Abstract
Background
Failure to follow-up test results is a critical safety issue. The objective was to systematically review evidence quantifying the extent of failure to follow-up test results and the impact on patient outcomes.
Methods
The authors searched Medline, CINAHL, Embase, Inspec and the Cochrane Database from 1990 to March 2010 for English-language articles which quantified the proportion of diagnostic tests not followed up for hospital patients. Four reviewers independently reviewed titles, abstracts and articles for inclusion.
Results
Twelve studies met the inclusion criteria and demonstrated a wide variation in the extent of the problem and the impact on patient outcomes. A lack of follow-up of test results for inpatients ranged from 20.04% to 61.6% and for patients treated in the emergency department ranged from 1.0% to 75% when calculated as a proportion of tests. Two areas where problems were particularly evident were: critical test results and results for patients moving across healthcare settings. Systems used to manage follow-up of test results were varied and included paper-based, electronic and hybrid paper-and-electronic systems. Evidence of the effectiveness of electronic test management systems was limited.
Conclusions
Failure to follow up test results for hospital patients is a substantial problem. Evidence of the negative impacts for patients when important results are not actioned, matched with advances in the functionality of clinical information systems, presents a convincing case for the need to explore solutions. These should include interventions such as on-line endorsement of results.
Keywords: Diagnostic tests, routine; medical errors; CPOE; assessment, patient outcomes; continuity of patient care; review; systematic; healthcare quality; medical error; patient outcomes
Introduction
The World Alliance for Patient Safety recently identified poor test follow-up as one of the major processes contributing to unsafe patient care.1 Failure to follow up test results increases the risk of missed or delayed diagnoses. This may produce suboptimal clinical outcomes2–8 with potential medicolegal implications.9–12
Clinicians are concerned that their test management practices are not systematic,7 13 and considerable variation exists.10 14 15 It has been claimed that information technology can improve this process, making it safer, easier and more systematic, reducing the risk of results being missed.6 16–18 Yet, evidence of its effective application in practice is limited.1 5 19 Managing the follow-up of diagnostic and radiological test results is a complex process.20–22 It entails information exchange between patients, doctors, nurses and laboratories using a combination of information systems, including paper-based, telephone and electronic systems, and involving a variety of policies and procedures. Multiple steps, players and information systems create an environment which increases the risk of errors.
There have been no published systematic reviews of the extent of the problem of failure to follow-up test results for hospital patients. Our aim was to review evidence which quantified the size of the problem and the impact on patient outcomes for hospital patients including patients attending the emergency department (ED).
Methods
Data sources and searches
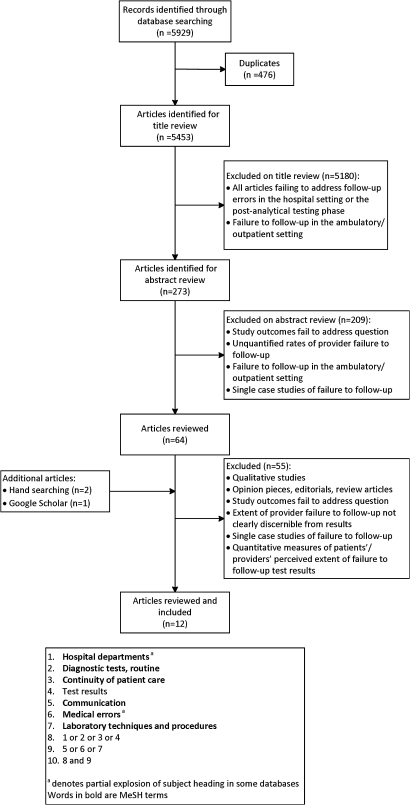
A literature search of the following databases was undertaken for English-language publications from January 1990 to March 2010: Medline; CINAHL; Embase; Inspec and the Cochrane Database of Systematic Reviews (figure 1). Search terms were identified from keyword lists of core journal articles related to the research topic. Reference lists of articles which met the inclusion criteria were hand-searched. A web search using the Google Scholar search engine was completed to locate unindexed publications in press.
Figure 1.
Search flow for failure to follow-up test results literature, including keywords and Medical Subject Headings (MeSH) terms used in search process.
