Abstract
Background: Coronary artery disease (CAD) remains the leading cause of death in the US. In 1996, Kaiser Permanente of Colorado (KPCO) developed the Collaborative Cardiac Care Service (CCCS) with the goal of improving the health of patients with CAD.
Description: CCCS consists of a nursing team (the KP Cardiac Rehabilitation program) and a pharmacy team (the Clinical Pharmacy Cardiac Risk Service). CCCS works collaboratively with patients, primary care physicians, cardiologists, and other health care professionals to coordinate proven cardiac risk reduction strategies for patients with CAD. Activities such as lifestyle modification, medication initiation and adjustment, patient education, laboratory monitoring, and management of adverse events are all coordinated through CCCS. The CCCS uses an electronic medical record and patient-tracking software to document all interactions with patients, track patient appointments, and collect data for evaluation of both short- and long-term outcomes.
Outcomes: The CCCS currently follows over 12,000 patients with CAD. The CCCS has demonstrated improvement in surrogate outcomes including: cholesterol screening (55% to 96.3%), the proportion of patients with a goal of low-density lipoprotein cholesterol (LDL-c) <100 mg/dL (22% to 76.9%), and has reduced the average LDL-c to 78.3 mg/dL for the CAD population it follows. The CCCS has shown a reduction in all-cause mortality associated with CAD by 76% in the patients followed by the service. Patient and physician satisfaction have been high with CCCS.
Conclusion: The CCCS coordinates many aspects of cardiac risk reduction care resulting in excellent continuity of care. The CCCS has continued to grow and expand the number of patients enrolled by using innovative strategies and technology and has resulted in excellent care and improved outcomes of the CAD population at KPCO.
Introduction
Cardiovascular disease remains the leading cause of death in the US.1 It is estimated that in 2008, 770,000 Americans will have a new coronary event and 430,000 will have a recurrent event.1 Fewer than half of patients with coronary artery disease (CAD) are treated to nationally recommended targets for low-density lipoprotein cholesterol (LDL-c).2 Individual pharmacologic strategies have been shown to reduce CAD morbidity and mortality by up to 30%, but it is unknown what the reduction would be with the initiation of proven secondary strategies. It is estimated that morbidity and mortality could be reduced up to 97% when patients are taking a “poly-pill.” 3,4 Even with numerous studies and guidelines recommending the use of proven secondary prevention treatment strategies,5–15 data suggest a treatment gap between the evidence supporting these strategies and the implementation of these strategies.2,16,17 Such was the case with Kaiser Permanente of Colorado (KPCO).
The cause for the treatment gap is multifactorial, but largely related to patient, clinician, and health care system factors.2,16 To help close the CAD treatment gap, interventions should address each of these factors. Because of the baseline metrics in the Colorado Region, secondary prevention programs were developed, using multidisciplinary teams that focus on cardiac risk factor management to address the treatment gap.
Since 1996, the Collaborative Cardiac Care Service (CCCS) has improved the health of KPCO patients with CAD. CCCS is made up of a nursing team—the KP Cardiac Rehabilitation program (KPCR)—and a pharmacy team—the Clinical Pharmacy Cardiac Risk Service (CPCRS)—whose patient care activities complement each other (Table 1). The CCCS coordinates the provision of cardiac risk reduction activities by working collaboratively with and supporting patients, primary care physicians, cardiologists, and other health care professionals and focusing on activities that have been shown to improve patient outcomes. The goal of this paper is to describe the development, innovation, and outcomes of the CCCS.
