Abstract
Objectives
To identify variation in patient, event, and scene characteristics of out-of-hospital cardiac arrest (OOHCA) patients assessed by emergency medical services (EMS), and to investigate variation in transport practices in relation to documented prehospital return of spontaneous circulation (ROSC) within eight regional clinical centers participating in the Resuscitation Outcomes Consortium (ROC) Epistry–Cardiac Arrest.
Methods
OOHCA patient, event, and scene characteristics were compared to identify variation in treatment and transport practices across sites. Findings were adjusted for site and standard Utstein covariates. Using logistic regression, these covariates were modeled to identify factors related to the initiation of transport without documented prehospital ROSC as well as survival in these patients. Setting: Eight US and Canadian sites participating in the ROC Epistry–Cardiac Arrest. Population: Persons ≥ 20 years with OOHCA who a) received compressions or shock by EMS providers and/or received bystander AED shock or b) were pulseless but received no EMS compressions or shock between December 2005 and May 2007.
Results
23,233 OOHCA cases were assessed by EMS in the defined period. Resuscitation (treatment) was initiated by EMS in 13,518 cases (58%, site range: 36-69%, p<0.0001). Of treated cases, 59% were transported (site range: 49-88%, p<0.0001). Transport was initiated in the absence of documented ROSC for 58% of transported cases (site range: 14-95%, p<0.0001). Of these transported cases, 8% achieved ROSC before hospital arrival (site range: 5-21%, p<0.0001) and 4% survived to hospital discharge (site range: 1-21%, p<0.0001). In cases with transport from the scene initiated after documented ROSC, 28% survived to hospital discharge (site range: 18-44%, p<0.0001).
Conclusion
Initiation of resuscitation and transport of OOHCA and the reporting of ROSC prior to transport markedly varies among ROC sites. This variation may help clarify reported differences in survival rates among sites and provide a target for identifying EMS practices most likely to enhance survival from OOHCA.
Keywords: Out-of-Hospital Cardiac Arrest, ROSC, Termination of Resuscitation
Introduction
Out-of-hospital cardiac arrest (OOHCA) is a major cause of death in North America.1-4 Witnessed events, bystander initiated cardiopulmonary resuscitation (CPR), presenting rhythm of ventricular fibrillation, arrest location and the prehospital return of spontaneous circulation (ROSC) have all been associated with increased survival.1, 5-18 Assessments of incidence and outcome also indicate community-level variation as a significant factor in EMS treatment and survival from OOHCA.1, 6, 19 Reported survival to hospital discharge ranges from 2-25% in twenty-nine communities, and from 3.0-16.3% of EMS-treated patients in ten ROC communities.1, 6
Understanding regional survival is complicated by definitions used in reporting outcomes.6, 20, 21 Variation may be related to patient, event, system, and therapy factors, including treatment initiation and duration, field termination of resuscitation (TOR) efforts or local regulations guiding transport of non-resuscitated patients to the Emergency Department (ED). EMS strategies for OOHCA treatment and transport differ widely. In some communities, EMS is dispatched for every OOHCA, including those with clear signs of death. Some EMS agencies initiate transport regardless of circulatory status and after little time on scene while others do not initiate transport unless there is ROSC.
