Abstract
Purpose and Methods
This Phase 1 clinical trial combined qualitative and quantitative methods to modify a collaborative care, telephone based, depression care management intervention for adolescent mothers, and to determine the acceptability, feasibility, and initial efficacy of the intervention in a sample of adolescent mothers (n=97) who were recruited from a Teen Parent Program. Outcomes included measures of depressive symptoms, functioning, and use of mental health services.
Results
Acceptability of the intervention was demonstrated, but feasibility issues related to the complex life challenges confronting the adolescent mother. Although only four adolescent mothers received mental health treatment, there was a trend for improved depressive symptoms over time.
Conclusion
Results of the study provide data for the need of further refinement of the intervention before a large clinical trial is conducted for adolescent mothers with symptoms of depression.
Keywords: Adolescent mothers, depression, telephone
Little attention has been given to postpartum depression in adolescent mothers. This is unfortunate since up to one-half of adolescent mothers experience symptoms of depression in the early postpartum period (Cantilino, Barbosa, & Petribu, 2007; Miller, 1998), with potential long term adverse outcomes on development of both the mother and baby (Field et al, 2005; Riley et al, 2009). Adolescent mothers have described their experience of depression as feeling abandoned and rejected by partners and peers; feeling scared, different, and changed with the reality of motherhood; and questioning and not understanding the experience of depression and what was happening to them (Clemmens, 2002; Eshbaugh, 2006).
Symptoms of depression in adolescent mothers are common throughout the first postpartum year (Reid & Meadows, 2007). Using the CES-D depression screening tool, Logsdon and colleagues screened adolescent mothers for symptoms of depression at 4–6 weeks postpartum and again at 12 months postpartum (Logsdon, Birkimer, Simpson & Looney, 2005; Logsdon, 2008). Forty seven percent of adolescent mothers had significant symptoms of depression at 4–6 weeks postpartum, and the depressive symptoms continued at 12 months postpartum. Of particular concern, by 12 months postpartum no adolescent mothers had pursued referrals for mental health evaluation and treatment (Logsdon, 2008). Barriers to mental health treatment for adolescent mothers include personal barriers (e.g., lack of knowledge of depressive symptoms and depression treatment, life challenges that interfere with attention to mental illness; Logsdon, Hines-Martin & Rakestraw, 2009) and health service barriers (e.g., provider requirement that parental permission and presence is needed before treatment; lack of insurance coverage; National Academy of Sciences, 2008; MBaye & Logsdon, 2005). The intention to seek mental health treatment in adolescent mothers has been predicted by subjective norms, such as a personal experience with mental health treatment, mother’s history of depression and depression treatment, and family facilitation of treatment (Logsdon, Usui, Pinto Foltz & Rakestraw, 2009). Adolescent mothers prefer to discuss depressive symptoms with peers and their romantic partner before talking to a health care provider. Similar to adult women (Hudson-Scholle & Kelleher, 2003; Zittel-Palamara, Rockmaker, Schwabel, Weinstein, & Thompson, 2008), African American adolescent mothers prefer to discuss depressive symptoms with their minister rather than a health care provider (Logsdon et al, 2009; Nadeem, Lange, & Miranda, 2008). Interventions are needed that: 1. Address the specific components of depression that are manifested in adolescent mothers. 2. Engage adolescents into treatment. 3. Result in lower depression and higher functioning. Collaborative care is a promising strategy for overcoming barriers to mental health evaluation and treatment for adolescent mothers.
Collaborative Care
There is strong evidence to document that a collaborative care model that includes a depression care manager (DCM) and psychiatric consultation is an effective mechanism to increase patient adherence to antidepressant medication and improve symptoms of depression, and the improved outcomes are long lasting (Gilbody, Bower, Fletcher, Richards, & Sutton, 2006). The role of the DCM includes educating patients about depression; monitoring depression outcomes, treatment adherence and adverse effects of treatment; and facilitating treatments with primary care and/or mental health providers (Katon, Von Korff, Lin, & Simon, 2001). Including DCM with more expertise in mental health care has been associated with more improvement in depression scores (Gilby et al). The DCM intervention has been successfully delivered by telephone (Katzelnick et al, 2000), but has not been tested with adolescent mothers.
Telephone Interventions
The telephone is recognized as a powerful tool in enhancing depression care (Dietrich, 2000), particularly enhancing rates of psychiatric treatment (Zanjani, Miller, Turiano, Ross, & Oslin, 2008). Building on literature from other chronic conditions (Wasson et al, 1992), the impact of telephone management for the treatment of depression has been documented in several studies. Two investigators identified patients from primary care offices, and used existing nursing staff to serve as care managers (Humkeler et al, 2000; Smith et al, 2000). In the first study, nurse care managers in a California Health Maintenance Organization discussed medication management with patients who were given new prescriptions for antidepressants. In weekly contacts over a six week period, nurses in the second study helped patients who screened positive for depression to identify treatment preferences and address barriers to care. Two additional studies identified patients from HMO data systems and offered care management by health plan staff experienced in mental health or telephone assessment (Katzelnick et al, 2000; Simon et al, 2000). The first study targeted patients with new antidepressant prescriptions and focused primarily on medication treatment. The second study involved screening for depression in high users of general medical visits. Care managers had 2–3 contacts during a 3–4 month period. All four of the studies had improvements in either perceptions of quality of care (Smith et al, 2000), health outcomes (Simon et al, 2000; Humkeler et al, 2000), or both quality of care and health outcomes (Katzelnick et al, 2000).
Currently, Dr. Katherine Wisner is conducting a randomized controlled trial of telephone based depression care management compared to usual care for depression in 462 adult postpartum women (R01MH071825-01A2). After assessing for barriers to treatment and readiness to change, the care manager assists women with choices of depression treatment, encourages them to access their preferred treatment, counsels them to comply with treatment recommendations, and helps them to problem solve if failure to respond occurs. The care manager’s responses to women are scripted in a study manual and are tailored to the woman’s stage of change (precontemplation, contemplation, preparation for action, action and maintenance). The stage of change is determined by information that the patient volunteers and additional questions such as, “It sounds like your symptoms are affecting your life, what do you plan to do about these symptoms?” Both the group receiving the telephone based depression care management and the usual care groups have systematic evaluations at 3, 6, 9, and 12 months.