Study selection
Four researchers (JC, AG, JL, JW) individually screened titles and abstracts to determine eligibility. Studies which quantified the extent of the failure to follow-up laboratory or radiology test results for hospital inpatients or patients treated in the ED were included in the review. Failure to follow-up was defined as neglecting to document a follow-up of test results by the ordering physician or another provider. Studies examining laboratory or radiology departments' failure to report critical results, uncommunicated pending results during handover or discharge summaries and physicians' failure to communicate results to patients were excluded. Studies reporting physicians'23–26 or patients'27 perceived rates of failure to follow-up were excluded, as were studies which measured time to treatment or how rapidly test results were acted upon.6 28–30
Data extraction
Eligible studies were independently reviewed (JC, AG, JL, JW), and discrepancies were resolved by further discussion until consensus was reached. Authors of papers were contacted when necessary for additional information.
Results
Search results
Twelve studies3 4 20 31–39 met our inclusion criteria (table 1, available online only).
Study characteristics
Eight studies were conducted in the USA.3 4 20 33 34 36 38 39 Most study designs were medical record reviews, either retrospective4 20 32 33 36 37 39 or prospective.3 31 35 One study reviewed malpractice claims,38 while another retrospectively linked laboratory and pharmacy databases.34
Hospital inpatients
Extent of failure to follow-up results and impact on inpatient outcomes
Seven studies examined the extent of failure to follow-up for hospital inpatients.3 4 20 32–34 39 Three reported aggregated results for inpatients and outpatients.4 34 39 The extent of follow-up failure was reported as a proportion of inpatients4 20 33 34 or of tests under study.3 32 39 The extent of failure to follow-up ranged from 1.0%33 to 22.9% of inpatients4 and from 20.04%39 to 61.9%3 when reported per test type. The range of test types included: urgent32 and critical20 laboratory results; abnormal actionable results pending at discharge3; diagnostic imaging4 33 39 and elevated Thyroid Stimulating Hormone levels.34 A study of radiology follow-up using an email alert system for important but not urgent imaging findings reported that 20.0% (10 598/52 883) of electronic reports were not viewed by the referring physician.39
Four of the seven studies reported the impact of failure to follow-up which included missed diagnoses of malignancy,33 hypothyroidism,34 hyperthyroidism,3 osteoporosis,4 microbiological results which necessitated the starting or changing of antibiotic therapy,3 and positive serological test results for Helicobacter pylori.3
Follow-up of critical laboratory results and results pending at discharge
There was wide variation in the three studies which examined follow-up of critical values which can be life-threatening if action is not taken promptly.40 Kilpatrick and Holding32 assessed the effects of replacing telephone notification of urgent laboratory results with computer terminal access. They found that 529/1836 (28.8%) urgent biochemistry results during a 6-month period were never accessed electronically. Interestingly, for 27 (5.1%) of the 529 results never accessed, the clinician had attempted access using the ward terminal before the results were available. Tate et al20 found that 15.3% (19/124) of medical records audited for a 2-month period contained no documentation for which either the nurse or physician was aware of the critical laboratory value or had taken corrective action. A study of critical radiology result follow-up found that in four of the 395 (1.0%) suspected malignancy cases, the provider was unaware of the findings.33 These four inpatients would have been lost to follow-up if the semiautomated coding and review process had not been instituted.33
Results which are pending at the time of discharge from hospital present a particular challenge to physicians. Roy et al3 found that hospital physicians were unaware of 65 results (61.6% (95% CI 51.3% to 70.9%)), and of these, 24 (37.1% (95% CI 25.7% to 50.2%)) were actionable, with eight (12.6% (95% CI 6.4% to 23.3%)) requiring urgent action. Although several limitations were reported in this study, they concluded that there was a need for better systems to follow up results that arrive after a patient is discharged.3
Patients treated in the ED
Extent of failure to follow-up results and impact on patient outcomes
