Abstract
Context
Small area differences in health care use between Boston, Massachusetts, and New Haven, Connecticut, are well known. However, we do not know whether factors believed to account for these variations explain differences between other geographic areas.
Objective
To explore differences in health care use between the California counties of Los Angeles (LA) and San Diego.
Method
Medicare data were obtained form the Dartmouth interactive website. In addition, hospital-level data were obtained for the California Office of Statewide Health Planning and Development (OSPHD). Health outcomes and self-reported disease prevalence were estimated from the California Health Interview Survey (CHIS).
Results
Physician supply was comparable between LA and San Diego. Fees per unit service were also equivalent. Hospital beds beds per 10,000 population were 35% higher in LA. Intensity of service use, particularly during the last 2 years of life, was significantly higher in LA, and costs were dramatically higher. Most of the differences were explained by discretionary hospital admissions, end-of-life care, and lower use of hospice care. Quality indicators favor San Diego.
Conclusions
Medical care, particularly at the end of life, is significantly more expensive in LA than in San Diego, yet quality measures tend to favor in San Diego. Non-emergent hospital admissions and inpatient care at the end of life are important contributors to the cost differences. There is little reason to believe that the greater spending for health care in LA results in better patient outcomes.
Introduction
The large difference in service use between Boston, Massachusetts, and New Haven, Connecticut,1–3 is well known, but we do not know if the differences are replicable in other geographically proximal communities. Further, it is worth evaluating whether the common explanations for the Boston-New Haven difference apply in other communities. This paper explores differences in costs of end-of-life care between Los Angeles (LA) and San Diego, California.4
Method
Data sources
Data for this analysis come from several sources. The Dartmouth Atlas of Health Care interactive data tools2,5,6 were used to study all enrollees LA and San Diego counties and Medicare beneficiaries in these counties who died between January 1, 2004 and December 31, 2005. All persons in the decedent analysis were between the ages of 67 and 99 years at time of death. This allowed 2-year follow-back for those becoming eligible for Medicare at age 65 at time of death.
The data are based on Center for Medicare and Medicaid Services (CMS) fee-for- service claims and include demographic data, date of death, acute care discharges, stays in skilled nursing, rehabilitation, psychiatric, and other long-stay facilities, intermediate-, and high-intensity subtypes of intensive care unit stays, physician services for a 20% sample of Medicare beneficiaries, outpatient service use, home health and hospice use, and use of durable medical equipment.
All of decedents had been hospitalized in an acute care hospital at least one time during the last 2 years of their lives and each patient was assigned to a single hospital based on most frequent use. Patients whose only admission was for surgery were assigned to the hospital where they received the surgery, even if most of their other care was associated with other hospital facilities.
We considered costs to Medicare from an administrative perspective. Inpatient costs were estimated from the MedPAR record. In addition to total Medicare costs, they included indirect cost for medical education, disproportionate share payments, and outlier payments. The analysis does not consider costs or copayments from patients.
Claims are aggregated by zip code to create 3436 primary health care markets known as Hospital Service Areas (HSAs). The HSAs are further aggregated into 306 hospital referral regions (HRRs). The HRRs are tertiary service regions that must include at least one hospital that performed major cardiovascular procedures and neurosurgery. We focused on 19 HSAs in LA County and 8 HSAs in San Diego County. For studies of decedents we included 48 LA and 16 San Diego hospitals.
Data on number of hospital beds per community were obtained from the public access California Office of Statewide Health Planning and Development (OSPHD). The UCLA California Health Interview Survey (CHIS) was used to estimate demographic information and insurance status. The Consumer Assessment of Healthcare Providers and Systems Hospital Survey (CAHPS®) and the DHHS Hospital Compare web site (see www.hospitalcompare.hhs.gov) were used to estimate health care quality.
Analysis
For the Dartmouth data on costs per enrollee, HSA served as the unit of analysis. For studies of decedents, the analysis unit was Hospital or HRR. Analysis was conducted at several different levels. Descriptive analysis used means and percentages by county with tests between counties accomplished with t tests or confidence intervals.
Costs were calculated using the Dartmouth interactive data tool with ordinary least-squares adjustments for age, race, gender, primary chronic condition, and whether patients had one or more of nine chronic conditions. The model used crude spending for each component (such as Part A or Part B) as the dependent variable and obtained a predicted cost with the variance associated with each predictor variable removed.
