Abstract
Tailgut cysts, or retrorectal cystic hamartomas, are rare congenital developmental lesions, most commonly located in the retrorectal space, and are more common in women. We present a case of retrorectal tailgut cyst managed using a laparoscopic approach. A 36-year-old woman presented with incidentally detected retrorectal tumors during evaluation for a gallbladder polyp. Her past medical history revealed that she had undergone cesarean section twice. The tumor marker CA 19-9 level was 42.52 U/ml. CT of the pelvis with contrast and pelvic MRI revealed a 3.9 × 3.3 cm well-defined, homogeneous cystic mass in the right presacral area, and a 2.5 × 1.5 cm cystic mass in the precoccygeal space. The patient underwent laparoscopic exploration with a preoperative diagnosis of tailgut cysts based on radiological findings. The operative time was 90 min including 30 min of subsequent laparoscopic cholecystectomy without placement of additional trocars. The surgical specimens consisted of two fragments of fibrofatty tissues, unilocular cystic masses. The final pathologic diagnosis was tailgut cysts with no evidence of malignancy. Postoperative recovery was uneventful, and the patient was discharged after 3 days. In conclusion, surgical resection is recommended in the management of retrorectal tailgut cyst to establish a definite diagnosis and to rule out malignancy. The laparoscopic approach is a feasible and safe option.
Key Words: Retrorectal mass, Tailgut cyst, Surgical resection, Laparoscopic approach
Introduction
Tailgut cysts, or retrorectal cystic hamartomas, are rare congenital developmental lesions that are thought to be derived from remnants of the embryonic postanal gut with incomplete regression during development [1, 2]. They are most commonly located in the retrorectal space and are more common in women [2]. We present a case of retrorectal tailgut cysts managed using a laparoscopic approach.
Case Report
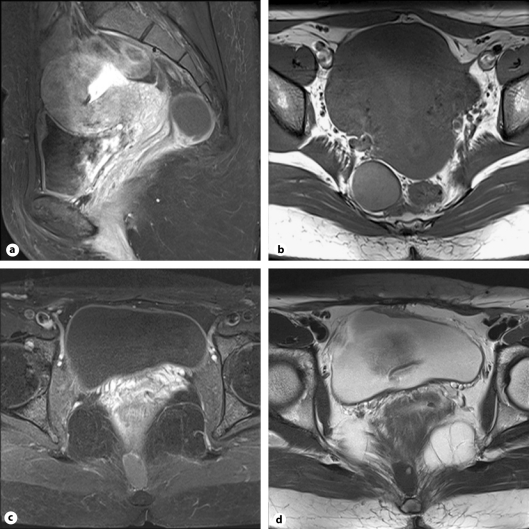
A 36-year-old woman presented with incidentally detected retrorectal tumors during evaluation for a gallbladder polyp. Her past medical history revealed that she had undergone cesarean section twice. On digital rectal examination a soft indurated mass was palpated. Her laboratory studies were unremarkable. The tumor marker CA 19-9 level was 42.52 U/ml. CT the of pelvis with contrast revealed a 3.9 × 3.3 cm well-defined, homogeneous cystic mass in the right presacral area. Pelvic MRI with contrast demonstrated a 4 × 3.8 × 3 cm retroperitoneal cystic tumor with intermediate high signal intensity on T1- and T2-weighted images in the right presacral area, and a 2.5 × 1.5 cm cystic mass in the precoccygeal space with high signal intensity on T1-weighted image (fig. 1).
fig. 1.
MRI scan showing the presacral and precoccygeal tailgut cyst lesions with intermediate signal intensity. a Sagittal view of the presacral cyst. b Axial view of the presacral cyst. c, d Axial view of the precoccygeal cyst.
The patient underwent laparoscopic exploration with a preoperative diagnosis of tailgut cysts based on the radiological findings. In brief, the patient was placed in the lithotomy position. Access was gained with a 10-mm supraumbilical port followed by four 5-mm ports in both the right upper/lower and left upper/lower quadrants. The abdomen was insufflated to an abdominal pressure of 12 mm Hg with CO2 gas. The uterus was fixed to the anterior abdominal wall by sutures. The mesorectal dissection from the sacral promontory was continued up to the level of puborectalis sling and the levator ani muscles. The excisions of cysts were complete with macroscopically negative margins, and there was no injury to the rectum. There was no intraoperative event. The operative time was 90 min including 30 min of subsequent laparoscopic cholecystectomy with no placement of additional trocars. No drain was placed.
