Abstract
An almost universal side effect of long-term therapy with procainamide is the appearance of serum autoantibodies and less frequently a syndrome resembling lupus erythematosus. Previous studies demonstrated that procainamide-hydroxylamine (PAHA), a metabolite generated by hepatic mixed function oxidases, was highly toxic to dividing cells, but evidence that PAHA could be formed in the circulation was lacking. This study examines the capacity of neutrophils to metabolize procainamide to reactive forms. Neutrophils activated with opsonized zymosan were cytotoxic only if procainamide was present, whereas N-acetyl procainamide, which does not induce autoimmunity, was inert in this bioassay. PAHA was detected by HPLC in the extracellular medium if ascorbic acid was present. Generation of PAHA and cytotoxic procainamide metabolites was inhibited by NaN3 and catalase but not by superoxide dismutase, indicating that H2O2 and myeloperoxidase were involved. Nonactivated neutrophils and neutrophils from patients with chronic granulomatous disease did not generate cytotoxic PAHA, demonstrating that H2O2 was derived from the respiratory burst accompanying neutrophil activation. These conclusions were supported by results of a cell-free system in which neutrophils were replaced by myeloperoxidase and H2O2 or an H2O2 generating system. These studies demonstrate the capacity of neutrophils to mediate metabolism of procainamide and establish the role of myeloperoxidase released during degranulation and H2O2 derived from the respiratory burst in the direct cooxidation of procainamide to PAHA. The profound biologic activity of this metabolite and its possible generation within lymphoid compartments implicate this process in the induction of autoimmunity by procainamide.
