Abstract
The uncertain trajectory of chronic critical illness exposes the patient’s family to heightened levels of psychological distress. Symptoms of psychological distress affect more than half of family members exposed to the patient’s chronic critical illness. Although symptoms often dissipate over time, a significant proportion of family members will remain at moderate to high risk for psychological distress well after the patient’s death or discharge from the intensive care unit. Family members of chronically critically ill (CCI) patients are often involved in the decision making for the CCI. Irrational or uninformed decision making can occur when family members experience high levels of psychological distress. Attention to the psychological needs and provision of support to family members enhance the formulation of treatment decisions consistent with the patient’s preferences and mitigate unnecessary resource use. In this article, the impact of chronic critical illness on family members’ risk for depression, anxiety, and post-traumatic stress disorder is described and a review of evidence-based strategies to support the psychological needs of family members coping with a patient’s chronic critical illness is provided.
Keywords: chronically critically ill (CCI), prolonged mechanical ventilation, family members, depression, anxiety, post-traumatic stress disorder, psychological outcomes, evidence-based practices
Exposure to chronic critical illness has devastating physiological effects on patients and damaging psychological consequences for their family members. The proportion of family members exposed to psychologically taxing conditions of chronic critical illness will continue to mount, consistent with steadily increasing rates of patients admitted to an intensive care unit (ICU) and demand for prolonged mechanical ventilation.1,2 The chronically critically ill (CCI) are a cohort of critically ill patients who require prolonged mechanical ventilation and consume an abundance of healthcare resources in an effort to enhance their likelihood for survival. Patients affected by chronic critical illness have been identified by protracted ICU lengths of stay, need for costly life-sustaining medical technologies, such as a tracheostomy and artificial enteral nutrition, and poor survival rates.3–10
The growing availability of critical care resources, along with technological advances in life-sustaining devices, have allowed many patients to survive acute life-threatening critical illnesses and transition to a chronic phase of critical illness. The CCI are a small and steadily increasing proportion of the critically ill who require prolonged mechanical ventilation during their hospitalization. To date, it is estimated that 5% of mechanically ventilated patients require prolonged mechanical ventilation (> 72 hours) and transition to the state of being chronically critically ill.11,12 Chronic critical illness is a syndrome that consists of patient characteristics such as respiratory insufficiency or failure requiring mechanical ventilation, multiple organ dysfunction related to underlying chronic disease, neuromuscular deterioration, malnutrition, symptom burden and psychological disturbances, such as delirium and depression.10, 13–15 The CCI are a subset of the critically ill that have a prolonged state of critical illness that necessitates their utilization of costly hospital and post-hospital resources. 3, 14–16
An episode of chronic critical illness exposes the patient’s family to an uncertain trajectory of critical illness that includes recurrent infections, hospital readmissions, and decrements in the patient’s condition over time. Moreover, chronic exposure to psychological stressors depletes the internal and external coping resources of the family system. Historically, the delivery of care in an ICU has been centered on the patients and marginalized the needs of the family. The admission of a patient to an ICU is often an acute, non-elective transition that elicits uncertainty for patients as well as their families. Most often the physiological needs of the patient are the principal concerns for critical care clinicians. Prioritizing the needs of the critically ill is essential during an episode of critical illness; however, critical care providers are now recognizing the need to also address the psychological needs of the patient’s family at the onset of critical illness.17
Family-Centered Critical Care
Family-centered critical care aims to simultaneously recognize the needs of the patient and family during critical illness. For family members, having a loved one in an ICU can be a traumatic and stressful experience due to communication barriers, uncertainty, and fear of the patient’s physical disability or death. Families of the critically ill are not just visitors, but they are caregivers, decision makers and persons who are dealing with the hour by hour psychological stress of uncertainty. The model of family-centered critical care reflects a philosophy of care that approaches the family as an extension of the critically ill, who also experience the process of care.18 This model is a departure from the traditional patient-centered care model that has commonly guided the delivery of care in the ICU.
Like the CCI, their family members have distinct characteristics and needs during an episode of chronic critical illness. In general, family members of the CCI are middle-age, Caucasian females who are the patient’s spouse or adult child.15,16,19 Most report having obtained at least a high school education, earning a mid-level annual household income, and did not consider themselves the patient’s caregiver prior to an ICU admission.15,16,19 They also report a change in employment status related to the episode of chronic critical illness.19
The lack of attention to psychological needs of the family during chronic critical illness may indirectly affect the clinical outcomes and resource use of the CCI. The severity of psychological distress among family members of the CCI is likely to interfere with their ability to comprehend vital medical information and formulate informed decisions regarding the patient’s medical care. The purpose of this article is to review the psychological impact of chronic critical illness on the family and to introduce evidence based practices that address the psychological needs of family members of CCI patients.
Impact of Psychological Symptoms on Family Members’ Decision Making
Since many CCI patients are not cognitively intact, attention to the psychological needs of the family may ultimately enhance the formulation of informed decisions and the integration of the patient’s preferences into the medical plan of care. Several clinical studies have explored the incidence of impaired cognitive status among the CCI. The purpose of these studies was to describe the occurrence of cognitive impairment in the CCI, in order to assess the likelihood of patient participation in decision making about medical plans of care. Among CCI patients, more than one-third were cognitively impaired upon admission to an ICU.15, 19–21 Most CCI patients who require prolonged mechanical ventilation go on to need a decision about the placement of tracheostomy. A majority (>80%) of CCI patients who receive an elective tracheostomy while in the ICU were unable to make the decision themselves because of impaired cognitive status.22,23 The inability to participate in the decision making process adds to the complexity of the CCI and shifts the burdensome responsibility of decision making to their family members.