Results
LA and San Diego counties are roughly equivalent in physical size. However, the LA population is about three times as large. Although racial and ethnic composition is similar, San Diego has a higher percentage of white, non-Hispanic residents and fewer black and Hispanic citizens. Median age in the two counties is almost identical and educational attainment is slightly higher in San Diego. 2005 CHIS data show that the percentage of people who visited an emergency room in the last 12 months was nearly identical in LA (18.4%) and San Diego (18.5%). In LA, 85.6% of CHIS respondents reported that they had a usual source of health care, in comparison to 88% in San Diego (differences not statistically significant; Table 1).
Table 1.
Comparison of Los Angeles and San Diego Demographic Profiles, 2006 (Data from U.S. Census Bureau 2007 quickfacts.census.gov/qfd/states/06, Data on Medicare Recipients from CHIS)
| Variable | Los Angeles | San Diego |
|---|---|---|
| Geographic area (square miles) | 4,752 | 4,199 |
| Population | 9,878,554 | 2,974,859 |
| Percent Hispanic | 47.3 (13.8) | 30.3 (3.9) |
| Persons 65 years or older (percent) | 10.4 | 11.1 |
| Percent white, Non-Hispanic | 29.1 (65.3) | 51.4 (84.4) |
| Percent black | 9.5% (6.6%) | 5.5% (3.5%) |
| Percent Asian-Pacific Islander | 13.5 (13.00) | 10.9% (5.8) |
| Percent high school | 69.9 | 82.6 |
| Percent bachelor's degree | 24.9 | 29.5 |
| Median age (2000 years) | 32.0 | 32.2 |
| Median household income (dollars) | 53,494 | 61,724 |
| Persons below poverty (percent) | 14.8 | 11.1 |
Insurance coverage, as estimated from CHIS is similar in the two communities. LA has significantly more uninsured (16% versus 13%, p < 0.05) and Medicaid (16% versus 9%, p < 0.05) patients, and San Diego has a higher portion with employer-based health insurance (58% versus 47%, p < 0.05). The percentage with Medicare-only coverage is identical in the two counties (1.3%) and the percentage with Medicare plus some other insurance is very similar (LA 10.7% versus SD 11.1%, p = NS). Differences between rates of privately purchased insurance (4.9% versus 5.3%) are not significantly different. (Percentages do not at to 100% because some categories are not included. Excluded categories are Healthy Families/CHIP and other public programs. Differences in these excluded categories are nonsignificant.)
Medicare costs
Medicare costs (Parts A and B) for residents of LA and San Diego HSAs in 2005 are summarized in Table 2. LA HSAs are shaded in gray. The lowest-cost LA HSA (Torrence) was more expensive than the highest-cost HSA (La Mesa) in San Diego County. All of the LA communities are higher in Medicare costs than the highest-cost San Diego communities and also higher than the U.S. average for the combination of Part A plus Part B and for total Part B costs. Similar to total costs, there is no overlap in physician payments per enrollee in 2005 (Medicare Part B) between LA and San Diego communities.
Table 2.
Total Medicare Expenditures from Parts A and B as a Ratio of Los Angeles Spending. Dartmouth data
| City name (HSAs) | 2005 Total Medicare (Parts A + B) | Part A % of total |
|---|---|---|
| Tarzana | 13698 | 55 |
| Lynwood | 13369 | 49 |
| Los Angeles | 12638 | 53 |
| Inglewood | 12301 | 60 |
| Fountain Valley | 12211 | 54 |
| Panorama City | 12122 | 55 |
| Glendale | 11830 | 54 |
| Van Nuys | 11813 | 49 |
| Pomona | 11462 | 58 |
| Lancaster | 10734 | 56 |
| Burbank | 10718 | 52 |
| Arcadia | 10551 | 52 |
| West Covina | 10526 | 53 |
| Canoga Park | 10285 | 51 |
| Pasadena | 10217 | 55 |
| Monterey Park | 10150 | 57 |
| Downey | 9519 | 56 |
| Santa Monica | 9144 | 45 |
| Torrance | 8828 | 53 |
| La Mesa | 8708 | 57 |
| Escondido | 8664 | 56 |
| Encinitas | 8296 | 52 |
| San Diego | 7962 | 57 |
| Poway | 7275 | 52 |
| Oceanside | 7215 | 49 |
| Chula Vista | 6610 | 54 |
| La Jolla | 6544 | 48 |
Shaded areas represent Los Angeles County, non-shaded are San Diego County
Capacity
Based on the American Medical Association 2008 report of physician characteristics and distribution, San Diego has a higher density of physicians than LA (26.3 versus 23.5 per 10,000 population). San Diego has more generalists (26.95 versus 21.54), more specialists (13.41 versus 12.61), and more surgeons (4.65 versus 4.29) per 10,000 population than does LA. However, the ratio of generalists to total physicians is comparable: 9% in LA and 10% in San Diego.
