Introduction
Since the first report, in 1981, of AIDS in five men who have sex with men (MSM) in Los Angeles,1 the AIDS epidemic has swept the world. In the US, during the intervening 27 years, the demographics of the disease have changed dramatically. What was once a disease of Caucasian MSM has evolved into a disease that increasingly affects women and disproportionately affects people of color.2 This brief review will examine the demographics of the HIV epidemic as it now exists in the US.

“The World of AIDS” photo by Chris Jacobs.
Tracking the Epidemic
The Centers for Disease Control and Prevention (CDC) has assumed a pivotal role in tracking the spread of the AIDS epidemic. During the early years of the epidemic, the CDC tracked only AIDS cases, defined as: T-cell count less than 200 or development of AIDS-defining opportunistic infections. Given the poor response to HIV therapy in those early years, this method enabled the CDC to estimate with greater accuracy the numbers of people who were infected with HIV because the disease often progressed in a predictable pattern. Beginning in the mid-1990s, however, the era of highly active antiretroviral therapy (HAART) was ushered in with the advent of the protease inhibitors. For the first time, it became possible to control effectively viral replication and forestall the progression of HIV-infested patients to fulminate AIDS.3 As a result, simply tracking the new cases of AIDS was no longer a reliable way to track the spread of HIV. In recent years, nearly every state has adopted names-based HIV reporting as the most accurate method of tracking the disease. For the purposes of this review, data for AIDS cases will be reviewed for all 50 states, although HIV data will be presented only for the 33 states that had names-based HIV reporting as of 2006.
AIDS Cases and Death
Figure 1 illustrates the estimated number of AIDS cases and deaths in the US from 1985 through 2006.2 Although it appears that a “peak” occurred in 1993, this was in fact because of the expansion of the CDC's case definition of AIDS in 1993. With the introduction of HAART in 1996, many in the field expected a continued decline in the AIDS cases seen. Instead, a leveling of the number of AIDS cases was seen in the period 1999–2006.
Figure 1.
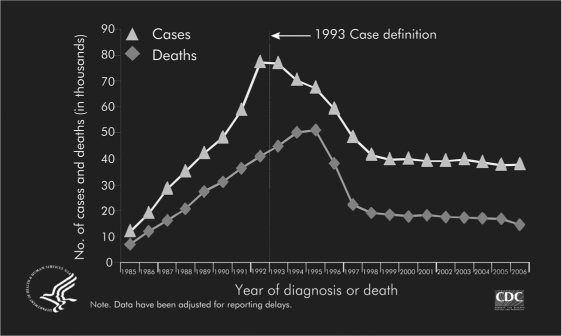
Estimated number of AIDS cases and deaths among adults and adolescents with AIDS, 1985–2006—US and dependent areas.2
Reprinted from: Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. Cases of HIV infection and AIDS in the US and Dependent Areas, 2005 [monograph on the Internet]. Atlanta (GA): US Department of Health and Human Services, Centers for Disease Control and Prevention; 2005, Rev 2007 Jun Vol 17 [cited 2008 Apr 17]. Available from: www.cdc.gov/hiv/topics/surveillance/resources/reports/2005report/default.htm.
Increasing Men-Who-Have-Sex-With-Men Rate
Turning more specifically to look at data regarding HIV infection, a gradual increase in cases has been seen consistently since 2001 (Figure 2).2 Whereas heterosexual contact cases have been stable, cases attributed to male-male contact have been on the rise consistently since 1999. In fact, the jump in male-male cases from 2004 to 2006 was among the largest jumps seen, from 16,167 cases to 18,296 cases, a 13% increase. The proportion of HIV/AIDS cases attributed to male-to-male sexual contact increased from 45% in 2003 to 50% in 2006. HIV/AIDS cases attributed to injection drug use, high-risk heterosexual contact, and male-to-male sexual contact and injection drug use remained stable from 2003 through 2006.2 These numbers are corroborated by data that also shows the rate of syphilis rising among MSM during the same time frame,4 and with data from survey-based studies reporting on the sexual habits of men.5
Figure 2.