Though not targeting mental health outcomes, home visits and telephone calls to low-income adolescent mothers by public health nurses have been shown to: improve infant morbidity and school drop out, overcome barriers related to limited time, competing priorities and unreliable transportation, and be acceptable to young women (Koniak Griffin et al, 2000). The evidence for the intensity of the intervention needed to improve perinatal outcomes, i.e., home visits by public health nurses compared to telephone calls, is equivocal (Brooten et al, 1996; Kitzman et al, 1997; Koniak Griffin et al, 2000; Moore & Krowchuck, 1997; Olds et al, 2000; York et al, 1997).
The primary aim of this study was to examine the processes and outcomes (acceptability, feasibility, and preliminary efficacy) associated with revising and testing a collaborative care model of telephone based depression care management in adolescent mothers. With permission, the study revised the telephone based depression care management intervention that was developed by Dr. Katherine Wisner at the University of Pittsburgh for research with adult mothers, as described above.
Intervention Development
A Phase 1 clinical trial (first stage of testing in a small group of participants) and a mixed methods approach (combining qualitative and quantitative research methods) are often used when the efficacy of interventions are tested in a new population (Morse, 2006). Development of effective interventions must be based upon understanding of why individuals might not adhere to intervention protocols or why they might experience barriers to treatment (Morse, 2006). Qualitative research plays an important role in the development of promising interventions, in adapting existing interventions, and in understanding the diversity and complexity of needs and preferences within a population (Van Meijel, Gamel, Van Swieten-Duijfjes & Grypdonck, 2004). Once the intervention has been developed or revised, quantitative methods can be used to evaluate feasibility and efficacy of the intervention.
Methods
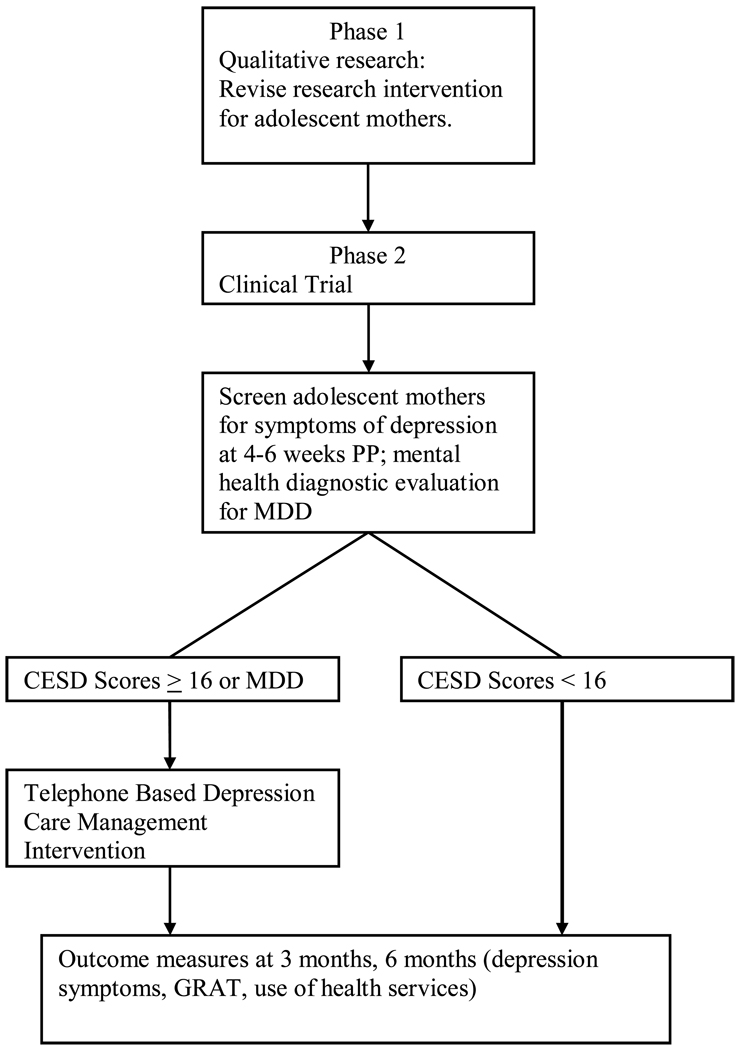
A Phase 1 clinical trial and a mixed method approach were used to modify a telephone based depression care management program that is currently in use with adult postpartum women (Wisner, Scholle, & Stein, 2008) and to evaluate the processes and outcomes associated with implementing the program with adolescent mothers. The study had two distinct phases. Phase one included qualitative methods with the goal of revising the intervention and the research protocol so that it was appropriate for use in adolescent mothers (Sandelowski, 2000). Phase two was a clinical trial to: 1. Screen adolescent mothers for symptoms of depression. 2. Enroll adolescent mothers with significant symptoms of depression or a clinical diagnosis of major depressive disorder in the intervention. 3. Evaluate the impact of the intervention on depressive symptoms, functioning, and use of health services at three months and six months after screening. Verbatim transcripts of audiotaped intervention sessions provided insights into the nature of the interventions as well as participant responses to the interventions and allowed determination of intervention fidelity (Schumacher et al, 2005; Verhoff, Casebeer, & Hilsden, 2002; Whittemore & Grey, 2002).
Phase One: Adaptation of Telephone Based Depression Care Management Intervention
Sample
We utilized the expertise of our Research and Community Advisory Board in adapting the intervention used in this study. The Board consists of fourteen professionals who frequently interact with adolescents or have expertise with adolescents, e.g., adolescent gynecologist; representatives from local Healthy Start Program, a Department of Health and Human Services funded program for low income pregnant women and their families; Medical Director of public school based teen parent program; Director of local Teen Pregnancy Prevention Program; Director of Adolescent Programs for public funded mental health care; representatives from faith based organizations; representative from Office of Youth Programs in city government; Director of Residential Foster Care Program for adolescent girls; Field Representative for elected official; Community Affairs Coordinator for local Medicaid program.
Procedures
Board members evaluated the telephone based depression care management manual used by Dr. Katherine Wisner at the University of Pittsburgh for her screening and telephone based DCM program with adult postpartum women. Board members provided written and oral feedback on how the manual should be revised for use with adolescent mothers. They also reviewed a packet of education materials on adolescent depression from the American Academy of Pediatrics, The Society for Adolescent Medicine, and the National Institute of Mental Health. Reading levels of materials were evaluated, in addition to content.
