Abstract
Posttraumatic stress disorder (PTSD) diagnosis requires first identifying a traumatic event, but very few studies have evaluated methods of potential traumatic event assessment and their impact on PTSD diagnosis. We compared a behaviorally-specific comprehensive multiple-item traumatic event measure to a single-item measure to determine their impact on traumatic event identification and subsequent PTSD diagnosis. In a within-subject, counterbalanced design, the Traumatic Life Events Questionnaire (TLEQ; Kubany et al., 2000) was compared to the single-question traumatic event assessment in the Structured Clinical Interview for DSM-IV (SCID; First, Spitzer, Gibbon, & Williams, 1998) in 129 participants in opioid dependence treatment. The TLEQ produced a 9-fold higher rate of traumatic events reported by the participants as compared to the SCID. As a result, PTSD diagnoses in the sample increased to 33% after the TLEQ measure from 24% after the SCID. The increase in potential traumatic event identification and PTSD diagnosis was greater in women than men. This study provides strong support for the use of comprehensive traumatic event assessments to measure traumatic events and PTSD diagnoses, particularly in women.
Keywords: traumatic event, posttraumatic stress disorder, substance use disorder, assessment, gender differences
Posttraumatic stress disorder (PTSD) is commonly diagnosed in people with and without substance use disorder (Frans, Rimmo, Aberg, & Fredrikson, 2005; Mills, Teesson, Ross, & Peters, 2006). Despite ongoing debate about the validity of certain diagnostic criteria, documentation of traumatic event exposure is clearly a necessary precursor to evaluation of the syndrome (Weathers & Keane, 2007). Traumatic event assessments for the diagnosis of PTSD range from a single question on the Structured Clinical Interview for DSM-IV (SCID; First et al., 1998) to a comprehensive, multiple-item list of potential traumatic events, such as the Traumatic Life Events Questionnaire (TLEQ; Goodman, Corcoran, Turner, Yuan, & Green, 1998; Gray, Litz, Hsu, & Lombardo, 2004; Kubany et al., 2000). Most specialists in PTSD diagnosis strongly recommend the use of a comprehensive, multiple-item measure in which each potential traumatic event category is assessed separately (Cusack, Falsetti, & De Arellano, 2002; Elhai, Gray, Kashdan, & Franklin, 2005), although most treatment providers and researchers in other areas of psychopathology continue to use briefer and less comprehensive approaches in assessing traumatic event exposure (Elhai, Franklin, & Gray, 2008). Since traumatic event exposure is a necessary criterion for diagnosis of PTSD, traumatic event assessments that systematically over- or under-identify actual exposures can affect the rate of PTSD diagnosis.
The recommendation to use more comprehensive and detailed approaches to traumatic event assessment is supported by the belief that this method is more accurate than less comprehensive screening of traumatic events, like that employed by the SCID. A review of the literature, however, produced only four published reports comparing the two methods of traumatic event assessment. Two studies of outpatient psychiatric patients (Franklin, Sheeran, & Zimmerman, 2002), primary care patients (Elhai et al., 2008), and non-treatment seeking college students (Elhai et al., 2008) reported that more individuals with traumatic event exposure were identified with the more comprehensive and structured list of potential traumatic events compared to the single-item SCID approach. However, the specific number and type of traumatic event exposures were not reported in those studies. A third study of women seeking help for intimate partner violence reported a larger number and wider range of events with the comprehensive traumatic event assessment than the standard SCID probe, although there was no difference in reports of intimate partner violence (Weaver, 1998). In a fourth study of substance users, the comprehensive multiple-item measure identified far higher rates of potential traumatic event exposure than the three general trauma screening questions included in the Addiction Severity Index (Najavits et al., 1998).
Although traumatic event identification is central to the diagnostic assessment of PTSD, it is not yet clear whether an accurate and full description of all traumatic event exposure is necessary to correctly diagnose PTSD (Weathers & Keane, 2007). In the transition from DSM-III-R to DSM-IV, the range of potential traumatic events was widened to include indirectly experienced events; this resulted in a 59% increase in prevalence of PTSD in a community population (Breslau & Kessler, 2001). Both Franklin et al. (2002) and Elhai et al. (2008) reported that more individuals endorsed traumatic event exposure with the multiple-item assessment versus the single-item SCID assessment, though neither group concluded that the increased endorsement of traumatic events resulted in a significant overall increase in PTSD diagnosis. Separate from the traumatic event assessment, PTSD symptom screening on the SCID assesses for up to four types of Cluster B symptoms: distressing recollections, distressing dreams, flashbacks, and psychological distress upon exposure to a traumatic event reminder. Failure to endorse any of the four symptoms results in automatic skip-out of the PTSD diagnostic module, although the fifth possible symptom of physiological reactivity is not assessed. This screening approach is designed to maximize both sensitivity and specificity, since people rarely have many Cluster C and D symptoms without significant Cluster B symptoms (Franklin et al., 2002). However, we can find no published evaluations of the symptom screening approach for PTSD diagnosis.
Gender also appears to play a significant role in the assessment of traumatic event exposure and in diagnosis of PTSD. For example, the increase in traumatic event identification due to DSM-IV criteria changes was attributed primarily to increased detection of traumatic events in women (Breslau & Kessler, 2001). Unfortunately, the three other studies directly comparing traumatic event probes either did not report gender analyses (Elhai et al., 2008; Franklin et al., 2002) or were limited to women (Weaver, 1998), precluding gender analyses. Women are at greater risk of developing PTSD, in part because they are more likely to experience traumatic events that convey a higher risk of precipitating PTSD (e.g., sexual assault). Even when analyses account for specific traumatic event exposure, however, women remain at higher risk for PTSD (Breslau, 2002; Nemeroff et al., 2006; Tolin & Foa, 2006). In addition, women substance users may respond to traumatic event assessments differently from men (Thombs, Lewis, Bernstein, Medrano, & Hatch, 2007), which will affect both event reporting and PTSD diagnosis. It is important to improve our understanding of the relationship between traumatic event assessments and diagnosis of PTSD, particularly with attention to potential gender differences.