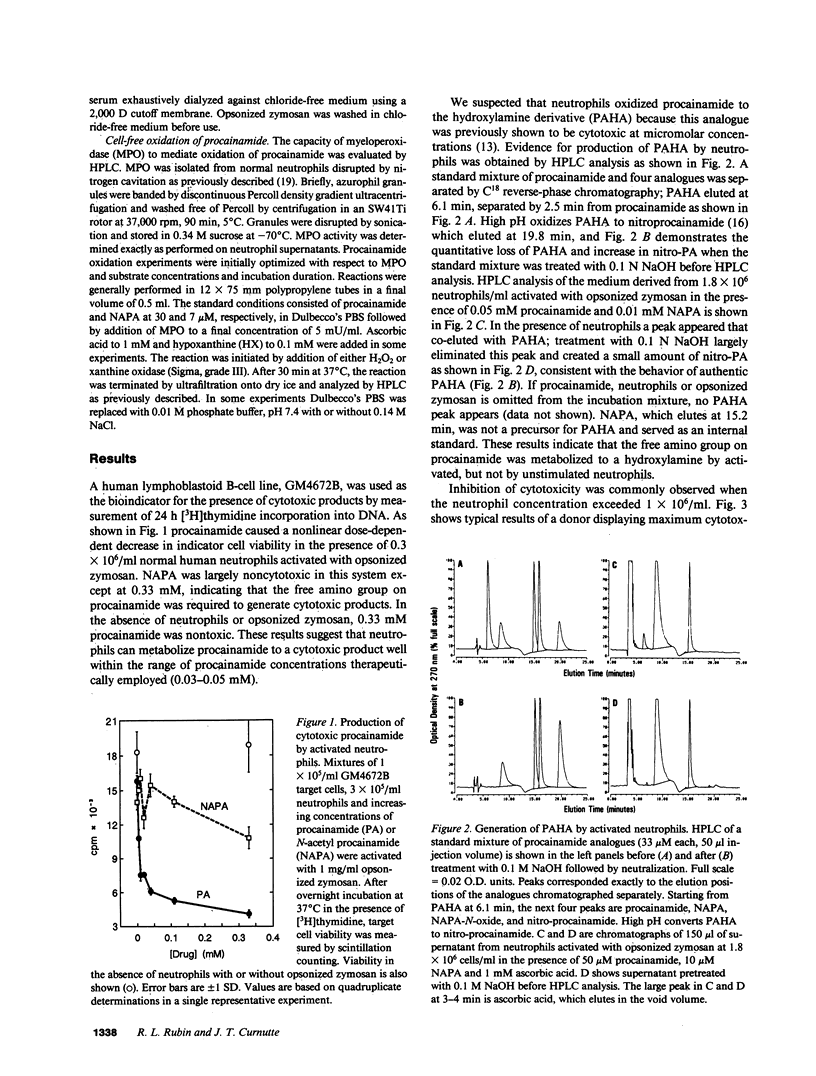
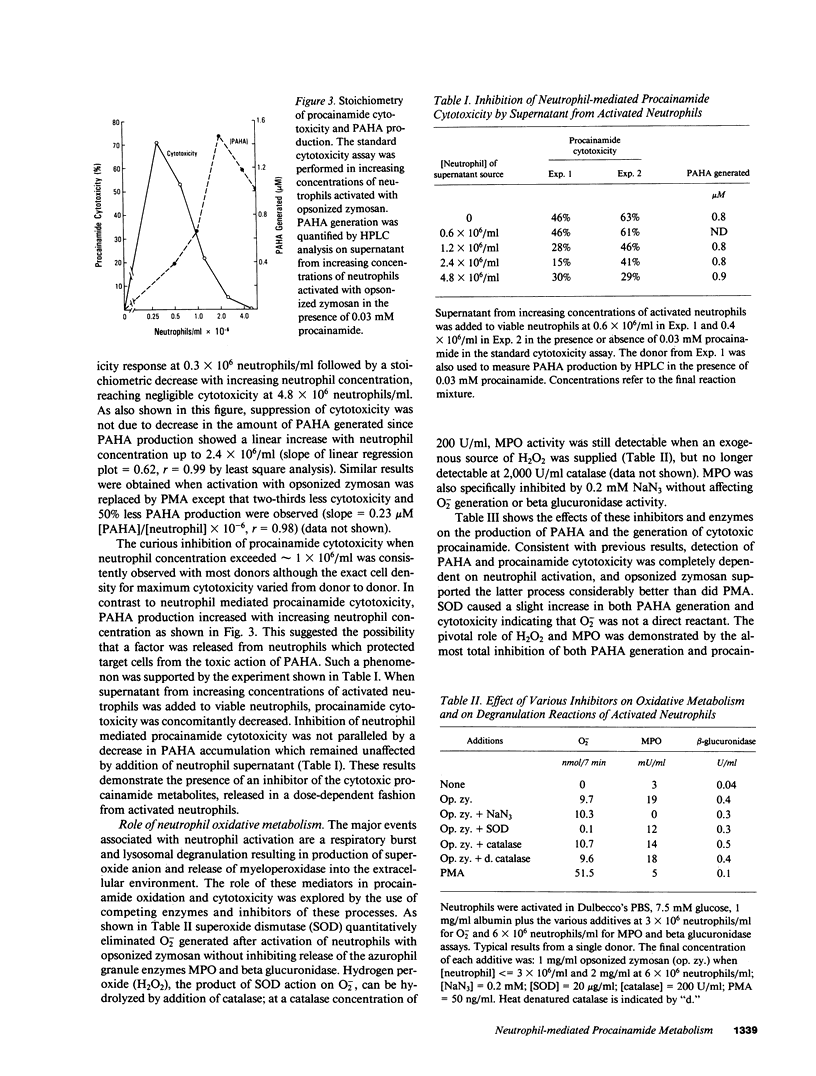
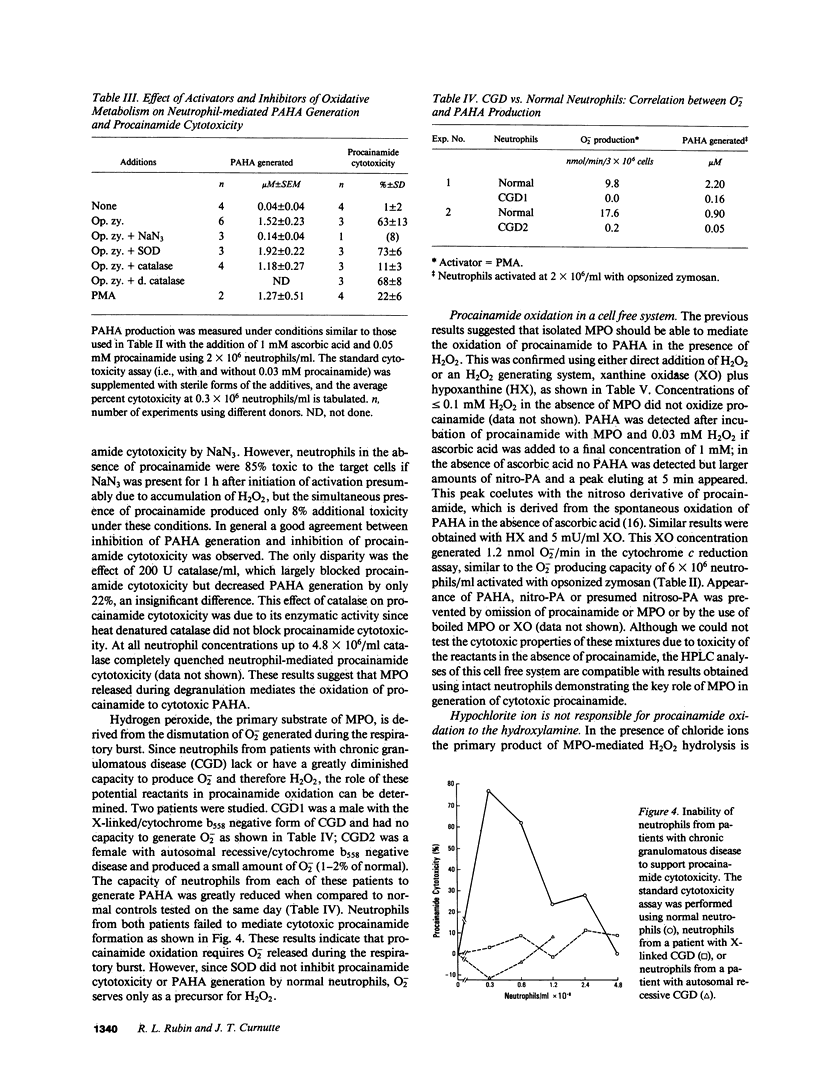
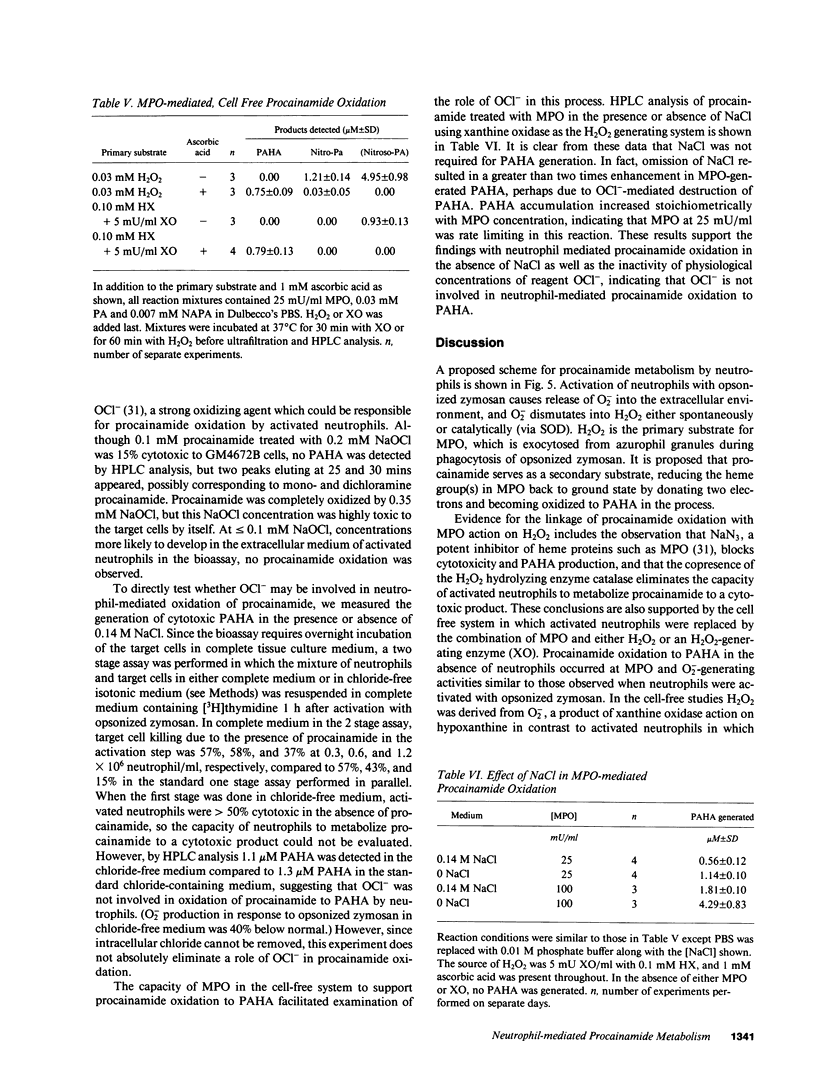
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bluestein H. G., Zvaifler N. J., Weisman M. H., Shapiro R. F. Lymphocyte alteration by procainamide: relation to drug-induced lupus erythematosus syndrome. Lancet. 1979 Oct 20;2(8147):816–819. doi: 10.1016/s0140-6736(79)92174-3. [DOI] [PubMed] [Google Scholar]
- Bretz U., Baggiolini M. Biochemical and morphological characterization of azurophil and specific granules of human neutrophilic polymorphonuclear leukocytes. J Cell Biol. 1974 Oct;63(1):251–269. doi: 10.1083/jcb.63.1.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brittinger G., Hirschhorn R., Douglas S. D., Weissmann G. Studies on lysosomes. XI. Characterization of a hydrolase-rich fraction from human lymphocytes. J Cell Biol. 1968 May;37(2):394–411. doi: 10.1083/jcb.37.2.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budinsky R. A., Roberts S. M., Coats E. A., Adams L., Hess E. V. The formation of procainamide hydroxylamine by rat and human liver microsomes. Drug Metab Dispos. 1987 Jan-Feb;15(1):37–43. [PubMed] [Google Scholar]
- Cornacchia E., Golbus J., Maybaum J., Strahler J., Hanash S., Richardson B. Hydralazine and procainamide inhibit T cell DNA methylation and induce autoreactivity. J Immunol. 1988 Apr 1;140(7):2197–2200. [PubMed] [Google Scholar]
- Curnutte J. T. Classification of chronic granulomatous disease. Hematol Oncol Clin North Am. 1988 Jun;2(2):241–252. [PubMed] [Google Scholar]
- Curnutte J. T., Kuver R., Scott P. J. Activation of neutrophil NADPH oxidase in a cell-free system. Partial purification of components and characterization of the activation process. J Biol Chem. 1987 Apr 25;262(12):5563–5569. [PubMed] [Google Scholar]
