Abstract
Background
Few studies have examined proxy decision-making regarding end-of-life treatment decisions. Proxy accuracy is defined as whether proxy treatment choices are consistent with the expressed wishes of their index elder. The purpose of this study was to examine proxy accuracy in relation to two family factors that may influence proxy accuracy: perceived family conflict and type of elder-proxy relationship.
Methods
Telephone interviews with 202 community-dwelling elders and their proxy decision makers were conducted including the Life-Support Preferences Questionnaire (LSPQ), and a measure of family conflict, and sociodemographic characteristics, including type of relationship.
Results
Elder-proxy accuracy was associated with the type of elder-proxy relationship. Adult children demonstrated the lowest elder-proxy accuracy and spousal proxies the highest elder-proxy accuracy. Elder-proxy accuracy was associated with family conflict. Proxies reporting higher family conflict had lower elder-proxy accuracy. No interaction between family conflict and relationship type was revealed.
Conclusions
Spousal proxies were more accurate in their substituted judgment than adult children, and proxies who perceive higher degree of family conflict tended to be less accurate than those with lower family conflict. Health care providers should be aware of these family factors when discussing advance care planning.
Introduction
End-of-life (EOL) care in the United States has been increasingly studied since the passage of the Patient Self-Determination Act (PSDA) in 1990 and the landmark SUPPORT Study in 1995.1,2 Specifically, clear decision-making by patients, their families, and health care teams has been identified as an important component of a “good death” experience.3 Unfortunately, many people are unable to participate in their own treatment decisions at the end of their lives because of a variety of end-stage conditions, such as coma or delirium, leaving them without decision-making capacity. Thus, treatment decisions at the EOL often fall to the closest family member by next-of-kin determination or legally designated surrogate decision makers.4 The term “proxy” decision-maker will be used throughout this article referring to both formal and informal family decision-makers.
Studies examining the accuracy of proxy decision-makers have found it to be highly variable. Proxy accuracy is defined as whether proxy treatment choices are consistent with the expressed wishes of their index elder. Early studies found that proxy accuracy was approaching chance, with accuracy rates of 50%–64%.5–7 Recent studies have documented slightly higher degrees of accuracy ranging from 68%–74%.8,9 The reasons for this variability in proxy accuracy between older and newer studies are not clearly understood.
Prior research has investigated factors influencing proxy accuracy with varied results. Proxy gender has not yielded consistent findings.9–11 Neither the presence of a formal Durable Power of Attorney for Healthcare (DPAHC) or an advance directive influenced the degree of accuracy.11,12 In one study, race did not effect proxy accuarcy.13 The literature on whether proxy relationship influences proxy accuracy has produced mixed findings.8,14–16
What accounts for low proxy accuracy in EOL treatment preferences? Some speculation has centered on family disagreement, especially conflict surrounding the elder relative's care. Such conflict could explain low proxy accuracy because pressure from other family members may weigh more heavily on proxies than on patients themselves. The patient's right to make decisions about his or her own care is widely recognized. But for family proxies, the need to consider the wishes of other family members may pose a barrier to clear decision-making. A proxy may be reluctant to withhold or withdraw life-prolonging measures on behalf of an incapacitated relative because of anticipated or actual disapproval from others or fear of offending them. Such social pressures or conflicts would result in stronger preferences for life-prolonging treatments by proxies than by patients themselves and may influence proxy accuracy in EOL care preferences.
Family conflict helps to explain why families in disagreement are more likely to chose life-prolonging care for incapacitated relatives. In Kaufman's qualitative study of death in the two U.S. hospitals, she observed that families in conflict about the care of a hospitalized relative were more likely to opt for aggressive care.21 Similarly, Winter and Parks in 2008 found higher family conflict to be associated with stronger preferences for life-prolonging care among family proxies of community-dwelling individuals with dementia. Family conflict may therefore have a negative impact on the adequacy of substituted judgment and help explain proxy inaccuracy in representing their relatives' treatment preferences.
Furthermore, this conflict may be greater for some types of proxies than for others. Spousal proxies may be less vulnerable to pressure from other family members than adult children or other types of proxies. Therefore, we examined both family conflict and type or relationship to determine whether these factors may influence treatment preferences and whether they may interact to affect proxy accuracy.