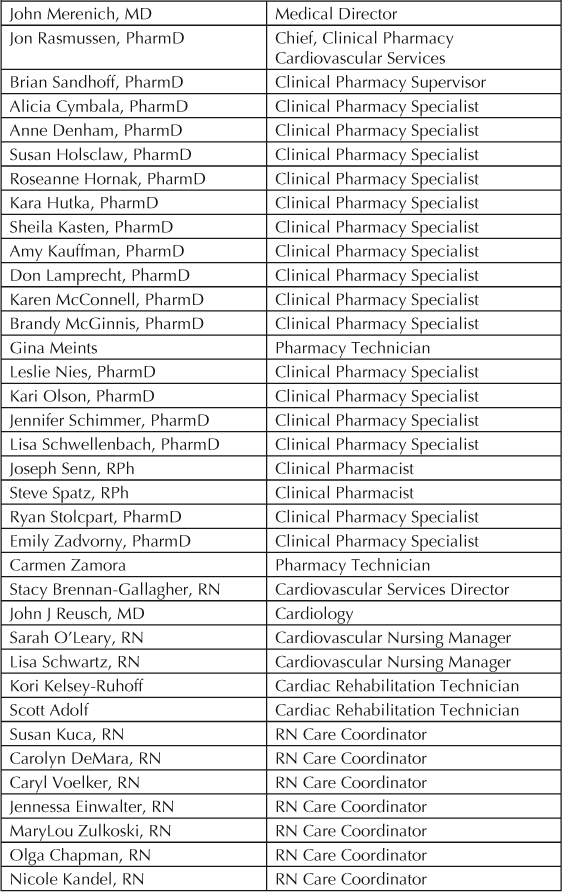
Table 1.
Members of the Collaborative Cardiac Care Service in Kaiser Permanente Colorado
History
In 1996, KPCO implemented a registered nurse-managed cardiac rehabilitation program, based on the Multifit program, that focused on management and education of patients discharged from the hospital following acute coronary events. After completion of the cardiac rehabilitation program, the patients were transferred back to their primary care physician for follow-up. There was no formal long-term follow-up for patients following discharge from the rehabilitation program. The nurse-managed cardiac rehabilitation program helped improve the CAD surrogate outcomes of the patients (eg, cholesterol levels) but, because of the program design, focused on short-term follow-up of patients with recent events.18
In 1998, KPCO assessed the use of secondary prevention strategies in the entire CAD population. The results were similar to reports in the literature: 22% of the CAD population had achieved the LDL-c goal of less than 100 mg/dL, 85% were on beta-blockers following myocardial infarction, and 90% were on aspirin.18 KPCO also participated in the Quality Assurance Program, which showed that of 48,000 patients with CAD, only 44% had annual LDL-c testing, and of these patients 25% had an LDL-c of less than 100mg/dL.19 These results suggested that, in addition to modifying the current cardiac rehabilitation program, another program that focused on the long-term management of patients with CAD was necessary. Additionally, this program would need to follow patients with a history of previous coronary events, not just patients with recent coronary events.
Modifications were made to the nurse-managed cardiac rehabilitation program—primarily the Multifit program. The case-management concept was maintained but more efficiencies were included: consolidating the number of phone calls and having more group visits than one-on-one visits. In April 1998, in an effort to improve adherence and to increase the number of acute coronary syndrome (ACS) patients discharged on HMG Coenzyme-A reductase inhibitors (statin) therapy, a guideline was implemented allowing KPCR nurses to enroll patients, and initiate statin therapy at discharge, without in-patient cholesterol measurement. In addition, the cardiac rehab team targeted patients using tobacco. Guidelines allowed nurses to start pharmacologic therapy at discharge for smoking cessation.
The focus of CCCS is on both short-term and long-term outcomes. … has improved both surrogate and clinical outcomes.
CPCRS was created to improve management and treatment of patients with CAD. The focus of CPCRS is long-term management to ensure appropriate cholesterol-lowering, hypertension, diabetes, and smoking-cessation medications are initiated and adjusted. Follow-up laboratory tests assess achievements of LDL-c, blood pressure, and diabetes goals, to ensure that other medications (shown to reduce the risk of future cardiac events)—aspirin, beta-blockers, and angiontensin-converting enzyme inhibitors (ACEI)—are initiated when appropriate. CPCRS monitors and assists management of disease states that increase cardiovascular risk, provides patient education and recommendations for nonpharmacologic therapy, and acts as a resource to primary care physicians, cardiologists, cardiac rehabilitation nurses, and other health care professionals.
