Abstract
Objective
Researchers commonly use the femoral shaft-tibial shaft angle (FS-TS) from knee radiographs to estimate the hip-knee-ankle angle (HKA) in studies examining risk factors for knee osteoarthritis (OA) incidence and progression. The objective of this study was to determine the relationship between HKA and FS-TS, depending on the method of calculating FS-TS and the direction and degree of knee deformity.
Methods
120 full-length digital radiographs were assigned, with 30 in each of four alignment groups (0.0° to 4.9°, and ≥ 5.0° of varus and valgus), from a large cohort of persons with and at risk of knee osteoarthritis. HKA and 5 measures of FS-TS (using progressively shorter shaft lengths) were obtained using Horizons Analysis Software, OAISYS Inc. The offsets between HKA and the different versions of FS-TS were calculated, with 95% confidence intervals (CI). Pearson correlations were calculated.
Results
In varus limbs use of a shorter shaft length increased the offset between HKA and FS-TS from 5.1° to 7.0°. The opposite occurred with valgus limbs (from 5.0° to 3.7°). Correlations between HKA and FS-TS for the whole sample of 120 individuals were excellent (r range 1.00 to 0.88). However, correlations for individual alignment groups were low to moderate, especially for the shortest-shaft FS-TS (r range 0.41 to 0.66).
Conclusions
The offsets obtained using the shorter FS-TS measurements vary depending on direction and degree of knee deformity, and therefore may not provide reliable predictions for HKA We recommend that full-length radiographs be used whenever an accurate estimation of HKA is required, although broad categories of alignment can be estimated with FS-TS.
Keywords: knee osteoarthritis, alignment, radiography, anatomic axis, mechanical axis, deformity
Symptomatic knee osteoarthritis (OA) with radiographic changes was estimated to affect between 6.7% and 16.7% of individuals over 45 years old in a 2005 review of studies performed in the United States.1 This rate is increasing, primarily due to demographic factors such as aging of the population, increasing rates of obesity and an increasing prevalence of traumatic osteoarthritis.2 Varus or valgus alignment of the lower limb has been shown to increase the risk of progression of knee OA.3–8 More specifically, the odds ratio (OR) of OA progression in the medial tibiofemoral compartment for those with varus deformity has been calculated to be between 2.90 and 10.96.3, 4, 6, 7 For progression of lateral compartment OA in individuals with valgus deformity the OR is between 1.39 and 10.44.3, 4, 6, 7
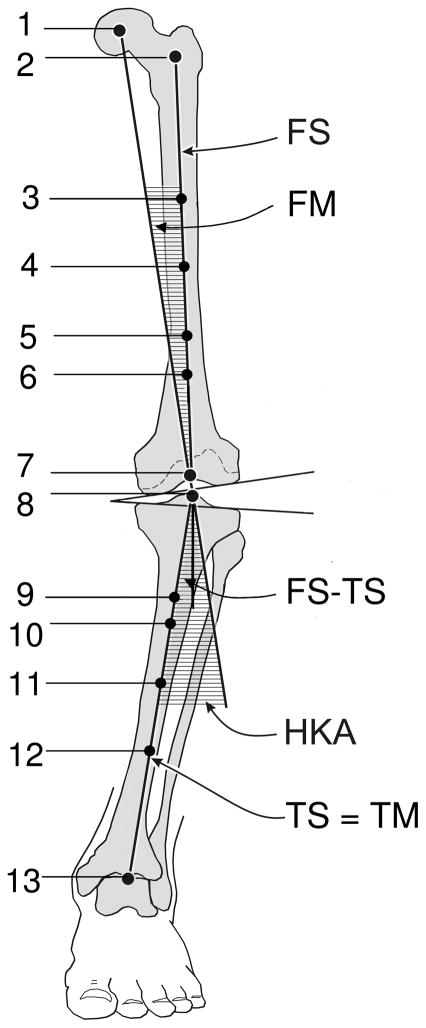
The hip-knee-ankle angle (HKA) is a measure of lower limb alignment, defined as the angle between the mechanical axes of the femur and the tibia (Figure 1). HKA is measured from a full-length lower-limb radiograph. In healthy adults with a neutral alignment, HKA is between 1.0° and 1.5° of varus.9, 10 The femoral shaft-tibial shaft angle (FS-TS) is the angle between the anatomic axes of the femur and the tibia (Figure 1). Many advocate the use of FS-TS taken from radiographs of the knee to estimate HKA, with or without an offset, which is the difference between HKA and FS-TS.11–13 They argue that there is a high correlation (r = 0.65 to 0.88) between HKA and FS-TS, and that there are several advantages of a knee radiograph over a full-length one. However, others argue that in order to obtain the best estimate of mechanical alignment, HKA must be directly measured from full-limb radiographs, because using a knee radiograph limits the accuracy of the measurement.14, 15 Deformities of shafts of the long bones might alter the relationship between HKA and FS-TS, as may subluxation at the knee.15–17
Figure 1.