The objective of this study was to identify site-level variation in the proportion of OOHCA patients assessed by EMS for whom efforts are initiated, the proportion of patients transported to EDs, and variation in transport practices in relation to ROSC. We also examined predictors of transport in relation to ROSC and survival in the subgroup of patients whose transport was initiated in the absence of ROSC. Differences in treatment and transport practices could account for some of the variation in reported OOHCA survival across ROC sites.1
Methods
Setting and Population
The Resuscitation Outcomes Consortium (ROC) is a network of 9 Regional Clinical Centers consisting of 11 major North American sites investigating OOHCA including US and Canadian communities with geographic dispersion and diversity, serving an estimated 23.7 million population. ROC includes more than 260 EMS agencies including urban and rural, private and municipal agencies.22
The ROC Epistry–Cardiac Arrest is a prospective, multicenter, observational registry that collects uniform data on all EMS-assessed OOHCA across sites allowing a unique opportunity to compare regional variation in treatment and transport practices. The ROC Epistry–Cardiac Arrest was approved by 74 US institutional review boards (IRBs) and 34 Canadian research ethics boards as well as 26 EMS IRBs. 22, 23
Data for all eligible 911-initiated calls attended by participating EMS agencies within defined regions were submitted to the ROC Epistry–Cardiac Arrest database at the centralized ROC Data Coordinating Center (University of Washington, Seattle). Eligible subjects for this analysis included 23,233 adult (≥20 years of age) non-traumatic OOHCA patients whose cardiac arrests were evaluated by EMS agencies between December 1, 2005 and May 31, 2007 in eight ROC sites. Patients experiencing OOHCA as a consequence of blunt, penetrating, or burn trauma were excluded, while drowning and mechanical suffocation etiologies were included.23 Three of 11 ROC sites were excluded due to inability to consistently document the presence or absence of prehospital ROSC.
The eight sites included in this analysis represent 151 EMS agencies and 200 hospitals, and reflect an EMS service population of nearly 16 million.22 They include fire-based as well as private and third party -governmental EMS agencies in systems utilizing varied response schema.
All patients were evaluated by a participating ROC EMS agency and: a) received chest compressions or shock by EMS providers and/or received bystander AED shock (treated group) or b) were pulseless but received no EMS chest compressions or bystander AED shock (untreated group). The untreated group included patients with known DNR orders, those for whom treatment was considered futile (as defined by protocol or law at each site), and those who were obviously dead. Subgroups of the study population included patients transported for ongoing care, and, within this group, those whose transport was initiated without first achieving documented ROSC. Criteria for attempting or terminating resuscitation were not standardized among study sites.
The ROC Epistry–Cardiac Arrest data elements included age and gender of patients, OOHCA location (public or private), witnessed-status, bystander CPR, initial recorded cardiac rhythm, first documented return of spontaneous circulation (ROSC) and response and scene time intervals. The initial cardiac arrest rhythm was obtained from the patient care records or electronic ECG and was defined as the first rhythm obtained within five minutes of pad or electrode placement and before drug administration. ROSC was defined as the first documented return of a palpable pulse, blood pressure, or a perfusing cardiac rhythm. Initiation of transport without documented ROSC was determined by comparing time of first ROSC and time of transport from the scene. Only cases with known vital status at hospital discharge were included in this analysis and only cases with data for each variable were included in logistic regression models.
Analysis
Counts and percentages of patients treated and transported in relation to ROSC, and survival to hospital discharge are reported for each site and overall. Chi-square tests of heterogeneity across the sites are reported. Tests of heterogeneity (adjusted for age, gender, initial rhythm, location, EMS witnessed, bystander CPR, highest level of prehospital care) using logistic regression are also reported. The variables selected are standard Utstein covariates. Patient demographic and call characteristics are summarized using descriptive statistics. Tests for differences in means were conducted using two-sample t-tests allowing for unequal variances. Tests for differences in proportions were conducted using likelihood ratio chi-square tests.
Multivariate logistic regression models, adjusting for site, were fit to investigate the association of arrest characteristics with transport initiation without documented ROSC or field termination of resuscitation (i.e. no transport) of patients treated by EMS as well as survival in the subset of treated patients who were transported without first achieving ROSC. Factors considered for inclusion in the models were pre-determined by the investigators. Only first order terms were included in the logistic regression models. Second order and higher terms and interactions were not considered.
No adjustments were made to p-values for multiple comparisons. The data analysis for this paper was generated using SAS software, copyright, SAS Institute Inc. SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc., Cary, NC, USA.
Results
Aggregate findings are summarized in Figure 1. Resuscitation by EMS was attempted for 13,518 patients (58%), with 7,945 of these patients (59%) transported. A total of 1,124 transported patients survived to hospital discharge (8.3% of patients for whom resuscitation was attempted). We investigated subgroups of those transported after documented field ROSC (42% of all treated patients) and those for whom transport was initiated without documented prehospital ROSC (58% of all treated patients) and found that survival to hospital discharge was significantly different with 28% of patients transported after ROSC surviving to hospital discharge, compared to 4% of patients surviving in the subgroup for whom transport was initiated without documented ROSC.