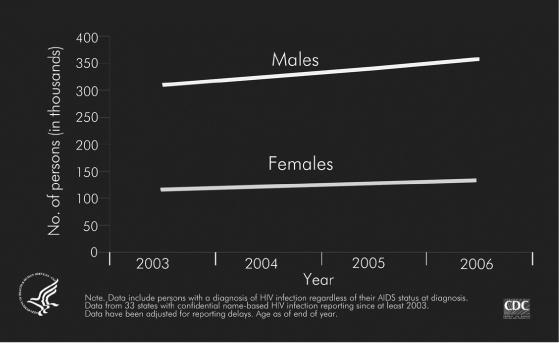
Estimated number of adults and adolescents living with HIV/AIDS, by sex, 2001–2006—33 states.2
Reprinted from: Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. Cases of HIV infection and AIDS in the US and Dependent Areas, 2005 [monograph on the Internet]. Atlanta (GA): US Department of Health and Human Services, Centers for Disease Control and Prevention; 2005, Rev 2007 Jun Vol 17 [cited 2008 Apr 17]. Available from: www.cdc.gov/hiv/topics/surveillance/resources/reports/2005report/default.htm.
Potential explanations for the rising rate in MSM could include complacency among MSM due to the now “chronic disease” nature of HIV, which HAART has enabled,6 substance abuse (particularly methamphetamines), and awareness of HIV-infection status. Indeed, one study found that, adjusted for covariates, there was a hazard ratio of 1.46 (Confidence interval 1.12–1.92) for methamphetamine use and HIV seroconversion.7 The high rate of HIV-infected individuals who do not know their serostatus was the impetus, in 2006, for the CDC to call for universal screening for HIV in the US.8 Whatever the cause, the rise in HIV cases among MSM has concerned public health authorities and HIV activists.
People Of Color
Another statistic that has long caused concern is the disproportionate rate of HIV infection among people of color. As seen in Figure 3, the prevalence rate of infection of African-American males in the US is nearly seven times the rate of Caucasians, whereas the infection rate in Hispanics is more than twice the rate of non-Hispanic white males.2
Figure 3.
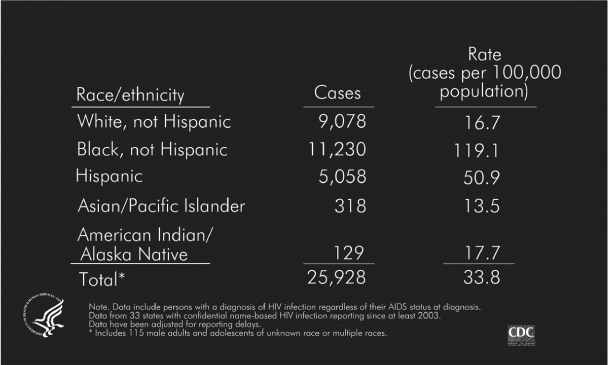
Estimated number of HIV/AIDS cases and rates for male adults and adolescents, by race/ethnicity 2006—33 states
Reprinted from: Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. Cases of HIV infection and AIDS in the US and Dependent Areas, 2005 [monograph on the Internet]. Atlanta (GA): US Department of Health and Human Services, Centers for Disease Control and Prevention; 2005, Rev 2007 Jun Vol 17 [cited 2008 Apr 17]. Available from: www.cdc.gov/hiv/topics/surveillance/resources/reports/2005report/default.htm.
In females, the racial disparity is even more striking, with African-American women having a prevalence rate that is 20 times that of non-Hispanic whites (Figure 4).2 Many hypotheses have been introduced to explain this racial disparity, among them socioeconomic factors and sexual network patterns among African Americans.9
Figure 4.