Methods
Participants
Participants were 202 elder-proxy pairs (404 total study subjects). Elders were defined as age 70 and over. Proxies were named by the elder and did not require a legal designation of DPAHC. A proxy was defined as an individual whom the elder would choose to make health care decisions on his/her behalf if he/she were unable to make such decisions. Elders were recruited into the study through a variety of sources selected to reach a representative sample of elders. These included two senior centers, two senior housing developments, and two area continuing care retirement communities, display ads, and mailings to patients of two family medicine practices. Both elders and proxies were cognitively intact with an average age of 79 years for the elders and 60 for the proxies. Characteristics of the elders and proxies are displayed in Table 1.
Table 1.
Characteristics of Sample
| |
Elders |
Proxies |
||
|---|---|---|---|---|
| Percentage | Mean (SD) | Percentage | Mean (SD) | |
| Age | 78.9 (6.2) | 59.6 (13.6) | ||
| Gender (% female) | 73.0 | 71.8 | ||
| Race | ||||
| White | 62.0 | 65.3 | ||
| Non-white | 38.0 | 34.7 | ||
| Religious affiliation | ||||
| Protestant | 49.0 | 41.6 | ||
| Catholic | 15.8 | 17.3 | ||
| Jewish | 25.7 | 21.3 | ||
| Other | 3.6 | 6.4 | ||
| None | 5.9 | 13.4 | ||
| Years of education | ||||
| High School or less | 28.0 | 18.3 | ||
| Some college | 29.0 | 20.8 | ||
| College degree | 23.0 | 28.2 | ||
| Postgrad degree | 20.0 | 32.7 | ||
| Financial difficultya | 0.90 (0.98) | 0.95 (0.95) | ||
| Marital status (% married) | 23.0 | 58.4 | ||
| Relationship to elder | ||||
| Wife | 14.4 | |||
| Husband | 11.4 | |||
| Daughter | 40.1 | |||
| Son | 14.4 | |||
| Other | 19.7 | |||
Financial well-being scale measures difficulty paying for basics like food, housing, medical care, etc. Scale from 0 (not at all difficult) to 3 (extremely difficult). The mean value of 0.90 represents “Not very difficult.”
SD, standard deviation.
Measures
Preferences for life-prolonging treatments
Treatment preferences were measured using the Life Support Preferences Questionnaire (LSPQ).23 This instrument elicits ratings of preferences for four medical treatments for acute life-threatening conditions: antibiotics, gallbladder surgery, cardiopulmonary resuscitation (CPR), and tube feeding. For each treatment, a preference is elicited in the context of seven hypothetical health scenarios that vary in severity, prognosis, and level of pain, and a scenario for “current health.” Participants consider their preferences for life-prolonging treatment in the context of each specific scenario, rather than in the abstract. The seven scenarios are presented in Appendix A. Elder and proxy treatment preferences were elicited on 5-point acceptability ratings from 0 (not at all) to 4 (very much).
Interviewers instructed proxies to use the ethical principle of substituted judgment as the method of decision-making.24 Each proxy was told: “I would like you to respond to these questions as if you had to make decisions on behalf of (name of relative), because s/he is unable to speak for himself or herself. Please base your decision on what you think (the relative) would want. If you are not sure what (the relative) would want, please make your best guess.”
Type of elder-proxy relationship
Elders identified their proxies' relationship to them. These were coded as follows: spouse = 1, adult child = 2, or other relationship = 3. Proxies who were not related to the elder were grouped with “other relationship.”
Family conflict
The authors' measure of proxy-reported family conflict regarding care decisions was used.22 The proxy identified each relative (aside from him/herself) who would be involved in decision-making for the elder, then rated how important this person's opinions were on a 0–6 scale. The degree to which the proxy and this person agreed on the patient's treatment was also scored on a 0–6 scale (0 = no agreement/6 = total agreement). For each relative named by the proxy, his/her 0–6 agree-disagree rating was weighted by the importance of the individual's opinions. The mean across all relatives was calculated. Thus, the family conflict score was the mean of the product of importance × disagreement (theoretical range, 0–36) across all relatives potentially involved in care decisions for the elder. Family conflict scores ranged from 0 to 31.2, with a mean score of 7.20 (standard deviation [SD] = 7.77). The distribution was positively skewed (skewness = 0.729, SD = 0.171), with 23.3% of proxies reporting no family conflict. Because of this skewed distribution, a dichotomous family conflict variable was created using a median split (7.2). Scores of 7.2 or larger were considered high conflict families, those less than 7.2 low conflict.