The present study systematically compares the effect of a comprehensive multiple-item assessment of traumatic event exposure to a general single-item (SCID-based) measure on the number of traumatic events identified and the subsequent rates of PTSD in men and women with opioid and other drug use disorders (N = 129). The SCID was specifically included in the study because it is one of the most commonly used diagnostic interviews in studies of PTSD in treatment- and non-treatment-seeking populations (Elhai et al., 2005). Traumatic event exposure rates in opioid use disordered patients are near 100%, and lifetime PTSD diagnosis rates are about 40% (Mills, Lynskey, Teesson, Ross, & Darke, 2005). Thus, this population is ideal for an empirical test of assessment in that it will be subject neither to a “floor” effect of traumatic event exposure, as with community populations, nor to a “ceiling” effect, as with patients seeking treatment for trauma-related problems. Since extensive traumatic event exposure is anticipated, the current study can greatly extend previous work to compare the number and range of events identified by each assessment approach, in addition to gender-related differences. The study addresses the following questions: 1) whether the number of traumatic events is greater when a comprehensive multiple-item event measure is used; 2) whether a difference in the number of traumatic events alters the rate of PTSD diagnosis; 3) whether the symptom screening procedure in the SCID PTSD module screens out cases of PTSD that would be diagnosed if the full module were administered; and 4) the degree to which gender is related to either traumatic event assessment or PTSD diagnosis.
Method
Participants
Participants were male and female admissions to an outpatient opioid agonist treatment program. All participants were concurrently enrolled in a larger study of psychiatric assessment and on- versus off-site psychiatric care for patients with a current comorbid disorder. Primary inclusion criteria for the parent study included enrollment in the substance use disorder treatment program, self-reported psychiatric problems, and a stated desire for help with those problems. Exclusion criteria for the parent study were: 1) receiving psychiatric care elsewhere and 2) evidence of an emergent or potentially life-threatening medical illness (e.g., acute liver failure). The present study had the additional inclusion criterion that participants had to provide specific and separate written consent to participate in this evaluation. Both studies (parent study and present study) were conducted in accordance with APA ethical guidelines and with local Institutional Review Board review and approval. All participants signed informed consent for each study separately. Of 160 participants in the parent study approached for the present study, 133 provided informed consent during the study period of March 2004 to January 2006.
Of 133 consented participants, 4 did not complete the two necessary study sessions, leaving a final study sample of 129 participants. Non-completers were similar to completers in gender, age, race and ethnicity, and education. A majority of the sample participants were female (n = 78) and the average age was 40 years (SD = 9, range: 20-64). The sample was almost evenly divided between non-minority and minority participants [54% Caucasian (n = 70), 43% African American (n = 56), 2% Latino American (n = 2), 1% Asian American (n = 1)]. Average education was 10.6 years (SD = 2, range: 6-16), and only 40% had a high school degree or equivalent. Very few participants were employed in any capacity (8%). All participants met criteria for physical dependence on opioids. Prevalence rates of other current and lifetime psychiatric disorders are shown in Table 1.
Table 1. Selected Lifetime and Current Psychiatric Disorders Diagnosed with the Structured Clinical Interview for DSM-IV, Excluding PTSD (N = 129).
| Diagnosis | Lifetime % (n) |
Current % (n) |
|---|---|---|
| Alcohol use disorder | 75 (97) | 10 (13) |
| Sedative use disorder | 50 (64) | 12 (15) |
| Cocaine use disorder | 85 (110) | 35 (45) |
| Cannabis use disorder | 64 (82) | 4 (5) |
| Major depressive disorder | 62 (80) | 47 (60) |
| Bipolar disorder | 16 (20) | 16 (20) |
| Dysthymia | -- | 16 (20) |
| Schizophrenia/schizoaffective disorder | 4 (5) | 4 (5) |
| Panic disorder | 12 (16) | 9 (12) |
| Agoraphobia | 5 (6) | 4 (5) |
| Social phobia | 18 (23) | 12 (15) |
| Obsessive-compulsive disorder | 7 (9) | 5 (7) |
| Generalized anxiety disorder | -- | 11 (14) |
| Adjustment disorder | -- | 2 (2) |
| Borderline personality disorder | -- | 26 (33) |
| Antisocial personality disorder | -- | 38 (49) |
| Any Axis I | 96 (124) | 92 (118) |
| Any Axis II | -- | 40 (52) |
| Any Axis I or II | 98 (127) | 97 (125) |
Note. Dash indicates no SCID lifetime diagnosis was made.
Measures
The Structured Clinical Interview for DSM-IV (SCID; First et al., 1998) was used both to assess for exposure to potential traumatic events and to diagnose lifetime (past and current) rates of PTSD, as part of the complete Axis I SCID diagnostic assessment. The SCID traumatic event measure is a single open-ended question: “Sometimes things happen to people that are extremely upsetting—things like being in a life threatening situation, a major disaster, very serious accident or fire; being physically assaulted or raped; seeing another person killed or dead, or badly hurt, or hearing about something horrible that has happened to someone you are close to. At any time during your life, have any of these kinds of things happened to you?” All events elicited by this probe were recorded, along with any information provided. In accordance with SCID administration procedures, interviewers elicited an approximate date or age at the time of the event, but did not prompt for any further information. Regardless of the event assessment measure used, all participants reporting at least one traumatic event were administered the SCID diagnostic module for PTSD using standard SCID administration procedures. Any symptom that was rated subthreshold or unclear did not contribute to the number of positive symptoms for the diagnosis; this happened very rarely.
Participants were interviewed with the Traumatic Life Events Questionnaire (TLEQ; Kubany et al., 2000) to assess for a history of potential traumatic event exposure. The interview format was chosen to mirror the SCID administration and to minimize problems with participant literacy. The authors have compared the results from a standard written questionnaire to those produced in an interview format and found small nonsignificant differences in reported traumatic event exposure (Kubany et al., 2000). The well-validated TLEQ is considered an exemplar of the “gold standard” of traumatic event assessments (Gray et al., 2004; Weathers & Keane, 2007). People seeking treatment for substance use disorder do not generally find a comprehensive and highly structured assessment of traumatic event exposure very distressing, nor is there evidence that patients suffer adverse events as a result of this type of assessment (McHugo et al., 2005).