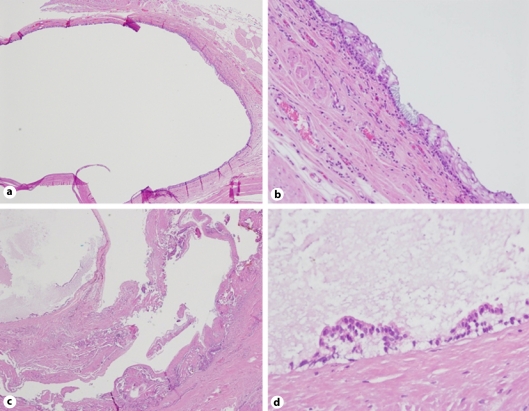
The surgical specimens consisted of two fragments of fibrofatty tissues, the larger presacral mass a unilocular cyst with a stalk of connective tissue, and measured 4 × 3.5 × 3 cm (fig. 2). The presacral and precoccygeal cysts were filled with thick, mucoid, yellowish-colored fluid. The inner surface of the cyst was irregular and yellow in color. Microscopically, the walls of the cyst were partially lined with stratified squamous epithelium and columnar epithelium (fig. 3). The final pathologic diagnosis was tailgut cysts and chronic cholecystitis. There was no evidence of malignancy.
fig. 2.

The macroscopic findings displayed an oval-shaped, gray-white appearance and the cysts was filled with a thick yellowish material.
fig. 3.
Microscopic pathological findings. a, b The presacral cyst was lined by squamous epithelium and focal columnar epithelium. c, d The precoccygeal cyst wall was lined by stratified squamous epithelium.
Enteral feeding was started on the second postoperative day. Postoperative recovery was uneventful, and the patient was discharged after 3 days.
Discussion
Retrorectal tailgut cysts, also known as retrorectal cystic hamartomas, are rare congenital lesions, located in the retrorectal space, which is bounded anteriorly by the rectum, posteriorly by the sacrum, superiorly by the peritoneal reflection, inferiorly by the levator ani and coccygeus muscles, and laterally by the ureters and iliac vessels [3]. Tailgut cyst is most prevalent in middle-aged women, arising from postnatal primitive gut remnants, but can be found in a wide range of age groups including infancy [2, 4]. Most tailgut cysts are asymptomatic, and they often are discovered incidentally or presented as a compressive effect of a growing mass within the pelvis such as change in stool caliber, a palpable rectal mass, urinary frequency, and frequently as infected tailgut cyst with rectal fistula or anal fistula [3, 5].
CT showed a retrorectal mass and transrectal ultrasound and rectal MRI are good diagnostic tools. A diagnostic biopsy is not recommended due to the risk of spillage of malignant cells or spread of infection into the abdominal cavity [5]. Although malignant transformation is known to be rare, the important factors for a good prognosis are the time of diagnosis and surgical radicality [6].
Complete surgical resection is the traditional treatment of choice, eliminating the potential of recurrence, hemorrhage, infection, compression, and malignant changes [2, 7, 8]. Several surgical approaches are proposed for the resection of retrorectal tumors: anterior (abdominal), posterior, and combined anterior and posterior pelvic approach [5, 7]. The posterior approach of perianal intersphincteric excision or the parasacrococcygeal approach are recommended for a low-lying tumor under the promontory or below the level of S4 [9]. Perianal intersphincteric excision preserves good sphincter function, whereas the parasacrococcygeal approach is preferred in lesions with a suspicion of malignancy. In addition, transanal endoscopic microsurgery is used for the resection of retrorectal tumors and allows accurate excision through the rectal wall under excellent view [10]. The laparoscopic approach is reported as a safe and effective option for low-lying retrorectal tumors with the advantage of a magnifying effect in the narrow pelvis [11, 12].
In the present case, we dissected the specimen meticulously, preserving the pelvic plexus without entering the cysts and avoiding rectal injury in magnification of the surgical field. Comparatively short operative time, less than estimated blood loss, and a short postoperative hospital stay were achieved by taking benefits of the laparoscopic approach.