- DeChatelet L. R., McCall C. E., Cooper M. R., Shirley P. S. Ascorbic acid levels in phagocytic cells. Proc Soc Exp Biol Med. 1974 Apr;145(4):1170–1173. doi: 10.3181/00379727-145-37974. [DOI] [PubMed] [Google Scholar]
- Fujii S., Hitomi Y. New synthetic inhibitors of C1r, C1 esterase, thrombin, plasmin, kallikrein and trypsin. Biochim Biophys Acta. 1981 Oct 13;661(2):342–345. doi: 10.1016/0005-2744(81)90023-1. [DOI] [PubMed] [Google Scholar]
- Holmes B., Park B. H., Malawista S. E., Quie P. G., Nelson D. L., Good R. A. Chronic granulomatous disease in females. N Engl J Med. 1970 Jul 30;283(5):217–221. doi: 10.1056/NEJM197007302830501. [DOI] [PubMed] [Google Scholar]
- Johnston R. B., Jr, Lehmeyer J. E. Elaboration of toxic oxygen by-products by neutrophils in a model of immune complex disease. J Clin Invest. 1976 Apr;57(4):836–841. doi: 10.1172/JCI108359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klebanoff S. J., Hamon C. B. Role of myeloperoxidase-mediated antimicrobial systems in intact leukocytes. J Reticuloendothel Soc. 1972 Aug;12(2):170–196. [PubMed] [Google Scholar]
- Lahita R., Kluger J., Drayer D. E., Koffler D., Reidenberg M. M. Antibodies to nuclear antigens in patients treated with procainamide or acetylprocainamide. N Engl J Med. 1979 Dec 20;301(25):1382–1385. doi: 10.1056/NEJM197912203012506. [DOI] [PubMed] [Google Scholar]
- Lee S. L., CHase P. H. Drug-induced systemic lupus erythematosus: a critical review. Semin Arthritis Rheum. 1975 Aug;5(1):83–103. doi: 10.1016/0049-0172(75)90024-4. [DOI] [PubMed] [Google Scholar]
- Miller K. B., Salem D. Immune regulatory abnormalities produced by procainamide. Am J Med. 1982 Oct;73(4):487–492. doi: 10.1016/0002-9343(82)90326-6. [DOI] [PubMed] [Google Scholar]