The TLEQ is a comprehensive list of 22 behaviorally-descriptive potential traumatic events and a 23rd category of “other events” with examples. The following question for adult physical assault is an example of the type of questions on the assessment: “Have you been robbed or been present during a robbery where the robber(s) used or displayed a weapon?” Once an event was endorsed, participants were asked how often such an event had happened to them. Responses were coded “never,” “once,” “twice,” “3 times,” “4 times,” “5 times,” and “more than 5 times,” coded as 6. The TLEQ was administered using all 23 items as written. To simplify presentation, a few similar types of traumatic events were collapsed in the results. Motor vehicle accidents and other accidents were grouped together as “accident.” Robbery with a weapon and physical assault occurring during adulthood were categorized as “adult physical assault.” All sexual assaults before age 13 (including assaults by a peer or by someone at least 5 years older) were grouped into “childhood sexual assault.” Unwanted sexual attention (other than sexual assault) and stalking were categorized as “other threats.” Finally, “other” events included all responses that did not fit into other categories, as well as the specific TLEQ questions about miscarriage and abortion. The remaining categories reported here are responses to single items. Results of each of the 23 items are in the supplemental material available online. There were two cases of a missing response for an event (i.e., one serious illness, one young adult sexual assault). We used the most conservative approach to analysis and assumed those events were negative. Endorsement of events on the TLEQ is designed to meet criterion A1 of the posttraumatic stress disorder diagnosis (American Psychiatric Association, 1994), and is followed by a question to assess for criterion A2 (reaction to the event). To more closely parallel the SCID traumatic event probe, which does not assess criterion A2 until the start of the diagnostic module, TLEQ-identified traumatic events reported here did not require endorsement of criterion A2. Thus, all events reported were potential traumatic events. The TLEQ only assesses exposure to traumatic events and cannot be used to diagnose PTSD.
Procedures
Participants undergoing psychiatric assessment for the parent study were asked whether they would be willing to participate in a second separate study while completing the assessments for the parent study. They were informed that their participation in the present study had no effect on eligibility for the parent study or their routine care in the treatment program. To reduce the effect of acute distress on psychiatric symptom reporting and diagnostic validity, participants were assessed for psychiatric diagnosis 3 to 4 weeks after recruitment into the parent study. Prior to all assessment sessions, participants were administered a Mini-Mental Status Exam (Folstein, Folstein, & McHugh, 1975) to identify acute cognitive impairment, including that possibly related to drug intoxication. Participants who scored below 27 out of 30 on the measure were rescheduled for another day and referred to senior clinical staff for evaluation. Participants received $10 in compensation for completing each session.
Traumatic Event Assessments
After consent, participants were randomly assigned to receive either the SCID or TLEQ event assessment, followed by the SCID diagnostic module for PTSD. Participants returned no sooner than 1 day and no later than 2 weeks for a second interview in which they were administered the alternate event probe and the SCID diagnostic module for PTSD, if indicated. Assessments were spaced in this way to reduce potential carryover effect from the first interview while also limiting the chance of new events occurring in the interim. Traumatic event reports are relatively stable over such short periods of time (Kubany et al., 2000; Wyshak, 1994). The average length of time between assessments was 4.3 days (median 3 days). To maintain independence of the data, the second assessment session was conducted by a different interviewer who did not have access to the traumatic event and PTSD information obtained in the first interview. Traumatic event assessments (TLEQ vs. SCID) were confirmed to have been presented in a random order throughout the study (47% TLEQ first vs. 53% SCID first; Binomial Test; p > .1).
PTSD Diagnostic Module Screening
After potential traumatic event identification with either the TLEQ or SCID, participants who reported more than one event were asked: “Of the events we just talked about, which event causes you the most distress?” There is no direction on the SCID for methods to elicit the target event, so this language from the TLEQ was used in both assessments. The screening questions for PTSD in the SCID were directed to the event chosen by the participant. The SCID screening questions are located after the list of potential traumatic events and at least one must be positive in order to continue the PTSD diagnostic evaluation. In all cases, the screening was initially administered in accordance with SCID administration rules. The only change to the methods occurred after the interview was completed. At that time, if the participant had originally screened out of the PTSD diagnostic module, the interviewer returned to the module at the end of the interview and completed it as if the participant had screened in. This procedure was used in both sessions.
Interviewer Training: SCID and TLEQ Assessments
Interviewers had master's degrees in psychology and at least two years as trained research interviewers supervised by the senior author. A two-stage training process was completed by the 8 interviewers (4 male, 4 female) who collected data in this study. Stage 1 involved approximately 30 hours of didactic (manual and videotape) training supplemented by practice interviewing on the SCID. Stage 2 involved interviewers co-rating at least 3 consecutive interviews that agreed with an expert rating (presence or absence of a diagnosis), followed by their conducting at least 3 interviews that produced ratings that agreed with expert co-ratings. The experts used in the present study were trained on the SCID by Dr. Michael First. Interviewers were trained to ask the PTSD module traumatic event exposure question as written first, and to repeat the question if they received an unclear response. Interviewers were permitted to ask a limited number of follow-up questions to clarify the response. If these efforts failed to produce a clear rating, the participant could then be re-interviewed by an expert. While the SCID training covered this procedure and provided examples of the types of questions that might be asked to clarify unclear responses, interviewers were not provided a list of such questions they could use in the study. Prior studies using this basic two-step interviewer training procedure with the SCID produced high levels of rater reliability (see Brooner, King, Kidorf, Schmidt, & Bigelow, 1997), although no data were collected on rater reliability concerning the traumatic event question in the PTSD module. Training on the TLEQ was provided by the lead author and included didactic training, review of the first 20 interviews, and regular staff meetings to review and clarify procedures. Interviewers were informed about the purpose of the evaluation and no effort was made to mask specific study hypotheses.