CCCS Approach
All patients diagnosed with an acute coronary event are offered enrollment into CCCS, and can opt out if later not interested. Patients are offered intensive cardiac rehabilitation education, psychosocial support, exercise therapy, and secondary risk-factor modification —smoking cessation and dietary counseling.
KPCR
The KPCR team contacts all patients hospitalized with an acute coronary event within 24 hours of discharge. Patients seen in non-KP hospitals are identified and KPCR is notified and contacts those patients to enroll them. This outreach call is typically divided into safety and risk-factor counseling. The cardiac rehabilitation nurse assesses symptom recognition, current symptoms, incision care, and medication reconciliation. On identifying an issue, the nurse contacts a clinician for orders or disposition (home care, clinic follow-up, or Emergency Department). Medication issues are clarified with the physician. The medical record is updated and the patient is educated. If the patient is not on an appropriate dose of cholesterol-lowering medications or does not have sublingual (SL) nitroglycerin and it is indicated, the medications are ordered per KPCR guidelines. Following the safety assessment and medication reconciliation, the nurse reviews the risk factors for CAD and assists in setting appropriate goals. A detailed plan is developed with the patient including time of contacts, education, and referrals to other specialists, as indicated. Tobacco cessation counseling is provided for all patients who use tobacco. If a patient is ready to quit smoking, the cardiac rehabilitation nurse can order appropriate smoking cessation medications per regional guidelines. During follow-up visits—by phone, in educational sessions, or in-person visits depending on patient need—the nurse assesses the current plan, which, in conjunction with the patient, is modified as necessary, reviewing barriers and solutions for meeting goals. Patients are followed for three to six months, but KPCR is a resource for as long as the patient is a member of KP. Following discharge from KPCR, the patient is referred to CPCRS for enrollment and long-term follow-up.
CPCRS
Primary care physicians may also refer patients to CPCRS. Additionally, patients with a CAD event prior to their enrollment in KPCO are enrolled in CPCRS through the Colorado Region Disease State Management Registry, and assigned to a personal clinical pharmacy specialist, who manages the patient's medication regimen as long as the patient is a member of KP. The average enrollment time in CPCRS is 4.5 years. The average panel size for a clinical pharmacy specialist is approximately 800 patients. The clinical pharmacy staff at CPCRS ensures that patients receive appropriate cardiac risk-reduction medications, and orders the appropriate laboratory tests to monitor the efficacy and safety of those medications. They provide ongoing diet and exercise education and refer patients to KPCO education resources. CPCRS also emphasizes the importance of medication adherence in reducing recurrent cardiac events. The CPCRS staff ensures that patients with major cardiovascular risk factors —uncontrolled diabetes or hypertension—receive the necessary care to improve. Furthermore, patients who smoke are advised to stop and are referred for behavior modification therapy through the Health Education Department at KPCO or the Colorado Quitline. CPCRS ensures that patients are evaluated and started, when no contraindications are identified, on beta-blockers (for a history of myocardial infarction) and a daily aspirin (to reduce the risk of death and recurrent cardiovascular events).
CCCS uses an electronic medical chart, HealthConnect: to document all interactions with patients, to order medications and follow-up laboratory tests, and to notify physicians about abnormal values and adverse drug reactions. With HealthConnect, CCCS staff reviews records for pertinent patient's care information and to reinforce prescribed therapies.
CCCS patients are also entered into a Web-based tracking database, HealthTrac—used in conjunction with HealthConnect—and schedule follow-up appointments such as fasting lipid profiles and blood pressure checks. Through these appointments all patients are tracked, allowing identification of patients not receiving follow-up laboratory tests as scheduled.
Monthly queries using HealthTrac identify patients with laboratory tests scheduled for that month, and letters are mailed reminding them. If the patient does not respond after two reminder letters, they receive a telephone call from a pharmacy technician. In addition, HealthTrac generates surrogate outcome reports, such as LDL-c cholesterol or blood pressure measurements, as tracking tools, and is updated daily with administrative, pharmacy, laboratory, diagnosis and procedure, vital sign, and demographic data.