Cognitive status
Cognitive status was assessed using a telephone version of the Mini-Mental State Exam.25 Possible scores range from 0 to 23, with 23 indicating no errors. All participants scored in the cognitively intact range (17 or higher), with a mean of 21.4 (SD = 1.6).
Demographic characteristics
For both elder and proxy, age, race, gender, years of education, occupation, financial difficulty, and marital status were elicited (Table 1).
Procedure
Interested elder participants called the office or returned a stamped self-addressed postcard and were contacted by telephone. A trained interviewer explained the study and confirmed the person's eligibility by age and willingness to participate. Informed consent was obtained using an Institutional Review Board-approved verbal consent script. The 35-minute interview was conducted by telephone. Proxies were contacted and interviewed separately. All participants were offered a $25 honorarium.
Data analysis
Elder-proxy accuracy in treatment preferences
For each treatment (antibiotics, CPR, gallbladder surgery, and tube feeding) in each scenario, a score was computed representing the difference between the proxy preferences and the elder preference. This yielded 28 difference scores. The larger the difference, the lower the elder-proxy accuracy.
Elder-proxy accuracy in relation to family conflict and type of relationship
Proxy-elder difference scores were examined in an analysis of covariance (ANCOVA) model, with repeated measures on the seven health scenarios and four types of treatments. The between-subjects independent variables were family conflict and type of elder-proxy relationship (spouse, adult child, or other). Post hoc least significant difference (LSD) tests were conducted on all pairs of relationship type.
Results
Type of family relationship
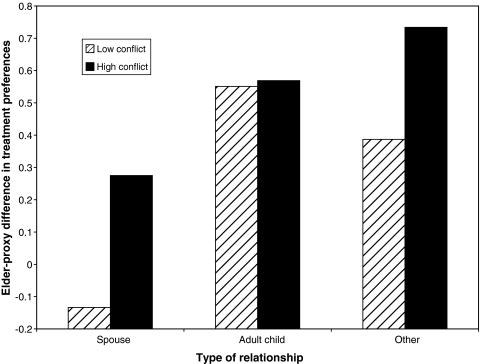
Elder-proxy accuracy was associated with the type of elder-proxy relationship (F[2,198] = 4.479, p = 0.013). Adult children demonstrated the lowest elder-proxy accuracy (mean = 0.56, SD = 1.00), spousal proxies the highest elder-proxy accuracy (mean = 0.10, SD = 0.94). Other proxies had a mean difference score of 0.46 (SD = 1.13). Post hoc LSD test results showed that spouses demonstrated significantly higher elder-proxy accuracy than adult children (p = 0.007) and marginally higher accuracy than other proxies (p = 0.085). Accuracy for adult children versus other proxies did not differ (p = 0.617; Fig. 1).
FIG. 1.
Proxy-elder discordance by type of relationship (spouse, adult child, other) for families with high versus low conflict.
Family conflict
Elder-proxy accuracy was associated with family conflict (F[1,198] = 4.479, p = 0.036). Proxies reporting higher family conflict showed lower elder-proxy accuracy (Fig. 1). No main effect was found for health scenario (F[6,193] = 1.748, p = 0.112), and a marginal main effect was found for treatment type (F[3,196) = 2.155, p = 0.095). Similarly, no interaction effects emerged for scenario by either family conflict (F[6,193) = 1,544, p = 0.166) or elder-proxy relationship (F[112, 388) = 0.795, p = 0.656), or for treatment type by family conflict (F[3,196] = 0.925, p = 0.430) or elder-proxy relationship (F[6,394] = 0.646, p = 0.694).