Data analysis
Means, standard errors, and proportions were used to describe prevalence of psychiatric disorders (including PTSD) in the entire sample and within gender. All data on number and types of traumatic events were analyzed using the full dataset (i.e., each of the 23 items on the TLEQ); item categories were collapsed only in presentation. Proportions of each gender with exposure to particular types of potential traumatic events were compared using prevalence ratios with 95% confidence intervals (CI) using males as the reference group. The primary advantage of prevalence ratios over odds ratios is that as the occurrence of an outcome increases, odds ratios increasingly inflate the differences between groups while prevalence ratios remain accurate and interpretable. Proportions of each gender with PTSD diagnosis and specific events selected for PTSD assessment were compared with χ2 tests. Effect sizes for χ2 are given as phi (φ). Proportions of participants who screen out of the diagnostic module after the TLEQ and SCID probes were compared using the McNemar test across and within gender. The sensitivity and specificity (with 95% CI) of the SCID event probe to identify potential traumatic events were analyzed using the TLEQ results as the reference. Sensitivity is also known as the “true positive” rate and specificity is the “true negative” rate. PTSD diagnostic agreement across sessions was tested using Cohen's kappa (κ).
The number of potential traumatic events elicited in response to the TLEQ and SCID event probes was analyzed with a series of Generalized Estimating Equation (GEE) models (Zeger & Liang, 1986). GEE is a form of generalized linear modeling that allows for within-subject correlations. Although the distribution of the number of events on the TLEQ approached normality, the number of events on the SCID event probe was more appropriately characterized as a Poisson distribution. To correctly model the results that include the SCID probe, all GEE models treated both variables as Poisson. GEE is able to correct for the potential overdisperson common in Poisson distributions (Slymen, Ayala, Arredondo, & Elder, 2006), and is more appropriate than other Poisson models (e.g., negative binomial regression) for repeated-measures designs. We tested the main effects of order, probe and gender and the 2-way and 3-way interactions using GEE specified with a log link and treating the distributions as Poisson variables. Later analyses were collapsed across order, but otherwise performed in the same way. Means and standard errors of the counts for each effect are presented. A priori contrasts were computed to represent the incidence rate ratios (IRR) in the counts (along with 95% CIs) for each effect, indicating the degree to which the number of events on the TLEQ assessment were different from the number on the SCID assessment. The IRR is interpreted similarly to an odds ratio.
Results
Traumatic Event Probes
Overall Number of Potential Traumatic Events Reported
Order effects
There were no significant interactions that included the Order term: Order × Gender × Assessment, χ2(1, N = 129) = 2.59, p = .108 and Order × Assessment, χ2(1, N = 129) = 0.12, p = .725. Subsequent analyses were collapsed across order.
Assessment effects
The total number of potential traumatic events reported in response to the TLEQ was 9 times greater than the number of events obtained using the SCID assessment, even when the effect was adjusted for gender (TLEQ M = 21.21, SEM = 1.05 vs. SCID M = 2.29, SEM = 1.09), IRR = 9.27, 95% CI = 7.90 – 10.86, χ2(1, N = 129) = 74.99, p < .0001. All participants reported at least one event on the TLEQ (range: 1-63) and 86% reported at least one event on the SCID (range: 0-10). In no case were there fewer potential traumatic events reported on the TLEQ than on the SCID. There was no correlation between the length of time between the two assessments and the magnitude of difference in the number of events reported, r = -.1; p > .1.
Gender differences
Although both women and men reported more potential traumatic events in response to the TLEQ as compared to the SCID, women had a greater disparity in the number of events reported, see Figure 1. This difference was largely due to women reporting more events than men in response to the TLEQ (women M = 24.96, SEM = 1.07 vs. men M = 17.96, SEM = 1.09), IRR = 1.39, 95% CI = 1.13 – 1.71.
Figure 1.
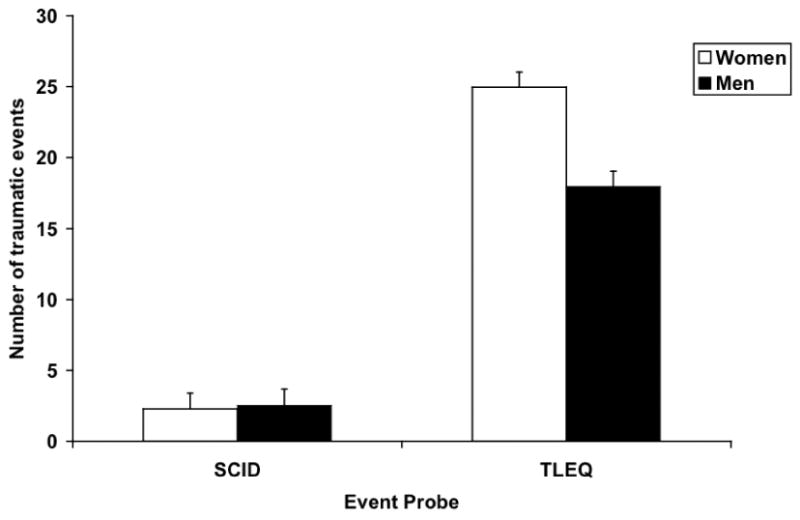
Gender differences in total traumatic events identified by event probe. Gender × Assessment, χ2(1, N = 129) = 6.64, p = .010.
Types of Potential Traumatic Events Reported
Differences were also observed in the types of events reported (see Table 2). Nearly all potential traumatic events identified by the SCID measure were also reported on the TLEQ; that is, the SCID had nearly 100% specificity for potential traumatic events. However, the SCID assessment for these events was much less sensitive and especially poor at detecting TLEQ-identified serious illnesses, injury/illness of loved one, family violence, intimate partner violence, and threats of physical assault.