Outcomes
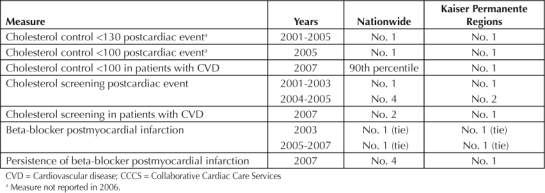
The focus of CCCS is on both short-term and long-term outcomes. Since its inception, CCCS has improved both surrogate and clinical outcomes. In an early analysis of 100 patients followed by KPCR for one year, improvements in LDL-c control and screening, smoking cessation rates, and patient-reported diet and activity were shown.18 These preliminary results led to the expansion of KPCR. KPCR also demonstrated improvement in tobacco cessation. In a review of 269 patients, those receiving counseling while still in the hospital resulted in better long-term outcomes on tobacco cessation, 60%, compared with those counseled after discharge, 41%.a An early analysis of 1716 patients enrolled in CPCRS showed that the LDL-c screening rates increased from 55% to 97% in less than one year. Additionally, patients with an LDL-c of less than 100mg/dL increased to 48%, from 22%. Patients taking aspirin or other antiplatelet therapy increased from 90% to 97% and patients taking beta-blockers following myocardial infarction improved from 85% to 92% in the initial assessment of the program.18 CCCS achieved benchmark status in many clinically important outcome measures for Healthcare Effectiveness Data and Information Set (HEDIS). In 2007, KPCO was in the 90th percentile in the nation for cholesterol control <100mg/dL and number two in the nation for cholesterol screening in patients with cardiovascular disease. KPCO was also number four in the nation for persistence of beta-blockers in postmyocardial infarction patients. HEDIS results from 2001 to 2007 are shown in Table 2.
Table 2.
Healthcare Effectiveness Data and Information Set (HEDIS) results for CCCS
During the first two years of CCCS, the service only impacted approximately 200 patients. On the basis of the preliminary results, the decision was made to expand the service. To date, more than 27,000 patients have been screened for enrollment into CCCS and more than 25,000 (93%) have been validated for enrollment. CCCS is currently following over 12,000 patients with CAD.
Random surveys sent out to patients followed by KPCR revealed that 95% were “very satisfied” or “extremely satisfied” with the service that KPCR offered.18 In a survey of CPCRS patients, 94.6% of 491 patients who responded showed they strongly agreed or agreed that they were satisfied with the care they received from CPCRS, and 83.7% strongly agreed or agreed that they could easily contact the CPCRS staff.20 Also, internal physician satisfaction survey demonstrated that 88% of the respondents were satisfied or very satisfied with the care that CCCS provided their patients.
A retrospective, cohort observational review in 2005 of 8014 patients enrolled in the program showed that screening for cholesterol increased from 66.9% to 97.3% at the end of the evaluation period. The number of patients attaining an LDL-c goal of <100mg/dL increased from 25.5% to 72.7%. Approximately 85% of these patients were receiving statin monotherapy. The average LDL-c for those 8014 patients decreased from 119 mg/dL to 89mg/dL.21
CCCS also demonstrated an improvement in morbidity and mortality. In an analysis of patients enrolled from 1996 to 2004, all-cause and CAD-related mortality decreased when compared with patients not enrolled in CCCS (Figure 1).22 In this analysis, patients were categorized into four cohorts on the basis of their type of enrollment: 1) early CCCS—enrolled within 90 days of their event and continuously followed; 2) delayed CCCS—enrolled in the program 90 or more days following their event and continuously followed; 3) intermitted CCCS—patients enrolled after their event but not continuously followed; and 4) no CCCS—patients who were not followed at any point by CCCS. Over an average enrollment of 3.6 years, patients experienced a reduced incidence of all-cause mortality by 76% and cardiac-related mortality by73%. Patients in the early CCCS cohort had an 89% reduction in all-cause mortality and an 88% reduction in cardiac-related mortality when compared with those patients with no exposure to CCCS.22 These results suggest that comprehensive, aggressive, and continuous implementation of secondary prevention strategies using systems that enable close follow-up and monitoring of patients is associated with reduced mortality. Current demographic information and metrics for CCCS are shown in Table 3.