Interview Guide
In two focus groups, the Board discussed the following questions which were developed from literature on adolescent development (e.g., Erikson, 1959) and family intervention (Josephson, 2008): 1. How might power differential impact building a relationship between the Depression Care Manager and the adolescent mother? 2. What is the impact of cognitive and emotional development of the adolescent on recommended self management strategies? 3. How could lack of emancipation for decision making related to mental health services impact potential self management strategies? 4 What is the impact of the young woman’s family dynamics on her depression self management strategies?
Data Analysis
Field notes were recorded and transcribed by two research assistants. Both conversation and expressions were included. Open coding was undertaken through line by line analysis of interview transcripts and the development of descriptive labels for responses to each question in the interview guide. Thematic analysis was performed to identify common threads. Consensus of findings was reached by the first author and the two research team members. Two Board members provided feedback on the summary to provide further credibility of the findings (Lincoln & Guba, 1985).
Results
Themes that were identified from the data included the following: disappointment with relationships with father of baby, conflicted family relationships, primary role of adolescent’s mother and dependence on mother, straddling the fence between childhood and adulthood.
Discussion
The New Mother Program, a telephone based depression care management intervention for adolescent mothers, was developed as an outcome of Phase 1. Specifically, adaptation of the intervention included strategies to overcome barriers to treatment related to relationship and self esteem concerns, education of family members about her depression if requested by the adolescent, age appropriate depression education and professional support to indicate respect for attitudes and behaviors that are typical of adolescents. Specific content of the intervention is described in Table 1.
Table 1.
Description of DCM Intervention
|
Phase Two: Testing Intervention
Sample and Procedures
Over a twelve month time period, a convenience sample of adolescent mothers (n=97) who attended the Teenage Parent Program in a southern, urban area of the United States was screened at four to six weeks postpartum for symptoms of depression and functional status. Inclusion criteria included the following: delivery of a live child within the last 4–6 weeks, English speaking, primiparas, 13–18 years of age, able to provide assent and informed consent of parent/guardian, and baby lives with adolescent mother. Screening was repeated at 3 and 6 months after the baseline measure. Screening occurred at the school or a community location of the adolescent mother’s choice, such as her home. In addition, Independent Evaluators completed mental health diagnostic evaluations at baseline. The evaluators were psychiatric clinical nurse specialists or psychologists, and they were blind to study aims and depression status of the participants. After the baseline screening and evaluation, adolescent mothers with symptoms of depression (CES-D scores greater than or equal to 16) as well as those with DSM-IV diagnosis of major depressive disorder were enrolled in the intervention in order that results of the study could be generalized to community samples where psychiatric experts may not be available for mental health diagnostic evaluations. See Figure 1.
Figure 1.
New Mother Program Telephone Based DCM Intervention
The purpose of the intervention was to assist adolescent mothers to overcome barriers to mental health evaluation and/or treatment. The DCM did not provide therapy. Adolescent mothers were enrolled in the intervention for six months. Although the length of the study was shorter, the dose of the intervention followed the template created by Dr Wisner at the University of Pittsburgh (study with adult postpartum women that we were replicating) and was as follows: weekly calls of 15–20 minutes each for the first four weeks; calls every two weeks for two months lasting 10 minutes each; monthly calls for two months lasting 10 minutes each. Each participant received eleven interactions over six months.
The intervention was framed by the trans-theoretical model (TTM; Prochaska & Velicer, 1997), a theory to explain intentional behavioral change. Manualized responses by the DCM to the adolescent mother were based upon which stage of change the adolescent mother exhibited, e.g., precontemplation, contemplation, preparation, action, maintenance, and termination. Adolescent development theory (Erikson, 1959) and principles of family intervention (Josephson, 2008) also guided manualized responses by the DCM. The DCM utilized motivational interviewing, a method of communication that focuses on a person’s intrinsic motivation to change behavior (Miller & Rollnick, 2002). The focus was on collaboration between DCM and adolescent mother. The DCM affirms the client’s right to change and her capacity to be self-directed, as well as expressing empathy and supporting the client’s self efficacy. See Table 1 for content of intervention.
Training of Depression Care Manager
The DCM received thirty hours of training which included use of the New Mother Program manual, didactic materials on postpartum depression in adolescent mothers, telephone based interventions and role play. The DCM was an experienced child/adolescent psychiatric clinical nurse specialist with extensive knowledge of psychiatric services for adolescents in the community and other community resources.
Intervention Fidelity
All telephone interventions were audiotaped. An expert on intervention fidelity served as a consultant to the study and developed a fidelity rating scale, based on the New Mother Program manual. Ten percent of the interventions were evaluated by two independent raters for fidelity. Results were used as training vehicle for the DCM after the first month of the study.
Treatment of Depression
Our research team included a child adolescent psychiatrist who leads a psychiatric treatment facility, and is an expert in family intervention (Josephson, 2008). He was available for consultation and facilitation of any treatment issues. He also provided guidance to the research team and the data collection site related to procedures to be used if research participants expressed thoughts of harm to self or others.
Study Measures
Mental Health Diagnostic Evaluation
The Schedule for Affective Disorders and Schizophrenia for School Age Children-Present and Lifetime Version (K-SADS-PL) is a clinical interview that incorporates DSM-IV diagnoses (Kaufman et al, 1997). The KSADS-PL takes 45–90 minutes to complete and is the gold standard for diagnosis of depression in adolescents.
Outcome Measures
Center for Epidemiologic Studies of Depression (CES-D)
CES-D instrument was developed for use in the general population to screen for evidence of depression and has high sensitivity and specificity in adolescents (Garrison, et al., 1991; Roberts et al., 1991), including ethnic minority adolescents (Prescott et al., 1998). The CES-D depression instrument is a 20-item instrument with possible responses ranging from 0 (rarely) to 3 (most of the time). Four of the items are reversed coded. Average total scores range from 7.8 to 9.9 (Radloff & Locke, 1986), with a score of 16 or higher indicating evidence of depression. Researchers using the CES-D in samples of pregnant and postpartum women have reported means from 8.5 to 18.7 for pregnant women and 5.3 to 14.4 for postpartum women (Logsdon et al., 1996). Evidence of content, concurrent, and discriminate validity of the CES-D has been demonstrated (Weissman et al., 1977), and high internal consistency reliability has been reported in pregnant and postpartum women (Logsdon, 2002), including samples of young pregnant and parenting women (13–17 years of age) (Wilcox et al., 1998; Logsdon, et al., 2004). The CES-D has great utility as a screening instrument (Myers & Winters, 2002). Recent research suggests stability in CES-D scores over the first year postpartum and that CES-D scores are related to depression diagnostic status (Beeghly et al., 2002, 2003).