Interaction between family conflict and type of relationship
No interaction was found between type of family relationship and degree of family conflict (F[2,196] = 0.850, p = 0.429). This indicates that degree of family conflict was independent of type of elder-proxy relationship.
Figure 1 presents proxy-elder differences by type of relationship (spouse, adult child, other) for high- and low-conflict families.
Discussion
The two family-centered factors assessed in this study emerged as independent influences of the degree of elder-proxy accuracy. The first family factor, the type of family relationship of the proxy to the elder, was predictive of the magnitude of elder-proxy accuracy, indicating that the lowest degree of elder-proxy accuracy was observed when an adult child was the proxy decision-maker. Additionally, the highest elder-proxy accuracy was found for spousal proxies. Other work around the type of family relationship has failed to yield consensus around the type of family proxy with the highest degree of accuracy. This study's findings support the notion that spousal proxies are likely to have the highest degree of accuracy in hypothetical decision-making.
We also found that higher family conflict (as reported by the proxy) was negatively associated with proxy accuracy. This finding confirms prior work showing that proxies who perceived higher degree of family conflict were more likely to chose life-prolonging therapies.14 The current study adds to that work by analyzing the elder-proxy pairs and demonstrating that perceived family conflict is associated with lower elder-proxy accuracy with treatment preferences.
Limitations of this study include the relatively high educational levels and socioeconomic backgrounds of elders and proxies. They were also a volunteer sample who had a proxy willing to participate. These considerations may make the sample less representative of the elder population. Additionally, although the elders were asked not to discuss the topic of our interview with their proxy prior to our interview with them, we could not confirm that they had not had such a discussion. If a discussion was had between that interval, that could contaminate our results. Also, questions in this study were posed using hypothetical scenarios rather than in real time. However, it should be kept in mind that all advance care planning is done with hypothetical scenarios.
Fortunately, an increasing numbers of Americans complete advance directives.27,28 Nevertheless, health care providers still must work with proxies. These study findings have clear clinical and research applications. The advances in the palliative care movement in the United States have led to a call for more nuanced advance care planning. The findings from this study underscore the importance of an advance care planning process with a family-centered approach. This study shows that family conflict should be assessed by health care teams during the end of life decision-making process. If conflict is reported by a proxy decision maker, health care teams should consider addressing this conflict in an effort to enhance proxy accuracy in decision-making. Also needed is further study of ways to successfully engage proxies in the process of advance care planning. Similarly, new tools for advance directives should be developed for decision-making by families rather than the current legal format of naming a single durable POA.
Additional research in end-of-life decision-making is needed to analyze the decision-making process as it occurs in real time (i.e., when a decisionally incapacity patient is seriously ill) and develop tools for health care teams to provide family-centered counseling and decision-making at the end of life.
Appendix A.
Life Support Preference Questionnaire–Elder Version; Seven Health Scenarios23
| 1. Current state of health. You are in your current state of health. |
| 2. Alzheimer's disease. You have trouble remembering things and thinking clearly. You cannot recognize people you know, make decisions for yourself, or communicate. You have no chance of recovery. Your mental abilities may get worse quickly or may stay the way they are now for a long time. Your physical condition and abilities are unaffected. |