Before performing this laparoscopic tailgut cyst excision, 1,101 resections of patients out of a total of 1,584 cases of laparoscopic colorectal cancer surgery, including low-lying rectal cancer, were performed between January 2004 and September 2010 by a single colorectal surgeon (H.R. Kim) in our institution. With the advancement in laparoscopic technique and an experienced colorectal surgeon, we could perform excision of the tailgut cysts laparoscopically at the level of S4 and the levator ani muscles.
Conclusion
In conclusion, we report a case of tailgut cysts arising in the retrorectal area in a 36-year-old woman. Surgical resection is recommended in the management of tailgut cyst to establish a definite diagnosis and to rule out malignancy, and a laparoscopic approach could be applied as a feasible, minimally invasive and safe option to this type of retrorectal tumor.
Footnotes
This is an Open Access article licensed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs 3.0 License (www.karger.com/OA-license), applicable to the online version of the article only. Distribution for non-commercial purposes only.
References
- 1.Rafindadi AH, Shehu SM, Ameh EA. Retrorectal cystic harmatoma (tailgut cyst) in an infant: case report. East Afr Med J. 1998;75:726–727. [PubMed] [Google Scholar]
- 2.Hjermstad BM, Helwig EB. Tailgut cysts. Report of 53 cases. Am J Clin Pathol. 1988;89:139–147. doi: 10.1093/ajcp/89.2.139. [DOI] [PubMed] [Google Scholar]
- 3.Hutton KA, Benson EA. Case report: tailgut cyst – assessment with transrectal ultrasound. Clin Radiol. 1992;45:288–289. doi: 10.1016/s0009-9260(05)80020-0. [DOI] [PubMed] [Google Scholar]
- 4.Mourra N, Caplin S, Parc R, Flejou JF. Presacral neuroendocrine carcinoma developed in a tailgut cyst: report of a case. Dis Colon Rectum. 2003;46:411–413. doi: 10.1007/s10350-004-6564-7. [DOI] [PubMed] [Google Scholar]
- 5.Schwarz RE, Lyda M, Lew M, Paz IB. A carcinoembryonic antigen-secreting adenocarcinoma arising within a retrorectal tailgut cyst: clinicopathological considerations. Am J Gastroenterol. 2000;95:1344–1347. doi: 10.1111/j.1572-0241.2000.02023.x. [DOI] [PubMed] [Google Scholar]
- 6.Prasad AR, Amin MB, Randolph TL, Lee CS, Ma CK. Retrorectal cystic hamartoma: report of 5 cases with malignancy arising in 2. Arch Pathol Lab Med. 2000;124:725–729. doi: 10.5858/2000-124-0725-RCH. [DOI] [PubMed] [Google Scholar]
- 7.Singer MA, Cintron, Martz JE, Schoetz DJ, Abcarian H. Retrorectal cyst: a rare tumor frequently misdiagnosed. J Am Coll Surg. 2003;196:880–886. doi: 10.1016/S1072-7515(03)00133-9. [DOI] [PubMed] [Google Scholar]
- 8.Sriganeshan V, Alexis JB. A 37-year-old woman with a presacral mass. Tailgut cyst (retrorectal cystic hamartoma) Arch Pathol Lab Med. 2006;130:e77–e78. doi: 10.5858/2006-130-e77-AYWWAP. [DOI] [PubMed] [Google Scholar]
- 9.Buchs N, Taylor S, Roche B. The posterior approach for low retrorectal tumors in adults. Int J Colorectal Dis. 2007;22:381–385. doi: 10.1007/s00384-006-0183-9. [DOI] [PubMed] [Google Scholar]
- 10.Zoller S, Joos A, Dinter D, Back W, Horisberger K, Post S, Palma P. Retrorectal tumors: excision by transanal endoscopic microsurgery. Rev Esp Enferm Dig. 2007;99:547–550. doi: 10.4321/s1130-01082007000900011. [DOI] [PubMed] [Google Scholar]
- 11.Bax NM, van der Zee DC. The laparoscopic approach to sacrococcygeal teratomas. Surg Endosc. 2004;18:128–130. doi: 10.1007/s00464-003-9093-x. [DOI] [PubMed] [Google Scholar]
- 12.Konstantinidis K, Theodoropoulos GE, Sambalis G, Georgiou M, Vorias M, Anastassakou K, Mpontozoglou N. Laparoscopic resection of presacral schwannomas. Surg Laparosc Endosc Percutan Tech. 2005;15:302–304. doi: 10.1097/01.sle.0000183252.96808.78. [DOI] [PubMed] [Google Scholar]