Seven studies quantified the extent of failure to follow-up in EDs.31–33 35–38 This ranged from 1.0%31 to 75% of tests36 and 0%33 to 16.5%38 of patients treated in the ED. Test types included: radiology with failure to follow-up ranging from none to 5.6%31 33 37; microbiology with failed follow-up ranging from 3.0% to 75%31 35 36; serum lead levels with 33.3% lost to follow-up36; and urgent biochemistry with 44.7% not followed up.32 One study examined 122 closed malpractice claims, for which test types were unknown, from four liability insurers for injuries which ED patients sustained between 1979 and 2001.38 The study found that 79 of the 122 claims (64.8%) involved missed ED diagnoses that harmed patients, and 13 of these 79 claims (16.5%) identified the breakdown to have occurred at the step of ‘test results transmitted to and received by the provider.’38
All seven studies explored the impact on patient outcomes31–33 35–38 which included no negative effects,31 a delayed diagnosis from a missed x-ray report,37 one case of missed positive Chlamydia where the patient subsequently developed pelvic inflammatory disease,36 inappropriate or unnecessary antibiotics prescribed,35 missed cancer diagnoses33 and death.38
Discussion
Extent of the problem and impact on patient outcomes
There is evidence to suggest that the proportion of missed test results is a substantial problem which impacts on patient safety. However, there was enormous variability reported on the extent of the problem. Lack of follow-up of test results for patients treated in the ED ranged from 1.0%31 to 75%36 and for inpatients from 20.04%39 to 61.9%3 when calculated as a proportion of tests. The range when calculated as a proportion of patients was 0%33 to 16.5%38 for patients treated in the ED and 1.0%33 to 22.9%4 for hospital inpatients. Examples of serious patient outcomes were identified, including missed cancer diagnoses33 and positive Chlamydia with subsequent development of pelvic inflammatory disease.36
The studies were heterogeneous in their approach limiting robust comparison. Medical record review was frequently used, which relied upon documentary evidence of follow-up. This may lead to an overestimation of the problem, since, in some cases, results may have been seen and acted upon but not documented. Publication bias may also be a factor whereby papers which reported high rates of missed test results are more likely to be published than those which did not. We found that factors associated with missed results included: the systems and practices used; reporting critical results, and test results for patients moving across care settings.
Systems and practices used to follow-up test results
Only two studies described complete electronic test management systems3 20 where tests were ordered on-line and results reported electronically with no paper used. The rate of missed results was high in both these studies, although it could be argued that the technology made the problem more explicit and easier to measure. Rates were also high in hospitals which used entirely paper-based systems4 36 and in those which used a mixture of paper and electronic systems.32 35 There was no evidence of any link between the system used and the extent of missed test results. Other studies have shown that the use of hybrid paper and electronic clinical information systems is associated with errors and duplications, with complete electronic systems showing fewer errors.13 41 A study of outpatient test results reported that the use of a partial electronic medical record (paper-based progress notes and electronic test results or vice versa) was associated with higher rates of failure to inform patients of clinically significant results compared with not having an electronic medical record (OR=1.92; p=0.03), or compared with having an electronic medical record that included both progress notes and test results (OR=2.37; p=0.007).42 A qualitative study which evaluated an electronic results management system in paediatric ambulatory care found that practices which had fully adopted the electronic system reported gains in efficiency, reliability, timeliness and provider satisfaction, whereas some partial adopters reported decreased efficiency and increased risk of lost test results.14
Despite many advocates of the use of information technologies to improve the management of test results,6 18 19 28 43–45 few studies have evaluated electronic test management systems, and results have been mixed.6 32 Existing electronic systems now provide the capacity for clinicians to acknowledge that they have viewed test results on-line and document their follow-up actions. Electronic test management systems also have the capability of reporting results to the ordering clinician and other members of the team to facilitate endorsement of results in team-based environments and shift handover situations. This on-line endorsement function would enable reports of rates of missed test results to be produced which could provide a continuous quality audit capability for use by management and physicians.