Figure 1.
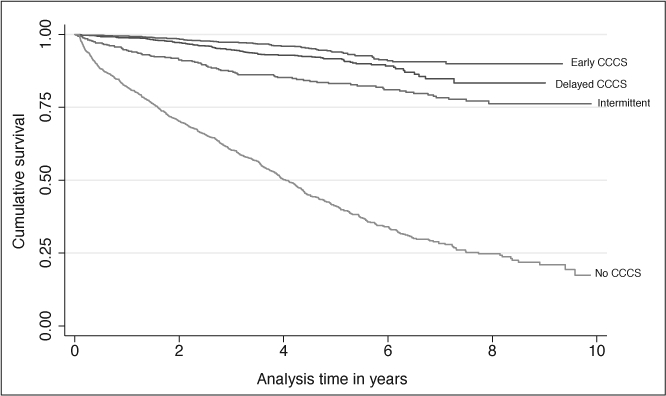
Kaplan-Meier curves for all-cause and cardiac-related mortality by year: All cause.
CCCS = Collaborative Cardiac Care Service
Table 3.
Demographic and metric information for patients currently enrolled in CCCS
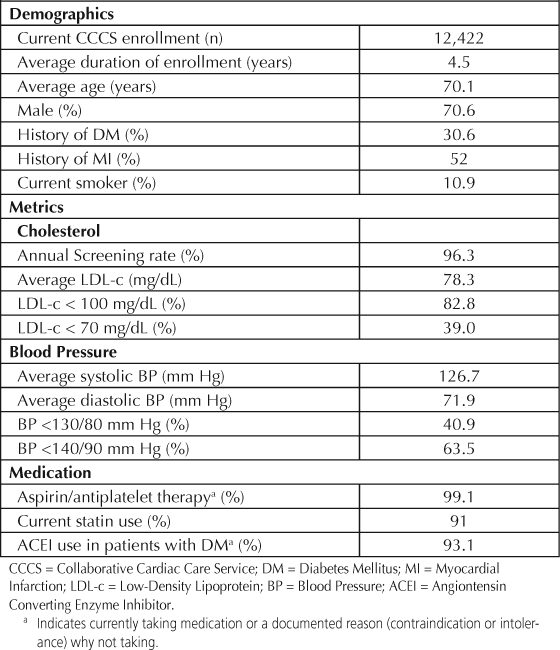
Figure 2.
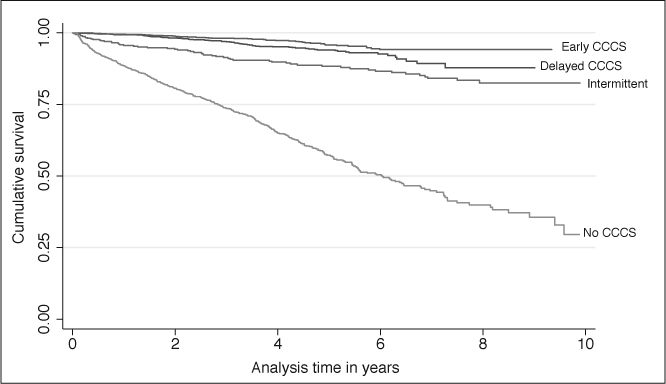
Kaplan-Meier curves for all-cause and cardiac-related mortality by year: Cardiac related.1
CCCS = Collaborative Cardiac Care Service
Note: Patients with a CAD event were categorized into one of four cohorts by time to enrollment into the Collaborative Cardiac Care Service relative to cardiac event: enrolled within (early CCCS) or outside (delayed CCCS) 90 days of cardiac event; enrolled intermittently (intermittent CCCS); or never enrolled (No CCCS).