Figure 1.
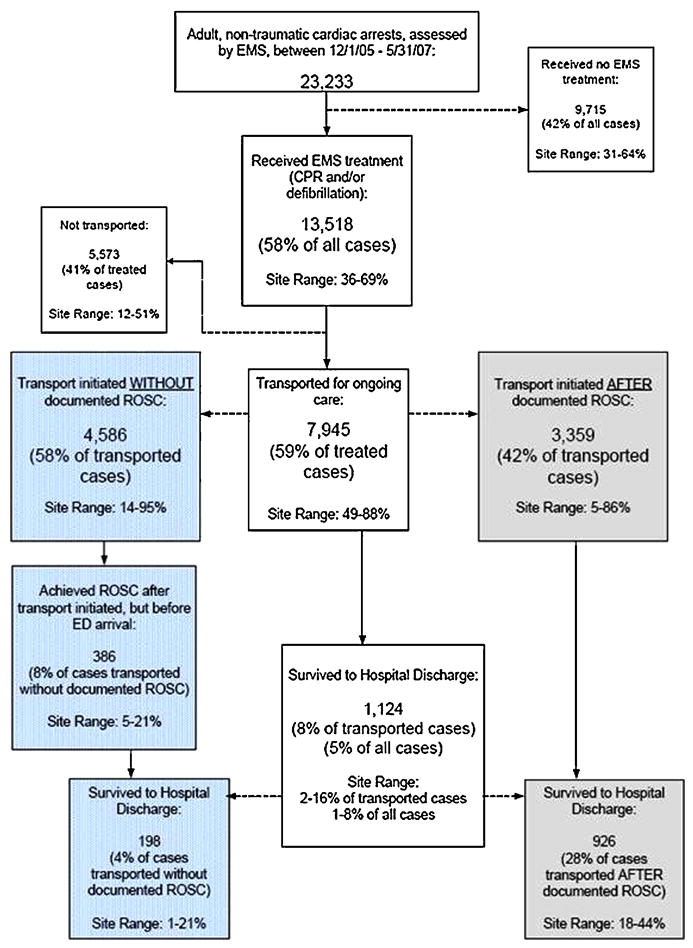
Overall and Site-level OOHCA Treatment, Transport, and Survival Summary
While the majority of patients encountered across all sites were treated by EMS, site values range from 36-69%. Significant site-level variation (Table 1) was also identified in the proportion of treated patients who were transported (site range: 49-88%), and survival to hospital discharge for both EMS-assessed (site range: 0.7-8.3%) and EMS-treated (site range: 1.9-16.0%) patients.
Table 1.
Site variation in treatment, transport, and survival of OOHCA to hospital discharge in relation to documented prehospital ROSC
| Site | A: Adult Non-Traumatic OOHCA Assessed by EMS | B: Treated by EMS | C: Transported for ongoing care | D. Survival to Hospital Discharge (all cases) | E: Survival to Hospital Discharge (treated cases only) | F: Transport Initiated AFTER Documented ROSC | G: Transport Initiated AFTER Documented ROSC and Survived | H: Transport Initiated WITHOUT Documented ROSC | I: Transport Initiated WITHOUT Documented ROSC and Survived |
|---|---|---|---|---|---|---|---|---|---|
| N | N (% of A) | N (% of B) | N (% of A) | N (% of B) | N (% of B) | N (% of F) | N (% of B) | N (% of H) | |
| Alabama | 1024 | 373 (36) | 328 (88) | 7 (0.7) | 7 (1.9) | 17 (5) | 3 (18) | 311 (95) | 4 (1) |
| Iowa | 1419 | 764 (54) | 656 (86) | 76 (5.4) | 76 (10.0) | 120 (18) | 53 (44) | 536 (82) | 23 (4) |
| Ottawa-OPALS Group, Ontario, Canada | 4397 | 2796 (64) | 1732 (62) | 148 (3.4) | 148 (5.3) | 520 (30) | 110 (21) | 1212 (70) | 38 (3) |
| Pittsburgh, Pennsylvania | 1634 | 770 (47) | 543 (71) | 61 (3.7) | 61 (7.9) | 146 (27) | 47 (32) | 397 (73) | 14 (4) |
| Portland, Oregon | 1999 | 1198 (60) | 691 (58) | 138 (6.9) | 138 (11.5) | 407 (59) | 120 (29) | 284 (41) | 18 (6) |
| Seattle/King County, Washington | 3304 | 1716 (52) | 840 (49) | 275 (8.3) | 275 (16.0) | 722 (86) | 250 (35) | 118 (14) | 25 (21) |
| Toronto, Ontario, Canada | 6154 | 3631 (59) | 1960 (54) | 202 (3.3) | 202 (5.6) | 647 (33) | 154 (24) | 1313 (67) | 48 (4) |
| Vancouver, British Columbia, Canada | 3302 | 2270 (69) | 1195 (53) | 217 (6.6) | 217 (9.6) | 780 (65) | 189 (24) | 415 (35) | 28 (7) |
| Overall (All Sites) | 23233 | 13518 (58) | 7945 (59) | 1124 (4.8) | 1124 (8.3) | 3359 (42) | 926 (28) | 4586 (58) | 198 (4) |
| Adjusted p-value* | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