Table 2. Sensitivity and Specificity of Traumatic Event Reports on the Structured Clinical Interview for DSM-IV Event Probe, as Compared to the Traumatic Life Events Questionnaire (N = 129).
| Event | TLEQ % (n) |
SCID % (95% CI) |
|
|---|---|---|---|
| Sensitivity | Specificity | ||
| Natural disaster | 22 (28) | 21 (9 – 42) | 100 (95 – 100) |
| Accident | 57 (74) | 30 (20 – 42) | 96 (86 – 99) |
| Combat | 1 (1) | 0 (0 – 95) | 100 (96 – 100) |
| Serious illness (e.g., HIV, cancer) | 41 (53) | 6 (2 – 17) | 99 (92 – 100) |
| Death of loved one | 84 (108) | 48 (39 – 58) | 86 (63 – 96) |
| Injury/illness of loved one | 41 (53) | 9 (4 – 21) | 93 (85 – 98) |
| Witness family violence | 56 (72) | 4 (1 – 13) | 100 (92 – 100) |
| Childhood physical assault | 30 (39) | 15 (6 – 31) | 100 (95 – 100) |
| Adult physical assault | 79 (102) | 21 (14 – 30) | 100 (85 – 100) |
| Intimate partner violence | 51 (66) | 9 (4 – 19) | 100 (93 – 100) |
| Witness physical assault | 52 (67) | 21 (12 – 33) | 95 (86 – 99) |
| Threatened with physical assault | 49 (63) | 2 (0 – 10) | 100 (93 – 100) |
| Childhood sexual assault | 29 (38) | 34 (20 – 51) | 98 (92 – 100) |
| Young adult sexual assault | 24 (31) | 29 (15 – 48) | 98 (92 – 100) |
| Adult sexual assault | 22 (28) | 32 (17 – 52) | 99 (94 – 100) |
| Other threats | 39 (50) | 0 (0 – 9) | 100 (94 – 100) |
| Other (e.g., miscarriage, finding dead bodies, violent death of pet, witness drug overdose of stranger) | 69 (89) | 11 (6 – 20) | 90 (75 – 97) |
| Any traumatic event | 100 (129) | 86 (79 – 91) | -- |
Note. CI = confidence interval. Dash indicates that specificity could not be calculated.
Gender differences
As expected, there were significant gender differences in exposure to potential traumatic events (Table 3). Combat was reported only by men and adult sexual assault only by women. Men were more likely than women to report having been physically assaulted by a stranger as an adult, and women were more likely to report intimate partner violence. There was no significant gender difference in exposure to childhood sexual assault, but women were more likely than men to report sexual assault after age 13.
Table 3. Gender Differences in Prevalence of Traumatic Events Reported on the Traumatic Life Events Questionnaire (N = 129).
| Event | Mena % (n) |
Womenb % (n) |
PR (95% CI) |
|---|---|---|---|
| Natural disaster | 29 (15) | 17 (13) | 1.77 (0.92, 3.39) |
| Accident | 57 (29) | 58 (45) | 0.99 (0.73, 1.30) |
| Combat | 2 (1) | 0 | -- |
| Serious illness (e.g., HIV, cancer) | 37 (19) | 44 (34) | 0.86 (0.55, 1.32) |
| Death of loved one | 80 (41) | 86 (67) | 0.94 (0.80, 1.10) |
| Injury/illness of loved one | 45 (23) | 39 (30) | 1.17 (0.78, 1.78) |
| Witness family violence | 45 (23) | 63 (49) | 0.72 (0.51, 1.02) |
| Childhood physical assault | 31 (16) | 30 (23) | 1.06 (0.63, 1.81) |
| Adult physical assault | 90 (46) | 72 (56) | 1.26 (1.06, 1.48) |
| Intimate partner violence | 24 (12) | 69 (54) | 0.34 (0.20, 0.57) |
| Witness physical assault | 57 (29) | 49 (38) | 1.17 (0.84, 1.62) |
| Threatened with physical assault | 51 (26) | 47 (37) | 1.08 (0.75, 1.54) |
| Childhood sexual assault | 24 (12) | 33 (26) | 0.71 (0.39, 1.27) |
| Young adult sexual assault | 4 (2) | 37 (29) | 0.11 (0.03, 0.42) |
| Adult sexual assault | 0 | 36 (28) | -- |
| Other threats | 29 (15) | 45 (35) | 0.66 (0.40, 1.07) |
| Other (e.g., miscarriage, finding dead bodies, violent death of pet, witness drug overdose) | 59 (30) | 76 (59) | 0.78 (0.60, 1.01) |
Note. The reference category is women. Dash indicates that the prevalence ratio could not be calculated. PR = Prevalence ratio; CI = confidence interval.
n = 51.
n = 78.
Posttraumatic Stress Disorder
PTSD Diagnosis in Response to TLEQ and SCID Event Assessments
Lifetime PTSD (past and current episodes) was diagnosed after the TLEQ assessment in 33% of participants compared to 24% of participants after the SCID assessment. A large majority of these lifetime diagnoses were current at the time of the assessment (32 of 43 TLEQ; 25 of 31 SCID). Interestingly, lifetime PTSD diagnostic groups based on the TLEQ versus SCID traumatic event assessment did not overlap completely. Thirteen percent of the sample (n = 17) received a lifetime diagnosis of PTSD after both of the potential traumatic event assessments; 20% (n = 26) after the TLEQ only; and 11% (n = 14) after the SCID event assessment only. The remaining participants (56%; n = 72) did not meet criteria for a lifetime diagnosis of PTSD following either assessment for traumatic events. Fourteen percent (n = 18) of the sample did not report any potential traumatic events on the SCID event measure, so were not assessed for PTSD in that session. Most of these participants received the SCID before the TLEQ (14 vs. 4, Binomial test, p < .04). One-third of these 18 individuals, however, met criteria for lifetime PTSD subsequent to the TLEQ and 5 of them met diagnostic criteria for current PTSD. Of the remaining 34 participants with diagnostic discrepancy, 21 reported events in clearly different categories for each PTSD assessment. In nearly every case, the event that precipitated the PTSD diagnosis was in a higher risk category (e.g., childhood sexual assault vs. death of loved one). Since the precise characteristics of each individual event could not always be determined, it is likely that the remaining discrepancies were due to different events that fell in the same category, but carried different levels of risk for PTSD. No differences were found between discrepant subgroups in assessment order, days between assessments, or interviewers (data not shown).
Gender differences
There were no differences between men and women on the proportion of participants with PTSD subsequent to the SCID event assessment, χ2(1, N = 129) = 0.28, p > .1, φ = .05. When compared after the TLEQ assessment, the percentage of men with PTSD remained approximately the same while more women met criteria for PTSD, φ = .24 (see Figure 2). Diagnostic agreement across event assessment, although generally poor, was clearly better for men (κ = .46; p < .01) than for women (κ = .14; p > .1).