Children’s Global Assessment Scale (CGAS)
The Children’s Global Assessment Scale (CGAS) is a measure developed by Schaffer and colleagues at the Department of Psychiatry, Columbia University to provide a global measure of level of functioning in children and adolescents. The measure provides a single global rating only, on scale of 0–100. In making their rating, the independent evaluator will make use of the glossary details to determine the meaning of the points on the scale (Schaffer et al., 1983).
Gratification in the Maternal Role (GRAT)
The GRAT is a 14-item checklist in which postpartum women rate the extent that each item is true for them on a 5 point scale from 1 = not at all to 5 = very much, with 3 representing somewhat. Examples of statements include "pride in my baby’s development.” GRAT was derived by content analysis of interview data in which parents described sources of satisfaction and rewards in the parenting role (content validity). The split half reliability was .93 (Russell, 1974). The scale was revised by Mercer (1985) who reported Chronbach alpha reliabilities or .80 at 1 month, .78 at 8 months, and .77 at 12 months. Other researchers have reported internal consistency reliabilities of .79 to .85 (Killien, 1998; Panzarine, Slater, & Sharps, 1995). The instrument has been used with adult and adolescent postpartum mothers of term infants. In a longitudinal study of 142 postpartum women, Killien (1998) found lower GRAT scores in depressed women. Panzarine et al (1995) found lower GRAT scores to be related to depression in a sample of 50 primiparous adolescents at six months postpartum.
Use of Mental Health Services
We obtained data from subjects at baseline, 3 months and 6 months on depression visits (defined as visits with primary care or mental health clinician in which depression was discussed or treatment provided). Adolescent mothers reported the number of visits to emergency department, the number of hospitalizations and hospital days, and any mental health counseling visits. Consent procedures included permission to obtain medical records from mental health providers to corroborate self report data. Adequacy of depression care was measured using procedures reported in other studies (Smith et al., 2000): psychotropic medication at minimum therapeutic guideline-concordant daily doses for at least 3 months, adequate follow-up of antidepressant medication defined as at least 3 visits during the six months following the initial prescription; an adequate trial of psychotherapy, defined as at least 8 visits to mental health specialist during a six-month period.
Results of Phase Two
The study was funded for 12 months, thus data were collected over a year time period. Ninety seven adolescent mothers were screened for symptoms of depression at 4–6 weeks postpartum. Four additional adolescent mothers refused to be screened due to lack of interest in the study. Forty five and twenty adolescents were evaluated at 3 and 6 months postpartum, respectively. The average participant was 16 years of age (M=16.44; SD=1.26), Caucasian (44%) or African American (42%), enrolled in the 10th grade (M=9.72, SD=1.22), unmarried, lived with her mother (22%), and did not work outside the home.
From the KSAD-P diagnostic evaluations, 10 participants were diagnosed with Major Depressive Disorder. Twenty-two participants had CES-D scores indicating significant symptoms of depression. CES-D scores ranged from 5 to 40. Note: Either a KSAD-P diagnosis of MDD or significant symptoms of depression on the CES-D were criteria for enrollment in the intervention.
Feasibility of the Intervention
Twenty two adolescent mothers were referred into the intervention, and 13 completed all 11 calls of the intervention. Five other adolescent mothers completed 2–9 calls due to the following reasons: the study ended before the calls could be completed (2), felt they no longer needed intervention (1), lost access to telephone (2). The other four participants provided assent and parental consent but were never able to be contacted by telephone. Thus, the attrition rate was 30%. The DCM made 327 attempts to reach the adolescent mothers, and she was successful in connecting with the adolescents to deliver the intervention 176 times.
From the narrative comments recorded by the DCM, the adolescent mothers reported many life challenges including personal illness, baby illness, unstable living arrangements, inadequate finances, and lack of supportive relationships. These challenges impacted their abilities to participate in the New Mother Program intervention. For example, one adolescent mother had gallbladder surgery and another suffered from insomnia. One baby had severe anemia, and several infants had other chronic conditions that required frequent visits to health care providers. One adolescent mother moved to another state and back twice. Though five telephone numbers were collected for each participant, several adolescent mothers had disconnected phones and were difficult to reach on alternate phone numbers. Several of the adolescent mothers worked in fast food restaurants, attended school full time, and were the primary care givers of their infants; thus time constraints created challenges for study participation. One adolescent mother was physically abused by her romantic partner. Another adolescent mother was stressed because her father and boyfriend were in prison. Most adolescent mothers depended upon their own mothers for financial support, transportation, and child care.
Despite high scores on depression screening tools and referrals for mental health diagnostic evaluation and treatment, many adolescent mothers saw their symptoms as due to “normal life issues” and perceived that “all new moms feel this way.” One adolescent mother stated that she was “not crazy” and did not need mental health treatment and would “just get through it.”
Acceptability of the Intervention
At the conclusion of the study, the adolescent mothers who received the New Mother Program intervention were interviewed by the Research Project Manager about their satisfaction with their experience in the study. Five adolescent mothers were able to be reached and responded to the satisfaction survey. Mean scores indicate that adolescent mothers found the New Mother Program intervention to be helpful, and they were satisfied with the intervention. Narrative comments indicated that the adolescents appreciated the attention, insights and the information from the Depression Care Manager. See Table 2.
Table 2.
Questions and Narrative Comments Related to Acceptability of Intervention
| On a scale of 1 to 3 (1=not helpful; 2=somewhat helpful; 3=very helpful) please tell me your satisfaction with your experience of receiving telephone intervention from nurse. | |
|---|---|
| Questions | Narrative Comments |
| 1. How helpful was the telephone based intervention? Mean score=2.2 |
Gave insight to me on things that could help me that I didn’t know about. |
|
I have someone to talk to and didn’t have to be embarrassed because she understood what you going through because she works with people like you. | |
| 2. Are you satisfied with the telephone based intervention? Mean score=2.6 |
2. Very interesting. If I was in the situation that I needed help for depression, the help was there. |
| 3. What did you like about the intervention? | 3. Getting advice from the nurse. |
|
Check up on you. | |
|
Someone to check how you are doing. | |
|
Tell me how happy they were for how well you are doing. | |
|
Somebody to talk to. Was satisfied | |
| 4. What do you recommend that we change in order to better help young mothers like you? | 4. Have somebody available to call all the time. |
| Satisfied with the intervention. | |
| Don’t call so late/Call late at night. | |
In addition, adolescent mothers described personal characteristics of the DCM using an investigator developed rating scale. The DCM received high scores for being comforting, positive, informative, personal, caring, supportive, a good listener, and respectful. The scores were slightly lower for aware of your feelings and able to offer hope. However, there were high scores for “she understands me.”