Adjusted for covariates: age, gender, initial rhythm, location, EMS witnessed, bystander CPR, ALS care
Across all sites, the majority (58%, site range: 14-95%) of transported patients had transport initiated without documented ROSC (Table 1). Of those transported without documented ROSC, 4% survived to hospital discharge across all sites (site range of 1-21%), as compared to 28% of those transported after ROSC (site range: 18-44%).
Initial cardiac arrest rhythms for the two transport subgroups (transported after ROSC and transported without ROSC) and survivors from each site each are described in Table 2. Patients with initial rhythms of ventricular fibrillation (VF), pulseless ventricular tachycardia (pVT), or AED-shock were the largest group of those transported after ROSC (40.1% overall, site range: 30.1-46.4%) while this group made up 27.4% of those transported without documented ROSC (site range: 19.9-51.1%). Of those transported after ROSC, almost half (45.5%) of all patients with initial rhythms of VF/pVT/AED shock survived (site range: 25.0-62.2%). However, amongst all patients transported in the absence of ROSC, only 9.1% of those with these rhythms survived to hospital discharge (site range: 3.6-33.3%).
Table 2.
Initial cardiac arrest rhythms of both transport groups and survivors, by site
| Group | Rhythm | Alabama | Iowa | Ottawa - OPALS Group, Ontario, Canada | Pittsburgh, Pennsylvania | Portland, Oregon | Seattle/King County, Washington | Toronto, Ontario, Canada | Vancouver, British Columbia, Canada | All Sites |
|---|---|---|---|---|---|---|---|---|---|---|
| Transport Initiated AFTER ROSC N=3359 (Survior n=926) | VF/VT/AED Shock: N (%) | 8 (47.0) | 50 (41.7) | 207 (39.8) | 45 (30.1) | 168 (41.3) | 283 (39.2) | 225 (34.8) | 362 (46.4) | 1348 (40.1) |
| Survived to discharge: n (%) | 2 (25.0) | 29 (58.0) | 69 (33.3) | 28 (62.2) | 84 (50.0) | 153 (54.1) | 97 (43.1) | 152 (42.0) | 614 (45.5) | |
| PEA: N (%) | 6 (35.3) | 17 (14.2) | 115 (22.1) | 41 (28.0) | 117 (28.8) | 246 (34.0) | 137 (21.2) | 150 (19.2) | 829 (24.7) | |
| Survived to discharge: n (%) | -- | 3 (17.6) | 15 (13.0) | 7 (17.1) | 23 (19.7) | 63 (25.6) | 19 (13.9) | 13 (8.7) | 143 (17.2) | |
| Asystole: N (%) | 1 (5.9) | 32 (26.7) | 99 (19.0) | 31 (21.2) | 108 (26.5) | 139 (19.3) | 186 (28.8) | 166 (21.3) | 762 (22.7) | |
| Survived to discharge: n (%) | -- | 7 (21.9) | 5 (5.1) | 0 (0) | 7 (6.5) | 10 (7.2) | 13 (7.0) | 5 (3.0) | 47 (6.2) | |
