHR, were also significantly correlated with measures of LV size and function (Table 3); WHR was weakly correlated with LV mass and cardiac output for both sexes.
Table 3.
Correlation Coefficients Between Measures of Obesity and LV Size by Sex in MESA Participants With CMR (N = 5,004)
| Women |
Men |
|||||||
|---|---|---|---|---|---|---|---|---|
| LV Mass | LV EDV | SV | CO | LV Mass | LV EDV | SV | CO | |
| Weight | 0.60 | 0.54 | 0.50 | 0.43 | 0.51 | 0.38 | 0.33 | 0.30 |
| BMI | 0.52 | 0.41 | 0.39 | 0.36 | 0.42 | 0.22 | 0.20 | 0.22 |
| FM | 0.56 | 0.48 | 0.45 | 0.40 | 0.47 | 0.30 | 0.27 | 0.27 |
| WC | 0.48 | 0.31 | 0.30 | 0.29 | 0.39 | 0.22 | 0.19 | 0.22 |
| WHR | 0.19 | −0.03 | −0.004 | 0.05 | 0.15 | 0.01 | −0.01 | 0.06 |
Association of LV size and function with BMI
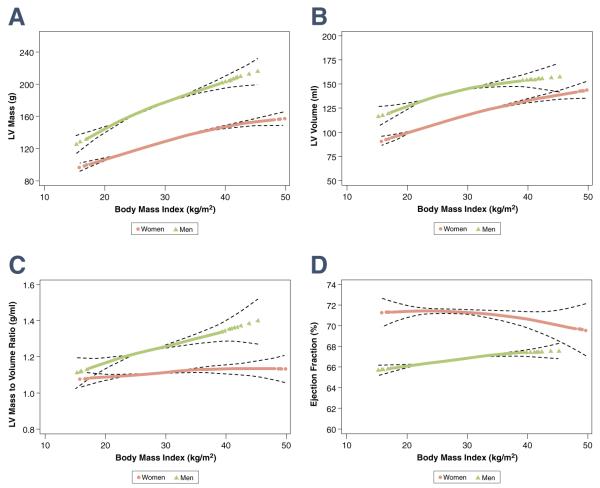
LV mass and end-diastolic volume were positively associated with BMI in a nonlinear fashion for both sexes (Fig. 1A, B). The increase in LV mass per each 10-kg/m2 increase in BMI for men was 44 g for lean individuals (i.e., BMI <25 kg/m2) versus 28 g for obese individuals (p < 0.001 for both). For men with an average LV size (169 g), a 10-unit change in BMI corresponded to a 26% increase in LV mass. The increase in LV end-diastolic volume per each 10-kg/m2 increase in BMI for lean and obese men was 27 ml and 10 ml, respectively (p < 0.001 and p = 0.008, respectively). For men with an average LV volume (140 ml), a 10-unit change in BMI corresponded to a 19% increase in LV volume. Similar relationships were also observed for women. The slope of the mean LV mass curve was steeper for men than for women in the obese range (p < 0.001 for sex interaction), whereas the slope of LV end-diastolic volume did not differ significantly by sex (p = 0.35 for sex interaction) (Table 4).
Figure 1. Association of BMI With LV Parameters.
Generalized additive models representing the association of body mass index (BMI) with left ventricular (LV) mass (A), end-diastolic volume (B), mass-to-volume ratio (C), and ejection fraction (D) after adjustment for risk factors. Fully adjusted models per Table 4. The color lines represent the mean values of LV parameters and the dashed lines represent 95% confidence intervals.
Table 4.