Diagram of a full-length lower limb radiograph with a varus alignment. Mechanical and anatomic axes as well as the various angles are represented. The points marked on the radiograph in order to calculate the hip-knee-ankle angle (HKA) and the various femoral shaft-tibial shaft angles (FS-TS) are numbered 1 to 13. 1 – centre of head of femur, 2 – femoral intertrochanteric point, 3 – ⅔ femoral shaft point, 4 – ½ femoral shaft point, 5 – ⅓ femoral shaft point, 6 – 10 cm femoral shaft point, 7 – femoral intercondylar point, 8 – tibial interspinous point, 9 – 10 cm tibial shaft point, 10 – ⅓ tibial shaft point, 11 – ½ tibial shaft point, 12 – ⅔ tibial shaft point, 13 – tibial mid-plafond point. FS – femoral shaft (femoral anatomic axis), FM – femoral mechanical axis, TS – tibial shaft (tibial anatomic axis), TM – tibial mechanical axis, HKA – hip-knee-ankle angle, FS-TS – femoral shaft-tibial shaft angle.
Modified from Cooke et al. J Rheumatol 2007;34:1796–1801, with permission.
One factor which might influence the ability of FS-TS to accurately estimate HKA is the method used to calculate FS-TS. Statistically significant differences in FS-TS measurements have been found depending on how the anatomic axes were measured.10, 18 FS-TS is commonly measured on knee radiographs using lines drawn from the knee to a point 10 cm along the shafts of the long bones.11, 13, 14 However, the use of other locations for the shaft points might change the relationship of FS-TS to HKA. Therefore, we wished to compare several different versions of FS-TS, using different points of origin, to estimate HKA. An important consideration is that for the results to be useful the shaft points must be visible on commonly acquired radiographs.
It is also possible that the relationship between HKA and FS-TS might vary with respect to the nature (varus or valgus) and severity of deformity. We were unable to find any prior studies that evaluated this question. Therefore, we wished to study this relationship in cohorts of individuals with mild and severe varus and valgus deformities.
Thus, the aim of the current study was to determine the relationship between HKA and FS-TS in subjects with or at high risk of knee osteoarthritis. We asked three research questions. Does the relationship between FS-TS and HKA differ depending on direction and magnitude of knee deformity? Does the shaft length used to determine FS-TS affect its ability to accurately estimate HKA? What proportions of the femoral and tibial shafts are seen on a typical knee x-ray? The results of this study will inform researchers who perform clinical and epidemiological studies which method of measuring lower limb alignment best suites their needs.
Patients and Methods
The database of full-length lower limb radiographs from the Multicenter Osteoarthritis (MOST) Study was used to select images for this study. The MOST study was approved by institutional review boards at the University of Iowa, University of Alabama, Birmingham, University of California, San Francisco and Boston University Medical Campus and participants provided written informed consent. All of the participants in the MOST study either had knee OA or were at high risk for developing knee OA. This included individuals who were overweight or obese, those with current knee pain or a history of knee injury or surgery.6 Individuals were excluded if they had rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, Reiter’s syndrome, significant kidney disease, cancer, bilateral knee replacement, were unable to walk without assistance or were planning to move out of the study area in the next three years.6 Full-length films were obtained from 1598 subjects, according to the method of Sharma et al.7, with both right and left limbs viewed. Various joint angles (including HKA) and limb lengths had previously been determined as described by Cooke et al.19 The reliability of this technique has been confirmed [inter-reader reliability for HKA: Intraclass correlation coefficient (ICC) = 0.995 [95% confidence interval (CI), 0.994 – 1]; intra-reader reliability for HKA: ICC = 0.998 (95% CI, 0.998 – 1); inter-reader reliabilities for other angles between the femur and tibia: ICCs between 0.839 and 0.993; intra-reader reliabilities for other angles between the femur and tibia: ICCs between 0.908 and 0.998].20 To avoid selecting both limbs from the same subject only right limbs were selected. Limbs that showed fractures, pins or plates and hip or knee replacements were excluded, as were those where full analysis was not possible because of poor image quality or because some of the limb was not visible on the image. Finally, chosen images must have had a ruler to allow for scaling. Thus 1240 limb images were available for analysis. From these, 30 right limbs were randomly selected for each of four categories, based on HKA; group 1: HKA of 5.0° varus or greater, group 2: HKA from 0.0° up to and including 4.9° varus, group 3: HKA from 0.1° up to and including 4.9° valgus, and group 4: HKA of 5.0° valgus or greater. Group 1 was chosen from 181 individuals (14.6% of the available limb images), group 2 from 598 individuals (48.2%), group 3 from 406 individuals (32.7%) and group 4 from 55 individuals (4.4%). We attempted to select each group so that it would contain balanced representation of the sexes. While equal numbers of radiograph images were selected for each sex for 3 of the 4 HKA-based alignment groups, only 2 male subjects had valgus deformities of greater than 5°. Both were included in group 4. The groups were compared with respect to demographic variables [age, weight, height, body mass index (BMI) and Kellgren-Lawrence grade (K/L)] using t-tests for continuous variables and Chi-square for ordinal variables (Table 1). K/L grade was significantly associated with group (χ2 = 55.8, p<0.0001). Subjects with greater deformity (varus and valgus) more often had osteoarthritis, based on K/L grade.
Table 1.