Advances in the functionality of test management systems are not sufficient to solve the problem. The complexity of the test management process and high volume of test results requires significant review and reform of work practices to allow electronic endorsement to occur easily. Management of test results can differ depending on the needs and work practices of physicians in different clinical settings, and so electronic test management systems need to be flexible to adapt to these divergent requirements.46–49
Reporting of critical test results
A commonly cited problem in test result reporting was the breakdown in the communication process, including documentation of actions, between clinical units and the laboratories. This was particularly evident in studies which reported lack of follow-up for critical test results.20 32 33 Others have identified the follow-up of critical results as an area requiring attention.2 50 51 Despite established practice guidelines requiring critical values to be telephoned to the clinical team, compliance may be low, and information may not always go to the person involved in the patients' care.20 28 The traditional practice of laboratories telephoning results of urgent or critical tests is time-consuming with potential for errors.32 For the follow-up of critical results to occur without error, the information transfer between laboratory staff and clinicians must be examined to devise technological, work practice and policy solutions which take account of this cross-boundary communication process.38 Nurses have been shown to play an important role in test-result follow-up and should be included in any solutions devised.20 33
Electronic test management systems provide the potential to support notification of critical results. However, the study by Kilpatrick and Holding32 concluded that substituting the telephoning of urgent results with computer access could hinder, rather than promote, communication between laboratory and clinicians. Limitations of that study were that computer terminals had been in place for only 6 months, and it was not stated whether all clinicians were mandated to use the computers.32 Interestingly, Kilpatrick and Holding found that some results were never accessed: clinicians had attempted access via the ward terminals before the results were available.32 Thus, time may be wasted by clinicians continually checking if results are available. These passive retrieval systems rely on the clinician to ‘pull’ the information from the test management system rather than actively notifying clinicians of urgent results.18 Active notification of abnormal and critical results to clinicians using alerts has been shown to be effective.29 30 52–57
Test results for patients moving across settings
Our review showed that patients moving across settings, for example, from inpatient to outpatient services, or patients treated in the ED discharged to the care of their general practitioner or to the ward, can cause problems with follow-up of results and continuity of care.3 35 36 The ED is particularly challenging for test-result follow-up due to the high patient throughput, team-based care, handoffs and lack of continuous relationships between patients and clinicians.36 38 Given the short length of stay for discharged ED patients, late-arriving results also increase the risk of certain test results being missed.36 37 One study reported a more comprehensive test follow-up for hospitalised than for discharged ED patients.35 Other studies have supported this finding, relating medical errors to discontinuity of care during handoffs between hospital teams or transfer of care between inpatient and outpatient settings.58–60 These studies highlight the need for systems, policies and practices which facilitate communication of information across different settings. The discharge summary is a standard means of communication between settings, but it may not always reach the intended recipient61–63 or be complete. One advantage of electronic discharge summaries is that family physicians are more likely to receive them in a timely fashion64–66 and hence seek to follow up any outstanding results. An electronic test management and discharge summary system which provided secure access for health professionals, both in hospital and in the community, could facilitate the follow-up of test results pending at discharge.
Conclusions
The number of research studies in this area is limited, and the methods used prevent robust comparisons. The existing evidence suggests that the problem of missed test results is considerable and reported negative impacts on patients warrant the exploration of solutions. Further studies are urgently needed to test the effectiveness of interventions such as on-line endorsement of results. Attention must be paid to integration of solutions, particularly those which involve information technology, into clinical work practices.