Association of Obesity Measures With LV Parameters by Sex After Adjustment for Risk Factors in MESA Participants With CMR (N = 5,004)
| Women |
Men |
|||||
|---|---|---|---|---|---|---|
| LV Parameter | Obesity Measure | Slope (per 10-Unit Change in Obesity Measure) |
p Value | Slope (per 10-Unit Change in Obesity Measure) |
p Value | p Value for Sex Interaction |
| LV mass (g) | BMI range (kg/m2) | |||||
| <25 | 21.9 | <0.001 | 44.2 | <0.001 | <0.001 | |
| 25–30 | 27.0 | <0.001 | 26.1 | <0.001 | ||
| >30 | 15.4 | <0.001 | 27.6 | <0.001 | ||
| FM (kg) | 5.7 | <0.001 | 6.9 | <0.001 | 0.15 | |
| LBM (kg) | 19.1 | <0.001 | 18.6 | <0.001 | 0.36 | |
| WHR* | 48.3 | <0.001 | 69.4 | <0.001 | <0.001 | |
| LV volume (ml) | BMI range (kg/m2) | |||||
| <25 | 21.7 | <0.001 | 27.2 | <0.001 | 0.35 | |
| 25–30 | 19.1 | <0.001 | 13.0 | 0.001 | ||
| >30 | 13.4 | <0.001 | 10.4 | 0.008 | ||
| FM (kg) | 3.4 | <0.001 | −2.1 | 0.052 | <0.001 | |
| LBM (kg) | 21.7 | <0.001 | 23.9 | <0.001 | 0.10 | |
| WHR* | 12.8 | 0.038 | 25.9 | 0.013 | 0.38 | |
| M/V ratio (g/ml) | BMI range (kg/m2) | |||||
| <25 | 0.01 | 0.997 | 0.10 | 0.024 | <0.001 | |
| 25–30 | 0.05 | 0.051 | 0.08 | 0.021 | ||
| >30 | 0.01 | 0.497 | 0.09 | 0.004 | ||
| FM (kg) | 0.02 | <0.001 | 0.06 | <0.001 | <0.001 | |
| LBM (kg) | −0.04 | 0.001 | −0.07 | <0.001 | 0.45 | |
| WHR* | 0.32 | <0.001 | 0.33 | <0.001 | 0.74 | |
| Ejection fraction (%) | BMI range (kg/m2) | |||||
| <25 | 0.2 | 0.88 | 2.2 | 0.11 | 0.80 | |
| 25–30 | 0.1 | 0.90 | 0.0 | 0.98 | ||
| >30 | −1.0 | 0.06 | −0.7 | 0.47 | ||
| FM (kg) | −1.0 | 0.46 | 0.4 | 0.14 | 0.28 | |
| LBM (kg) | −0.4 | 0.34 | −1.0 | 0.02 | 0.48 | |
| WHR* | 0.82 | 0.64 | −0.97 | 0.70 | 0.20 | |
Each slope corresponds to 1-unit change in WHR. All models are stratified by sex, and adjusted for age, race, systolic and diastolic blood pressures, use of antihypertensive medications, diabetes, cigarette smoking, total cholesterol, HDL, log triglycerides, use of lipid-lowering medication, family history of heart attack, heavy drinking, and intentional exercise in quartiles. Linear regression models examining associations between FM and LV parameters additionally adjusted for LBM.
LV M/V ratio was positively associated with BMI for men (slope: 0.09-g/ml increase in M/V ratio per 10-unit increase in BMI for obese individuals or approximately 8% increase in M/V ratio). Over the range of observed M/V ratios (approximately 1.1 to 1.4), 30% of that range was accounted for by a 10-unit change in BMI. For women, there was no significant change in M/V ratio with increasing BMI (slope: 0.01-g/ml increase in M/V ratio per 10-unit increase in BMI for obese individuals) (Fig. 1C, Table 4).
There were no significant associations between ejection fraction and BMI for either sex (p = 0.8, for sex interaction) (Fig. 1D).
Association of LV size and function with FM
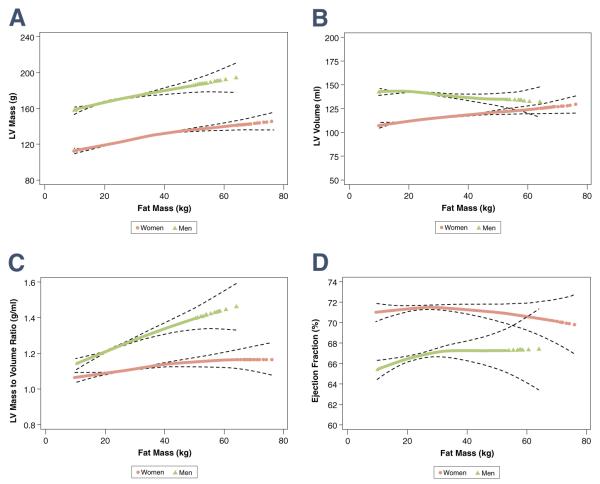
LV mass was positively associated with FM at a given level of lean body mass for both sexes (p = 0.15 for sex interaction) (Fig. 2A). On average, LV mass increased 5.7 g (4.5%) for women and 6.9 g (4.1%) for men per 10-kg increase in FM (p < 0.001 for both). At a given level of lean body mass (Fig. 2B), the increase in the mean LV end-diastolic volume was 3.4 ml for women (p < 0.001) and −2.1 ml for men (p = 0.052) per 10 kg of FM (Table 4).
