Abstract
Fuchs heterochromic uveitis (FHU) in its classic presentation is a unilateral, chronic, low grade, often asymptomatic anterior uveitis. It is characterized by a classic triad of iris heterochromia, cataract and keratic precipitates. Neovascularization of the iris and the anterior chamber (AC) angle (radial and circumferential) occurs in 6–22% of cases. This angle and iris new vessels can sometimes lead to a characteristic filiform haemorrhage and formation of hyphaema after AC paracentesis and is a hallmark of FHU known as Amsler–Verrey sign. This haemorrhage has been previously associated with trivial trauma, mydriasis, applanation tonometry, gonioscopy, or it may occur spontaneously. In the setting of cataract surgery it has been previously reported with the use of a Honan balloon. We report a case of cataract and FHU where the Amsler–Verrey sign developed intraoperatively during a phacoemulsification procedure. To the best of our knowledge, this is the first documented report of this sign occurring intraoperatively during cataract surgery.
Background
Amsler–Verrey sign describes the characteristic anterior chamber (AC) bleeding that is noted in patients with Fuchs heterochromic uveitis (FHU). AC bleeding in patients with Fuchs uveitis has been known to occur either be spontaneous or associated with trivial trauma, gonioscopy, applanation tonometry and pharmacological mydriasis. The use of a Honan balloon during cataract surgery has also been known to cause the AC haemorrhage. To the best of our knowledge, this is the first documented case of intraoperative AC bleeding occurring during cataract surgery in a patient with FHU. We describe the clinical features (surgical video attached) and management strategies to deal with this very rare complication during cataract surgery.
Video 1.
Case presentation
A 53-year-old Caucasian woman with past history of anterior uveitis and cataract was referred for cataract surgery in the right eye (RE). Her past medical history was unremarkable. Ocular history was significant for recurrent FHU in the RE. On examination best-corrected visual acuities were hand movements in the RE and 6/6 in the left eye (LE). Examination of the left eye was unremarkable. Slit lamp biomicroscopy of the right eye showed characteristic stellate keratic precipitates scattered throughout the corneal endothelium, heterochromia irides and a dense, white cataract. The AC appeared quiet and the intraocular pressures were within normal limits. B-scan ultrasonography showed a normal posterior segment in the RE. Under perioperative steroid cover (oral steroids 40 mg per day started a week prior to surgery and tapered postoperatively over a period of 4 weeks) cataract surgery was performed under topical (proxymethacaine 0.5% Minims; Chauvin Pharmaceuticals, Romford, UK) and intracameral anaesthesia (1% preservative free lidocaine).
Treatment
Surgical procedure
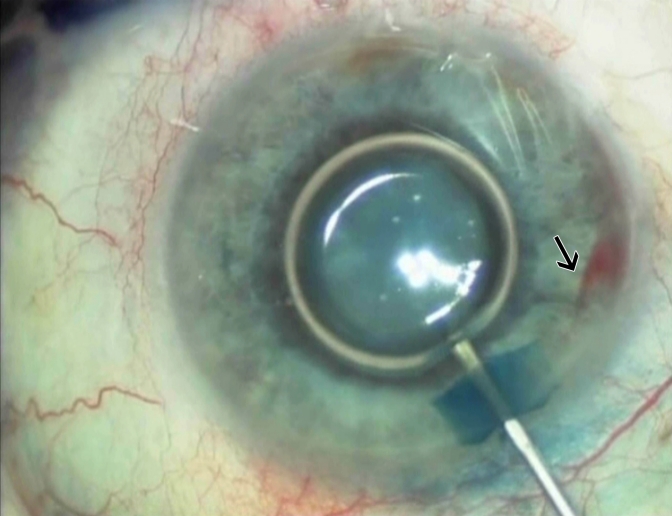
A 20-gauge micro-vitreoretinal blade was used to create two paracentesis wounds 180 degrees apart (for bimanual irrigation and aspiration), and a 2.75 mm clear corneal wound was constructed in the superior cornea. Following injection of sterile air to maintain the AC, 0.1% trypan blue (Vision Blue; DORC International, Zuidland, The Netherlands) was injected under the air bubble over the anterior capsule with a 27-gauge cannula to allow even contact of the dye with the anterior lens capsule. Following this, the dye was washed out from the AC with balanced salt solution (BSS). At this stage, fresh bleeding was noted in the AC arising from the nasal angle (figure 1). A high-density cohesive ophthalmic viscoelastic device (OVD; 1.4% sodium hyaluronate, Healon GV, Abbott Medical Optics, Santa Ana, California, USA) was used to tamponade the bleeding and to maintain the AC. This resulted in cessation of the bleeding, and the phacoemulsification procedure was performed without any complications with placement of a single-piece intraocular lens implant (IOL) within the capsular bag (Video attachment).