Footnotes
Funding: This study is part of an Australian Research Council Linkage Grant (LP0989144) funded project to investigate the use of information and communication technologies to support effective work practice innovation in the health sector.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.World Alliance for Patient Safety Summary of the Evidence on Patient Safety: Implications for Research. Geneva: World Health Organization, 2008 [Google Scholar]
- 2.Bates DW, Leape LL. Doing better with critical test results. Jt Comm J Qual Patient Saf 2005;31:66–7 [DOI] [PubMed] [Google Scholar]
- 3.Roy CL, Poon EG, Karson AS, et al. Improving patient care. Patient safety concerns arising from test results that return after hospital discharge. Ann Intern Med 2005;143:121–8 [DOI] [PubMed] [Google Scholar]
- 4.Cram P, Rosenthal GE, Ohsfeldt R, et al. Failure to recognize and act on abnormal test results: the case of screening bone densitometry. Jt Comm J Qual Patient Saf 2005;31:90–7 [DOI] [PubMed] [Google Scholar]
- 5.Gandhi TK. Fumbled handoffs: one dropped ball after another. Ann Intern Med 2005;142:352–8 [DOI] [PubMed] [Google Scholar]
- 6.Kuperman GJ, Teich JM, Tanasijevic MJ, et al. Improving response to critical laboratory results with automation: results of a randomized controlled trial. J Am Med Inform Assoc 1999;6:512–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Poon EG, Gandhi TK, Sequist TD, et al. ‘I wish I had seen this test result earlier!’: Dissatisfaction with test result management systems in primary care. Arch Intern Med 2004;164:2223–8 [DOI] [PubMed] [Google Scholar]
- 8.Singh H, Sethi S, Raber M, et al. Errors in cancer diagnosis: current understanding and future directions. J Clin Oncol 2007;25:5009–18 [DOI] [PubMed] [Google Scholar]
- 9.Bird S. Missing test results and failure to diagnose. Aust Fam Physician 2004;33:360–1 [PubMed] [Google Scholar]
- 10.Boohaker EA, Ward RE, Uman JE, et al. Patient notification and follow-up of abnormal test results. A physician survey. Arch Intern Med 1996;156:327–31 [PubMed] [Google Scholar]
- 11.Karcz A, Holbrook J, Burke MC, et al. Massachusetts emergency medicine closed malpractice claims: 1988–1990. Ann Emerg Med 1993;22:553–9 [DOI] [PubMed] [Google Scholar]
- 12.Osuch JR, Bonham VL, Morris LL. Primary care guide to managing a breast mass: a legal perspective on risk management. Medscape Women's Health 1998;3:3. [PubMed] [Google Scholar]
- 13.Callen JL, Westbrook JI, Braithwaite J. The effect of physicians' long-term use of CPOE on their test management work practices. J Am Med Inform Assoc 2006;13:643–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ferris TG, Johnson SA, Co JP, et al. Electronic results management in pediatric ambulatory care: qualitative assessment. Pediatrics 2009;123(Suppl 2):S85–91 [DOI] [PubMed] [Google Scholar]
- 15.Lin JJ, Dunn A, Moore C. Follow-up of outpatient test results: a survey of house-staff practices and perceptions. Am J Med Qual 2006;21:178–84 [DOI] [PubMed] [Google Scholar]
- 16.Bates DW, Gawande AA. Improving safety with information technology. N Engl J Med 2003;348:2526–34 [DOI] [PubMed] [Google Scholar]
- 17.Bates DW, Cohen M, Leape LL, et al. Reducing the frequency of errors in medicine using information technology. J Am Med Inform Assoc 2001;8:299–308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Poon EG, Wang SJ, Gandhi TK, et al. Design and implementation of a comprehensive outpatient Results Manager. J Biomed Inform 2003;36:80–91 [DOI] [PubMed] [Google Scholar]
- 19.Poon EG, Kuperman GJ, Fiskio J, et al. Real-time notification of laboratory data requested by users through alphanumeric pagers. J Am Med Inform Assoc 2002;9:217–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tate KE, Gardner RM. Computers, quality, and the clinical laboratory: a look at critical value reporting. Proc Annu Symp Comput Appl Med Care 1993:193–7 [PMC free article] [PubMed] [Google Scholar]
- 21.Hollensead SC, Lockwood WB, Elin RJ. Errors in pathology and laboratory medicine: consequences and prevention. J Surg Oncol 2004;88:161–81 [DOI] [PubMed] [Google Scholar]
- 22.Georgiou A, Williamson M, Westbrook JI, et al. The impact of computerised physician order entry systems on pathology services: a systematic review. Int J Med Inf 2007;76:514–29 [DOI] [PubMed] [Google Scholar]