Using the Dartmouth database, we estimated that there are more acute hospital beds per 1000 persons in the population in LA (2.15) than in San Diego (1.66). The OSPHD database shows there were 2.56 total beds per 1000 population in LA in comparison to 1.89 per 1000 in San Diego. In other words, LA has about 30% more acute hospital beds according to the Dartmouth database and 35% more according to the OSPHD database.
Price differences
Mean 2005 Medicare Part B payments per physician visit were not significantly higher in LA ($66.00) in comparison to San Diego ($64.00). LA payments were approximately 10% above the national average while in San Diego they were approximately 7% higher than the national average.
Volume
Volume was evaluated using Dartmouth data on physician service use during the last 6 months of life with Hospital as the unit of analysis. The analysis uses the 20% Part B Medicare claims file and was available only for hospitals with at least 400 deaths. Hospitals with less than 400 deaths were not used in order to preserve both patient confidentiality and to increase the precision of the estimates. This left a sample of 48 LA hospitals and 16 San Diego hospitals. Total physician visits were 81% higher in LA and specialist visits were more than twice as high in LA. Primary care visits were 52% higher, while the number of physicians seen in the last six months of life was about 11% higher (all p < 0.001; Table 3).
Table 3.
Mean and (Standard Error) for Volume in Los Angles and San Diego Hospitals: Dartmouth Data, Medicare Part B
| Variable | Los Angeles | San Diego | t value | Ratio |
|---|---|---|---|---|
| Total physician visits per decedent during the last 6 months of life (2001–2005) | 64.44 (2.49) | 35.48 (1.85) | 9.32a | 1.81 |
| Medical specialist visits per decedent during the last 6 months of life (2001–2005) | 39.45 (1.78) | 18.62 (1.32) | 9.38a | 2.11 |
| Primary care physician visits per decedent during the last 6 months of life (2001–2005) | 21.53 (.87) | 14.11 (.88) | 5.96a | 1.52 |
| Number of different physicians seen per decedent during the last 6 months of life (2001–2005) | 9.99 (.15) | 9.02 (.22) | 3.51a | 1.11 |
P < 0.001.
Note: Hospital is unit of analysis
Intensity
The Dartmouth Hospital Care Intensity Index combines hospital days and number of inpatient physician encounters with adjustments for age, gender, race, and illness. During the last 6 months of life, mean intensity in the 48 LA hospitals was higher (M = 92.74, SD = 7.67) than in 16 San Diego hospitals (M = 57.72, SD = 22.22; p < 0.001).
Variation by diagnosis and procedure
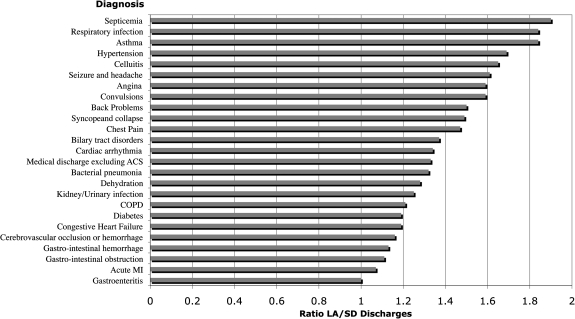
The ratios of LA/San Diego hospital discharges per 1000 Medicare enrollees for 25 common diagnoses are shown in Figure 1. For acute and serious medical problems, such as gastroenteritis, acute myocardial infarction, GI obstruction or hemorrhage, or cerebrovascular occlusion/hemorrhage, there is very little variation between LA and San Diego. On the other hand, there was substantial variability for problems such as respiratory infections, asthma, or hypertension. For these conditions, LA patients are 70%–84% more likely to be hospitalized in comparison to San Diego patients.
FIG. 1.
Ratio of LA/San Diego discharges per 100,00 Medicare enrollees by diagnosis. Dartmouth 2005 data.