1Merenich JA, Olson KL, Delate T, Rasmussen J, Helling DK, Ward DG; Clinical Pharmacy Cardiac Risk Service Study Group. Mortality reduction benefits of a comprehensive cardiac care program for patients with occlusive coronary artery disease. Reprinted with permission from Pharmacotherapy.
Future
By working as a collaborative team to manage the risk factors of patients with CAD, CCCS, using the skills of both nurses and clinical pharmacy specialists, demonstrated improved cardiovascular care. The CCCS uses technology to quickly and efficiently communicate with clinicians and patients, resulting in seamless care. The CCCS allows primary care physicians and cardiologists to focus on other acute patient issues knowing that their risk factors are being addressed.
CCCS currently follows patients with CAD for the duration of their membership in KP, but is often asked to follow other high-risk populations. To extend services to other high-risk patient populations, CCCS adapted the way it identifies and follows patients. Using administrative reports, nurses identify hospitalized patients without being on-site, and so could expand their focus to include patients with peripheral arterial disease and high-risk cardiology patients. As the patient panels for the clinical pharmacy specialists neared capacity, the large number of well-controlled patients were moved to a new maintenance program that allowed transfer of patients back to their primary care physician. To ensure risk-factor control, queries identify patients due for annual cholesterol screening, nonadherent to their secondary prevention medications, or with uncontrolled cholesterol or blood pressure values. Patients who exceed their targets are re-enrolled into active CCCS management. In 2007, nearly 2500 patients were gradually enrolled into the maintenance program, reducing the number of laboratory tests addressed by CCCS staff by 90%. By focusing resources on only those patients requiring interventions, the services of CCCS can now be offered to other high-risk populations. This innovative program has allowed for the expansion of CCCS so that clinical pharmacy specialists now follow high-risk cardiology and ischemic stroke patients.
Economic Assessment
The business case for starting CCCS was driven by the Scandinavian Simvastatin Survival Study (4S) trial data, which showed patients who started on simvastatin 20mg daily had a 30% reduction in morbidity and mortality over 5.4 years.5 Using this data, it was estimated that CCCS would save $9 million in hospitalization costs over six years. CCCS improved the surrogate outcomes in the CAD patients it follows, and demonstrated a decrease in their morbidity and mortality.22 The indirect costs associated with the improvement in morbidity and mortality has not been evaluated. Using National Committee for Quality Assurance (NCQA) data, it was estimated that CCCS provides $3,000,000 annualized cost-savings, attributed to reduced hospitalizations (based on a reduction of 266 major cardiac events/year). CCCS is currently evaluating total costs associated with the program, including staffing and drug intervention costs, and comparing them to the costs associated with improvements in morbidity and mortality.
Transferability
Successful implementation of a CCCS in other regions depends on specific key factors. First, identifying appropriate personnel is critical. CCCS is designed to use the strengths of the individual health care professionals involved in the program. The nurses play a critical role educating patients following hospitalization. Patients can be overwhelmed on discharge following a CAD event. Medications play a significant role in the long-term management of patients with CAD. The clinical pharmacy specialists in CPCRS are medication experts who maximize therapy and minimize problems patients may have with medications. It is necessary to have appropriate systems available to manage and to identify patients enrolled in CCCS—HealthTrac and HealthConnect track patients and minimize patients lost to follow-up. These systems streamline communication of treatment plans and problems to the clinicians in the region. They also generate outcomes reports, which provide feedback to CCCS on performance. Lastly, collaboration between CCCS and physicians is integral to the success of CCCS. The CCCS has been implemented (in modified form) in the KP Georgia Region which has experienced success with this model—they were the #1 HMO in the nation in Cholesterol Screening Post-Cardiac Event in 2005 as reported by NCQA.23
In 2007, KPCO was in the 90th percentile in the nation for cholesterol control <100mg/dL and number two in the nation for cholesterol screening in patients with cardiovascular disease.
