Abstract
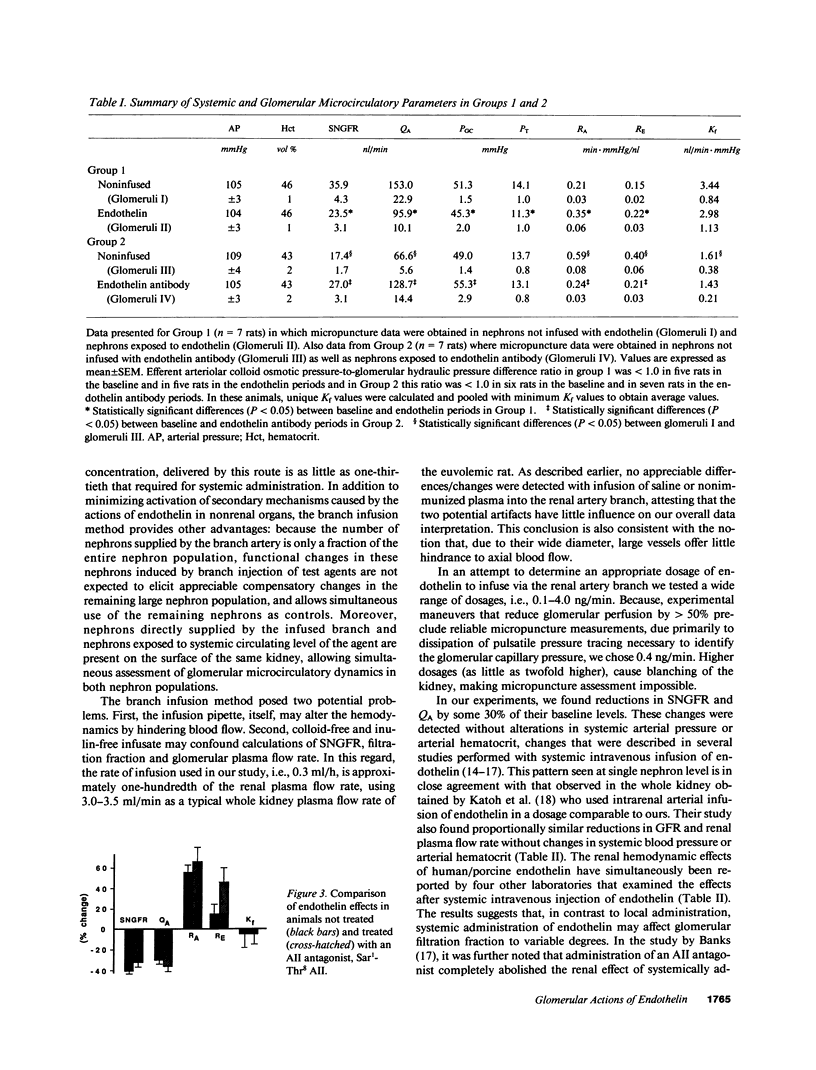
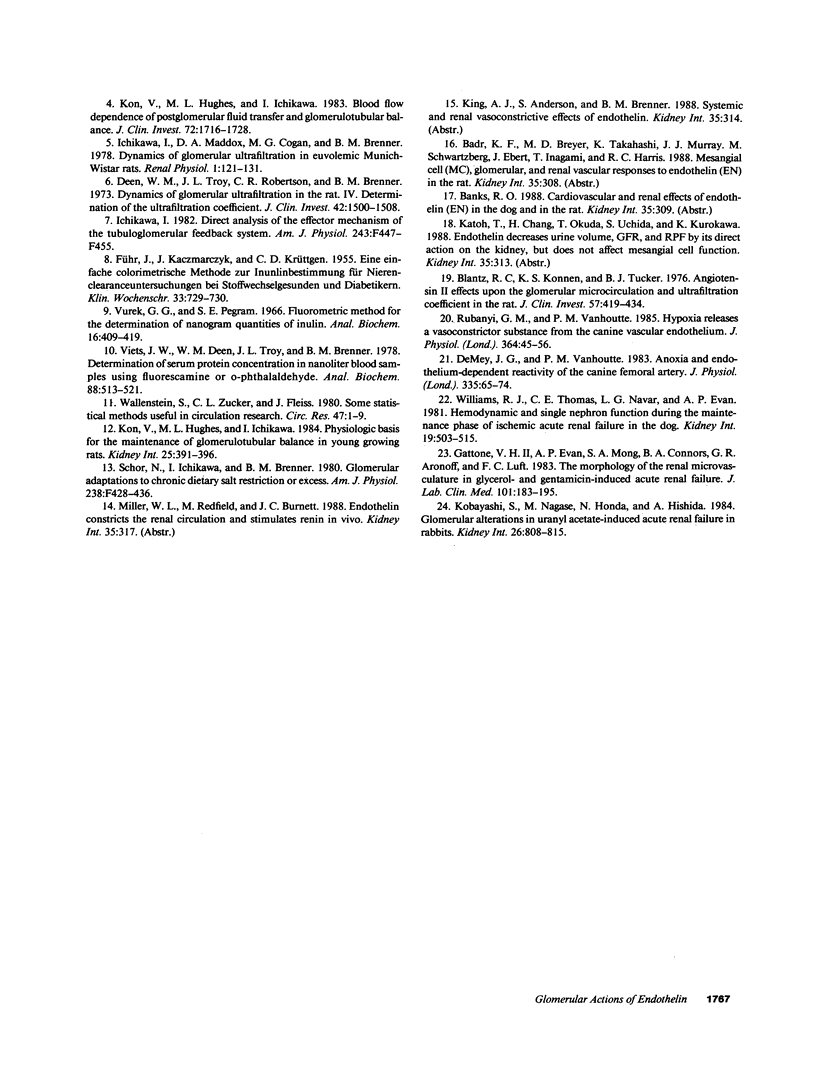
In Munich-Wistar rats, a micropipette was inserted into a first-order branch of the left main renal artery and continuously infused with human/porcine endothelin (0.4 ng/min). Micropuncture measurements revealed substantial differences within the cortical microcirculation of the same left kidney: SNGFR was some 35% lower in glomeruli exposed to endothelin compared with non-endothelin-perfused glomeruli (P less than 0.005). Similarly, glomerular plasma flow rate was some 38% lower in the endothelin-exposed glomeruli (P less than 0.001). The hypoperfusion and hypofiltration in the endothelin-exposed glomeruli reflected an increase in resistances in the afferent and efferent arterioles. There was no difference in the value of the glomerular capillary ultrafiltration coefficient between the two populations of glomeruli. We also studied kidneys that underwent 25 min of renal artery clamping 48 h before study. Antiendothelin antibody infused into one of the branches of the main renal artery ameliorated the vasoconstriction characteristic of postischemic nephrons: within the cortical microcirculation, the SNGFR in glomeruli exposed to antiendothelin antibody was 27.0 +/- 3.1 nl/min as compared with 17.4 +/- 1.7 measured in glomeruli not perfused with the antibody (P less than 0.001). Similarly, glomerular plasma flow rate was higher in the glomeruli exposed to antiendothelin antibody (128.7 +/- 14.4 nl/min vs. 66.6 +/- 5.6, P less than 0.005). Resistances in both the afferent and efferent arterioles were substantially lower in the antibody-exposed glomeruli. It is, therefore, suggested that endothelin, presumably released from damaged endothelium, may play an important intermediary role in the hypoperfusion and hypofiltration observed in postischemic kidneys.