Figure 2. Association of FM With LV Parameters.
Generalized additive models representing the association of fat mass (FM) with left ventricular (LV) mass (A), volume (B), mass-to-volume ratio (C), and ejection fraction (D) after adjustment for risk factors. Fully adjusted models per Table 4. The color lines represent the mean values of LV parameters and the dashed lines represent 95% confidence intervals.
M/V ratio was positively associated with FM (Fig. 2C) (slope: 0.02-g/ml increase in M/V ratio for women and 0.06-g/ml increase in M/V ratio for men per 10-kg increase in FM). The slopes were steeper for men compared with women (p < 0.001 for sex interaction). There was no significant association between ejection fraction and FM for either sex (p = 0.28 for sex interaction) (Fig. 2D).
Associations of LV size and function with WHR
The associations of LV mass (Online Appendix Fig. 1A) and end-diastolic volume (Online Appendix Fig. 1B) with WHR had the same trend as for other measures of obesity but with diminished magnitude. The M/V ratio (Online Appendix Fig. 1C) increased with increasing WHR for women (slope: 0.32-g/ml increase in M/V ratio per unit increase in WHR) and men (slope: 0.33-g/ml increase in M/V ratio per unit increase in WHR) in a similar fashion (p = 0.74 for sex interaction) (Table 4). There was no significant association between ejection fraction and WHR (p = 0.20 for sex interaction) (Online Appendix Fig. 1D).
WC showed a similar pattern in the associations for LV mass, end-diastolic volume, and M/V ratio (not shown).
Differences between obese groups with and without risk factors
We examined differences in LV mass and function in participants with and without cardiovascular risk factors (i.e., diabetes, hypertension, smoking, alcohol use). Both groups showed similar associations with BMI and FM for all LV parameters (p > 0.05 for all). Those with risk factors had a significantly higher LV mass, but a nonsignificantly higher LV volume at baseline compared with those without risk factors for both sexes across the whole range of BMIs (not shown).
Race/ethnicity differences
The associations of LV indexes with measures of body size were in a similar direction and of the same magnitude for all ethnic groups except the associations of LV mass and M/V ratio with FM and BMI for men. The associations between FM and BMI were stronger in Caucasian and Hispanic men than in African-American and Chinese men. The increase in the mean LV mass per 10-kg increase in FM was 6.1 g in Caucasian men (p = 0.001), 7.7 g in Chinese men (p = 0.027), 6.4 g in African-American men (p = 0.009), and 9.7 g (p = 0.001) in Hispanic men.
For M/V ratio, the increase in M/V ratio per 10-kg increase in FM was 0.08 kg/ml in Caucasian men (p < 0.001), 0.06 kg/ml in Chinese men (p = 0.047), 0.03 kg/ml in African-American men (p = 0.13), and 0.10 kg/ml (p < 0.001) in Hispanic men.
DISCUSSION
The results of this study indicate that obesity is positively related to LV mass and volume in a large, community-based multiethnic population. Using multiple measures of obesity (BMI, WC, WHR, and FM), LV mass increased to a greater extent than LV volume. We observed 1) increasing levels of obesity were associated with concentric LV remodeling, expressed by increased LV M/V ratio; 2) the increased M/V ratio was due to a greater increase in LV mass relative to LV end-diastolic volume; 3) the relationships between obesity measures and LV mass and M/V ratio were generally greater in Hispanic and Caucasian men compared with other subgroups; 4) global ventricular systolic function (assessed by ejection fraction) was insensitive to myocardial changes associated with obesity.
Obesity has been considered as a state of chronic volume overload because the heart is required to circulate blood through the large and relatively low resistance depot of adipose tissue. Early studies had suggested that obesity was associated with eccentric LV remodeling. The results of this CMR study and other echocardiography studies instead now consistently show that both LV cavity size and wall thickness may be increased in obese subjects with wall thickness increased to a greater extent than cavity size (concentric LV remodeling) (3,14–16). Several studies have found that LV ejection fraction is normal to increased in the majority of obese subjects (14,17).