Demographic data, with mean and standard deviation, for each alignment group.
| Group | HKA | Sex % of women | Age mean (yrs.) SD (yrs.) |
Weight mean (kg) SD (kg) |
Height mean (mm) SD (mm) |
BMI mean (kg/m2) SD (kg/m2) |
K/L Grade % grade 2 or greater |
|---|---|---|---|---|---|---|---|
| Complete Dataset | 61% | 63.0 8.4 |
89.3 16.0 |
1682 91 |
31.6 5.8 |
51% | |
| 1 | ≥ 5.0° Varus | 50% | 62.4 9.5 |
93.7 15.6 |
1674 109 |
33.8 6.8 |
70% |
| 2 | between 0.0° – 4.9° Varus | 50% | 61.5 8.0 |
88.8 18.3 |
1683 85 |
31.4 6.0 |
33% |
| 3 | between 0.0° – 4.9° Valgus | 50% | 63.9 9.1 |
86.8 13.1 |
1722 94 |
29.2 3.3 |
20% |
| 4 | ≥ 5.0° Valgus | 93% | 64.2 7.0 |
87.8 16.4 |
1652 61 |
32.2 5.9 |
80% |
| Significant Differences (p < 0.05) | none | none | 3 & 4 p = 0.025 |
1 & 3 p = 0.022 |
A custom version of Surveyor 2.0 software from Orthopaedic Alignment & Imaging Systems Inc. (OAISYS) was used to determine HKA and several variations of FS-TS on the full-length radiographs (Figure 1). Points were placed on the images with digital “tools” (center-line, circle, ruler), using strict criteria to minimize bias. For measurements of HKA, points placed at the centre of the femoral head, the femoral intercondylar notch, the tibial interspinous groove and at the centre of the tibial plafond were used. The first two points defined the femoral mechanical axis and the second two points defined the tibial mechanical axis. The angle at the intersection of the two lines was HKA, with negative numbers indicating varus alignment and positive numbers indicating valgus alignment. For full-length FS-TS, the points were located at the intertrochanteric point between the greater and lesser femoral trochanters in line with the femoral neck axis and at the femoral intercondylar notch (femoral anatomic axis), as well as at the tibial interspinous groove and at the centre of the tibial plafond (tibial anatomic axis). The angle between these axes defined the full-length FS-TS. Three additional points were located on the mid-shaft of the femur, two thirds, one half and one third of the length of the femoral shaft from the knee. Corresponding points were located on the mid-shaft of the tibia. Finally, points were located on the femoral and tibial shafts 10 cm from the knee points. The shaft points were used to calculate four different FS-TS angles, described as ⅔ FS-TS, ½ FS-TS, ⅓ FS-TS and 10 cm FS-TS. To minimize bias, the points were marked in proximal to distal order, and the resulting angles were not reviewed until after all points were marked. The images were analysed in order of acquisition rather than by group.
Mean offset was defined as the mean HKA minus the mean FS-TS. Mean offsets and 95% confidence intervals (CI) between HKA and the different methods of calculating FS-TS were determined for the complete sample of 120 limbs and for each alignment group. Pearson correlation coefficients (CC) were used to compare HKA and the different methods of calculating FS-TS, for the complete sample and separately for each alignment group. To determine if the relationship between FS-TS and HKA differed depending on direction and magnitude of knee deformity, the size of the mean offsets was examined between alignment groups and compared to that of the complete sample. CIs and CCs were used to study the ability of the various FS-TS measurements to accurately estimate HKA.
To determine any effect of sex on the results we carried out a 2-way analysis of variance (ANOVA) to compare sex differences with group, sex and group*sex as factors, for all of the alignment angles and mean offsets. Post-hoc Tukey analyses were performed as needed. Group 4 was not included due to insufficient numbers of male subjects. For groups 1 to 3 there were no group*sex interactions or sex main effects for the angles and offsets, with two exceptions. Sex had a main effect for the angle 10 cm FS-TS and the offset HKA – 10 cm FS-TS (Table 2). However, we did not find significant offset sex differences in the offsets among alignment groups.
Table 2.
Means and 95% confidence intervals (CI) for lower limb angles and (HKA - FS-TS) offsets, divided by sex. Group 4 was not included in the ANOVA to compare group and sex due to insufficient male subjects.