- 23.Wahls TL, Cram PM. The frequency of missed test results and associated treatment delays in a highly computerized health system. BMC Fam Pract 2007;8:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hickner J, Graham DG, Elder NC, et al. Testing process errors and their harms and consequences reported from family medicine practices: a study of the American Academy of Family Physicians National Research Network. Qual Saf Health Care 2008;17:194–200 [DOI] [PubMed] [Google Scholar]
- 25.Shah RK, Kentala E, Healy GB, et al. Classification and consequences of errors in otolaryngology. Laryngoscope 2004;114:1322–35 [DOI] [PubMed] [Google Scholar]
- 26.Baig N, Myers RE, Turner BJ, et al. Physician-reported reasons for limited follow-up of patients with a postiive fecal occult blood test screening result. Am J Gastroenterol 2003;98:2078–81 [DOI] [PubMed] [Google Scholar]
- 27.Keren R, Muret-Wagstaff S, Goldmann DA, et al. Notifying emergency department patients of negative test results: pitfalls of passive communication. Pediatr Emerg Care 2003;19:226–30 [DOI] [PubMed] [Google Scholar]
- 28.Kuperman GJ, Boyle D, Jha A, et al. How promptly are inpatients treated for critical laboratory results? J Am Med Inform Assoc 1998;5:112–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Paltiel O, Gordon L, Berg D, et al. Effect of a computerized alert on the management of hypokalemia in hospitalized patients. Arch Intern Med 2003;163:200–4 [DOI] [PubMed] [Google Scholar]
- 30.Park HI, Min WK, Lee W, et al. Evaluating the short message service alerting system for critical value notification via PDA telephones. Ann Clin Lab Sci 2008;38:149–56 [PubMed] [Google Scholar]
- 31.Callen J, Paoloni R, Georgiou A, et al. The rate of missed test results in an emergency department. Methods Inf Med 2009;37–43 [DOI] [PubMed] [Google Scholar]
- 32.Kilpatrick ES, Holding S. Use of computer terminals on wards to access emergency test results: a retrospective audit [see comment]. BMJ 2001;322:1101–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Choksi V, Marn C, Bell Y, et al. Efficiency of a semiautomated coding and review process for notification of critical findings in diagnostic imaging. Am J Roentgenol 2006;186:933–6 [DOI] [PubMed] [Google Scholar]
- 34.Schiff GD, Kim S, Krosnjar N, et al. Missed hypothyroidism diagnosis uncovered by linking laboratory and pharmacy data. Arch Intern Med 2005;165:574–7 [DOI] [PubMed] [Google Scholar]
- 35.Block C, Laloum J, Rajs A, et al. Limitations of paperless on-line reporting of diagnostic bacteriology culture results. J Clin Pathol 1996;49:759–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Greenes DS, Fleisher GR, Kohane I. Potential impact of a computerized system to report late-arriving laboratory results in the emergency department. Pediatr Emerg Care 2000;16:313–15 [DOI] [PubMed] [Google Scholar]
- 37.Platzer P, Hauswirth N, Jaindl M, et al. Delayed or missed diagnosis of cervical spine injuries. J Trauma 2006;61:150–5 [DOI] [PubMed] [Google Scholar]
- 38.Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Intern Med 2007;49:196–205 [DOI] [PubMed] [Google Scholar]
- 39.Abujudeh HH, Kaewlai R, Choy G, et al. Important imaging finding e-mail alert system: experience after 3 years of implementation. Radiology 2009;252:747–53 [DOI] [PubMed] [Google Scholar]
- 40.Lundberg GD. Critical (panic) value notification: an established laboratory practice policy (parameter). JAMA 1990;263:709. [PubMed] [Google Scholar]
- 41.Stausberg J, Koch D, Ingenerf J, et al. Comparing paper-based with electronic patient records: lessons learned during a study on diagnosis and procedure codes. J Am Med Inform Assoc 2003;10:470–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Casalino LP, Dunham D, Chin MH, et al. Frequency of failure to inform patients of clinically significant outpatient test results. Arch Intern Med 2009;169:1123–9 [DOI] [PubMed] [Google Scholar]
- 43.Singh H, Arora HS, Vij MS, et al. Communication outcomes of critical imaging results in a computerized notification system. J Am Med Inform Assoc 2007;14:459–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bates DW, Pappius E, Kuperman GJ, et al. Using information systems to measure and improve quality. Int J Med Inform 1999;53:115–24 [DOI] [PubMed] [Google Scholar]