Full text
PDF



Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Blantz R. C., Konnen K. S., Tucker B. J. Angiotensin II effects upon the glomerular microcirculation and ultrafiltration coefficient of the rat. J Clin Invest. 1976 Feb;57(2):419–434. doi: 10.1172/JCI108293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Mey J. G., Vanhoutte P. M. Anoxia and endothelium-dependent reactivity of the canine femoral artery. J Physiol. 1983 Feb;335:65–74. doi: 10.1113/jphysiol.1983.sp014519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deen W. M., Troy J. L., Robertson C. R., Brenner B. M. Dynamics of glomerular ultrafiltration in the rat. IV. Determination of the ultrafiltration coefficient. J Clin Invest. 1973 Jun;52(6):1500–1508. doi: 10.1172/JCI107324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FUHR J., KACZMARCZYK J., KRUTTGEN C. D. Eine einfache colorimetrische Methode zur Inulinbestimmung für Nieren-Clearance-Untersuchungen bei Stoffwechselgesunden und Diabetikern. Klin Wochenschr. 1955 Aug 1;33(29-30):729–730. doi: 10.1007/BF01473295. [DOI] [PubMed] [Google Scholar]
- Gattone V. H., 2nd, Evan A. P., Mong S. A., Connors B. A., Aronoff G. R., Luft F. C. The morphology of the renal microvasculature in glycerol- and gentamicin-induced acute renal failure. J Lab Clin Med. 1983 Feb;101(2):183–195. [PubMed] [Google Scholar]
- Ichikawa I. Direct analysis of the effector mechanism of the tubuloglomerular feedback system. Am J Physiol. 1982 Nov;243(5):F447–F455. doi: 10.1152/ajprenal.1982.243.5.F447. [DOI] [PubMed] [Google Scholar]
- Kobayashi S., Nagase M., Honda N., Hishida A. Glomerular alterations in uranyl acetate-induced acute renal failure in rabbits. Kidney Int. 1984 Dec;26(6):808–815. doi: 10.1038/ki.1984.222. [DOI] [PubMed] [Google Scholar]
- Kon V., Hughes M. L., Ichikawa I. Blood flow dependence of postglomerular fluid transfer and glomerulotubular balance. J Clin Invest. 1983 Nov;72(5):1716–1728. doi: 10.1172/JCI111131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kon V., Hughes M. L., Ichikawa I. Physiologic basis for the maintenance of glomerulotubular balance in young growing rats. Kidney Int. 1984 Feb;25(2):391–396. doi: 10.1038/ki.1984.29. [DOI] [PubMed] [Google Scholar]
- Rubanyi G. M., Vanhoutte P. M. Hypoxia releases a vasoconstrictor substance from the canine vascular endothelium. J Physiol. 1985 Jul;364:45–56. doi: 10.1113/jphysiol.1985.sp015728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schor N., Ichikawa I., Brenner B. M. Glomerular adaptations to chronic dietary salt restriction or excess. Am J Physiol. 1980 May;238(5):F428–F436. doi: 10.1152/ajprenal.1980.238.5.F428. [DOI] [PubMed] [Google Scholar]
- Viets J. W., Deen W. M., Troy J. L., Brenner B. M. Determination of serum protein concentration in nanoliter blood samples using fluorescamine or 9-phthalaldehyde. Anal Biochem. 1978 Aug 1;88(2):513–521. doi: 10.1016/0003-2697(78)90451-7. [DOI] [PubMed] [Google Scholar]
- Wallenstein S., Zucker C. L., Fleiss J. L. Some statistical methods useful in circulation research. Circ Res. 1980 Jul;47(1):1–9. doi: 10.1161/01.res.47.1.1. [DOI] [PubMed] [Google Scholar]
- Williams R. H., Thomas C. E., Navar L. G., Evan A. P. Hemodynamic and single nephron function during the maintenance phase of ischemic acute renal failure in the dog. Kidney Int. 1981 Apr;19(4):503–515. doi: 10.1038/ki.1981.48. [DOI] [PubMed] [Google Scholar]
- Yanagisawa M., Kurihara H., Kimura S., Tomobe Y., Kobayashi M., Mitsui Y., Yazaki Y., Goto K., Masaki T. A novel potent vasoconstrictor peptide produced by vascular endothelial cells. Nature. 1988 Mar 31;332(6163):411–415. doi: 10.1038/332411a0. [DOI] [PubMed] [Google Scholar]