When a CCI patient is cognitively impaired, critical care providers turn to the patient’s family members for treatment decisions. Family members designated in the role of a surrogate or family decision maker (FDM) are expected to be actively involved in making decisions that are consistent with the patient’s treatment preferences. Family members in the role of a FDM are burdened with the responsibility of making the “right” decisions for the patient. Often FDMs are unaware of the patient’s treatment preferences and opinions about life-sustaining therapies but are faced with making decisions with little certainty about the consequences of their decisions. In one recent report, a majority (82%) of CCI patients did not have established advanced directives, living wills, or prior discussion about their treatment preferences with their family.23 The involvement of the family in the decision making process may not ensure a plan of medical care that is consistent with the patient’s preferences and values, especially when there is a lack of knowledge about the patient’s wishes prior to the hospitalization.
The psychological distress of critical illness and a lack of knowledge regarding the patient’s treatment preferences can interfere with the family member’s decision making. A state of high negative emotions can influence the ability to formulate rational and well-informed decisions. Advancements in radiographic imaging confirm the association between emotion and decision making. The emerging disciplines of neuropsychology and cognitive science have demonstrated the influence of negative emotion (anxiety, depression, fear, and stress) on regions of the human brain that enable an individual to process information and formulate a decision.24–28 Human brain mapping confirms that states of high negative emotions interfere with the function of the orbitofrontal cortex of the brain, which is the brain region responsible for information recall and rational decision making.29–31 The use of functional magnetic resonance imaging (fMRI) provides anatomical and cognitive frameworks for decision making and explain the influence of negative emotion on an individual’s ability to conduct rational decision making.25
Prior research has documented the insufficient informational and psychological support for family members of CCI patients.14,22,32 Nelson and colleagues found that family members of CCI patients did not comprehend the impact the decision would have on the patient or their own psychological well being.14 This study revealed that family members in the FDM role often regretted their decisions to continue or withdraw life-sustaining therapies for cognitively impaired CCI patients. Moreover, attention to perceived inadequacies of communication or informational needs may improve the psychological condition of family members as well as produce treatment decisions that align with the patient’s and family’s preferences and expectations. Thus, human brain mapping and clinical research indicate that states of high negative emotion can produce poor comprehension of medical information and irrational decisions that may not reflect the patient’s or family’s treatment preferences.
Family Systems in Crisis
The uncertainty and life-threatening nature of chronic critical illness elicit states of crisis for patients and their family systems. The family system, inclusive of the critically ill patient, indirectly experiences the impact of the patient’s physical condition. A family of a critically ill patient can be vulnerable to the effects of psychological stress associated with patient’s severity of illness and concurrent stressors. Perpetual exposure to situational conditions, such as readmissions to an ICU, failure to wean from mechanical ventilation, recurrent hospital acquired infections, and anticipation of the patient’s death, have psychologically detrimental effects on the patient’s as well as the family’s psychological well-being. Over time, families of the CCI are exposed to an array of conditions that reduce their ability to effectively cope with stressful conditions.
Chronic exposure to these stressful conditions has the potential to elicit a state of psychological crisis in the family system. Families of the CCI indirectly experience waves of recurrent episodes of the patient’s acute illness increasing their perceptions of stress and over time depleting their ability to employ effective coping strategies. For families of the CCI, the prolonged state of the critical illness initiates a host of concerns such as role changes, financial issues, and disruption in daily activities or work schedules for the family members. The patient’s critical illness is a stressful event that modifies the family structure and the prolonged state and severity of illness adds to the instability of the family structure. However, this process does not occur as an isolated crisis event and it is not uncommon for a family to have multiple pre-existing stressors or strains which may amplify impaired family coping and adaption during the patient’s chronic critical illness.33 Therefore, in this section we will discuss the impact of chronic critical illness as a contributor to symptoms of depression, anxiety, and posttraumatic stress disorder in family members of CCI patients.
Depression
From the onset of critical illness, family members are likely to report symptoms of depression that slowly abate over time. Assessments of depressive symptoms in family members of the critically ill were conducted by a group of French researchers. Their research confirmed that more than one-third of family members suffer depressive symptoms as early as 3–5 days after the patient’s admission to an ICU.34,35 Spouses of critically ill patients were more likely to suffer from depressive symptoms compared to all other family members.33 In addition to the family member’s kinship, the patient’s age (younger age), the family member’s gender (female), and ethnicity (Non-caucasian) contributed to the risk for depression.35
In comparison to the studies conducted in French ICUs, several American studies have found similar patterns of depressive symptoms in family members of critically ill patients. Among family members of patients requiring at least 48 hours of mechanical ventilation, one-third (34%) of family members were at risk for clinical depression and the amount of depressive symptoms reported after hospital discharge was influenced by the perception of the patient’s functional status.36,37 Although not statistically significant, family members of patients who resided in a institutional setting after hospital discharge were more likely to have a higher risk for depression compared to family members of patients who were at home.36
Critical illness places the patient’s family at risk for depression in spite of patient’s survival to hospital discharge. Although the amount of depressive symptoms decrease over time, some (23%) family members have shown to remain at risk for clinical depression a year after the patient’s discharge from the hospital.37 Siegal and colleagues examined the next of kin of patients who died in an ICU.38 They found that the most common psychiatric illness was major depressive disorder and 30% of their family members met diagnostic criteria for the disorder 3–12 months after the patient’s death.38 In comparison, the rate of depression in family members of patients who survived their critical illness was lower than in family members of patients died in an ICU; however, the proportion of family members at risk for depression in both groups was greater than family caregivers of patients with chronic illnesses.36 Thus, exposure to a patient’s critical illness may have longstanding effects on the family member’s risk for depression.