Efficacy of the Intervention
Data were analyzed by descriptive statistics, and the baseline and longitudinal scores for the intervention and non-intervention groups were compared using independent samples t-tests. Depression scores were higher and functioning scores were lower for the adolescents in the intervention group at baseline, but their depression scores improved over time to approach the non-depressed group by time 3 (six months postpartum). Interestingly, there were no differences in gratification in the maternal role by intervention group. See Table 3. Mean scores for use of health services across time were low in both the intervention and non intervention groups, though the intervention group had more visits overall. See Table 4.
Table 3.
Measures of Depression Symptoms and Functioning in Intervention and Non Intervention Groups
| Instrument | Intervention Status |
Time 1 | Time 2 | Time 3 |
|---|---|---|---|---|
| CES-D (Depression) | ||||
| I | M = 24.04 | M =14.14 | M = 5.00 | |
| Not I | M = 10.38 | M = 8.45 | M = 4.75 | |
| t =−8.49, p =.00 | t =−2.80, p =.00 | t =−.19, p =.85 | ||
| GRAT (Functioning) | ||||
| I | M = 57.29 | M = 56.57 | M = 59.87 | |
| Not I | M = 59.83 | M = 58.70 | M = 64 | |
| t =1.59, p =.11 | t =.910, p =.368 | t =1.49, p =.15 | ||
| CGAS (Functioning) | ||||
| I | M = 72.18 | |||
| Not I | M = 80.36 | |||
| t =3.94, p =.00 |
Note: I=Enrolled in New Mother Program, telephone based depression care management
Not I=Not enrolled in intervention
Table 4.
Use of Mental Health Services Across Time
| I | I | II | II | III | III | |
|---|---|---|---|---|---|---|
| Variable | Not In Intervention |
In Intervention |
Not In Intervention |
In Intervention |
Not In Intervention |
In Intervention |
| Average nights in a hospital or other treatment facility for treatment of physical problems | 3.34 | 3.35 | 0.97 | 1.21 | 1.38 | 0.00 |
| Average nights in a hospital of other treatment facility for any personal or emotional problems | 0.09 | 0.39 | 0.00 | 0.00 | 0.00 | 0.00 |
| Average visits to hospital emergency room | 1.56 | 2.70 | 0.16 | 0.71 | 0.63 | 0.00 |
| Average visits to medical providers | 10.91 | 13.61 | 1.19 | 3.07 | 1.00 | 1.00 |
| Average visits in which discussed personal or emotional problems such as emotions, nerves, alcohol, drugs, or mental health | 0.82 | 2.09 | 0.16 | 0.86 | 0.00 | 0.57 |
| Average visits to psychiatrists, psychologists, social workers, psychiatric nurses or counselors | 1.96 | 5.65 | 0.23 | 0.43 | 0.25 | 2.57 |
For the four adolescent mothers who received mental health treatment, there were 20 total visits to health care providers. Three adolescent mothers received both therapy and medications, and one adolescent mother received medication only. The medications included Zoloft (Sertaline) and Lexapro at recommended doses. The number and character of interventions were lower than a priori description of adequate depression care for each participant. As would be expected with this treatment history, the mean depression scores did not change over time for these four adolescents (Mean = 28.10 at each time period).
Discussion
The purposes of this Phase 1 clinical trial were to revise a collaborative care, telephone based depression care management intervention so that it was appropriate for adolescent mothers, and then to evaluate the processes and outcomes associated with the reaction of the adolescent mothers to the intervention in terms of feasibility, acceptability, and initial efficacy. Results of the study demonstrated the acceptability of the New Mother Program, telephone based depression care management, to adolescent mothers. However, the small number of adolescent mothers who could be reached to provide this feedback is a limitation.
The feasibility of the current program should be reevaluated. The DCM was only able to reach the adolescent mothers 53% of the time when she called. The DCM worked flexible hours and asked each adolescent mother for her call time preferences at the first contact. However, the financial instability of the adolescent mothers impacted their access to telephones and created limited time to talk to the DCM as many balanced work, school, and baby care. Based upon the adolescent mother’s stage of change, the DCM provided education about symptoms of depression and the importance of evaluation and treatment. The DCM facilitated involvement of the adolescent’s family, as requested. However, the culture in which the adolescent mother lives (Logsdon et al, 2009) and her peers may exert such a strong influence that she cannot see herself taking steps to seek treatment (Sword et al, 2008). Perhaps a public marketing campaign for adolescent mothers that applies a branding strategy related to seeking health care for depression would be an effective approach to overcoming this barrier (Evans & Hastings, 2008). This approach has been used successfully with adolescents for health promotion issues (Asbury, Wong, Price, & Nolin, 2008).
In terms of initial efficacy, depression scores for the adolescent mothers in the intervention group improved from baseline. The results are in stark contrast to an earlier research study from the same population in which depression scores at 4–6 weeks postpartum did not improve over time (Logsdon et al, 2005; Logsdon, 2008). However, without use of a control group, results must be viewed cautiously and threats to validity considered. It is possible that improvement in scores could be due to a Hawthorne effect or testing effects. Characteristics of the sample may have impacted study findings. For example, the primarily low-income adolescent mothers who attend the Teenage Parent Program in one city in the southern United States may have unique characteristics that impact the study results. Alternately, contact with the DCM could have provided sufficient professional support to improve depression symptoms and functioning.
This community based Phase 1 trial has several strengths. This is the first study to systematically adapt a manualized depression care management intervention so that it is specific to adolescent mothers, using rigorous qualitative methods and guidance from a Community Research Advisory Board. Rigor in quantitative research methods included creation of a fidelity measure that was used in training of the DCM as well as use of instruments with strong psychometric properties in the population. In addition, the study was longitudinal and allows calculation of attrition rates that can be used in planning further research studies.