- Ochi T., Goldings E. A., Lipsky P. E., Ziff M. Immunomodulatory effect of procainamide in man. Inhibition of human suppressor T-cell activity in vitro. J Clin Invest. 1983 Jan;71(1):36–45. doi: 10.1172/JCI110749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quie P. G., Kaplan E. L., Page A. R., Gruskay F. L., Malawista S. E. Defective polymorphonuclear-leukocyte function and chronic granulomatous disease in two female children. N Engl J Med. 1968 May 2;278(18):976–980. doi: 10.1056/NEJM196805022781802. [DOI] [PubMed] [Google Scholar]
- Roden D. M., Reele S. B., Higgins S. B., Wilkinson G. R., Smith R. F., Oates J. A., Woosley R. L. Antiarrhythmic efficacy, pharmacokinetics and safety of N-acetylprocainamide in human subjects: comparison with procainamide. Am J Cardiol. 1980 Sep;46(3):463–468. doi: 10.1016/0002-9149(80)90016-8. [DOI] [PubMed] [Google Scholar]
- Rubin R. L., Uetrecht J. P., Jones J. E. Cytotoxicity of oxidative metabolites of procainamide. J Pharmacol Exp Ther. 1987 Sep;242(3):833–841. [PubMed] [Google Scholar]
- SKOOG W. A., BECK W. S. Studies on the fibrinogen, dextran and phytohemagglutinin methods of isolating leukocytes. Blood. 1956 May;11(5):436–454. [PubMed] [Google Scholar]
- Tannen R. H., Weber W. W. Antinuclear antibodies related to acetylator phenotype in mice. J Pharmacol Exp Ther. 1980 Jun;213(3):485–490. [PubMed] [Google Scholar]
- Totoritis M. C., Tan E. M., McNally E. M., Rubin R. L. Association of antibody to histone complex H2A-H2B with symptomatic procainamide-induced lupus. N Engl J Med. 1988 Jun 2;318(22):1431–1436. doi: 10.1056/NEJM198806023182204. [DOI] [PubMed] [Google Scholar]