| 3. Constant shortness of breath as result of a condition such as congestive heart failure, emphysema, or chronic obstructive pulmonary disease (COPD). You are unable to climb stairs or walk more than a few feet. Your medical condition cannot improve. Your condition may get worse very quickly or slowly decline over several years. Your ability to think, reason, and remember is unaffected. |
| 4. Severe stroke: You have suffered a severe stroke and have been in a coma for 6 weeks. In the opinion of the doctor, you have no chance for regaining awareness. Your current physical condition is stable but will slowly decline over time. You rely on others for help with feeding, bathing, dressing, and toileting. You may live in this condition for several years. |
| 5. Moderately severe stroke. One arm and leg are paralyzed. You have trouble speaking and trouble understanding when others speak. You rely on others for help with feeding, dressing, bathing and toileting. In the opinion of your doctor, you have a very slight chance of improvement. |
| 6. Colon cancer that has spread to the liver, no pain. You are tired and weak. Your thinking and memory are unaffected. You are not in pain. In the opinion of your doctor, you have no chance of recovery. Your doctor estimates that you have about 6 months to live. |
| 7. Colon cancer that has spread to the liver, with pain. You are tired and weak. Your thinking and memory are unaffected. You have pain that requires the constant use of medication. In the opinion of your doctor, you have no chance of recovery. Your doctor estimates that you have about 6 months to live. |
Acknowledgments
This work was supported by National Institute of Nursing Research grant #R21NR010263. This work was presented as a poster at the AGS Annual Symposium in 2010. It was published in abstract form in JAGS. The citation is: Parks S, Winter L, Santana A et al: Family conflict, type of proxy, and proxy decision making for end-of-life treatments. JAGS 2010;58:591.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Patient Self-Determination Act of 1990. www.fha.org/acrobat/Patient%20Self%20Determination%20Act%201990.pdf. [Jan 15;2010 ]. www.fha.org/acrobat/Patient%20Self%20Determination%20Act%201990.pdf
- 2.SUPPORT Investigators. A controlled trial to improve care for seriously ill hospitalized patients in the Study to Understand Prognoses and Preferences for Outcomes and Risk of Treatments. JAMA. 1995;274:1591–1598. [PubMed] [Google Scholar]
- 3.Steinhouser KE. Clipp EC. McNeilly M. Christakis NA. McIntyre LM. Tulsky JA. In search of a good death: Observations of patients, families and providers. Ann Intern Med. 2000;132:825–832. doi: 10.7326/0003-4819-132-10-200005160-00011. [DOI] [PubMed] [Google Scholar]
- 4.Sabatino CP. The legal and functional status of the medical proxy: Suggestions for statutory reform. J Las Med Ethics. 1999;27:52–68. doi: 10.1111/j.1748-720x.1999.tb01436.x. [DOI] [PubMed] [Google Scholar]
- 5.Barrio-Cantelejo IM. Molina-Ruiz A. Simon-Lorda P, et al. Advance directives and proxies' predictions about patients' treatment preferences. Nurs Ethics. 2009;16:93–109. doi: 10.1177/0969733008097995. [DOI] [PubMed] [Google Scholar]
- 6.Fagerlin A. Ditto PH. Danks JH. Houts RM. Smucker WD. Projection in surrogate decisions about life-sustaining medical treatments. Health Psychol. 2001;20:166–175. [PubMed] [Google Scholar]
- 7.Smucker WD. Houts RM. Danks JH. Ditto PH. Fagerlin A. Coppola KM. Modal preferences predict elderly patients life-sustaining treatment choices as well as patients' chosen surrogates do. Med Decis Making. 2000;20:271–280. doi: 10.1177/0272989X0002000303. [DOI] [PubMed] [Google Scholar]
- 8.Shalowitz D. Garrett-Mayer E. Wendler D. The accuracy of surrogate decision makers. Arch Intern Med. 2006;166:493–497. doi: 10.1001/archinte.166.5.493. [DOI] [PubMed] [Google Scholar]
- 9.Zettel-Watson L. Ditto P. Danks JH. Smucker WD. Actual and perceived gender differences in the accuracy of surrogate decisions about life-sustaining medical treatment among older spouses. Death Stud. 2009;32:273–290. doi: 10.1080/07481180701881230. [DOI] [PubMed] [Google Scholar]