The findings of this study offer insight into the need for refinement of the intervention before initiating a randomized clinical trial. A small percentage of adolescent mothers followed recommendations for diagnostic evaluation and treatment. It is important to continue to explore strategies for how to engage low income adolescent mothers into behavioral health evaluation and treatment (Shanok, 1997). Is the telephone the best delivery model? Could the intervention be more effectively delivered by use of social networking strategies? Are professionals the best source of support? The DCM was a middle aged woman. Does age of the professional impact the adolescent mother’s willingness to engage in the intervention? How can subjective norms be addressed? Although the intervention included interaction with the adolescent’s mother, (with the adolescent’s permission), perhaps further research should consider focusing the intervention on the mother daughter dyad. Other family interventions may also be indicated due to conflicted relationships. Family therapy may help the adolescent to develop self efficacy by reconnecting to her family in appropriate ways (Josephson, 2008). As these questions are answered in further research, outcomes can be used in the development of interventions that can be integrated into existing maternity and clinical services (Lumley, Austin, & Mitchell, 2004).
Acknowledgement
This Phase 1 clinical trial to study issues related to access to mental health treatment for adolescent mothers was funded by the Improved Health Outcome Program, Passport Health Services/University Hospital Foundation. The authors express appreciation to Dr. Katherine Wisner for permission to use her Depression Care Management intervention and to revise the intervention for use with adolescent mothers.
Contributor Information
M. Cynthia Logsdon, Professor, School of Nursing, Professor, Department of Obstetrics & Gynecology, School of Medicine, Associate Faculty, Department of Psychological & Brain Sciences, University of Louisville, Louisville, Kentucky, 502-852-5825 Office Phone, 502-852-8783 FAX, mclogs01@gwise.louisville.edu.
Melissa D. Pinto-Foltz, KL2 Scholar, Multidisciplinary Clinical Research Training Program, Case Western Reserve University/Cleveland Clinic, Instructor, Frances Payne Bolton School of Nursing, Case Western Reserve University, Cleveland, Ohio.
Bradley Stein, Associate Professor, Department of Psychiatry, University of Pittsburgh School of Medicine, Adjunct Natural Scientist, RAND Corporation, Pittsburgh, PA.
Wayne Usui, Professor, Department of Sociology, University of Louisville, Louisville, Kentucky.
Allan Josephson, Professor and Associate Chair for Child & Adolescent Psychiatric Services, Division Chief, Adolescent & Family Psychiatry, Department of Psychiatry & Behavioral Sciences, School of Medicine, Chief Executive Officer, Bingham Child Guidance Center, University of Louisville, Louisville, Kentucky.
References
- Asbury LD, Wong FL, Price SM, Nolin MJ. The VERB campaign: Applying a branding strategy in public health. American Journal of Preventive Medicine. 2008;34:183–187. doi: 10.1016/j.amepre.2008.03.010. [DOI] [PubMed] [Google Scholar]
- Beeghly M, Olsen K, Weinberg M, Pierre S, Downey N, Tronick E. Prevalence, stability, and sociodemographic correlates of depressive symptoms in Black mothers during the first 18 months postpartum. Maternal and Child Health Journal. 2003;7:157–167. doi: 10.1023/a:1025132320321. [DOI] [PubMed] [Google Scholar]
- Brooten D, Kumar S, Brown LP, Butts P, Finkler SA, Bakewell-Sachs S, et al. A randomized clinical trial of early hospital discharge and home follow up of very low birth weight infants. New England Journal of Medicine. 1986;315:934–939. doi: 10.1056/NEJM198610093151505. [DOI] [PubMed] [Google Scholar]
- Cantilino A, Barbosa EM, Petribu K. Postpartum depression in adolescents in Brazil: An issue of concern. Archives of Women’s Mental Health. 2007;10(6):1434–1816. doi: 10.1007/s00737-007-0206-8. [DOI] [PubMed] [Google Scholar]
- Clemmens D. Adolescent mothers' depression after the birth of their babies: Weathering the storm. Adolescence. 2002;37:551–565. [PubMed] [Google Scholar]
- Dietrich AJ. The telephone as a new weapon in the battle against depression. [Retrieved April 10, 2009];2000 from http://www.acponline.org. [PubMed] [Google Scholar]
- Erikson EH. Identity and the life cycle. New York: International Universities Press; 1959. [Google Scholar]
- Eshbaugh EM. Predictors of depressive symptomology among low-income Adolescent mothers. Archives of Women’s Mental Health. 2006;9:339–342. doi: 10.1007/s00737-006-0146-8. [DOI] [PubMed] [Google Scholar]
- Evans WD, Hastings G. Public health branding: Applying marketing for social change. London, UK: Oxford University Press; 2008. [Google Scholar]
- Field T, Hernandez-Reif M, Vera Y, Gil K, Diego M, Sanders C. Infants of depressed mothers facing a mirror versus their mother. Infant Behavior and Development. 2005;28:48–53. [Google Scholar]
- Garrison CZ, Addy A, Jackson KL, McKeown R, Waller JL. The CES-D as a screen for depression and other psychiatric disorders in adolescents. J Am Acad Child Adolesc Psychiatry. 1991;30:636–641. doi: 10.1097/00004583-199107000-00017. [DOI] [PubMed] [Google Scholar]
- Gilbody S, Bower P, Fletcher J, Richards D, Sutton AJ. Collaborative care for depression: A cumulative meta-analysis and review of longer term outcomes. Archives of Internal Medicine. 2006;166:2314–2321. doi: 10.1001/archinte.166.21.2314. [DOI] [PubMed] [Google Scholar]
- Hudson-Scholle S, Kelleher K. Preferences for depression advice among low-income income women. Maternal and Child Health Journal. 2003;7(2):1573–6628. doi: 10.1023/a:1023864810207. [DOI] [PubMed] [Google Scholar]