The exposure to a patient’s chronic critical illness may intensify the patterns of depressive symptoms among the family members of the CCI. In a series of research studies, Douglas and Daly have examined the patterns of depressive symptomatology in family members of CCI patients who received at least 72 hours of mechanical ventilation. In 2005, Douglas and Daly published the results of their longitudinal study describing the incidence and predictors of depressive symptoms in family members of CCI patients. Their study indicated that more than half (51.2%) of family members of CCI patients had some degree of depression symptomatology at hospital discharge and the proportion of family members who continued to have some degree of depression was more than one-third (36.4%).15 Over time, they found 12.2% of family members at hospital discharge were at risk for depression and 15.6% of family members at six months after hospital discharge remained at risk for depression. The most influential factors for depression at six months after hospital discharge were family members’ perceptions of their physical health status and their appraisal of caregiver burden.15
In a trial of a post-hospital disease management intervention for the CCI and their families, Douglas and Daly examined the impact of the intervention upon the reduction of family members’ depressive symptoms. Subsequently, they found that half (50%) of family members at hospital discharge and approximately one-third (31%) of family members at six months after hospital discharge were at risk for depression as indicated by depression symptom scores. Two months after the patient’s discharge, depression scores among family members of the CCI were influenced by the patient’s disposition and functional status, as well as the family member’s gender, report of poor general health status, and caregiver burden.17 The post-hospital disease management intervention did not demonstrate a difference in depression scores between family members’ who received the intervention compared to individuals who received usual care. Failure to reduce the risk of depression in family members with a post-hospital disease management intervention suggests interventions initiated at the patient’s discharge may be too late to reduce depression scores in these family members.
Douglas and her colleagues continued to examine risk factors for depression among family member’s designated as family decision makers, as part of an effectiveness trial of a structured communication system implemented at the onset of chronic critical illness. The implementation of a structured communication system while CCI patients were in an ICU did not influence family members’ risk for clinical depression but did facilitate the recognition of patients’ preferences and earlier decisions not to pursue an aggressive medical plan of care.39 Descriptive data from this effectiveness trial revealed a racial disparity between Caucasian and non-Caucasian (African American, Hispanic, Asian) family members’ risk for depression and treatment for depression. Non-Caucasian family members of patients living in an institutional setting two months after hospital discharge had the highest risk for depression (OR: 2.75, p=.001). They also found non-Caucasian family members who had a significant risk for depression were three times less likely to be treated with psychotropic medications than at risk Caucasian family members.
Given the risk of depression among family members of the CCI, it is important to identify ways to address this psychological outcome. Research on influential personality traits of family members may provide future direction for interventions that reduce the risk of depression. An individual’s informational processing style is a characteristic of personality that activates dispositional coping behaviors in order to manage a stressful situation through scanning for informational cues or avoiding sources of threatening information. Hickman & Daly investigated the influences of informational processing style, informational satisfaction, and role stress on depressive symptoms in family members during the first week of the patient’s chronic critical illness.40 Their investigation confirmed that family members who report a preference towards information seeking behaviors, higher scores of role stress, and less satisfaction were more likely to experience more depressive symptoms.40 Although information processing style and informational satisfaction predicted risk for depression, the most significant predictor was the perception of stress from being the FDM for a cognitively impaired CCI patient.
The high levels of depressive symptoms and the proportion of family members affected confirms the need for critical care clinicians to proactively screen for depression among family members of CCI patients. Depression is one of the most common psychological problems reported by family members of the CCI. The chronic exposure to the host of family and individual stressors and strains require clinicians to carefully assess for symptoms of depression and provide psychosocial support for the family across the continuum of care.
Anxiety
The uncertainty associated with critical illness contributes to states of anxiety among family members. During critical illness, family members search for cues that signal improvements or deterioration in the patient’s condition. However, when informational cues are absent or not easily comprehended, family members are likely to manifest symptoms of anxiety related to the psychological stress of uncertainty. The uncertainty of the patient’s critical illness is often exacerbated by fluctuations in the patient’s condition as well as during transitions in the patient’s care.
Transitions in care, such as transferring the patient from the ICU to a regular nursing floor or to an extended care facility, are clinical milestones that produce uncertainty and psychological stress in patients and their family members. Mitchell & Courtney examined the association between uncertainty in illness and anxiety in family members of critically ill patients at ICU discharge.41 Their study confirms a moderate amount of perceived uncertainty is experienced before and after the patient is discharged from the ICU. More importantly, the higher the level of uncertainty, the more symptoms of anxiety expressed by family members during this transitional period.41
In the general critical care literature, family members of ICU patients experience symptoms of anxiety that respond to the rapid changes in patient’s condition or transitions between levels of care. Anxiety is a common psychological disorder experienced among family members of critically ill patients.38 During the course of the patient’s critical illness, family members are likely to be exposed to conditions that induce symptoms of anxiety and research has shown that as many as two-thirds of family members have symptoms of anxiety while the patient is hospitalized in an ICU.34,42 Consistent with the occurrence of depressive symptoms, being female and a spouse of younger patients increases the probability of symptoms of anxiety among family members.35 Although symptoms of anxiety are elevated at the onset of critical illness, acute changes in the patient condition or periods of transitions may exacerbate family members’ anxiety and reduce the dissipation of symptoms.43
To date, the impact of chronic critical illness on family members’ anxiety has not been explored. Despite the lack of empirical evidence about anxiety in this specific subset of family members of the critically ill, screening and psychological support should be provided to families to identify and address symptoms of anxiety. The body of evidence in the family members of non-CCI patients confirms a need to allocate resources (sufficient RN staffing, family liaison, family support groups) to minimize uncertainty by providing timely information, as well as the preparation of families for transitions in the delivery of care.