| AED No Shock: N (%) | 1 (5.9) | 6 (5.0) | 50 (9.6) | 4 (2.7) | 2 (0.5) | 15 (2.1) | 71 (11.0) | 74 (9.5) | 223 (6.6) | |
| Survived to discharge: n (%) | 1 (100) | 2 (33.3) | 4 (8.0) | 2 (50.0) | 1 (50.0) | 5 (13.3) | 11 (15.5) | 5 (6.8) | 31 (13.9) | |
| Cannot Determine/Missing: N (%) | 1 (5.9) | 15 (12.5) | 49 (9.4) | 25 (17.1) | 12 (2.9) | 39 (5.4) | 28 (4.3) | 28 (3.6) | 197 (5.9) | |
| Survived to discharge: n (%) | -- | 12 (80.0) | 17 (34.7) | 10 (40.0) | 5 (41.7) | 19 (48.7) | 14 (50.0) | 14 (50.0) | 91 (46.2) | |
| Transport Initiated without ROSC N=4586 (Survivor n=198) | VF/VT/AED Shock: N (%) | 84 (27.1) | 138 (25.8) | 324 (26.7) | 79 (19.9) | 145 (51.1) | 45 (38.1) | 332 (25.3) | 109 (26.3) | 1256 (27.4) |
| Survived to discharge: n (%) | 3 (3.6) | 17 (12.3) | 19 (5.9) | 6 (7.6) | 12 (8.3) | 15 (33.3) | 27 (8.1) | 15 (13.8) | 114 (9.1) | |
| PEA: N (%) | 97 (31.2) | 128 (23.9) | 259 (21.4) | 91 (22.9) | 70 (24.7) | 43 (36.4) | 228 (17.4) | 105 (25.3) | 1021 (22.3) | |
| Survived to discharge: n (%) | -- | 2 (1.6) | 5 (1.9) | 3 (3.3) | 3 (4.3) | 4 (9.3) | 3 (1.3) | 3 (2.9) | 23 (2.3) | |
| Asystole: N (%) | 90 (28.9) | 212 (39.6) | 408 (33.7) | 173 (43.6) | 60 (21.1) | 19 (16.1) | 303 (23.1) | 132 (31.8) | 1397 (30.5) | |
| Survived to discharge: n (%) | 1 (1.1) | 2 (0.9) | 4 (1.0) | 2 (1.1) | 2 (3.3) | 1 (5.3) | 3 (1.0) | 1 (0.8) | 16 (1.1) | |
| AED No Shock: N (%) | 15 (4.8) | 18 (3.4) | 113 (9.3) | 6 (1.5) | -- | 4 (3.4) | 400 (30.5) | 47 (11.3) | 603 (13.2) | |
| Survived to discharge: n (%) | -- | -- | -- | 1 (16.7) | -- | 1 (25.0) | 8 (2.0) | 2 (4.3) | 12 (2.0) | |
| Cannot Determine/Missing: N (%) | 25 (8.0) | 40 (7.5) | 108 (8.9) | 48 (12.1) | 9 (3.2) | 7 (5.9) | 50 (3.8) | 22 (5.3) | 309 (6.7) | |
| Survived to discharge: n (%) | -- | 2 (5.0) | 10 (9.3) | 2 (4.2) | 1 (11.1) | 4 (57.1) | 7 (14.0) | 7 (31.8) | 33 (10.7) | |
Using multivariate logistic regression, we examined the characteristics of who were either transported without documented ROSC or not transported to determine predictors of transport initiation in the absence of ROSC (Figure 2, Model 1). Those transported without documented ROSC were also studied to determine predictors of survival (Figure 2, Model 2). Included in the models were patient (gender, age), scene (location), and event (bystander CPR, EMS-witnessed arrest, highest level of prehospital care, initial rhythm) characteristics.
Figure 2.