Figure 2.
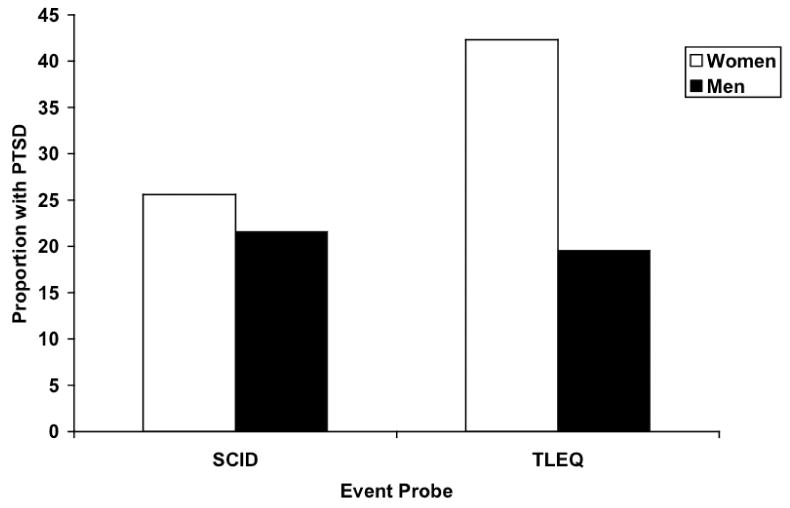
Gender differences in PTSD diagnosis by event probe. SCID: χ2(1, N = 129) = 0.28, p > .1, TLEQ: χ2(1, N = 129) = 7.15, p < .01.
PTSD Precipitating Events after TLEQ or SCID Event Assessments
Only 37% of participants were assessed for lifetime PTSD for the same category of event after both potential traumatic event assessments. The most common event assessed for PTSD after the TLEQ was death of a loved one (26%), followed by “other” events (10%), childhood sexual assault (9%) and adult physical assault (9%). Among participants reporting at least one event on the SCID event assessment, 36% were assessed for PTSD related to death of a loved one, followed by witnessing physical assault (10%), accident (9%), and adult sexual assault (8%).
Of participants diagnosed with PTSD, the most common precipitating event identified on the TLEQ was childhood sexual assault (26%), followed by death of a loved one (16%), and young adult sexual assault (12%). The most common PTSD precipitating events on the SCID assessment were childhood sexual assault (19%), young adult sexual assault (16%), and death of a loved one (13%).
Gender differences
Men (33%) and women (40%) were equally likely to report the same events for PTSD diagnostic assessment after each potential traumatic event assessment, χ2(1, N = 129) = 0.54, p > .1. The most common PTSD precipitating event identified on the TLEQ for men was an accident and, for women, childhood sexual assault. The most common PTSD event identified with the SCID event assessment was again an accident for men, but young adult sexual assault for women.
PTSD Diagnostic Module Screening
Participants were more likely to screen out of the PTSD diagnostic module after the SCID event assessment (29%) versus the TLEQ event assessment (16%), McNemar Test, p < .01. This difference was related to gender; women screened out more often after the SCID event assessment (28%) than the TLEQ assessment (8%), McNemar Test, p < .01, while men were equally likely to screen out following either event assessment, 31% SCID vs 29% TLEQ, McNemar Test, p > .1. The diagnostic screen sensitivity was poor regardless of which event assessment measure was used (TLEQ 24% vs. SCID 39%). That is, screening in was not highly predictive of meeting PTSD criteria. However, no participant who screened out was found to meet criteria for PTSD when the full diagnostic assessment was completed. In other words, the PTSD diagnostic module screening was 100% specific in this sample.
Discussion
The use of a comprehensive, highly structured, and behaviorally detailed multiple-item assessment for potential traumatic events versus a single-item traumatic event measure as used by the SCID has been advocated by experts in the assessment of trauma and PTSD for several years (Elhai et al., 2005). Nonetheless, briefer and far less structured approaches are often used to assess exposure to potential traumatic events, often to simplify and shorten the assessment process. The present study is the first known published report that directly compares a comprehensive and highly structured behaviorally-specific assessment for potential traumatic event exposure to a single-item measure in a rigorous randomized trial. In this direct comparison, nine times as many potential traumatic events were reported using the comprehensive multiple-item measure versus the less structured single question assessment used in the SCID. The rate of PTSD increased from 25% to 33% of the sample when the multiple-item TLEQ was used to assess potential traumatic event exposure.
Traumatic Events and PTSD
The dramatic increase in traumatic event identification when using the TLEQ as compared to the SCID event assessment is not unexpected. Previous studies have reported similar disparities in women seeking treatment for intimate partner violence (Weaver, 1998) and in psychiatric outpatients (Franklin et al., 2002). The sensitivity of the SCID event assessment for “any” potential event in the present study is also remarkably similar to that reported by Franklin, although the present study extends the earlier work by providing data on the sensitivity and specificity of individual traumatic event types and gender difference in responding. It is remarkable that the sensitivity of the SCID's potential traumatic event assessment should be so universally low, even for highly salient events that most often precipitated the diagnosis of PTSD in this sample—death of a loved one, childhood sexual assault and young adult sexual assault. Although some of the events reported on the TLEQ that were missed by the SCID may be false positives, the number is so great and consistent across categories that it is highly unlikely that all of them are false. Thus, the present results suggest that the single-item SCID traumatic event question (criterion A1) identifies fewer potential traumatic events across event categories than the TLEQ, especially for women.