| a) Lower limb angles | ||||||||
|---|---|---|---|---|---|---|---|---|
| Group | Sex | HKA mean (°) CI (°) |
FS-TS mean (°) CI (°) |
⅔ FS-TS mean (°) CI (°) |
½ FS-TS mean (°) CI (°) |
⅓ FS-TS mean (°) CI (°) |
10cm FS-TS mean (°) CI (°) |
|
| Complete Dataset | 73 ♀ | 1.4 (0.0, 2.8) | 6.4 (5.1, 7.8) | 7.3 (6.0, 8.5) | 6.8 (5.6, 7.9) | 6.2 (5.1, 7.3) | 6.0* (4.9, 7.1) | |
| 47 ♂ | −2.0 (−3.4, −0.5) | 3.0 (1.6, 4.5) | 4.2 (2.8, 5.5) | 4.1 (2.8, 5.4) | 4.0 (2.8, 5.3) | 4.6* (3.3, 5.8) | ||
| 1 | ≥ 5.0° Varus | 15 ♀ | −7.0 (−7.6, −6.3) | −1.5 (−2.3, −0.7) | 0.1 (−0.7, 1.0) | 0.3 (−0.6, 1.2) | 0.2 (−0.9, 1.3) | 0.3 (−0.9, 1.5) |
| 15 ♂ | −7.7 (−8.7, −6.7) | −2.6 (−3.5, −1.7) | −1.2 (−2.0, −0.3) | −0.9 (−2.1, 0.2) | −0.7 (−2.0, 0.6) | −0.2 (−1.7, 1.4) | ||
| 2 | between 0.0° – 4.9° Varus | 15 ♀ | −2.6 (−3.4, −1.8) | 2.3 (1.5, 3.1) | 3.8 (2.8, 4.7) | 3.9 (2.9, 4.8) | 3.6 (2.3, 4.9) | 3.5 (2.1, 4.9) |
| 15 ♂ | −2.0 (−2.6, −1.4) | 2.9 (2.3, 3.5) | 4.3 (3.6, 5.0) | 4.5 (3.7, 5.3) | 4.6 (3.8, 5.3) | 5.2 (4.4, 6.1) | ||
| 3 | between 0.1° – 4.9° Valgus | 15 ♀ | 2.0 (1.2, 2.7) | 7.1 (6.4, 7.8) | 7.4 (6.6, 8.2) | 6.6 (5.6, 7.5) | 5.7 (4.7, 6.7) | 5.4 (4.3, 6.6) |
| 15 ♂ | 2.0 (1.4, 2.6) | 6.9 6.3, 7.5) | 7.6 (6.8, 8.3) | 7.2 (6.4, 8.0) | 6.9 (6.1, 7.7) | 7.4 (6.4, 8.4) | ||
| 4 | ≥ 5.0° Valgus | 28 ♀ | 7.7 (7.0, 8.5) | 12.6 (11.8, 13.4) | 12.9 (12.0, 13.8) | 11.9 (11.0, 12.9) | 11.0 (10.0, 12.0) | 10.7 (9.6, 11.8) |
| 2 ♂ | 12.0 (9.9, 14.0) | 17.3 15.0, 19.7) | 17.3 (16.2, 18.3) | 15.6 (15.0, 16.2) | 14.4 (14.0, 14.8) | 13.7 (12.6, 14.7) | ||
| b) Lower limb (HKA – FS-TS) offsets | |||||||
|---|---|---|---|---|---|---|---|
| Group | Sex | HKA – FS-TS mean (°) CI (°) |
HKA – ⅔ FS-TS mean (°) CI (°) |
HKA – ½ FS-TS mean (°) CI (°) |
HKA – ⅓ FS-TS mean (°) CI (°) |
HKA – 10 cm FS-TS mean (°) CI (°) |
|
| Complete Dataset | 73 ♀ | −5.0 (−5.2, −4.9) | −5.9 (−6.2, −5.6) | −5.4 (−5.8, −5.0) | −4.7 (−5.3, −4.2) | −4.6* (−5.2, −4.0) | |
| 47 ♂ | −5.0 (−5.2, −4.8) | −6.1 (−6.4, −5.8) | −6.1 (−6.5, −5.6) | −6.0 (−6.6, −5.4) | −6.5* (−7.3, −5.8) | ||
| 1 | ≥ 5.0° Varus | 15 ♀ | −5.4 (−5.7, −5.1) | −7.1 (−7.5, −6.7) | −7.3 (−7.8, −6.7) | −7.2 (−8.0, −6.3) | −7.2 (−8.2, −6.2) |
| 15 ♂ | −5.1 (−5.4, −4.8) | −6.5 (−7.1, −6.0) | −6.8 (−7.7, −5.9) | −7.0 (−8.2, −5.7) | −7.5 (−9.1, −6.0) | ||
| 2 | between 0.0° – 4.9° Varus | 15 ♀ | −4.9 (−5.3, −4.6) | −6.4 (−7.0, −5.8) | −6.5 (−7.2, −5.7) | −6.2 (−7.3, −5.1) | −6.2 (−7.4, −4.9) |
| 15 ♂ | −4.9 (−5.2, −4.6) | −6.3 (−6.8, −5.8) | −6.5 (−7.1, −5.8) | −6.5 (−7.3, −5.8) | −7.2 (−8.1, −6.4) | ||
| 3 | between 0.1° – 4.9° Valgus | 15 ♀ | −5.1 (−5.4, −4.9) | −5.4 (−5.9, −5.0) | −4.6 (−5.2, −4.0) | −3.8 (−4.6, −3.0) | −3.5 (−4.4, −2.6) |
| 15 ♂ | −4.9 (−5.3, −4.5) | −5.6 (−6.3, −5.0) | −5.3 (−6.0, −4.5) | −4.9 (−5.7, −4.1) | −5.5 (−6.4, −4.6) | ||
| 4 | ≥ 5.0° Valgus | 28 ♀ | −4.9 (−5.0, −4.7) | −5.2 (−5.6, −4.8) | −4.2 (−4.8, −3.7) | −3.2 (−4.0, −2.5) | −2.9 (−3.8, −2.1) |
| 2 ♂ | −5.4 (−5.6, −5.1) | −5.3 (−6.3, −4.3) | −3.7 (−5.1, −2.2) | −2.5 (−4.9, 0.0) | −1.7 (−4.8, 1.4) | ||
sex main effect, p < 0.05
All statistical analyses were performed using Minitab™ statistical software (Release 15.1.30, Minitab Inc., State College, Pennsylvania). Statistical significance was set at α = 0.05 (two-sided) for all tests.