Acute & Post-traumatic Stress Disorder
Post-traumatic stress disorder (PTSD), once a psychological disturbance associated with veterans and individuals exposed to traumatic life events, is emerging as a psychological concept of interest in studies of family members exposed to a patient’s critical illness. A precursor to post-traumatic stress disorder, acute stress disorder (ASD) is a cluster of symptoms experienced by family members during and up to four weeks after a traumatic event. The inability to recall information, “being in a daze”, emotional numbness, disturbing flashbacks of their experience, and insomnia are a few symptoms associated with acute/post-traumatic stress disorder.44 At the onset of a patient’s critical illness, acute stress disorder can have pronounced effects on family members. As early as the patient’s arrival to an ICU, Auerbach and colleagues found that family members’ ASD scores were equivalent to patients who were admitted to a PTSD unit for psychiatric treatment.44 The most common ASD symptoms in family members were hyperarousal and re-experiencing their ICU event through flashbacks or nightmares.
As the patient’s critical illness continues, family members with symptoms of ASD are at risk for developing PTSD. Paparrigopoulos and colleagues reported that during the first week of critical illness, a majority (81%) of family members had a quantity of symptoms which placed them at risk for PTSD.45 The proportion of family members suffering with symptoms of PTSD was found in more than a third (35%) of family members at three months by Azoulay and his colleagues; in comparison, Anderson and her colleagues found that almost half (49%) of family members six months after the patient’s discharge from an ICU or date of the patient’s death also reported PTSD symptoms.43,46 These studies indicate an increase in PTSD symptoms over time and describe the lingering effects that critical illness can have on family members.
Several studies have identified risk factors associated with the development of PTSD symptoms in family members of the critically ill.43,46–48 Azoulay and colleagues found family members who were female, an adult child, involved in the decision making process, and expressed feelings of dissatisfaction with information had higher risk for PTSD, while controlling for patient related factors (severity of illness, cancer diagnosis).48 Both trait and state anxiety levels and depression scores have been shown to further increase the risk for PTSD among relatives of the critically ill; neither, the patient’s severity of illness nor the age of the relative were influential.45 Consistent with the findings of Paparrigopoulos and colleagues, Anderson and her colleagues confirmed the relationship between family members’ with higher levels of anxiety and had a greater risk for PTSD at 6 months after the patient’s hospital discharge.43 The progression of symptoms of ASD to PTSD in family members of the critically ill suggests that the patient’s hospital discharge does not resolve psychological stress for family members. The continual psychological arousal from the patient’s prolonged state of critical illness and post-hospital stressors can predispose family members to PTSD.
Our understanding of acute stress and post-traumatic stress disorders in family members of CCI patients has not been previously explored. To date, the incidence of ASD and PTSD has been documented in family members of non-CCI patients. Although a significant proportion of family members will have symptoms of ASD and PTSD, family members of the CCI patients are suspected to be equally affected by symptoms of ASD and PTSD. Further research is needed to examine the occurrence and severity of symptoms of ASD and PTSD in family members of CCI patients.
Our discussion of the psychological impact of chronic critical illness illustrates the vulnerability of family members of CCI patients and their need for psychological support from the critical care team. Prolonged exposure to a patient’s critical illness subjects family members to chronic states of psychological arousal that over time puts them at risk for depression, anxiety and post-traumatic stress disorders. Table 1 presents characteristics that increase the likelihood of psychological symptoms of family members. Unfortunately, many family members involved in the act of decision making for a critically ill patient have an increased risk for one of these psychological disturbances which can alter the quality of informed decision making. Therefore, we advocate for the use of evidence based practices that mitigate the psychological impact of chronic critical illness on the patient’s family.
Table 1.
Psychological Symptoms and Associated Risk Factors in Family Members of the Chronically Critically Ill.
| Psychological Symptoms | Associated risk factors |
|---|---|
| Depression | Female35 |
| Spouse of a patient35 | |
| Non-Caucasian race/ethnicity35, 39 | |
| Information seeking coping style (monitoring)40 | |
| Role stress related to being a FDM40 | |
| Perceived high caregiver burden17, 19 | |
| Dissatisfaction with informational support40 | |
| Family member’s and patient’s perceived poor health status17, 19, 36, 37, 39 | |
| Patient’s post-hospital disposition (institutional setting)19, 36, 39 | |
| Age of the patient (younger)35 | |
| Death of the patient 37, 38 | |
| Anxiety | Female35 |
| Spouse of a patient35 | |
| Age of the patient (younger)35 | |
| Transitions in care41, 43 | |
| Perception of uncertainty41 | |
| Acute/Posttraumatic Stress | Female48 |
| Disorder | Adult child of a critically ill patient48 |
| Involvement in surrogate decision making48 | |
| Dissatisfaction with ICU care48 | |
| High levels of trait or state anxiety45 | |
| Depressive symptoms43, 45 | |
FDM = Family Decision Maker
Translating Research into Practice
Family members of CCI are emerging as a vital yet psychologically vulnerable component in decision making process for this cohort of the critically ill. There is a need to focus on evidence based strategies that provide psychological, informational, and social support resources for family members coping with the challenges of a patient’s chronic state of critical illness. Vulnerable family members of the CCI benefit when critical care clinicians recognize that patient and family outcomes are synergistic and integrate intensive psychological, informational, and social support resources into the plan of care. Shifting the paradigm from patient-centered to a family-centered care model emphasizes the implementation of evidence based practices that will optimize health related outcomes of all recipients of critical care. Therefore, critical care nurses must consciously act with intention, to incorporate evidence based family-centered strategies that are likely to influence patients’ clinical outcomes and can potentially mitigate the psychological harm of chronic critical illness on family members.
Establish Trust
Evidence-based strategies that support families of CCI patients should be initiated early in the course of the patient’s illness. Family members require a sense of trust in the critical care team; however, trust takes time to develop and must be cultivated over time. The first few days after the admission of the patient to the ICU is an ideal time to meet with the patient’s family and establish an empathic relationship. This simple act of proactively meeting the family can reduce uncertainty, provide an opportunity to express emotional support and lay the foundation for a therapeutic interpersonal relationship between the family and critical care team. Leon & Knapp advocate communication practices that incorporate psychosocial support during an interaction with family members of the critically ill and CCI (Table 2). 49
Table 2.