End-of-life costs and hospice use
We created ratios of Medicare costs in the last 2 years of life for LA, San Diego, and the U.S. average. Considering Medicare decedents, LA is 22% higher than San Diego in discharges and 42% higher in total costs. Table 4 summarizes end-of-life care in LA and San Diego. In San Diego, 44.6% of decedents were enrolled in hospice during the last 6 months of life in comparison to 22.4% in Los Angeles. The LA enrollment rate is near the 10th percentile nationwide while the San Diego enrollment rate exceeds the 90th percentile (44.7%). In LA the average number of hospice stays during the last 6 months (8.4) was significantly lower than in San Diego (17.0). LA exceeds the 90th percentile of deaths occurring in the hospital (30.4%) while San Diego is well below the national average in this category (national average = 31.7%).
Table 4.
Differences between Los Angeles and San Diego Patients for End-of-Life Care
| Measure | Los Angeles | San Diego |
|---|---|---|
| Hospice days per decedent during the last 6 months of life | 8.4 | 17.0 |
| Percent of decedents enrolled in hospice during the last 6 months of life | 44.6% | 22.4% |
| Hospital care intensity index, last 2 years of life, by component | 1.80 | 0.97 |
| Inpatient days per decedent during the hospitalization in which death occurred, by level of care intensity | 4.29 | 2.45 |
| Percent of deaths associated with ICU admission (2001–2005) | 30.2% | 21.1% |
| Percent of deaths occurring in hospital (2001–2005) | 39.4% | 28.7% |
ICU, intensive care unit.
LA is 78% higher than San Diego for ICU/CCU costs per decedent, 53% higher for inpatient reimbursement, and 65% higher for number of hospital days during the last 6 months of life and Medicare reimbursement during last 6 months of life. Although San Diego costs are almost twice the national average for ICU/CCU costs during the last 6 months of life, they remain close to the national average for other categories. LA, which is 3.5 times higher than the national average for ICU/CCU costs, is also 93% higher for inpatient reimbursement and 72% higher for total Medicare costs during the last 6 months of life. Hospice costs per decedent in San Diego are about twice as high ($2,810.00) as in LA ($1,327.00). Conversely, inpatient costs are 70% higher in LA ($25,920.00 versus $15,192.00). Because inpatient costs can be as much as ten times higher than hospice costs, total costs are about 50% higher in LA.
Quality of care
CMS Hospital Compare selected two indicators for publication in various American newspapers and we used the same measures for our comparison. The two indicators are (1) the percentage of people who received antibiotics one hour before surgery and (2) the percentage of people who always received help when they wanted it.
With 51 LA and 13 San Diego hospitals reporting to the system (with hospital as the unit of analysis), appropriate antibiotic use prior to surgery was more common in San Diego (M percentage = 84.69, SD = 12.89) than in LA (M = 81.55, SD = 13.80), although the difference was not statistically significant (t62 = 0.74, p = 0.46). For percentage of patients always receiving help when requested, San Diego hospitals (M = 55.25, SD = 5.25) performed significantly better than LA hospitals (M = 50.68, SD = 5.93: t62 = 2.53, p = 0.014).
The Dartmouth database includes four CMS quality indicators for clinical care. (The Dartmouth Group considers three indicators of quality of care. Propensity to refer patients is measured by the percentage of patients who had seen ten or more physicians during the last six months of life. High scores on this measure suggest poor continuity of care. Aggressiveness of care is indexed by the percentage of deaths occurring during a hospitalization that involved one or more ICU stay. The third index of quality care is based on quality indicators taken from the CMS Hospital Compare web site. The Dartmouth Group uses five measures for managing acute myocardial infarction (AMI), two for congestive heart failure (CHF), and three for the management of pneumonia. A composite score was created using the average of the three condition-specific summary scores weighted by the number of cases. Hospital scores were provided only for those institutions where there were 25 or more eligible patients. More details of the methodology are available in the Appendix to the 2005 Dartmouth atlas of health care.) For each of these, quality scores in San Diego hospitals are slightly higher, although the differences are very small (acute myocardial infarction: 92.26 versus 90.87; congestive heart failure: 86.00 versus 85.36; pneumonia care: 70.45 versus 69.70; overall composite: 84.46 versus 83.42).
Discussion
In their classic analysis, Wennberg and colleagues7 showed that Medicare spent significantly more per recipient in Boston than in New Haven.8 Our analysis suggests that the contemporary differences between San Diego and LA far exceed the contrast between Boston and New Haven. Today, Medicare costs per decedent for inpatient hospitalizations during the last 6 months of life are slightly lower in Boston than in New Haven. On the West Coast, end-of-life inpatient hospital costs are 65% higher in LA in comparison to San Diego. Hospital days per decedent during the last 6 months of life are now nearly identical in Boston and New Haven. However, LA is 50% higher than San Diego.