Figure 1.
Intraoperative photography showing a fresh haemorrhage (arrow) arising from the angle in the anterior chamber.
Outcome and follow-up
Slit-lamp biomicroscopy performed 20 min postoperatively and at day 1 showed a well-formed AC, centred IOL in the bag with no evidence of hyphaema. She was treated with topical 0.3% Ofloxacin (Exocin; Allergan, Irvine, California, USA) and 0.1% dexamethasone (Maxidex; Alcon, Fort Worth, Texas, USA) 4 times a day for 3 weeks. Gonioscopic examination at 1 week postoperatively showed an open angle with no evidence of new vessels in the angle. At 3 weeks follow-up she achieved an unaided vision of 6/9 correcting to 6/5.
Discussion
A characteristic filiform haemorrhage and formation of hyphaema after AC paracentesis is a hallmark of FHU and is known as the Amsler–Verrey sign.1 2 Amsler and Verrey first described this sign in 1946 and since then it is considered to be a hallmark sign of FHU.2 This filiform haemorrhage is a sign of fragility of the vessels in the iris or in the AC angle. It is unclear whether these iridocorneal angle vessels are neovascular or merely abnormal iris vasculature.1 Amsler sign can either be spontaneous or associated with trivial trauma, gonioscopy, applanation tonometry and pharmacological mydriasis.3 The use of a Honan balloon during cataract surgery has also been known to cause the AC haemorrhage.4 5 In our case, we noted bleeding while irrigating the AC with BSS following the use of trypan blue dye to stain the lens capsule. The sudden momentary decompression of the AC during this process may have resulted in bleeding from the fragile iris vessels in the angle. However, immediate tamponade of the AC with a high-density OVD helped to arrest the bleeding. The remainder of the phacoemulsification procedure was performed without any complications.
Learning points.
-
▶
Amsler–Verrey sign describes the characteristic AC bleeding that is noted in patients with FHU.
-
▶
Intraoperative AC bleeding can occur during cataract surgery in FHU due to the decompression of the AC and bleeding from the fragile iris vessels.
-
▶
Intraoperative tamponade with a high-density ophthalmic viscosurgical devise can arrest the intraoperative bleeding allowing the surgeon to proceed with cataract surgery.
Footnotes
1 20-gauge micro vitreoretinal blade used to create paracentesis
2 Intracameral anesthesia (1% preservative free lidocaine) injected into anterior chamber through paracentesis
3 2.75 mm clear corneal wound was constructed in the superior cornea
4 Injection of sterile air to maintain the anterior chamber
5 0.1 % trypan blue (Vision Blue, DORC International, Netherlands) injected under the air bubble over the anterior capsule to allow even contact of the dye with the anterior lens capsule
6 The dye is then washed out from the AC with balanced salt solution
7 Fresh bleeding noted in the AC arising from the nasal angle
8 A high density cohesive ophthalmic viscoelastic device (OVD) (1.4 % Sodium hyaluronate, Healon GV, Advanced Medical Optics, USA) was used to tamponade the bleeding and to maintain the AC
9 Continuous curvilinear capsulorhexis (CCC) performed
10 Cataract removed by phacoemulsification technique
11 A single piece intraocular lens implant (IOL) is placed within the capsular bag.
Competing interests None.
Patient consent Obtained.
References
- 1.Jones NP. Fuchs’ heterochromic uveitis: an update. Surv Ophthalmol 1993;37:253–72 [DOI] [PubMed] [Google Scholar]
- 2.Amsler M, Verrey F. Hétérochromie de Fuchs et fragilité vasculaire. Ophthalmologica 1946;111:177–81 [DOI] [PubMed] [Google Scholar]
- 3.Liesegang TJ. Fuchs uveitis syndrome. In: Pepose JS, Holland GN, Wilhelmus KR, editors. Ocular infection & immunity. St. Louis, Missouri, USA: Mosby; 1996;41:495–506 [Google Scholar]
- 4.Feldman ST, Deutsch TA. Hyphema following Honan balloon use in Fuchs’ heterochromic iridocyclitis. Arch Ophthalmol 1986;104:967. [DOI] [PubMed] [Google Scholar]
- 5.Jones NP. Cataract surgery in Fuchs’ heterochromic uveitis: past, present, and future. J Cataract Refract Surg 1996;22:261–8 [DOI] [PubMed] [Google Scholar]