Finally, the proportion of the femoral and tibial shafts visible on a typical knee radiograph was determined. Typical radiograph cassettes and digital radiograph systems have an exposure area that is 16.5 or 17.0 inches (419 or 432 mm) long. All 120 right limbs were reviewed to determine what proportion of the shaft lengths would be visible on a 419 mm long image.
Results
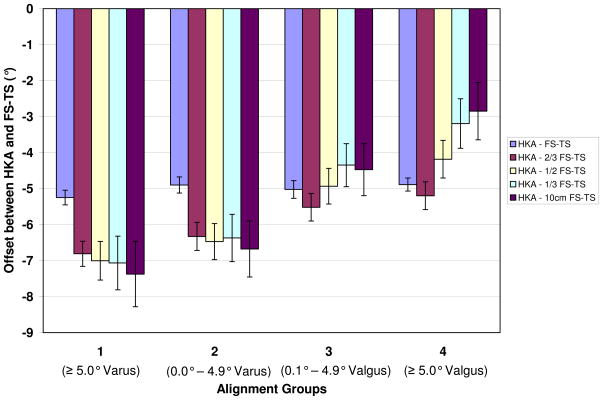
To investigate the relationship between HKA - FS-TS offset, FS-TS shaft length and alignment group, mean offsets and 95% CIs were calculated and plotted (Figure 2). The average offset between the mechanical and anatomic axes (full-length FS-TS) for the entire dataset was −5.0° (95% CI, −5.1, −4.9). However, when the sample was broken down into alignment groups, substantial variability was evident. For limbs with a varus deformity the magnitude of the offset increased as the shaft length for the FS-TS calculation decreased. But for limbs with a valgus deformity, the magnitude of this offset decreased. Similarly, the data for the individual alignment groups revealed much weaker correlations. Linear regression equations for HKA vs. 10 cm FS-TS were as follows: group 1 (severe varus) HKA = −7.34 + 0.266 10cm FS-TS; group 2 (mild varus) HKA = −3.47 + 0.267 10cm FSTS; group 3 (mild valgus) HKA = 0.039 + 0.298 10cm FSTS; and group 4 (severe valgus) HKA = 2.67 + 0.491 10cm FSTS.
Figure 2.
Mean offsets (with 95% confidence intervals) between HKA and the different methods of determining FS-TS, for each alignment group.
FS-TS shaft length appears to influence the ability to estimate HKA. When we examined the correlation between HKA and FS-TS, we found that correlations for the entire sample were high (r > 0.88) (Table 3). However the correlations were much weaker for shorter-shaft FS-TS measurements. Despite the sex main effect for HKA – 10 cm FS-TS the correlations for the entire sample divided into males (r = 0.87) and females (r = 0.89) were very similar.
Table 3.
Pearson correlations (r) between HKA and the different methods of measuring FS-TS. p < 0.05 in each case.
| Group | HKA vs. FS-TS r |
HKA vs. ⅔ FS-TS r |
HKA vs. ½ FS-TS r |
HKA vs. ⅓ FS-TS r |
HKA vs. 10 cm FS-TS r |
|
|---|---|---|---|---|---|---|
| Complete Dataset | 1.0 | 0.98 | 0.96 | 0.92 | 0.88 | |
| 1 | ≥ 5.0° Varus | 0.95 | 0.85 | 0.71 | 0.52 | 0.41 |
| 2 | between 0.0° – 4.9° Varus | 0.90 | 0.74 | 0.62 | 0.51 | 0.45 |
| 3 | between 0.1° – 4.9° Valgus | 0.87 | 0.73 | 0.60 | 0.50 | 0.50 |
| 4 | ≥ 5.0° Valgus | 0.98 | 0.91 | 0.82 | 0.72 | 0.66 |
Finally, we investigated how much of the femoral and tibial shafts are visible on a typical knee radiograph. Presuming that the knee was centered perfectly on the image, a 419 mm long radiograph image showed approximately 208 mm above and 208 mm below the joint line. One-third of the tibial and femoral shafts were seen on all images, as were the 10 cm points. One-half of the femoral shaft was seen on the shortest limbs (23% of the 120 limbs in the sample) and one-half of the tibial shaft was seen on most of the limbs (92% of the limbs). The two-thirds femoral and two-thirds tibial shaft points were not seen on limbs of any length.
Discussion
Several studies have investigated the relationship between HKA and FS-TS.11–14, 21 The current study, to our knowledge, is the first to suggest that the relationship between HKA and FS-TS differs depending on the direction and degree of deformity of the lower limb. Also, we found that using shorter FS-TS shaft lengths to estimate HKA modestly weakened the relation of anatomic axis with mechanical axis in the overall sample. The relation of these two measures was especially attenuated when both shorter shaft lengths were used and subcategories of alignment were studied.