Leon and Knapp’s recommendations for communication practices to establishing trust and psychosocial support in family members of the critically ill. 49
|
The use of experienced critical care nurses as liaisons between the family and critical care team has been well received by family members. In a recent study, advanced practice nurses (APNs) facilitated and conducted family meetings, provided personal contact and updates on the patient’s condition, and managed the patient and family after discharge.8,19 Opportunities to formulate trust and a caring relationship with the family must be identified early in the patient’s chronic critical illness and cultivated through discharge from the ICU.
Family Communication
The timing and structure of a family meeting can make a difference in patient outcomes. Family meetings are often held too late in the patient’s illness to provide significant benefit to the patient’s family or to change treatment goals. Too often family meetings are initiated by critical care clinicians when the family is needed to make major treatment decisions or when the provider perceives the severity of the patient’s condition warrants an end-of-life discussion. Family meetings should be held routinely in an effort to support the family and to integrate the patient’s and family’s treatment preferences into the plan of care.
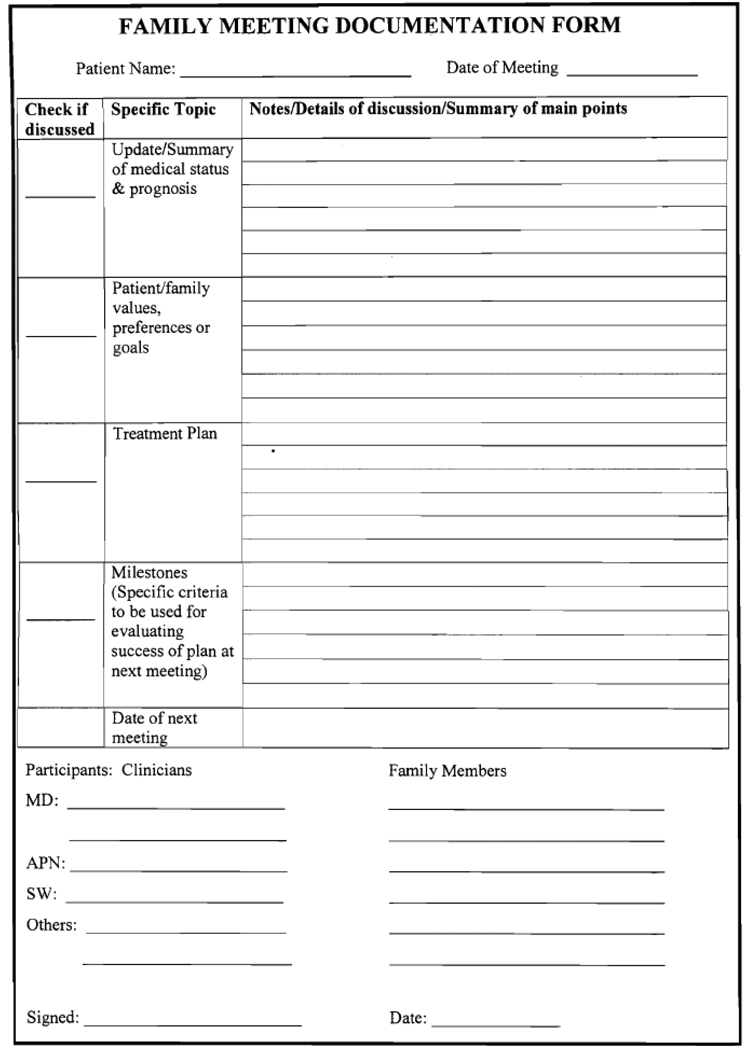
Lilly and colleagues implemented a structured process of proactive communication in the form of weekly multi-disciplinary family meetings, initiated within 72 hours of the patient’s admission to a medical ICU. Family meetings were held away from the patient’s bedside and followed a standardized communication process aimed to: 1) update the family on the patient’s medical condition and treatment options; 2) discuss the patient’s prognosis and gain understanding of the patient’s attitude towards death and dying; 3) obtain consensus from the family about the patient’s treatment plan; 4) establish clinical milestones that indicate the success or failure of the treatment plan; and 5) establish the next family conference.50 Each family conference was documented and the documentation was maintained in the patient’s medical record (Figure 1). The impact of early formal family meetings reduced the length of stay in patients within the highest quartile of severity of illness and resulted in initiation of palliative care sooner for dying critically ill patients. Early discussions with family members did not increase patient mortality. Early on-going family meetings with a structured communication process provide necessary information that enables families and critical care clinicians to tailor the treatment plan to the patient’s preferences.
Figure 1.
Clinical documentation form for family conferences in the ICU. This form prompts critical care clinicians to discuss the five components of the structured communication process developed by Lilly and colleagues. This multidisciplinary approach provides informational support, facilitates the discussion about treatment preferences and documents the conversations between clinicians and family members of critically ill patients.
Effective use of therapeutic interpersonal communication during the family meeting also facilitates the family members’ comprehension of medical information and satisfaction with care provided in the ICU. Often critical care clinicians spend a majority of time speaking to family members about the patient’s condition and treatment plan and do not devote enough time to addressing family concerns or identifying the patient’s preadmission quality of life and treatment preferences. McDonagh and colleagues examined the patterns of speech between family members and ICU clinicians during family meetings.51 They found that on average family meetings were relatively brief (32 minutes) but were dominated by ICU clinicians. Most (70%) of the time during the family meeting was spent by the clinician speaking to the family and little time was spent listening to family.51 Family members were more likely to be satisfied with the care provided in the ICU when permitted to speak more often during a family meeting. McDonagh and colleagues suggest that when clinicians take the time to listen to family members, opportunities arise that can influence family satisfaction with critical care services. This study reinforces the fact that communicating with family members is an artful balance between the amount of time spent speaking and listening to concerns.