- 10.Bar-Tal Y. Barnoy S. Zisser B. Whose informational needs are considered? A comparison between cancer patients and their spouses' perceptions of their own and their partners' knowledge and informational needs. Soc Sci Med. 2005;60:1459–1465. doi: 10.1016/j.socscimed.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 11.Moorman SM. Hauser RM. Carr D. Do older adults know their spouses' end-of-life treatment preferences? Res Aging. 2009;31:463–491. doi: 10.1177/0164027509333683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ditto PH. Danks JH. Smucker WD, Bookwala J, Coppola KM, Dresser R, Fagerlin A, Gready RM, Houts RM, Lockhart LK, Zyzanski S: Advance directives as acts of communication: A randomized controlled trial. Arch Intern Med. 2001;161:421–430. doi: 10.1001/archinte.161.3.421. [DOI] [PubMed] [Google Scholar]
- 13.Pruncho R. Cartwright FP. Wilson-Genderson M. The effects of race on patient preferences and spouse substituted judgments. Int J Aging Hum Dev. 2009;69:31–54. doi: 10.2190/AG.69.1.c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ouslander JG. Tymchuk AJ. Rahbar B. Health care decisions among elderly long-term care residents and their potential proxies. Arch Intern Med. 1999;149:1367–1372. [PubMed] [Google Scholar]
- 15.Seckler AB. Meier DE. Mulvihil M. Paris BE. Substituted judgment: how accurate are proxy predictions? Ann Intern Med. 1991;115:92–98. doi: 10.7326/0003-4819-115-2-92. [DOI] [PubMed] [Google Scholar]
- 16.Uhlmann RF. Pearlman RA. Cain KC. Physicians' and Spouses' predictions of elderly patients' resuscitation preferences. J Gerontol. 1988;43:M115–M121. doi: 10.1093/geronj/43.5.m115. [DOI] [PubMed] [Google Scholar]
- 17.National Consensus Project for Quality Palliative Care (US) Clinical practice guidelines for quality palliative care. Brooklyn, NY: National Consensus Project for Quality Palliative Care; 2004. [DOI] [PubMed] [Google Scholar]
- 18.National Institutes of Health (US) Improving End-of-Life Care. Proceedings of the State-of-the-Science Conference; Washington, D.C.. Dec 6–8;2004 ; [Google Scholar]
- 19.Kramer BJ. Christ GH. Bern-Klug M. Francoeur RB. A national agenda for social work research in palliative and end of life care. Palliat Med. 2005;8:418–431. doi: 10.1089/jpm.2005.8.418. [DOI] [PubMed] [Google Scholar]
- 20.Breen CM. Abernathy AP. Abbott KH. Tulsky JA. Conflict associated with decisions to limit life-sustaining treatment in intensive care units. J Gen Intern Med. 2001;16:283–289. doi: 10.1046/j.1525-1497.2001.00419.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaufman S. And a Time to Die: How Hospitals Shape the End of Life. New York: Scribner; 2005. [Google Scholar]
- 22.Winter L. Parks SM. Family discord and proxy decision makers' end-of-life treatment decisions. J Palliat Med. 2008;11:1109–1115. doi: 10.1089/jpm.2008.0039. [DOI] [PubMed] [Google Scholar]
- 23.Coppola KM. Bookwala J. Ditto PH. Lockhart LK. Danks JH. Smucker WD. Elderly adults' preferences for life-sustaining treatments, the role of impairment, prognosis and pain. Death Stud. 1999;23:617–634. doi: 10.1080/074811899200803. [DOI] [PubMed] [Google Scholar]
- 24.President's Commission for the Study of Ethical Problems in Medicine and Biomedical, Behavioral Research. Deciding to Forego Life-Sustaining Treatment. Washington, D.C.: US Government Printing Office; 1983. [Google Scholar]
- 25.Roccaforte WH. Burke WJ. Bayer BL, Wengel SP: Validation of a telephone version of the mini-mental state examination. J Am Geriatr Soc. 1992;40:697–702. doi: 10.1111/j.1532-5415.1992.tb01962.x. [DOI] [PubMed] [Google Scholar]
- 26.Zettel-Watson L. Ditto PH. Danks JH. Smucker WD. Actual, perceived gender differences in the accuracy of surrogate decisions about life-sustaining medical treatment among older spouses. Death Stud. 2008;32:273–290. doi: 10.1080/07481180701881230. [DOI] [PubMed] [Google Scholar]
- 27.Silveira MJ. Kim SY. Langa KM. Advance directives and outcomes of surrogate decision making before death. N Engl J Med. 2010;362:1211–1218. doi: 10.1056/NEJMsa0907901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Teno JM. Gruneir A. Schwartz Z. Nanda A. Wetle T. Association between advance directives and quality of end-of-life care: A national study. J Am Geriatr Soc. 2007;55:189–194. doi: 10.1111/j.1532-5415.2007.01045.x. [DOI] [PubMed] [Google Scholar]