The four alignment groups’ demographics did not differ significantly, with a few exceptions. Only two males in the entire MOST database had HKA angles of greater than 5° valgus. The rarity of valgus deformity in males has been noted before9, 11, 22 and partly explains the difference in height between groups three and four. Those with greater deformities (varus or valgus) had higher K/L grades and tended to have higher BMIs.
With only two exceptions no significant differences were found between the sexes with respect to the various angles and offsets, similar to prior results from adults with11 and without knee OA16, 18 However, in contrast to the current study, a difference has previously been found in HKA and (HKA – FS-TS) offsets between the sexes.11, 12, 17 The offset for females has been reported to be between 3.0° and 3.5° while that for males was between 4.7° to 6.4°.11, 12 Chang et al.17 reported the opposite trend, with females having a larger offset than males (7.3° versus 6.0°, FS-TS measured with 15 cm shaft lengths), at least for individuals with knee OA. Further comparisons of males and females need to be performed to confirm if real differences exist and in what direction.
Research question 1 asked whether the relationship between FS-TS and HKA differs depending on the direction and magnitude of knee deformity. Our average offset between HKA and full-length FS-TS of 5.0° is similar to findings from other studies where 4° – 6° is typically considered as the difference.10, 11, 21, 23 However, our data show that the HKA – FS-TS offset varied as a function of the degree of deformity, especially for FS-TS measures made using shorter shaft lengths. Specifically, for varus limbs the offset increased and for valgus limbs, it decreased. Therefore when dealing with individuals with significant varus or valgus deformity, it would be inaccurate to use 5.0° as the difference between HKA and the shorter-shaft versions of FS-TS, as FS-TS measurements vary widely from HKA.
Research question 2 asked whether the shaft length used to determine FS-TS affects its ability to accurately estimate HKA. As the FS-TS shaft length decreased, the confidence limits around our offsets increased and the correlations for the individual alignment groups decreased from greater than r = 0.87 (for HKA – full-length FS-TS) to less than r = 0.66 (for HKA – 10 cm FS-TS) (Table 3), contributing to a poor estimate for HKA. Prior studies, using 10 cm shaft lengths and the same knee points as in the current study, have found poor to excellent correlations between HKA and FS-TS (r = 0.27 to r = 0.88 for FS-TS obtained with standing radiographs11, 13, 14, 17 and r = 0.66 to r = 0.75 for FS-TS obtain with fixed-flexion radiographs11, 21). Some of these studies had a wide variety of subjects with varus, valgus and neutral lower limb alignments (r = 0.27 to 0.80)11, 17, 21 while others only used subjects with medial compartment OA, which is associated with varus alignment (r = 0.34 to 0.88).13, 14 When our subject sample was broken down into alignment strata the correlations become much weaker, especially for the ⅓ and 10 cm FS-TS calculations. One limitation of performing correlations on subgroups of a dataset is that because each group is limited to individuals within a small range of HKA values, the correlations will be attenuated. However, we also found that the correlations became weaker as the FS-TS shaft lengths decreased. Confidence limits around the HKAs imputed were wide enough to suggest caution when using ⅓ FS-TS and 10 cm FS-TS measurements to estimate HKA.
Several authors have reported results similar to ours when comparing different methods of calculating FS-TS, including greater variation between the mechanical axis and distal femoral anatomic axis than the full-length anatomic axis, and a higher correlation (r = 0.65, p < 0.0001) between HKA and FS-TS calculated using the mid-diaphyseal lines of the femur and tibia than 10 cm FS-TS (r = 0.34, p = 0.005).14, 18 As well, FS-TS measurements taken using a 15 cm shaft length (r = 0.81 for males, r = 0.88 for females) had greater correlations to HKA than those taken using a 10 cm shaft length (r = 0.69 for males, r = 0.80 for females).17 These studies lend support to our contention that short-shaft FS-TS measurements increase uncertainty if used to estimate HKA.
HKA measurements allow the opportunity to study the contribution of various parts of the limb to alignment.9, 24 Geometric changes in the shafts of the bones may cause some of the discordance between HKA and FS-TS.9, 17 These changes might predispose individuals to knee OA or may be brought on by bone remodelling that occurs with OA development.9, 17
Research question 3 asked what proportions of the femoral and tibial shafts are seen on a typical knee x-ray. Much of the prior research comparing HKA and FS-TS uses FS-TS measurements calculated using a 10 cm shaft length.11, 13, 14 The results show that one-third of the femoral and tibial shafts are visible on the average cassette, even for the tallest subjects. Unfortunately, the correlations are similarly poor for the 10 cm and ⅓ FS-TS comparisons to HKA.
One limitation to this study is that the various FS-TS measurements were determined from full-length radiographs rather than anteroposterior knee radiographs which are commonly used in research investigating the incidence and progression of knee OA. FS-TS calculated from full-length radiographs and anteroposterior knee radiographs have never been compared, however Kraus et al.11 found a good correlation (r = 0.73, p < 0.0001) between FS-TS measured from semiflexed knee radiographs and FS-TS measured from full-length radiographs.