- Hunkeler EM, Meresman JF, Hargreaves WA, Fireman B, Berman WH, Kirsch AJ, et al. Efficacy of nurse telehealth care and peer support in augmenting treatment of depression in primary care. Archives of Family Medicine. 2000;9:700–708. doi: 10.1001/archfami.9.8.700. [DOI] [PubMed] [Google Scholar]
- Josephson AM. Reinventing family therapy: Teaching family intervention as a new treatment modality. Academic Psychiatry. 2008;32:405–413. doi: 10.1176/appi.ap.32.5.405. [DOI] [PubMed] [Google Scholar]
- Katon W, von Korff M, Lin E, Simon G. Rethinking practitioner roles in chronic illness: The specialist, primary care physician, and the practice nurse. General Hospital Psychiatry. 2001;23:138–144. doi: 10.1016/s0163-8343(01)00136-0. [DOI] [PubMed] [Google Scholar]
- Katzelnick DJ, Simon GE, Pearson SD, Manning WG, Helstad CP, Henk HJ, et al. Randomized trial of a depression management program in high utilizers of medical care. Archives of Family Medicine. 2000;9:345–351. doi: 10.1001/archfami.9.4.345. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for affective disorders and schizophrenia for school age children-present and lifetime version: Initial reliability and validity data. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:980–981. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Killeen J. Postpartum return to work: Maternal stress, anxiety, and gratification. Canadian Journal of Nursing Research. 1998;30:50–63. [PubMed] [Google Scholar]
- Kitzman H, Olds DL, Henderson CR, Jr, Hanks C, Cole R, Tatelbaum R, et al. Effect of prenatal and infancy home visitation by nurses on pregnancy outcomes, childhood injuries, and repeated childbearing: A randomized clinical trial. Journal of the American Medical Association. 1997;278:644–652. [PubMed] [Google Scholar]
- Koniak Griffin D, Anderson N, Verzmenieks I, Brecht M. A public health nursing early intervention program for adolescent mothers: Outcomes from pregnancy through six weeks postpartum. Nursing Research. 2000;49:130–138. doi: 10.1097/00006199-200005000-00003. [DOI] [PubMed] [Google Scholar]
- Lincoln Y, Guba E. Naturalistic Inquiry. Newbury Park, Ca: Sage; 1985. [Google Scholar]
- Logsdon MC. The postpartum support questionnaire. In: Strickland OL, Dilorio C, editors. Measurement of Nursing Outcomes. 2nd ed. New York: Springer; 2002. pp. 199–215. [Google Scholar]
- Logsdon MC. Maternal role functioning in adolescents at 12 months postpartum. Women’s Health Care: A Practical Guide for Nurse Practitioners. 2008;7:27–32. [Google Scholar]
- Logsdon MC, Birkimer JC, Simpson T, Looney S. Postpartum depression and social support in adolescents. Journal of Obstetrics, Gynecology, and Neonatal Nursing. 2005;34:46–54. doi: 10.1177/0884217504272802. [DOI] [PubMed] [Google Scholar]
- Logsdon MC, Cross R, Williams B, Simpson T. Prediction of postpartum social support and symptoms of depression in pregnant adolescents: A pilot study. Journal of School Nursing. 2004;20:36–42. doi: 10.1177/10598405040200010701. [DOI] [PubMed] [Google Scholar]
- Logsdon MC, Hines Martin V, Rakestraw V. Barriers to depression treatment in low-income, unmarried, adolescent mothers in a southern, urban area of the United States. Issues in Mental Health Nursing. 2009 doi: 10.1080/01612840902722187. In press. [DOI] [PubMed] [Google Scholar]
- Logsdon MC, Usui W, Birkimer J, McBride AB. The postpartum support questionnaire: Reliability and validity. Journal of Nursing Measurement. 1996;4:129–142. [PubMed] [Google Scholar]
- Logsdon MC, Usui W, Pinto Foltz M, Rakestraw V. Intention to seek mental health treatment in adolescent mothers and a comparison group of adolescent girls. Archives of Psychiatric Nursing. 2009;23:41–49. doi: 10.1016/j.apnu.2008.02.013. [DOI] [PubMed] [Google Scholar]
- Lumley J, Austin M, Mitchell C. Intervening to reduce depression after birth: A systematic review of the randomized trials. International Journal of Technology Assessment in Health Care. 2004;20:128–144. doi: 10.1017/s0266462304000911. [DOI] [PubMed] [Google Scholar]
- MBaye A, Logsdon MC. Barriers to mental health service use by childbearing adolescents in MetroLouisville : Provider and system barriers. Research poster presented at the University of Louisville Undergraduate Research Poster Day; April 2004; Louisville, Kentucky. 2004. [Google Scholar]
- Mercer RT. The process of maternal role attainment over the first year. Western Journal of Nursing. 1985;34(4):198–204. [PubMed] [Google Scholar]
- Miller L. Depression among pregnant adolescents. Psychiatric Services. 1998;49:970. doi: 10.1176/ps.49.7.970. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational inteviewing: Preparing people for change. New York: Guilford Press; 2002. [Google Scholar]
- Moore M, Krowchuck H. Parent line: Nurse telephone intervention for parents and caregivers of children from birth through age five. Journal of the Society of Pediatric Nurses. 1997;2:179–184. doi: 10.1111/j.1744-6155.1997.tb00022.x. [DOI] [PubMed] [Google Scholar]
- Morse JM. The scope of qualitatively derived clinical interventions. Qualitative Health Research. 2006;16:591–593. doi: 10.1177/1049732306286908. [DOI] [PubMed] [Google Scholar]
- Myers K, Winters NC. Ten year review of rating scales: Scales for internalizing disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:634–659. doi: 10.1097/00004583-200206000-00004. [DOI] [PubMed] [Google Scholar]
- Nadeem E, Lange JM, Miranda J. Mental health care preferences among low-income and minority women. Archives of Women’s Mental Health. 2008;11(2):1434–1816. doi: 10.1007/s00737-008-0002-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academy of Sciences. Committee on Adolescent Health Care Services and Models of Care for Treatment, Prevention, and Health Development, National Research Council. [Retrieved April 8, 2009];Adolescent health services: Missing opportunities. 2008 from http://www.nap.edu.