More importantly, the increase in traumatic events reported on the TLEQ resulted in more cases of PTSD. This finding both illustrates and quantifies the importance of traumatic event assessment for PTSD diagnosis. The value of identifying more traumatic events with the more comprehensive and time-consuming TLEQ measure would be questionable if the difference in potential traumatic events was unrelated to the rate of PTSD diagnosis. The 9% increase in PTSD diagnosis subsequent to the more comprehensive TLEQ measure falls between the 2% increase reported by Franklin et al. (2002) and the 13% increase reported by Elhai et al. (2008). This similarity is remarkable, particularly considering that the method of PTSD diagnosis (SCID interview vs. self-report) and the sample characteristics (substance dependent patients vs. primary care patients, college students, and psychiatric outpatients) varied considerably between this and the previous studies. Further, the present findings extend previous work that did not report on possible reasons for PTSD diagnostic discrepancies. The difference is not due to artifacts such as the order of assessments, time between assessments, or interviewer effect, either overall or in cases of discrepancy. A significant portion of the discrepant diagnoses (6 of 40) resulted from the failure of the SCID to identify any potential traumatic event for PTSD evaluation. The remaining discrepant diagnoses were likely related to the participants having to choose their “most distressing” event from a smaller list generated by the SCID assessment (2 on average) than the average of 21 on the TLEQ. With fewer events to choose from on the SCID, participants more often chose one that, although relatively more distressing than the others, was not distressing enough to precipitate a PTSD diagnosis.
Gender Differences
The present study is also the first to systematically compare different potential traumatic event assessment methods and characterize their effect on PTSD diagnosis, with a particular emphasis on gender comparisons. The magnitude of change in traumatic event reports was much larger in women than men, which may be due to women reporting more events when specifically prompted for them. Other studies have reported higher rates of sexual assault when potential traumatic events were described in specific behavioral terms, as opposed to approaches using more general terms (Resnick, Kilpatrick, Dansky, Saunders, & Best, 1993). The increase in rates of PTSD in the present study is due almost entirely to the effect of the TLEQ on diagnostic cases of PTSD in women. With a greater number of events identified on the TLEQ, women simply had more events to choose from for further PTSD evaluation than men. In addition, women reported greater exposure overall to events that carry higher risk for PTSD, particularly sexual assault (see Table 3). As noted by others, other factors that remain undetected likely contribute to an independent gender-related risk of PTSD (Breslau, 2002). The failure to use a comprehensive and more behaviorally-specific multiple-item traumatic event measure will likely result in fewer reports of potential traumatic events and a correspondingly lower prevalence of PTSD in women.
Strengths and Limitations
One of the most important methodological strengths of the study is the randomized, counterbalanced, within-subject design that allowed a rigorous test of the two traumatic event assessment methods. In addition, we were careful to select common standardized measures, all of which were administered in interview format to minimize the potential effect of poor reading ability and attention. The sample was notable for its excellent representation of women and for its density of traumatic events and PTSD, which prevented skewed results from the undue influence of a few individuals with traumatic events or PTSD.
One notable limitation of the study is the extent of generalizability of the findings to different samples of men and women. This study was conducted in a sample of treatment-seeking opioid dependent patients with additional comorbid psychiatric disorders. It is unclear how findings from this sample will generalize to drug-dependent people who are not enrolled in treatment or who do not have other psychiatric diagnoses, or to people without substance use disorder. This concern is offset somewhat by the fact that the main findings in this study have been reported in earlier studies that used very different clinical samples (Elhai et al., 2008; Franklin et al., 2002; Weaver, 1998). Since the purpose of the study was to evaluate traumatic event assessment in a clinical population at risk for PTSD, but who have not been identified as having PTSD nor are seeking treatment for PTSD-related symptoms, these data cannot speak to traumatic event assessment in a PTSD clinical population. In addition, retrospective recall of traumatic events can be affected by PTSD symptomology (Roemer, Litz, Orsillo, Ehlich, & Friedman, 1998), so current PTSD symptoms may have increased traumatic event reporting. However, this effect appears to be less robust in women (King et al., 2000) and there is no good reason to believe that one traumatic event measure would be more affected than the other.
An important caveat to our findings and their discussion is that 11% of the sample met diagnostic criteria for PTSD following the SCID traumatic event assessment but not the TLEQ assessment. The strongest argument for using a more versus less comprehensive assessment of potential traumatic event exposure would have shown that the TLEQ identified all potential events and subsequent cases of PTSD detected by the SCID traumatic event assessment plus additional cases that were “missed” by the SCID event assessment. The study was not able to account for this finding. It may be related to one or more types of common measurement error (e.g., information, criterion, occasion, and subject variance). While the study design reduced the potential influence of information and criterion variance, it was not possible to comparably limit occasion or subject variability.
Summary
The TLEQ clearly identified more potential traumatic events than the single-item measure, which resulted in more cases of PTSD. Failure to use the more comprehensive assessment in substance use disordered populations, and likely other clinical populations, is likely to under diagnose PTSD. While comorbid psychiatric disorders often affect the course and outcome of treatment whether or not they are detected, identification of comorbid disorders increase the possibility of mitigating their effects with additional treatment.
Supplementary Material
Acknowledgments
This research was supported by NIH-NIDA grants K23DA015739 (Peirce) and R01DA016375 (Brooner). We thank Ken Kolodner, Sc.D. for his expert statistical support.