- Uetrecht J. P. Reactivity and possible significance of hydroxylamine and nitroso metabolites of procainamide. J Pharmacol Exp Ther. 1985 Feb;232(2):420–425. [PubMed] [Google Scholar]
- Uetrecht J. P., Sweetman B. J., Woosley R. L., Oates J. A. Metabolism of procainamide to a hydroxylamine by rat and human hepatic microsomes. Drug Metab Dispos. 1984 Jan-Feb;12(1):77–81. [PubMed] [Google Scholar]
- Uetrecht J., Zahid N., Rubin R. Metabolism of procainamide to a hydroxylamine by human neutrophils and mononuclear leukocytes. Chem Res Toxicol. 1988 Jan-Feb;1(1):74–78. doi: 10.1021/tx00001a013. [DOI] [PubMed] [Google Scholar]
- Van Epps D. E., Bender J. G., Steinkamp J. A., Chenoweth D. E. Modulation of neutrophil-reduced pyridine nucleotide content following stimulation with phorbol myristate acetate and chemotactic factors. J Leukoc Biol. 1985 Nov;38(5):587–601. doi: 10.1002/jlb.38.5.587. [DOI] [PubMed] [Google Scholar]
- Weinstein A. Drug-induced systemic lupus erythematosus. Prog Clin Immunol. 1980;4:1–21. [PubMed] [Google Scholar]
- Woosley R. L., Drayer D. E., Reidenberg M. M., Nies A. S., Carr K., Oates J. A. Effect of acetylator phenotype on the rate at which procainamide induces antinuclear antibodies and the lupus syndrome. N Engl J Med. 1978 May 25;298(21):1157–1159. doi: 10.1056/NEJM197805252982101. [DOI] [PubMed] [Google Scholar]
- Yu C. L., Ziff M. Effects of long-term procainamide therapy on immunoglobulin synthesis. Arthritis Rheum. 1985 Mar;28(3):276–284. doi: 10.1002/art.1780280307. [DOI] [PubMed] [Google Scholar]
- de Boccardo G., Drayer D., Rubin A. L., Novogrodsky A., Reidenberg M. M., Stenzel K. H. Inhibition of pokeweed mitogen-induced B cell differentiation by compounds containing primary amine or hydrazine groups. Clin Exp Immunol. 1985 Jan;59(1):69–76. [PMC free article] [PubMed] [Google Scholar]