The effects described here are not subtle. For most measures, there is no overlap in mean costs between Los Angeles and San Diego HSAs. Many of the explanations for variations in health care utilization seem not to apply to the LA–San Diego differences. LA does not have an excess capacity of providers in comparison to San Diego. It has been argued that costs are best controlled by higher ratios of primary care physicians to specialists.9 Yet, the proportion of physicians trained in primary care is also very similar across these two communities. The cost per unit of service does not differ significantly across the two counties.
Furthermore, the disease burden in the two areas appears to be approximately equal. However, consistent with the argument that excess capacity drives costs,10 LA has about 35% more hospital beds per 10,000 persons in the population.
What differs is the volume and intensity of services, particularly at the end of life. San Diego residents are significantly more likely to die with the assistance of hospice services and less likely to spend time in hospitals and intensive care units during the last two years of life. LA patients have significantly more visits with the same specialists and primary care doctors and LA residents face more intensive and aggressive care.
In health care, we often assume that more is better.1 If more is being spent on LA patients, it might be assumed that they are getting higher quality service. Our observation of equal quality in the two counties is consistent with other analyses showing that University of California medical centers in San Diego and Los Angeles perform quite comparably for summary quality measures for acute MI and congestive heart failure. UCSD has a higher quality score than UCLA for treatment of pneumonia (62.3 versus 52.3). At this point, we have no reason to believe that the quality of service received by LA patients is better.
Demographic and poverty differences between the Southern California communities remain an important rival explanation for our results. LA has a higher percentage of uninsured patients, more African American, and more Hispanic residents. Cooper suggests that costs are higher in zip codes where poverty and uninsured rates are also high.12 However, this report focuses on Medicare recipients. In this group, there are no uninsured, and the age distributions in LA and San Diego are very similar. We cannot rule out the possibility that the consequences of previous lack of insurance contribute to the greater demand in LA. However, lack of health insurance does not explain our findings.
Although the Dartmouth cost reports are adjusted for demographic variables, these models may still underadjust. Thus, results will need to be interpreted cautiously. In order to investigate whether excess capacity might explain the high costs in LA, we considered a third California county. San Bernardino is a community of 2,007,800 residents, which almost exactly matches LA on percentages white/non-Hispanic, African American, and income. Median education levels in San Bernardino are lower than LA. If costs are dominated by demographic variables, LA and San Bernardino should be similar. But end-of-life costs per decedent are very similar in San Bernardino ($30,950.00) and San Diego ($28,768.00), and both are lower than LA ($43,294.00).
This research has a significant number of limitations and we can only address a few of the issues and concerns here. End-of-life care is a major driver of costs, but we only know a death has occurred after the fact. Survival patterns in the two markets could dramatically affect the results if LA did a better job keeping very sick patients alive.13 Although this remains a concern, it is worth noting that the OSPHD data on nondecedents indicates a similar pattern of high costs in LA and we found no evidence that mortality patterns differ in the two counties.
One potential explanation for the difference is that in the mid-1990s HMO penetration in San Diego was much greater than Los Angeles and this may have affected practice styles. However, 2007 HMO penetration was nearly identical in the two counties (LA 42% versus SD 43%) and PPO penetration was the same (20% in each county). However, 80% of the care in San Diego is given by just five major provider groups, and two large groups each have about 25% market share. In Los Angeles, no group has more than 10% of the market, and the top five groups account for only 35% of the care.14,15 Thus, incentives within medical groups may play an important role in understanding the differences.
Another limitation is that the physician density and specialty data may be affected by Medicare's Part B Geographic Practice Cost Index (GPCI or "gypsy") adjustment. Physicians in San Diego are currently suing CMS because their GPCI is 7% lower than in Santa Clara, California. However, GPCI differences between LA and San Diego are much less than 7% and even a 7% difference could explain only a fraction of the LA–San Diego cost differences. We also considered differences in the Medicare Area Wage Index (MAWI) for LA County versus San Diego County. According to the CMS web site, the most recent hourly wage reported in the MAWI was in 2005: $29.86 in San Diego and $30.95 in LA. Both counties are at the high end of the national distribution. The differences are quite small and Medicare payment adjustments based on MAWI cannot explain the observed differences.