Conclusion
The CCCS program was developed to provide high-quality care to patients with CAD. Since its inception, CCCS has shown improvement in both surrogate and clinical outcomes. Many aspects of cardiac risk reduction therapy are coordinated through CCCS resulting in excellent continuity of care. Activities such as behavior modification, patient education, laboratory monitoring, medication initiation, adjustment of medications, and management of adverse events are all coordinated through the CCCS. Patients and physicians have been satisfied with the service that CCCS provides. CCCS has continued to grow and expand the number of patients enrolled by using innovative strategies and technology and has resulted in excellent care and improved outcomes of the CAD population at KPCO.
Disclosure Statement
The author(s) have no conflicts of interest to disclose.


Acknowledgments
The authors would like to thank the many people from the KPCO region that have contributed to the success of the CCCS.
Footnotes
aPresentation at the American Heart Association meeting, 2002 Nov; Chicago, IL. Schwartz L, Adolf S, Clemetson D, et.al. Initiating a tobacco cessation program during hospitalization for acute coronary events improves long-term cessation rates.
References
- Rosamond W, Flegal K, Furie K, et al. American Heart Association Statistics Committee & Stroke Statistics Subcommitee Heart disease and stroke statistics—2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008 Jan 29;117(4):e25–146. doi: 10.1161/CIRCULATIONAHA.107.187998. [DOI] [PubMed] [Google Scholar]
- Olson KL, Bungard TJ, Tsuyuki RT. Cholesterol risk management: a systematic examination of the gap from evidence to practice. Pharmacotherapy. 2001 Jul;21(7):807–17. doi: 10.1592/phco.21.9.807.34553. [DOI] [PubMed] [Google Scholar]
- Robinson JG, Maheshwari N. A “poly-portfolio” for secondary prevention: a strategy to reduce subsequent events by up to 97% over five years. Am J Cardiol. 2005 Feb 1;95(3):373–8. doi: 10.1016/j.amjcard.2004.09.036. [DOI] [PubMed] [Google Scholar]
- Wald NJ, Law MR. A strategy to reduce cardiovascular disease by more than 80% BMJ. 2003 Jun. 28;326(7404):1419. doi: 10.1136/bmj.326.7404.1419. Erratum in: BMJ 2003 Sep 13; 327(7415):586. Erratum in: BMJ 2006 Sep; 60(9):823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randomized trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study. Lancet. 1994 Nov 19;344(8934):1383–9. [PubMed] [Google Scholar]
- Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002 Jul 6;360(9326):7–22. doi: 10.1016/S0140-6736(02)09327-3. [DOI] [PubMed] [Google Scholar]
- Prevention of cardiovascular events & death with pravastatin in patients with coronary artery disease and a broad range of initial cholesterol levels. The Long-Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. N Engl J Med. 1998 Nov 5;339(19):1349–57. doi: 10.1056/NEJM199811053391902. [DOI] [PubMed] [Google Scholar]
- Sacks FM, Pfeffer MA, Moye LA, et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial Investigators. N Engl J Med. 1996 Oct 3;335(14):1001–9. doi: 10.1056/NEJM199610033351401. [DOI] [PubMed] [Google Scholar]
- Smith SC, Jr, Allen J, Blair SN, et al. AHA/ACC; National Heart, Lung, & Blood Institute AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update: endorsed by the National Heart, Lung, and Blood Institute. Circulation. 2006 May 16;113(19):2363–72. doi: 10.1161/CIRCULATIONAHA.106.174516. Erratum in: Circulation 2006 Jun 6; 113(22):3847. [DOI] [PubMed] [Google Scholar]
- Chobanian AV, Bakris GL, Black HR, et al. Joint National Committee on Prevention, Detection, Evaluation, & Treatment of High Blood Pressure, National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003 Dec;42(6):1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- Arauz-Pacheco C, Parrott MA, Raskin P, American Diabetes Association Treatment of hypertension in adults with diabetes. Diabetes Care. 2003 Jan;26(Suppl 1):S80–2. doi: 10.2337/diacare.26.2007.s80. [DOI] [PubMed] [Google Scholar]