Multiple biological mechanisms have been implicated in explaining the impact of excess adiposity on LV geometry and function. Visceral fat, which has been shown to be the metabolically active compartment of fat deposits, may mediate the increased LV mass by secreting a variety of bioactive molecules such as angiotensin II and inflammatory cytokines. A previous MESA study has reported that pathways related to inflammation might, at least partially, explain the association between obesity and chronic heart failure (18). Hyperinsulinemia and insulin resistance, which are also closely related to abdominal obesity, may induce myocardial hypertrophy by growth-stimulating effect of insulin or increasing blood volume (19). Typically, higher systolic blood pressures, even if they are not in the hypertensive range, have an additive effect on concentric myocardial remodeling. Finally, obstructive sleep apnea could contribute to LV hypertrophy by exacerbation of daytime and nighttime hypertension, increased sympathetic tone, and chronic hypoxemia (19).
Iacobellis and Sharma (20) proposed “uncomplicated obesity” as those individuals with elevated BMI but with normal fasting glucose, glucose tolerance, systolic and diastolic blood pressures, lipid profile, resting electrocardiogram, and thyroid function, without history of metabolic, cardiovascular, respiratory disease, and clinically significant abnormalities on physical examination. They reported that indexed LV mass and LV geometry in subjects with uncomplicated obesity (n = 75) were not significantly different from a lean control group (n = 60) (17). In the present study, only 1.8% (89/5,004) of participants were obese and without hypertension, impaired glucose tolerance/diabetes, dyslipidemia, and major electrocardiographic changes. Therefore, the concept of uncomplicated obesity was not useful in our study population due to the rare occurrence of this phenotype.
Determining the relationship between obesity and cardiac size is confounded by the known positive relationship of body size to LV mass and volume. Body surface area is the most common index for cardiac size but has been suggested to underestimate the impact of obesity on LV mass and geometry (21). Alternatively, indexing LV mass to the 2.7 power of height has been reported to be appropriate for but has unknown applicability for CMR. For the MESA population, LV mass indexed to the 2.7 power of height resulted in a higher proportion of LV hypertrophy for shorter participants compared with taller participants (data not shown), raising questions regarding the validity of this approach for our data.
To overcome this difficulty, we looked at multiple measures of obesity (BMI, WC, and WHR) and also examined the association of FM with LV size after controlling for fat-free mass. In addition, LV M/V ratio and ejection fraction allow ventricular geometry and function, respectively, to be assessed without the need for further body size adjustment. With all measures of obesity, ejection fraction showed no consistent change in relation to in- creased obesity levels.
Study limitations
Selection of participants in MESA was designed to minimize biases typically associated with studies of volunteers. Because all our participants were free of clinically apparent cardiovascular disease at baseline, participants represent a relatively healthy population-based sample. Severely obese participants (>300 pounds) had to be excluded because of CMR bore-diameter and table weight limits. Estimation of FM from weight-height models allowed only an approximate evaluation of FM amount.
CONCLUSIONS
In a multiethnic population, various measures of obesity are associated with concentric LV remodeling, marked by increased M/V ratio, due to a greater increase in LV mass than in LV end-diastolic volume. Ejection fraction was an insensitive marker of myocardial changes associated with obesity as assessed by multiple measures of body size and composition.
Supplementary Material
Acknowledgments
The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org.
This research was supported by contracts N01-HC-95159 through N01-HC-95169 from the National Heart, Lung, and Blood Institute.
ABBREVIATIONS AND ACRONYMS
- BMI
body mass index
- CMR
cardiac magnetic resonance
- FM
fat mass
- LV
left ventricular
- M/V
mass to volume
- WC
waist circumference
- WHR
waist-to-hip ratio
Footnotes
APPENDIX For additional figures, please see the online version of this article.