Footnotes
Portions of these data were presented at the 2005 meeting of the Association of Behavioral and Cognitive Therapies.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: Author; 1994. [Google Scholar]
- Breslau N. Gender differences in trauma and posttraumatic stress disorder. The Journal of Gender-specific Medicine. 2002;5:34–40. [PubMed] [Google Scholar]
- Breslau N, Kessler RC. The stressor criterion in DSM-IV posttraumatic stress disorder: An empirical investigation. Biological Psychiatry. 2001;50:699–704. doi: 10.1016/s0006-3223(01)01167-2. [DOI] [PubMed] [Google Scholar]
- Brooner RK, King VL, Kidorf M, Schmidt CW, Jr, Bigelow GE. Psychiatric and substance use comorbidity among treatment-seeking opioid abusers. Archives of General Psychiatry. 1997;54:71–80. doi: 10.1001/archpsyc.1997.01830130077015. [DOI] [PubMed] [Google Scholar]
- Cusack K, Falsetti S, De Arellano M. Gender considerations in the psychometric assessment of PTSD. In: Kimerling R, Ouimette P, Wolfe J, editors. Gender and PTSD. New York: The Guilford Press; 2002. pp. 150–176. [Google Scholar]
- Elhai JD, Franklin CL, Gray MJ. The SCID PTSD module's trauma screen: Validity with two samples in detecting trauma history. Depression and Anxiety. 2008;25:737–741. doi: 10.1002/da.20318. [DOI] [PubMed] [Google Scholar]
- Elhai JD, Gray MJ, Kashdan TB, Franklin CL. Which instruments are most commonly used to assess traumatic event exposure and posttraumatic effects?: A survey of traumatic stress professionals. Journal of Traumatic Stress. 2005;18:541–545. doi: 10.1002/jts.20062. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV axis I disorders, research version, patient edition (SCID-I/P) New York: Biometrics Research, New York State Psychiatric Institute; 1998. [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-Mental State: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Franklin CL, Sheeran T, Zimmerman M. Screening for trauma histories, posttraumatic stress disorder (PTSD), and subthreshold PTSD in psychiatric outpatients. Psychological Assessment. 2002;14:467–471. doi: 10.1037//1040-3590.14.4.467. [DOI] [PubMed] [Google Scholar]
- Frans O, Rimmo PA, Aberg L, Fredrikson M. Trauma exposure and post-traumatic stress disorder in the general population. Acta Psychiatrica Scandinavica. 2005;111:291–299. doi: 10.1111/j.1600-0447.2004.00463.x. [DOI] [PubMed] [Google Scholar]
- Goodman LA, Corcoran C, Turner K, Yuan N, Green BL. Assessing traumatic event exposure: General issues and preliminary findings for the stressful life events screening questionnaire. Journal of Traumatic Stress. 1998;11:521–542. doi: 10.1023/A:1024456713321. [DOI] [PubMed] [Google Scholar]
- Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the Life Events Checklist. Assessment. 2004;11:330–341. doi: 10.1177/1073191104269954. [DOI] [PubMed] [Google Scholar]
- King DW, King LA, Erickson DJ, Huang MT, Sharkansky EJ, Wolfe J. Posttraumatic stress disorder and retrospectively reported stressor exposure: A longitudinal prediction model. Journal of Abnormal Psychology. 2000;109:624–633. doi: 10.1037//0021-843x.109.4.624. [DOI] [PubMed] [Google Scholar]
- Kubany ES, Haynes SN, Leisen MB, Owens JA, Kaplan AS, Watson SB, et al. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The traumatic life events questionnaire. Psychological Assessment. 2000;12:210–224. doi: 10.1037//1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- McHugo GJ, Caspi Y, Kammerer N, Mazelis R, Jackson EW, Russell L, et al. The assessment of trauma history in women with co-occurring substance abuse and mental disorders and a history of interpersonal violence. The Journal of Behavioral Health Services & Research. 2005;32:113–127. doi: 10.1007/BF02287261. [DOI] [PubMed] [Google Scholar]
- Mills KL, Lynskey M, Teesson M, Ross J, Darke S. Post-traumatic stress disorder among people with heroin dependence in the Australian Treatment Outcome Study (ATOS): Prevalence and correlates. Drug and Alcohol Dependence. 2005;77:243–249. doi: 10.1016/j.drugalcdep.2004.08.016. [DOI] [PubMed] [Google Scholar]
- Mills KL, Teesson M, Ross J, Peters L. Trauma, PTSD, and substance use disorders: Findings from the Australian national survey of mental health and well-being. The American Journal of Psychiatry. 2006;163:652–658. doi: 10.1176/ajp.2006.163.4.652. [DOI] [PubMed] [Google Scholar]
- Najavits LM, Weiss RD, Reif S, Gastfriend DR, Siqueland L, Barber JP, et al. The Addiction Severity Index as a screen for trauma and posttraumatic stress disorder. Journal of Studies on Alcohol. 1998;59:56–62. doi: 10.15288/jsa.1998.59.56. [DOI] [PubMed] [Google Scholar]
- Nemeroff CB, Bremner JD, Foa EB, Mayberg HS, North CS, Stein MB. Posttraumatic stress disorder: A state-of-the-science review. Journal of Psychiatric Research. 2006;40:1–21. doi: 10.1016/j.jpsychires.2005.07.005. [DOI] [PubMed] [Google Scholar]
- Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. Journal of Consulting and Clinical Psychology. 1993;61:984–991. doi: 10.1037//0022-006x.61.6.984. [DOI] [PubMed] [Google Scholar]
- Roemer L, Litz BT, Orsillo SM, Ehlich PJ, Friedman MJ. Increases in retrospective accounts of war-zone exposure over time: The role of PTSD symptom severity. Journal of Traumatic Stress. 1998;11:597–605. doi: 10.1023/A:1024469116047. [DOI] [PubMed] [Google Scholar]
- Slymen DJ, Ayala GX, Arredondo EM, Elder JP. A demonstration of modeling count data with an application to physical activity. Epidemiologic Perspectives & Innovations. 2006;3:3. doi: 10.1186/1742-5573-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thombs BD, Lewis C, Bernstein DP, Medrano MA, Hatch JP. An evaluation of the measurement equivalence of the Childhood Trauma Questionnaire--Short Form across gender and race in a sample of drug-abusing adults. Journal of Psychosomatic Research. 2007;63:391–398. doi: 10.1016/j.jpsychores.2007.04.010. [DOI] [PubMed] [Google Scholar]
- Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Bulletin. 2006;132:959–992. doi: 10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Keane TM. The criterion A problem revisited: Controversies and challenges in defining and measuring psychological trauma. Journal of Traumatic Stress. 2007;20:107–121. doi: 10.1002/jts.20210. [DOI] [PubMed] [Google Scholar]
- Weaver TL. Method variance and sensitivity of screening for traumatic stressors. Journal of Traumatic Stress. 1998;11:181–185. doi: 10.1023/A:1024477620628. [DOI] [PubMed] [Google Scholar]
- Wyshak G. The relation between change in reports of traumatic events and symptoms of psychiatric distress. General Hospital Psychiatry. 1994;16:290–297. doi: 10.1016/0163-8343(94)90009-4. [DOI] [PubMed] [Google Scholar]
- Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–130. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