- Baigent C, Keech A, Kearney PM, et al. Cholesterol Treatment Trialists' (CTT) Collaborators Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005 Oct 8;366(9493):1267–78. doi: 10.1016/S0140-6736(05)67394-1. Erratum in: Lancet 2005 Oct 14–21; 366(9494):1358. [DOI] [PubMed] [Google Scholar]
- Freemantle N, Cleland J, Young P, Mason J, Harrison J. beta Blockade after myocardial infarction: systematic review and meta regression analysis. BMJ. 1999 Jun 26;318(7200):1730–7. doi: 10.1136/bmj.318.7200.1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antithrombotic Trialists' Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ. 2002 Jan 12;324(7329):71–86. doi: 10.1136/bmj.324.7329.71. Erratum in: BMJ 2002 Jan 19; 324(7330):141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danchin N, Cucherat M, Thuillez C, Durand E, Kadri Z, Steg PG. Angiotensin-converting enzyme inhibitors in patients with coronary artery disease and absence of heart failure or left ventricular systolic dysfunction: an overview of long-term randomized controlled trials. Arch Intern Med. 2006 Apr 10;166(7):787–96. doi: 10.1001/archinte.166.7.787. [DOI] [PubMed] [Google Scholar]
- Qureshi AI, Suri MF, Guterman LR, Hopkins LN. Ineffective secondary prevention in survivors of cardiovascular events in the US population: report from the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2001 Jul 9;161(13):1621–8. doi: 10.1001/archinte.161.13.1621. [DOI] [PubMed] [Google Scholar]
- Newby LK, LaPointe NM, Chen AY, et al. Long-term adherence to evidence-based secondary prevention therapies in coronary artery disease. Circulation. 2006 Jan 17;113(2):203–12. doi: 10.1161/CIRCULATIONAHA.105.505636. [DOI] [PubMed] [Google Scholar]
- Merenich JA, Lousberg TR, Brennan SH, Calonge NB. Optimizing treatment of dyslipidemia in patients with coronary artery disease in the managed-care environment (the Rocky Mountain Kaiser Permanente experience) Am J Cardiol. 2000 Feb 10;85(3A):36A–42A. doi: 10.1016/s0002-9149(99)00937-6. [DOI] [PubMed] [Google Scholar]
- Sueta CA, Chowdhury M, Boccuzzi SJ, et al. Analysis of the degree of undertreatment of hyperlipidemia and congestive heart failure secondary to coronary artery disease. Am J Cardiol. 1999 May 1;83(9):1303–7. doi: 10.1016/s0002-9149(99)00117-4. Erratum in: Am J Cardiol 1999 Nov 1; 84(9):1143. [DOI] [PubMed] [Google Scholar]
- Holsclaw S, Olson KL, Hornak R, Denham A. Assessment of patient satsifaction with telephone and mail interventions provided by a clinical pharmacy cardiac risk reduction service. J Manag Care Pharm. 2005 Jun;11(5):403–9. doi: 10.18553/jmcp.2005.11.5.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson KL, Rasmussen J, Sandhoff BG, Merenich JA, Clinical Pharmacy Cardiac Risk Service Study Group Lipid management of patients with coronary artery disease by a clinical pharmacy service in a group model health maintenance organization. Arch Int Med. 2005 Jan 10;165(1):49–54. doi: 10.1001/archinte.165.1.49. [DOI] [PubMed] [Google Scholar]
- Merenich JA, Olson KL, Delate T, Rasmussen J, Helling DK, Ward DG, Clinical Pharmacy Cardiac Risk Service Study Group Mortality reduction benefits of a comprehensive cardiac care program for patients with occlusive coronary artery disease. Pharmacotherapy. 2007 Oct;27(10):1370–8. doi: 10.1592/phco.27.10.1370. [DOI] [PubMed] [Google Scholar]
- National Committee for Quality Assurance. NCQA's definitive database of health plan performance: Quality Compass [monograph on the Internet] Washington, DC: NCQA; [cited 2008 Apr 14]. Available from: www.ncqa.org/tabid/177.Default.aspx; click on “Quality Compass” to order. [Google Scholar]