Psychological Screening
In addition to informational support obtained from family meetings or informal updates, families of the CCI can benefit from psychological screening and preventative strategies that maintain psychological well-being through the course of a patient’s critical illness. Screening family members for symptoms of depression, anxiety, and acute/post-traumatic stress disorder can be done quickly through the administration of questionnaires or through face-to-face interviews. The screening process can be useful in providing educational and social support resources to help family members through the stress of critical illness. Early psychological screening among family members of the critically ill can identify individuals who may benefit from interventions that prevent further psychological impairment. Screening family members for risk for psychological disturbances will enable critical care nurses to coordinate resources in order to prevent additional psychological harm. Additional recommendations for family support from the American College of Critical Care Medicine Task Force 2004–2005 are presented in Table 3.52
Table 3.
Recommended Practices and Strategies for Family Support in the ICU.52
| Clinical Domains | Recommended Practices | Family Support Strategies |
|---|---|---|
| Decision Making |
|
|
| Family Coping |
|
|
ASD = Acute Stress Disorder
PTSD = Post Traumatic Stress Disorder
Caregiver research conducted in family members of CCI patients suggest early identification and continued assessment of family members at the greatest risk for poor psychological outcomes. This growing body of caregiver literature supports the use of screening tools such as the Center for Epidemiological Studies Depression (CESD) scale.53 This instrument, originally intended for use in general community dwelling adult populations, can aid critical care clinicians in the identification of family members who may benefit from additional psychological support. Screening for psychological symptoms in family members of the chronically critically ill should be done early and frequently in order to refer at risk family members to supportive services or to their primary care provider for further evaluation and management of altered psychological states.
Conclusion
The experienced critical care clinician cannot apply the “one-size fits all” approach to dealing with the psychological needs of family members of the chronically critically ill. The armamentarium of evidence based strategies that reduce the psychological distress in family members of the chronically critically ill continues to expand. Simple acts of communication, such as family conferences, utilizing APNs or experienced critical care nurses as family liaisons, may prove to effectively reduce uncertainty and psychological distress in family members of CCI patients. Implementing strategies to reduce the psychological impact of a patient’s chronic critical illness are likely to be more effective when initiated early and intentionally to address the on-going needs of family members.
Acknowledgments
This publication was made possible by Grant Number 1KL2RR024990 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Ronald L. Hickman, Jr., Lecturer and Clinical Research Scholar, Frances Payne Bolton School of Nursing, Case Western Reserve University.
Sara L. Douglas, Associate Professor, Frances Payne Bolton School of Nursing, Case Western Reserve University.
References
- 1.Zilberberg M, Luippold, Rose, Sulsky, Sandra Prolonged acute ventilation, hospital resource utilization, and mortality in the United States. Crit Care Med. 2008;36(3):724–730. doi: 10.1097/CCM.0B013E31816536F7. [DOI] [PubMed] [Google Scholar]
- 2.Zilberberg M, De Wit M, Pirone J, Shorr A. Growth in adult prolonged acute mechanical ventilation: implication for healthcare delivery. Crit Care Med. 2008;36(5):1451–1455. doi: 10.1097/CCM.0b013e3181691a49. [DOI] [PubMed] [Google Scholar]
- 3.Carson S, Cox C, Holmes G, Howard A, Carey T. The changing epidemiology of mechanical ventilation: a population-based study. Journal of Intensive Care Medicine. 2006;21(3):173–182. doi: 10.1177/0885066605282784. [DOI] [PubMed] [Google Scholar]
- 4.Chelluri L, Mendelson A, Belle S. Hospital costs in patients recieving prolonged mechanical ventilation: does age have an impact? Crit Care Med. 2003;31(6):1746–1751. doi: 10.1097/01.CCM.0000063478.91096.7D. [DOI] [PubMed] [Google Scholar]
- 5.Chelluri L, Im K, Belle S, Schulz R, Rotondi A, Donahoe M, et al. Long-term mortality and quality of life after prolonged mechanical ventilation. Crit Care Med. 2004;32(1):61–69. doi: 10.1097/01.CCM.0000098029.65347.F9. [DOI] [PubMed] [Google Scholar]
- 6.Combes A, Costa A, Trouillet J, Baudot J, Mokharti M, Gibert C, et al. Morbidity, mortality, and quality of life outcomes of patients requiring ≥ 14 days of mechanical ventilation. Crit Care Med. 2003;31(5):1373–1381. doi: 10.1097/01.CCM.0000065188.87029.C3. [DOI] [PubMed] [Google Scholar]
- 7.Cox C, Carson S. An economic evaluation of prolonged mechanical ventilation. Crit Care Med. 2007;35(8):1918–1927. doi: 10.1097/01.CCM.0000275391.35834.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Daly B, Douglas S. Trial of a disease management program to reduce hospital readmissions of the chronically critically ill. CHEST. 2005;128(2):507–517. doi: 10.1378/chest.128.2.507. [DOI] [PubMed] [Google Scholar]