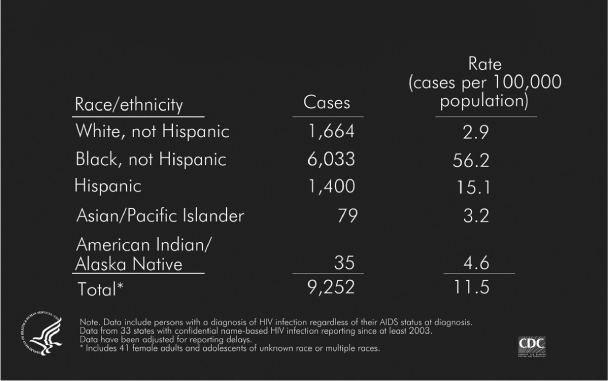
Estimated number of HIV/AIDS cases and rates of female adults and adolescents, by race/ethnicity 2006—33 states
Reprinted from: Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. Cases of HIV infection and AIDS in the US and Dependent Areas, 2005 [monograph on the Internet]. Atlanta (GA): US Department of Health and Human Services, Centers for Disease Control and Prevention; 2005, Rev 2007 Jun Vol 17 [cited 2008 Apr 17]. Available from: www.cdc.gov/hiv/topics/surveillance/resources/reports/2005report/default.htm.
Gender
Among women in the US, the absolute number of AIDS cases has stayed relatively consistent from 1998–2006. However, when looking at all cases of HIV in the US, the proportion of female adults and adolescents (age >13 years) with an AIDS diagnosis increased from 7% in 1985 to 27% in 2006.2
Among females diagnosed with HIV/AIDS in 2006, 80% of HIV/AIDS cases were attributed to high-risk heterosexual contact, 19% to injection drug use and 1% to other or unidentified risk factors.2
Looking at a longer time frame, from 2001 through 2006, an estimated 48,936 AIDS cases that were diagnosed among female adults and adolescents were attributed to either injection drug use or high-risk heterosexual contact. High-risk heterosexual contact accounted for the majority of AIDS cases among females, particularly in the southern states.2 Many of these women live in poverty in rural settings and are not aware of the primary risk behaviors of their male sexual contacts.10 However, the high rate of heterosexual transmission should alert all primary practitioners who care for female patients in the US to obtain a careful sexual history.
Age
Another interesting phenomenon occurring in the HIV epidemic is the gradual aging of the cohort in the US. The CDC has estimated that the number of AIDS cases among patients age 50 years or older increased more than five times between the years 1990 through 2000.11 Before the era of HAART, older age predicted a faster progression to clinical AIDS and death.12 Although data from randomized-controlled trials in this area are lacking, a large retrospective study by the Kaiser Permanente Division of Research recently published showed that older-age patients beginning HAART actually had better virologic responses than younger patients and, despite blunted initial immunologic responses, had similar CD4 T-cell counts after three years of therapy. Higher HAART adherence was advanced as a possible explanation for the improved virologic responses seen in the older group.13 From a long-term perspective, as the HIV population ages, they will be subject to many of the same diseases as the noninfected population. How HIV and HAART will interact with such common diseases such as diabetes, hypertension, and renal insuf-ficiency remains to be seen.
Another area of much concern is the rising rate of AIDS diagnoses in the young adult (ages 20–24 years) population. There has been a steady rise in cases among this age demographic, especially in males.2 Complacency about the disease, substance abuse, and a reduction in person to person communication about HIV may be driving some of this increase.14
Summary
In the more than 20 years since the first case of HIV, the demographics of the disease in the US have changed significantly. Although the mortality rate for HIV has plummeted during the last ten years, the disease remains an important cause of morbidity and mortality. The rate of MSM infection continues to rise and there continues to be marked disparities in the rate of infection by race. As the HIV-infected cohort ages, researchers will continue to explore how HIV interacts with other common conditions seen in the elderly.
After 27 years of the HIV epidemic, it appears that HIV will continue to be a health issue for many years to come. Thus, physicians and clinicians must remain as vigilant as ever for HIV in their practices. Preconceptions about age, gender, ethnicity, or sexual orientation should not deter clinicians from screening for HIV.
Disclosure Statement
The author discloses that he receives research grant support from Tibotec, Pfizer, Merck, Schering-Plough, and Gilead.

“Not Forgotten” photo by Chris Jacobs.
Chris Jacobs is a freelance photographer in Atlanta, GA and a graduate of The Center for Digital Imaging Arts at Boston University in MA. This photograph was taken at the Confederate Cemetery in Marietta, GA. The idea of a soldier whose actions are remembered while his person is forgotten was the inspiration for this photograph.