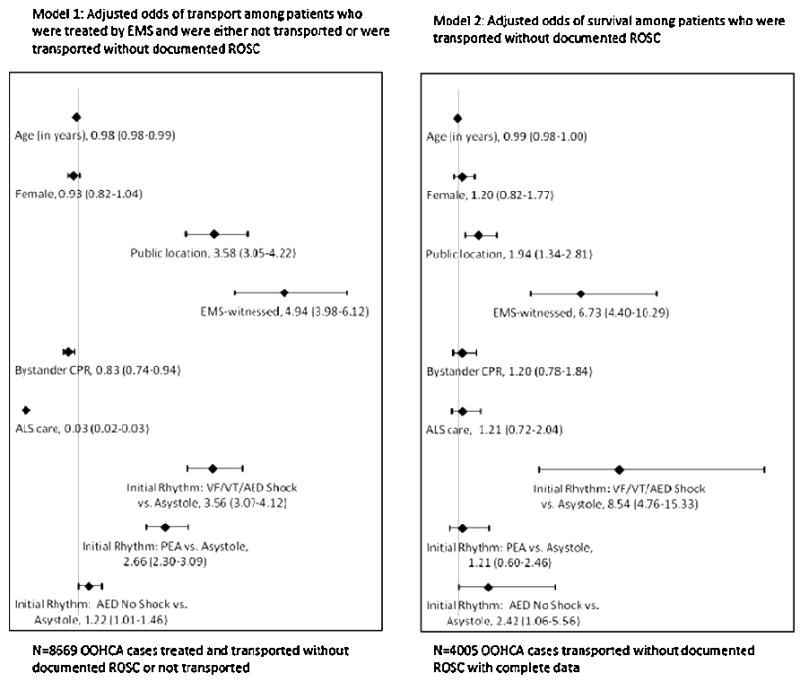
Adjusted odds of transport among patients who were either not transported or were transported without documented ROSC (Model 1) and adjusted odds of survival among patients who were transported without documented ROSC (Model 2)
Adjusting for site, Model 1 indicates that EMS-witnessed OOHCA, an arrest in a public location, and a “shockable” initial cardiac arrest rhythm (VF/pVT/AED-shock) were most positively associated with transport initiation without documented ROSC versus no transport. The odds of being transported without first achieving documented ROSC was much lower if ALS was highest care on scene versus BLS most likely due to the lack of authority of almost all BLS to pronounce deaths in the field. Site-level characteristics of the patients included in this model are in Table 3.
Table 3.
Patient, Scene, and Event Characteristics of OOHCA cases with transport initiated without documented ROSC or not transported, by site
| Site | Age | Sex | Location | Bystander CPR | Response Time | EMS-Witnessed | Highest Level of Care | Initial Cardiac Arrest Rhythm | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Median Age in years | % Female | % in public location | % with Bystander CPR | Median (minutes) | % EMS-witnessed | % ALS | % VF/V T or AED - Shock | % Asystole | % PEA | % AED - No Shock, No Strip | % Cannot Determine or Missing | |
| Alabama | 68 | 44.7 | 13.6 | 42.7 | 6.0 | 20.6 | 100 | 22.6 | 36.7 | 31.2 | 3.5 | 6.0 |
| Iowa | 66 | 35.8 | 19.3 | 34.4 | 4.0 | 15.4 | 99.2 | 25.9 | 44.0 | 22.8 | 3.3 | 3.9 |
| Ottawa-OPALS Group, Ontario, Canada | 70 | 33.9 | 12.7 | 26.6 | 5.5 | 9.1 | 90.0 | 22.4 | 43.0 | 19.6 | 12.7 | 1.7 |
| Pittsburgh, Pennsylvania | 66 | 38.0 | 13.5 | 40.0 | 5.2 | 8.6 | 99.8 | 17.9 | 54.8 | 22.3 | 3.1 | 2.0 |
| Portland, Oregon | 64 | 35.7 | 16.6 | 60.7 | 4.7 | 4.0 | 100 | 29.4 | 51.4 | 17.9 | 0.0 | 1.3 |
| Seattle/King County, Washington | 64 | 36.0 | 13.6 | 48.9 | 5.0 | 9.0 | 98.5 | 17.2 | 54.2 | 23.9 | 2.9 | 1.9 |
| Toronto, Ontario, Canada | 71 | 36.6 | 14.8 | 26.4 | 6.0 | 8.5 | 82.1 | 18.2 | 43.4 | 15.9 | 22.0 | 0.6 |
| Vancouver, British Columbia, Canada | 68 | 30.3 | 15.0 | 36.4 | 6.5 | 8.4 | 79.7 | 19.0 | 43.7 | 18.4 | 17.7 | 1.1 |
| All Sites | 69 | 35.1 | 14.5 | 34.0 | 5.6 | 9.1 | 88.6 | 20.4 | 45.6 | 19.1 | 13.4 | 1.5 |
| p value | <.0001 | 0.0002 | 0.014 | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 |
Model 2 identifies positive associations with survival to hospital discharge after initiation of transport without ROSC for initial rhythms of VF/pVT/AED-shock and EMS-witnessed OOHCA. Site-level characteristics of this group are summarized in Table 4, including time spent on scene with these patients. The median scene time interval was 21.5 minutes for patients transported in the absence of documented ROSC (site range: 15.0-33.8 minutes).