REFERENCES
- 1.Poirier P, Giles TD, Bray GA, et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2006;113:898–918. doi: 10.1161/CIRCULATIONAHA.106.171016. [DOI] [PubMed] [Google Scholar]
- 2.Vasan RS. Cardiac function and obesity. Heart. 2003;89:1127–9. doi: 10.1136/heart.89.10.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lauer MS, Anderson KM, Kannel WB, Levy D. The impact of obesity on left ventricular mass and geometry. The Framingham Heart Study. JAMA. 1991;266:231–6. [PubMed] [Google Scholar]
- 4.Peterson LR, Waggoner AD, Schechtman KB, et al. Alterations in left ventricular structure and function in young healthy obese women: assessment by echocardiography and tissue Doppler imaging. J Am Coll Cardiol. 2004;43:1399–404. doi: 10.1016/j.jacc.2003.10.062. [DOI] [PubMed] [Google Scholar]
- 5.Chuang ML, Danias PG, Riley MF, Hibberd MG, Manning WJ, Douglas PS. Effect of increased body mass index on accuracy of two-dimensional echocardiography for measurement of left ventricular volume, ejection fraction, and mass. Am J Cardiol. 2001;87:371–4. A10. doi: 10.1016/s0002-9149(00)01383-7. [DOI] [PubMed] [Google Scholar]
- 6.Bellenger NG, Burgess MI, Ray SG, et al. Comparison of left ventricular ejection fraction and volumes in heart failure by echocardiography, radionuclide ventriculography and cardiovascular magnetic resonance; are they interchangeable? Eur Heart J. 2000;21:1387–96. doi: 10.1053/euhj.2000.2011. [DOI] [PubMed] [Google Scholar]
- 7.Grothues F, Smith GC, Moon JCC, et al. Comparison of interstudy reproducibility of cardiovascular magnetic resonance with two-dimensional echocardiography in normal subjects and in patients with heart failure or left ventricular hypertrophy. Am J Cardiol. 2002;90:29–34. doi: 10.1016/s0002-9149(02)02381-0. [DOI] [PubMed] [Google Scholar]
- 8.Bild DE, Bluemke DA, Burke GL, et al. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–81. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 9.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 10.Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i–xii. 1–253. [PubMed] [Google Scholar]
- 11.Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—The Evidence Report. National Institutes of Healt. Obes Res. 1998;6(Suppl 2):51S–209S. [PubMed] [Google Scholar]
- 12.Kuch B, Gneiting B, Doring A, et al. Indexation of left ventricular mass in adults with a novel approximation for fat-free mass. J Hypertens. 2001;19:135–42. doi: 10.1097/00004872-200101000-00018. [DOI] [PubMed] [Google Scholar]
- 13.Natori S, Lai S, Finn JP, et al. Cardiovascular function in multi-ethnic study of atherosclerosis: normal values by age, sex, and ethnicity. AJR Am J Roentgenol. 2006;186:S357–65. doi: 10.2214/AJR.04.1868. [DOI] [PubMed] [Google Scholar]
- 14.Powell BD, Redfield MM, Bybee KA, Freeman WK, Rihal CS. Association of obesity with left ventricular remodeling and diastolic dysfunction in patients without coronary artery disease. Am J Cardiol. 2006;98:116–20. doi: 10.1016/j.amjcard.2006.01.063. [DOI] [PubMed] [Google Scholar]
- 15.Wong CY, O’Moore-Sullivan T, Leano R, Byrne N, Beller E, Marwick TH. Alterations of left ventricular myocardial characteristics associated with obesity. Circulation. 2004;110:3081–7. doi: 10.1161/01.CIR.0000147184.13872.0F. [DOI] [PubMed] [Google Scholar]
- 16.Fox E, Taylor H, Andrew M, et al. Body mass index and blood pressure influences on left ventricular mass and geometry in African Americans: The Atherosclerotic Risk In Communities (ARIC) Study. Hypertension. 2004;44:55–60. doi: 10.1161/01.HYP.0000132373.26489.58. [DOI] [PubMed] [Google Scholar]
- 17.Iacobellis G, Ribaudo MC, Leto G, et al. Influence of excess fat on cardiac morphology and function: study in uncomplicated obesity. Obes Res. 2002;10:767–73. doi: 10.1038/oby.2002.104. [DOI] [PubMed] [Google Scholar]
- 18.Bahrami H, Bluemke DA, Kronmal R, et al. Novel metabolic risk factors for incident heart failure and their relationship with obesity: the MESA (Multi-Ethnic Study of Atherosclerosis) study. J Am Coll Cardiol. 2008;51:1775–83. doi: 10.1016/j.jacc.2007.12.048. [DOI] [PubMed] [Google Scholar]
- 19.Abel ED, Litwin SE, Sweeney G. Cardiac remodeling in obesity. Physiol Rev. 2008;88:389–419. doi: 10.1152/physrev.00017.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Iacobellis G, Sharma AM. Obesity and the heart: redefinition of the relationship. Obes Rev. 2007;8:35–9. doi: 10.1111/j.1467-789X.2006.00257.x. [DOI] [PubMed] [Google Scholar]
- 21.Levy D, Anderson KM, Savage DD, Kannel WB, Christiansen JC, Castelli WP. Echocardiographically detected left ventricular hypertrophy: prevalence and risk factors. The Framingham Heart Study. Ann Intern Med. 1988;108:7–13. doi: 10.7326/0003-4819-108-1-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.