References
- Centers for Disease Control. Pneumocystits pneumonia-Los Angeles. MMWR Morb Mortal Wkly Resp. 1981 Jun 5;30(21):250–2. [PubMed] [Google Scholar]
- Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, & TB Prevention. Cases of HIV infection and AIDS in the United States and Dependent Areas, 2005 [monograph on the Internet] Atlanta (GA): US Department of Health and Human Services, Centers for Disease Control and Prevention; 2005. Rev 2007 Jun Vol 17 [cited 2008 Apr 17]. Available from: www.cdc.gov/hiv/topics/surveillance/resources/reports/2005report/default.htm. [Google Scholar]
- Gulick RM, Mellors JW, Havlir D, et al. Treatment with indinavir, zidovudine, and lamivudine in adults with human immunodeficiency virus infection and prior antiretroviral therapy. N Engl J Med. 1997 Sep 11;337(11):734–9. doi: 10.1056/NEJM199709113371102. [DOI] [PubMed] [Google Scholar]
- Heffelfinger JD, Swint EB, Berman SM, Weinstock HS. Trends in primary and secondary syphilis among men who have sex with men in the United States. Am J Public Health. 2007 Jun;97(6):1076–83. doi: 10.2105/AJPH.2005.070417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez T, Finlayson T, Drake A, et al. Centers for Disease Control & Prevention Human immunodeficiency virus (HIV) risk, prevention and testing behaviors—United States, National HIV Behavioral Surveillance System: men who have sex with men, November 2003–April 2005. MMWR Surveill Summ. 2006 Jul 7;55(6):1–16. [PubMed] [Google Scholar]
- Kaiser Public Opinion Spotlight. Public opinion on the HIV/AIDS epidemic in the United States [monograph on the Internet] Menlo Park (CA): The Henry J Kaiser Family Foundation; 2006 Aug. [cited 2007 Dec 15]. Available from: www.kff.org/spotlight/hivus/1.cfm. [Google Scholar]
- Plankey M, Ostrow D, Stall R, et al. The relationship between methamphetamine and popper use and risk of HIV seroconversion in the multicenter AIDS cohort study. J Acquir Immune Defic Syndr. 2007 May 1;45(1):85–92. doi: 10.1097/QAI.0b013e3180417c99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branson BM, Handsfield HH, Lampe MA, et al. Centers for Disease Control & Prevention Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006 Sep 22;55(RR-14):1–17. [PubMed] [Google Scholar]
- Hammett T, Drachman-Jones A. HIV/AIDS, sexually transmitted diseases, and incarceration among women: national and southern perspectives. Sex Transm Dis. 2006 Jul;33(7 Suppl):S17–22. doi: 10.1097/01.olq.0000218852.83584.7f. [DOI] [PubMed] [Google Scholar]
- Fleming PL, Lasky A, Lee L, Nakashima AK. The epidemiology of HIV/AIDS in women in the southern United States. Sex Transm Dis. 2006 Jul;33(7 Suppl):S32–8. doi: 10.1097/01.olq.0000221020.13749.de. [DOI] [PubMed] [Google Scholar]
- Mack KA, Ory MG. AIDS and older Americans at the end of the Twentieth Century. J Acquir Immune Defic Syndr. 2003 Jun 1;33(Suppl 2):S68–75. doi: 10.1097/00126334-200306012-00003. [DOI] [PubMed] [Google Scholar]
- Carre N, Deveau C, Belanger F, et al. Effect of age and exposure group on the onset of AIDS in heterosexual and homosexual HIV-infected patients. SEROCO Study Group. AIDS. 1994 Jun;8(6):797–802. doi: 10.1097/00002030-199406000-00012. [DOI] [PubMed] [Google Scholar]
- Silverberg MJ, Leyden W, Horberg MA, DeLorenze GN, Klein D, Quesenberry CP., Jr. Older age and the response to and tolerability of antiretroviral therapy. Arch Intern Med. 2007 Apr 9;167(7):684–91. doi: 10.1001/archinte.167.7.684. [DOI] [PubMed] [Google Scholar]
- Jaffee HW, Valdiserri RO, De Cock K. The reemerging HIV/AIDS epidemic in men who have sex with men. JAMA. 2007 Nov 28;298(20):2412–4. doi: 10.1001/jama.298.20.2412. [DOI] [PubMed] [Google Scholar]