In summary, the most plausible explanation for the LA–San Diego cost differences is greater discretionary use of the hospital as a site of care, owing to a greater per-capita supply of hospital beds. Furthermore, San Diego patients are much more likely to die with the assistance of hospice care and as a result their costs are lower and the quality of care they receive may be higher. The LA system creates more work and more expense without a clear health outcome advantage for the people it serves.
Acknowledgments
This paper was completed while the author was a resident scholar at the Rockefeller Foundation Bellagio Study Center.
Support was also provided by NIH grants 1 P01 AG020679-01A2, UCLA Claude D. Pepper Older Americans Independence Center, NIH/NIA 5P30AG028748, and CDC grant U48 DP000056-04.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Wennberg JE. Small area analysis, the medical care outcome problem. Paper presented at: Research Methodology: Strengthening Causal Interpretations of Nonexperimental Data; Rockville MD. 1990. [Google Scholar]
- 2.Wennberg JE. The Dartmouth Atlas of Health Care in the United States. Hanover, NH: Trustees of Dartmouth College; 1998. [Google Scholar]
- 3.Wennberg JE. Fisher ES. Skinner JS. Geography and the debate over Medicare reform. Health Aff (Millwood) 2002:W96–114. doi: 10.1377/hlthaff.w2.96. Supp Web Exclusives. [DOI] [PubMed] [Google Scholar]
- 4.Wennberg JE. Fisher ES. Baker L. Sharp SM. Bronner KK. Evaluating the efficiency of California providers in caring for patients with chronic illnesses. Health Aff (Millwood) 2005:W526–543. doi: 10.1377/hlthaff.w5.526. Suppl Web Exclusives. [DOI] [PubMed] [Google Scholar]
- 5.Flores G. Tomany-Korman SC. Racial and ethnic disparities in medical and dental health, access to care, and use of services in US children. Pediatrics. 2008;121:e286. doi: 10.1542/peds.2007-1243. [DOI] [PubMed] [Google Scholar]
- 6.Wennberg JE. Fisher ES. Goodman DC. Skinner JS. Hanover NH: Dartmouth Institute for Health Policy and Clinical Practice; 2008. Tracking the Care of Patients with Severe Chronic Illness: The Dartmouth Atlas Of Health Care. [PubMed] [Google Scholar]
- 7.Wennberg J. Gittelsohn A. Variations in medical care among small areas. Sci Am. 1982;246:120–134. doi: 10.1038/scientificamerican0482-120. [DOI] [PubMed] [Google Scholar]
- 8.Wennberg JE. Freeman JL. Culp WJ. Are hospital services rationed in New Haven or over-utilised in Boston? Lancet. 1987;1:1185–1189. doi: 10.1016/s0140-6736(87)92152-0. [DOI] [PubMed] [Google Scholar]
- 9.Starfield B. Birn AE. Income redistribution is not enough: Income inequality, social welfare programs, and achieving equity in health. J Epidemiol Community Health. 2007;61:1038–1041. doi: 10.1136/jech.2006.054627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fisher E. Bynum J. Skinner J. Slowing the frowth of health care costs: Lessons from regional variation. N Engl J Med. 2009;306:849–882. doi: 10.1056/NEJMp0809794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fisher ES. Welch HG. Could more health care lead to worse health? Hosp Pract (Off Ed) 1999;34:15–16. doi: 10.1080/21548331.1999.11443939. , 21–12, 25 passim. [DOI] [PubMed] [Google Scholar]
- 12.Cooper RA. States with more physicians have better-quality health care. Health Aff (Millwood) 2009;28:w91–102. doi: 10.1377/hlthaff.28.1.w91. [DOI] [PubMed] [Google Scholar]
- 13.Ong MK. Mangione CM. Romano PS. Zhou Q. Auerbach AD. Chun A. Davidson B. Ganiats TG. Greenfield S. Gropper MA. Malik S. Rosenthal JT. Escarce JJ. Looking forward, looking back: Assessing variations in hospital resource use and outcomes for elderly patients with heart failure. Circ Cardiovasc Qual Outcomes. 2009;2:548–557. doi: 10.1161/CIRCOUTCOMES.108.825612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.San Diego Market Analysis HealthLeaders-InterStudy. A Decision Resources. Nashville: 2009. [Google Scholar]
- 15.Los Angeles Market Analysis. HealthLeaders-InterStudy, A Decision Resources. Nashville: 2009. [Google Scholar]