This study has practical implications with respect to the measurement of lower-limb alignment for research purposes. There are significant limitations to using FS-TS to predict lower-limb alignment, especially when an accurate measurement of mechanical alignment is required and we recommend that HKA be used to determine lower-limb alignment. However, for samples with a variety of varus and valgus limbs and where broad categories of alignment are required for large numbers of persons in a study, FS-TS could be used with the correction factors we provide to categorize subjects as varus or valgus, with the recognition that limbs close to neutral will be hard to accurately classify. For subgroup studies, such as those of medial knee OA, categorizing limbs will produce more accurate estimates (i.e. all will probably be varus), but since there is uncertainty around each of the correction factors (see confidence intervals in tables), estimation of HKA from FS-TS is imperfect and using FS-TS to guess the exact HKA in individuals is problematic.
This caution also pertains to the use of lower-limb alignment to estimate joint space narrowing in the progression of knee OA. If FS-TS is used to estimate HKA, which in turn is used to estimate joint space narrowing, any error will be compounded. In individuals with severe valgus deformity, valgus malalignment severity would be underestimated using FS-TS, and thus any joint space change would be underestimated. Conversely, for individuals with severe varus deformity, the degree of varus malalignment would be overestimated using FS-TS and any joint space change would be overestimated.
In conclusion, we recommend that full-length radiographs be used whenever an accurate estimation of HKA is required. This is because the offset between HKA and short-shaft FS-TS measurements is variable, and is influenced by the direction and degree of malalignment of the lower limb. Imprecision around the correction factor would make it challenging to accurately predict an individual’s mechanical axis. However, broad categories of alignment in groups of persons can be estimated using short limb films, especially if the sample includes a variety of limbs that are varus, neutral and valgus.
Acknowledgments
Financial support was provided by NIH AR47785 and by AR051568. Software was provided courtesy of OAISYS, Inc.
We acknowledge Chris Wale for modifying the OAISYS Surveyor 2.0 software program for this study.
Declaration of Funding and Role of Funding Sources
Funding for the MOST was obtained through NIH and NIA under the following grant numbers: AG18820, AB18832, AG18947 and AG19069. Funding for this Ancillary Project of the MOST study was obtained from D. Felson, Boston University School of Medicine. D. Felson is one of the authors of this manuscript and had a role in the design of the study, the acquisition and interpretation of data, revising the manuscript for important intellectual content and final approval of the manuscript.
Footnotes
Competing Interest Statement
Dr. Cooke is President and principle shareholder of OAISYS Inc, a medical device company specializing in the analysis of radiographic images. Nothing of commercial value was received from any source during the course of this investigation.
Declaration of Authors’ Contributions
| Lisa Sheehy | David Felson | YuQing Zhang | Jingbo Niu | Yuk-Miu Lam | Neil Segal | John Lynch | T.D.V. Cooke | |
| Conception and design | √ | √ | √ | |||||
| Analysis and interpretation of the data | √ | √ | √ | √ | √ | √ | ||
| Drafting of the article | √ | √ | √ | |||||
| Critical revision of the article for important intellectual content | √ | √ | √ | √ | √ | √ | √ | √ |
| Provision of study materials or patients | √ | √ | √ | |||||
| Statistical expertise | √ | √ | √ | √ | √ | |||
| Obtaining of funding | √ | √ | ||||||
| Administrative, technical, or logistic support | √ | √ | ||||||
| Collection and assembly of data | √ | √ | √ | |||||
| Final approval of the article | √ | √ | √ | √ | √ | √ | √ | √ |
Lisa Sheehy takes responsibility for the integrity of the work as a whole, from inception to finished article. lisasheehy@sympatico.ca.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- 1.Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis and Rheumatism. 2008;58:26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Iorio R, Robb WJ, Healy WL, Berry DJ, Hozack WJ, Kyle RF, et al. Orthopaedic surgeon workforce and volume assessment for total hip and knee replacement in the United States: preparing for an epidemic. Journal of Bone & Joint Surgery American Volume. 2008;90-A:1598–1605. doi: 10.2106/JBJS.H.00067. [DOI] [PubMed] [Google Scholar]
- 3.Brouwer GM, van Tol AW, Bergink AP, Belo JN, Bernsen RM, Reijman M, et al. Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee. Arthritis and Rheumatism. 2007;56:1204–1211. doi: 10.1002/art.22515. [DOI] [PubMed] [Google Scholar]