- 9.Douglas S, Daly B, Gordon N, Brennan P. Survival and quality of life: short-term versus long-term ventilator patients. Crit Care Med. 2002;30(12):2655–2662. doi: 10.1097/00003246-200212000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Estenssoro E, Reina R, Canales H, Saenz M, Gonzalez F, Aprea M, et al. The distinct clinical profile of chronically critically ill patients: a cohort study. Critical Care. 2006;10(3):R89. doi: 10.1186/cc4941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Neirman D. A structure of care for the chronically critically ill. Critical Care Clinics. 2002;18:477–491. doi: 10.1016/s0749-0704(02)00010-6. [DOI] [PubMed] [Google Scholar]
- 12.Daly B, Rudy E, Thompson P, Sabo K, Happ M. Development of a special care unit for chronically ill patients. Heart & Lung. 1991;20:40–51. [PubMed] [Google Scholar]
- 13.Higgins P, Daly B, Lipson A, Guo S-E. Assessing nutritional status in chronically critically ill adult patients. American Journal of Critical Care. 2006;15(2):166–177. [PMC free article] [PubMed] [Google Scholar]
- 14.Nelson J, Kinjo K, Meier D, Ahmad K, Morrison R. When critical illness becomes chronic: informational needs of patients and families. Journal of Critical Care. 2005;20:79–89. doi: 10.1016/j.jcrc.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 15.Douglas S, Daly B. Caregivers of longterm ventilator patients. CHEST. 2003;123:1073–1081. doi: 10.1378/chest.123.4.1073. [DOI] [PubMed] [Google Scholar]
- 16.Lipson A, Kelley C, Higgins P, Daly B. "My mother's leaving today?": a pilot study on awareness of discharge date in the chronically critically ill. MEDSURG Nursing. 2006;15(1):8–12. [PMC free article] [PubMed] [Google Scholar]
- 17.Davidson J, Powers K, Hedaya tK, Tieszen M, Kon A, Shepard E, et al. Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Critical Care Medicine Task Force 2004–2005. Crit Care Med. 2007;35(2):605–622. doi: 10.1097/01.CCM.0000254067.14607.EB. [DOI] [PubMed] [Google Scholar]
- 18.Alvarez G, Kirby A. The perspective of families of the critically ill patient: their needs. Current Opinion in Critical Care. 2006;12:614–618. doi: 10.1097/MCC.0b013e328010c7ef. [DOI] [PubMed] [Google Scholar]
- 19.Douglas S, Daly B. Impact of a disease management program upon caregivers of chronically critically ill patients. Chest. 2005;128(6):3925–3936. doi: 10.1378/chest.128.6.3925. [DOI] [PubMed] [Google Scholar]
- 20.Douglas S, Daly B, Kelley C, O'Toole E, Montenegro H. Chronically critically ill patients: health-related quality of life and resource use after a disease management intervention. Journal of Critical Care. 2007;16(5):447–457. [PMC free article] [PubMed] [Google Scholar]
- 21.Douglas S, Daly B. Hospital readmission among long-term ventilator patients. CHEST. 2001;120(4):1278–1286. doi: 10.1378/chest.120.4.1278. [DOI] [PubMed] [Google Scholar]
- 22.Nelson J, Meier D, Litke A, Natale D, Siegal R, Morrison S. The symptom burden of chronic critical illness. Crit Care Med. 2004;32(7):1527–1534. doi: 10.1097/01.ccm.0000129485.08835.5a. [DOI] [PubMed] [Google Scholar]
- 23.Camhi S, Mercado A, Morrison S, Du Q, Platt D, August G, et al. Deciding in the dark: advance directives and continuation of treatment in chronic critical illness. Crit Care Med. 2009;37(3):919–925. doi: 10.1097/CCM.0b013e31819613ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bechara A. Characterization of the decision making deficit of patients with ventromedial prefrontal cortex lesions. Brain. 2000;123:2189–2202. doi: 10.1093/brain/123.11.2189. [DOI] [PubMed] [Google Scholar]
- 25.Bechara A. Risky business: emotion, decision-making, and addiction. Journal of Gambling Studies. 2003;19(1):23–51. doi: 10.1023/a:1021223113233. [DOI] [PubMed] [Google Scholar]
- 26.Bechara A. The role of emotion in decision making: evidence from neurological patients with orbitofrontal damage. Brain and Cognition. 2004;55:30–40. doi: 10.1016/j.bandc.2003.04.001. [DOI] [PubMed] [Google Scholar]
- 27.Bechara A, Damasio H, Damasio A. Emotion, decision making and the orbitofrontal cortex. Cerebral Cortex. 2000;10(3):295–307. doi: 10.1093/cercor/10.3.295. [DOI] [PubMed] [Google Scholar]
- 28.Bechara A, Dolan S. Decision making deficits, linked to a dysfunctional ventromedial prefrontal cortex, revealed in alcohol and stimulant abusers. Neuropsychologia. 2001;39:376–389. doi: 10.1016/s0028-3932(00)00136-6. [DOI] [PubMed] [Google Scholar]
- 29.Pham M. Emotion and rationality: a critical review and interpretation of empirical evidence. American Psychological Association. 2007;11(2):155–178. [Google Scholar]
- 30.Damasio A. The somatic marker hypothesis and the possible functions of the prefrontal cortex. Philosphical Transactions: Biological Sciences. 1996;351:1413–1420. doi: 10.1098/rstb.1996.0125. [DOI] [PubMed] [Google Scholar]
- 31.Damasio A. Emotion in the perspective of an integrated nervous system. Brain Research Reviews. 1998;26:83–86. doi: 10.1016/s0165-0173(97)00064-7. [DOI] [PubMed] [Google Scholar]
- 32.Leske J, Jiricka M. Impact of family demands and family strengths and capabilities on family well-being and adaption after critical injury. American Journal of Critical Care. 1998;7(5):383–392. [PubMed] [Google Scholar]
- 33.American Psychiatric Publishing, Inc. 2000 DSM-IV TR [Website] Available from: http://www.psychiatryonline.com/content.aspx?aID=3459. Access date?