- 45.Leape LL. Error in medicine. JAMA 1994;272:1851–7 [PubMed] [Google Scholar]
- 46.Berg M. Patient care information systems and health care work: a sociotechnical approach. Int J Med Inform 1999;55:87–101 [DOI] [PubMed] [Google Scholar]
- 47.Singh H, Naik AD, Rao R, et al. Reducing diagnsotic errors through effective communication: harnessing the power of information technology. J Gen Intern Med 2007;23:489–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Berg M. Medical work and the computer-based patient record: a sociological perspective. Methods Inf Med 1998;37:294–301 [PubMed] [Google Scholar]
- 49.Aarts J, Berg M. Extending the understanding of computerized physician order entry: implications for professional collaboration, workflow and quality of care. Int J Med Inform 2007;76(Suppl 1):S4–13 [DOI] [PubMed] [Google Scholar]
- 50.Saxena S, Kempf R, Wilcox S, et al. Critical laboratory value notification: a failure mode effects and criticality analysis. Jt Comm J Qual Patient Saf 2005;31:495–506 [DOI] [PubMed] [Google Scholar]
- 51.Kost GJ. Critical limits for urgent clinician notification at US medical centers. JAMA 1990;263:704–7 [PubMed] [Google Scholar]
- 52.Kuperman GJ, Teich JM, Bates DW, et al. Detecting alerts, notifying the physician, and offering action items: a comprehensive alerting system. Proc AMIA Annu Fall Symp 1996:704–8 [PMC free article] [PubMed] [Google Scholar]
- 53.Shabot MM, LoBue M. Real-time wireless decision support alerts on a Palmtop PDA. Proc Annu Symp Comput Appl Med Care 1995:174–7 [PMC free article] [PubMed] [Google Scholar]
- 54.Rind DM, Safran C, Phillips RS, et al. The effect of computer-based reminders on the management of hospitalized patients with worsening renal function. Proc Annu Symp Comput Appl Med Care 1991:28–32 [PMC free article] [PubMed] [Google Scholar]
- 55.Tate KE, Gardner RM, Weaver LK. A computerized laboratory alerting system. MD Comput 1990;7:296–301 [PubMed] [Google Scholar]
- 56.McDonald CJ, Hui SL, Smith DM, et al. Reminders to physicians from an introspective computer medical record. A two-year randomized trial. Ann Intern Med 1984;100:130–8 [DOI] [PubMed] [Google Scholar]
- 57.Oguz KK, Yousem DM, Deluca T, et al. Impact of pager notification on report verification times. Acad Radiol 2002;9:954–9 [DOI] [PubMed] [Google Scholar]
- 58.Moore C, Wisnivesky J, Williams S, et al. Medical errors related to discontinuity of care from an inpatient to an outpatient setting [see comment]. J Gen Intern Med 2003;18:646–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Petersen LA, Orav EJ, Teich JM, et al. Using a computerized sign-out program to improve continuity of inpatient care and prevent adverse events. Jt Comm J Qual Improv 1998;24:77–87 [DOI] [PubMed] [Google Scholar]
- 60.Ye K, Mc DTD, Knott JC, et al. Handover in the emergency department: deficiencies and adverse effects. Emerg Med Australas 2007;19:433–41 [DOI] [PubMed] [Google Scholar]
- 61.van Walraven C, Seth R, Laupacis A. Dissemination of discharge summaries. Not reaching follow-up physicians. Can Fam Physician 2002;48:737–42 [PMC free article] [PubMed] [Google Scholar]
- 62.van Walraven C, Seth R, Austin PC, et al. Effect of discharge summary availability during post-discharge visits on hospital readmission. J Gen Intern Med 2002;17:186–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bolton P, Mira M, Kennedy P, et al. The quality of communication between hospitals and general practitioners: an assessment. J Qual Clin Pract 1998;18:241–7 [DOI] [PubMed] [Google Scholar]
- 64.Castleden WM, Stacey MC, Norman PE, et al. General practitioners' attitudes to computer-generated surgical discharge letters. Members of the Department of General Surgery, Fremantle Hospital. Med J Aust 1992;157:380–2 [DOI] [PubMed] [Google Scholar]
- 65.van Walraven C, Laupacis A, Seth R, et al. Dictated versus database-generated discharge summaries: a randomized clinical trial. CMAJ 1999;160:319–26 [PMC free article] [PubMed] [Google Scholar]
- 66.Kirby J, Barker B, Fernando DJ, et al. A prospective case control study of the benefits of electronic discharge summaries. J Telemed Telecare 2006;12(Suppl 1):20–1 [DOI] [PubMed] [Google Scholar]