- Olds D, Hill P, Robinson J, Song N, Little C. Update on home visiting for pregnant women and parents of young children. Current Problems in Pediatrics. 2000;30:107–141. doi: 10.1067/mps.2000.105091. [DOI] [PubMed] [Google Scholar]
- Panzarine S, Slater E, Sharps P. Coping, social support, and depressive symptoms in adolescent mothers. Journal of Adolescent Health. 1995;17(2):113–119. doi: 10.1016/1054-139X(95)00064-Y. [DOI] [PubMed] [Google Scholar]
- Prescott CA, McArdle JJ, Hishinuma ES, Johnson RC, Miyamoto RH, Andrade NN, et al. Prediction of major depression and dysthymia from CES-D scores among ethnic minority adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;37:495–503. doi: 10.1097/00004583-199805000-00012. [DOI] [PubMed] [Google Scholar]
- Prochaska J, Velicer WF. Misinterpretations and misapplications of transtheoretical model. American Journal of Health Promotion. 1997;12:11–12. doi: 10.4278/0890-1171-12.1.11. [DOI] [PubMed] [Google Scholar]
- Radloff LS, Locke BZ. The community mental health assessment survey and the CES-D scale. In: Weissmann MM, Myers JK, Ross CE, editors. Community Surveys of Psychiatric Disorders. New Brunswick, NJ: Rutgers University Press; 1986. pp. 177–189. [Google Scholar]
- Reid V, Meadows-Oliver M. Postpartum depression in adolescent mothers: an integrative review of the literature. Journal of Pediatric Health Care. 2007;21(5):289–298. doi: 10.1016/j.pedhc.2006.05.010. [DOI] [PubMed] [Google Scholar]
- Riley AW, Coiro MJ, Broitman M, Colantuoni E, Hurley KM, Bandeen-Roche K, Miranda J. Mental health of children of low-income depressed Mothers: Influences of parenting, family environment, and raters. Psychiatric Services. 2009;60 doi: 10.1176/appi.ps.60.3.329. 329.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts RE, Lewinsohn PM, Seeley JR. Screening for adolescent depression: A comparison of depression scales. Journal of American Academy of Adolescent Psychiatry. 1991;30:58–66. doi: 10.1097/00004583-199101000-00009. [DOI] [PubMed] [Google Scholar]
- Russell CS. Transition to parenthood: Problems and gratifications. Journal of Marriage and the Family. 1974;102:295. [Google Scholar]
- Sandelowski M. Obtaining qualitative and quantitative sampling, data collection, and analysis techniques in mixed methods studies. Research in Nursing & Health. 2000;23:246–255. doi: 10.1002/1098-240x(200006)23:3<246::aid-nur9>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- Schaffer D, Gould M, Brasic J, Ambrosini P, Fisher P, Bird H, et al. A children's global assessment scale (CGAS) Archives of General Psychiatry. 1983;40(11):1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- Schumacher KL, Koresawa S, West C, Dodd M, Paul SM, Tripathy D, Koo P, Miaskowski C. Qualitative research contribution to a randomized clinical trial. Research in Nursing & Health. 2005;28:268–280. doi: 10.1002/nur.20080. [DOI] [PubMed] [Google Scholar]
- Shanok AF. Depression and treatment with inner city pregnant and parenting teens. Archives of Women’s Mental Health. 2007;10:199–210. doi: 10.1007/s00737-007-0194-8. [DOI] [PubMed] [Google Scholar]
- Simon GE, VonKorff M, Rutter C, Wagner E. Randomized trial of monitoring, feedback, and management of care by telephone to improve treatment of depression in primary care. British Medical Journal. 2000;320:550–554. doi: 10.1136/bmj.320.7234.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith J, et al. A primary care intervention for depression. The Journal of Rural Health. 2000;16:313–323. doi: 10.1111/j.1748-0361.2000.tb00482.x. [DOI] [PubMed] [Google Scholar]
- Sword W, Busser D, Ganann R, McMillan T, Swinton M. Women’s care-seeking experiences after referral for post-partum depression. Qualitative Health Research. 2008;18(9):1161–1173. doi: 10.1177/1049732308321736. [DOI] [PubMed] [Google Scholar]
- Van Meijel B, Gamel C, Van Swieten-Duijfjes B, Grypdonck M. The development of evidence based nursing interventions. Journal of Advanced Nursing. 2004;48:84–92. doi: 10.1111/j.1365-2648.2004.03171.x. [DOI] [PubMed] [Google Scholar]
- Verhoff MJ, Casebeer AL, Hilsden RJ. Assessing efficacy of complementary medicine: Adding qualitative research methods to the gold standard. The Journal of Alternative and Complementary Medicine. 2002;8:275–281. doi: 10.1089/10755530260127961. [DOI] [PubMed] [Google Scholar]
- Wasson J, et al. Benefits and obstacles of health status assessment in ambulatory settings: The clinician’s point of view. Medical Care. 1992;30:MS42–MS49. doi: 10.1097/00005650-199205001-00004. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Sholomskas D, Pottenger M, Prushoff BA, Locke BZ. Assessing depressive symptoms in five psychiatric patient populations: A validation study. American Journal of Epidemiology. 1977;106:203–214. doi: 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]
- Whittemore R, Grey M. The systematic development of nursing interventions. Journal of Nursing Scholarship. 2002;34:115–120. doi: 10.1111/j.1547-5069.2002.00115.x. [DOI] [PubMed] [Google Scholar]
- Wilcox H, Field T, Prodromidis M, Scafidi F. Correlation between BDI and CES-D in a sample of adolescent girls. Adolescence. 1998;33:565–574. [PubMed] [Google Scholar]
- Wisner KL, Scholle SH, Stein B. Perinatal disorders: Advancing public health opportunities. J Clin Psychiatry. 2008;69(10):1602–1605. doi: 10.4088/jcp.v69n1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- York R, Brown LP, Samuels P, Finkler SA, Jacobsen B, Persely CA, et al. A randomzied controlled trial of early discharge and nurse specialist transitional follow up care of high risk childbearing women. Nursing Research. 1997;40:254–261. doi: 10.1097/00006199-199709000-00003. [DOI] [PubMed] [Google Scholar]
- Zanjani F, Miller B, Turiano N, Ross J, Oslin D. Effectiveness of telephone-based referral care management, a brief intervention to improve psychiatric treatment engagement. Psychiatric Services. 2008;59:776–781. doi: 10.1176/ps.2008.59.7.776. [DOI] [PubMed] [Google Scholar]
- Zittel-Palamara K, Rockmaker JR, Schwabel KM, Weinstein WL, Thompson SJ. Desired assistance versus care received for postpartum depression: Access to care differences by race. Archives of Women’s Mental Health. 2008;11(2):1434–1816. doi: 10.1007/s00737-008-0001-1. [DOI] [PMC free article] [PubMed] [Google Scholar]