- 34.Pochard F, Darmon M, Fassier T, Bollaert P-E, Cheval C, Coloigner M, et al. Symptoms of anxiety and depression in family members of intensive care unit patients before discharge or death. A prospective multicenter study. Journal of Critical Care. 2005;20:90–96. doi: 10.1016/j.jcrc.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 35.Pochard F, Azoulay E, Chevret S, Lemaire F, Hubert P, Canoui P, et al. Symptoms of anxiety and depression in family members of intensive care unit patients: ethical hypothesis regarding decision-making capacity. Crit Care Med. 2001;29(10) doi: 10.1097/00003246-200110000-00007. [DOI] [PubMed] [Google Scholar]
- 36.Im K, Belle S, Schulz R, Mendelsohn A, Chelluri L. Prevalence and outcome of caregiving after prolonged (≥ 48 Hours) mechanical ventilation in the ICU. CHEST. 2004;125(2):597–606. doi: 10.1378/chest.125.2.597. [DOI] [PubMed] [Google Scholar]
- 37.Van Pelt D, Milbrandt E, Qin L, Weissfeld L, Rotondi A, Schulz R, et al. Informal caregiver burden among survivors of prolonged mechanical ventilation. American Journal of Respiratory and Critical Care Medicine. 2007;175(2):167–173. doi: 10.1164/rccm.200604-493OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Siegal M, Hayes E, Vanderwerker L, Loseth D, Pigerson H. Psychiatric illness in the next of kin of patients who die in the intensive care unit. Crit Care Med. 2008;36(6):1722–1728. doi: 10.1097/CCM.0b013e318174da72. [DOI] [PubMed] [Google Scholar]
- 39.Douglas S, Daly B, O'Toole E, Hickman R. Depression among Caucasian and Non-caucasian caregivers of the chronically critically ill. [Journal Article] doi: 10.1016/j.jcrc.2009.09.004. In press 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hickman R, Daly B, Douglas S, Clochesy J. Informational coping style and depressive symptoms in family decision makers of cognitively impaired chronically critically ill.[Journal Article] doi: 10.4037/ajcc2010354. In press 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mitchell M, Courtney M. Reducing family members' anxiety and uncertainty in illness around transfer from intensive care: an intervention study. Intensive and Critical Care Nursing. 2004;20:223–231. doi: 10.1016/j.iccn.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 42.Azoulay E, Pochard F, Chevret S, Lemaire F, Mokhtari M, Le Gall J, et al. Meeting the needs of intensive care unit families. American Journal of Respiratory Critical Care Medicine. 2001;163:135–139. doi: 10.1164/ajrccm.163.1.2005117. [DOI] [PubMed] [Google Scholar]
- 43.Anderson W, Arnold R, Angus D, Bryce C. Posttraumatic stress and complicated grief in family members of patients in the intensive care unit. Journal of General Internal Medicine. 2008;23(11):1871–1876. doi: 10.1007/s11606-008-0770-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Auerbach S, Kiesler D, Wartella J, Rausch S, Ward K, Ivatury R. Optimism, satisfaction with needs met, interpersonal perceptions of the healthcare team, and emotional distress in patients' family members during critical care hospitalization. American Journal of Critical Care. 2005;14(3):202–209. [PubMed] [Google Scholar]
- 45.Paparrigopoulos T, Melissaki A, Efthymiou A, Tsekou H, Vadala C, Kribeni G, et al. Short-term psychological impact on family members of intensive care unit patients. Journal of Psychosomatic Research. 2006;61:719–722. doi: 10.1016/j.jpsychores.2006.05.013. [DOI] [PubMed] [Google Scholar]
- 46.Azoulay E, Pochard F, Kentish-Barnes N, Chevret S, Aboab J, Adrie C, et al. Risk of posttraumatic stress symptoms in family members of intensive care unit patients. American Journal of Respiratory Critical Care Medicine. 2005;171(9):987–994. doi: 10.1164/rccm.200409-1295OC. [DOI] [PubMed] [Google Scholar]
- 47.Jones C, Skirrow P, Griffiths R, Humphris G, Ingleby S, Eddleston J, et al. Post-traumatic stress disorder-related symptoms in relatives of patients following intensive care. Intensive Care Medicine. 2004;30:456–460. doi: 10.1007/s00134-003-2149-5. [DOI] [PubMed] [Google Scholar]
- 48.Azoulay E, Pochard F, Kentish-Barnes N, Chevret S, Aboab J, Adrie C, et al. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. American Journal of Respiratory and Critical Care Medicine. 2005;171(9):987–994. doi: 10.1164/rccm.200409-1295OC. [DOI] [PubMed] [Google Scholar]
- 49.Leon A, Knapp S. Involving family systems in critical care nursing. Dimensions Critical Care Nursing. 2008;27(6):255–262. doi: 10.1097/01.DCC.0000338866.47164.6d. [DOI] [PubMed] [Google Scholar]
- 50.Lilly C, De Meo D, Sonna L, Haley K, Massaro A, Wallace R, et al. An intensive communication intervention for the critically ill. American Journal of Medicine. 2000;109:469–475. doi: 10.1016/s0002-9343(00)00524-6. [DOI] [PubMed] [Google Scholar]
- 51.McDonagh J, Elliot T, Engelberg R, Treece P, Shannon S, Rubenfeld G, et al. Family satisfaction with family conferences about end-of-life care in the intensive care unit: increased proportion of family speech is associated with increased satisfaction. Crit Care Med. 2004;32(7):1484–1488. doi: 10.1097/01.ccm.0000127262.16690.65. [DOI] [PubMed] [Google Scholar]
- 52.Davidson J, Powers K, Hedaya K, Tieszen M, Kon A, Shepard E, et al. Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Critical Care Medicine Task Force 2004–2005. Critical Care Medicine. 2007;35(2):605–622. doi: 10.1097/01.CCM.0000254067.14607.EB. [DOI] [PubMed] [Google Scholar]
- 53.Radloff L. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychological Measurement. 1977;1:385–401. [Google Scholar]