- 4.Cerejo R, Dunlop DD, Cahue S, Channin D, Song J, Sharma L. The influence of alignment on risk of knee osteoarthritis progression according to baseline stage of disease. Arthritis and Rheumatism. 2002;46:2632–2636. doi: 10.1002/art.10530. [DOI] [PubMed] [Google Scholar]
- 5.Cicuttini F, Wluka A, Hankin J, Wang Y. Longitudinal study of the relationship between knee angle and tibiofemoral cartilage volume in subjects with knee osteoarthritis. Rheumatology. 2004;43:321–324. doi: 10.1093/rheumatology/keh017. [DOI] [PubMed] [Google Scholar]
- 6.Felson DT, Nevitt MC, Yang M, Clancy M, Niu J, Torner JC, et al. A new approach yields high rates of radiographic progression in knee osteoarthritis. Journal of Rheumatology. 2008;35:2047–2054. [PMC free article] [PubMed] [Google Scholar]
- 7.Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286:188–195. doi: 10.1001/jama.286.2.188. [DOI] [PubMed] [Google Scholar]
- 8.Teichtahl AJ, vies-Tuck ML, Wluka AE, Jones G, Cicuttini FM. Change in knee angle influences the rate of medial tibial cartilage volume loss in knee osteoarthritis. Osteoarthritis and Cartilage. 2009;17:8–11. doi: 10.1016/j.joca.2008.05.013. [DOI] [PubMed] [Google Scholar]
- 9.Cooke D, Scudamore A, Li J, Wyss U, Bryant T, Costigan P. Axial lower-limb alignment: comparison of knee geometry in normal volunteers and osteoarthritis patients. Osteoarthritis and Cartilage. 1997;5:39–47. doi: 10.1016/s1063-4584(97)80030-1. [DOI] [PubMed] [Google Scholar]
- 10.Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. Journal of Bone and Joint Surgery American Volume. 1987;69-A:745–749. [PubMed] [Google Scholar]
- 11.Kraus VB, Vail TP, Worrell T, McDaniel G. A comparative assessment of alignment angle of the knee by radiographic and physical examination methods. Arthritis and Rheumatism. 2005;52:1730–1735. doi: 10.1002/art.21100. [DOI] [PubMed] [Google Scholar]
- 12.Issa SN, Dunlop D, Chang A, Song J, Prasad PV, Guermazi A, et al. Full-limb and knee radiography assessments of varus-valgus alignment and their relationship to osteoarthritis disease features by magnetic resonance imaging. Arthritis and Rheumatism. 2007;57:398–406. doi: 10.1002/art.22618. [DOI] [PubMed] [Google Scholar]
- 13.Hinman RS, May RL, Crossley KM. Is there an alternative to the full-leg radiograph for determining knee joint alignment in osteoarthritis? Arthritis and Rheumatism. 2006;55:306–313. doi: 10.1002/art.21836. [DOI] [PubMed] [Google Scholar]
- 14.van Raaij TM, Brouwer RW, Reijman M, Bierma-Zeinstra SM, Verhaar JA. Conventional knee films hamper accurate knee alignment determination in patients with varus osteoarthritis of the knee. The Knee. 2009;16:109–111. doi: 10.1016/j.knee.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 15.Cooke TD. Static knee alignment and its association with radiographic knee osteoarthritis. Osteoarthritis and Cartilage. 2007;15:844–845. doi: 10.1016/j.joca.2007.02.017. [DOI] [PubMed] [Google Scholar]
- 16.Nguyen C, Bryant JT, Cooke TDV, Chow D. Alignment and geometry of the normal knee in stance. Journal of Bone and Joint Surgery British Volume. 1989;71-B:346. [Google Scholar]
- 17.Chang CB, Choi JY, Koh IJ, Seo ES, Seong SC, Kim TK. What should be considered in using standard knee radiographs to estimate mechanical alignment of the knee? Osteoarthritis and Cartilage. 2010;18:530–538. doi: 10.1016/j.joca.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 18.Hsu RW, Himeno S, Coventry MB, Chao EY. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clinal Orthopaedics and Related Research. 1990:215–227. [PubMed] [Google Scholar]
- 19.Cooke TDV, Scudamore RA, Bryant JT, Sorbie C, Siu D, Fisher B. A quantitative approach to radiography of the lower limb. Journal of Bone and Joint Surgery British Volume. 1991;73-B:715–720. doi: 10.1302/0301-620X.73B5.1894656. [DOI] [PubMed] [Google Scholar]
- 20.Sled EA, Cooke D, Sheehy L, Lam M, Costigan P, Nevitt M, et al. Reliability of lower limb frontal plane alignment measures obtained with the use of a computer program and electronic tools. Osteoarthritis and Cartilage. 2007;15:S329. [Google Scholar]
- 21.Felson DT, Cooke TD, Niu J, Goggins J, Choi J, Yu J, et al. Can anatomic alignment measured from a knee radiograph substitute for mechanical alignment from full limb films? Osteoarthritis and Cartilage. 2009;17:1448–1452. doi: 10.1016/j.joca.2009.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cooke TD, Harrison L, Khan B, Scudamore A, Chaudhary MA. Analysis of limb alignment in the pathogenesis of osteoarthritis: a comparison of Saudi Arabian and Canadian cases. Rheumatology International. 2002;22:160–164. doi: 10.1007/s00296-002-0218-7. [DOI] [PubMed] [Google Scholar]
- 23.Cooke TD, Li J, Scudamore RA. Radiographic assessment of bony contributions to knee deformity. The Orthopedic Clinics of North America. 1994;25:387–393. [PubMed] [Google Scholar]
- 24.Yau WP, Chiu KY, Tang WM, Ng TP. Coronal bowing of the femur and tibia in Chinese: its incidence and effects on total knee arthroplasty planning. Journal of Orthopaedic Surgery (Hong Kong) 2007;15:32–36. doi: 10.1177/230949900701500108. [DOI] [PubMed] [Google Scholar]