Table 4.
Patient, Scene, and Event Characteristics of OOHCA cases with transport initiated without documented ROSC, by site
| % Female | Median Age (years) | Median Response Time (minutes) | Median Scene Time (minutes) | % in Public Location | % with Bystander CPR | % EMS-witnessed | % ALS on scene | % with ROSC After Transport Initiated | |
|---|---|---|---|---|---|---|---|---|---|
| Alabama | 43.4 | 65 | 6.0 | 15.0 | 13.5 | 24.8 | 13.8 | 99.7 | 4.8 |
| Iowa | 36.6 | 65 | 4.0 | 19.8 | 19.2 | 30.2 | 14.7 | 99.3 | 14.0 |
| Ottawa-OPALS Group, Ontario, Canada | 31.6 | 67 | 5.4 | 23.2 | 19.1 | 26.7 | 13.3 | 82.4 | 5.9 |
| Pittsburgh, Pennsylvania | 34.0 | 66 | 6.0 | 24.0 | 20.9 | 38.0 | 8.6 | 99.8 | 9.1 |
| Portland, Oregon | 25.7 | 60 | 4.7 | 25.1 | 27.8 | 43.3 | 8.8 | 100. 0 | 13.4 |
| Seattle/King County, Washington | 28.8 | 59 | 4.9 | 33.8 | 31.4 | 37.3 | 33.1 | 97.5 | 21.2 |
| Toronto, Ontario, Canada | 31.7 | 67 | 6.1 | 20.0 | 25.1 | 24.5 | 14.8 | 62.8 | 6.2 |
| Vancouver, British Columbia, Canada | 27.2 | 65 | 6.8 | 19.2 | 24.8 | 34.0 | 18.6 | 37.8 | 10.8 |
| All Sites | 32.4 | 66 | 5.7 | 21.5 | 22.0 | 29.3 | 14.2 | 78.9 | 8.4 |
| p value | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 |
Discussion
The use of standardized data collection (a single web-based data entry platform used by all sites) and definitions within the ROC Epistry–Cardiac Arrest allows consistent definition of data content and denominators for survival calculations across sites as opposed to chart review or other disparate data collection approaches. The need for consistent denominators in survival calculations has been previously noted, with Eisenberg, et al., calling for “national and international agreement about definitions of denominators for valid cross community comparisons.”20 Due to the standardization employed in this dataset, we were able to identify and describe variation in the initiation of resuscitation for OOHCA, decision to transport in the absence of ROSC, and survival across the eight ROC sites.
Site-level variation was identified in OOHCA practices of resuscitation initiation, transport, and transport in relation to documented ROSC. Understanding regional variation in the care and outcome of OOHCA can help identify both optimal resuscitation strategies and system-specific characteristics to improve survival while cost-effectively utilizing limited resources. Evaluating system practices and survival can also help in determining best practices for when to both withhold resuscitation and terminate resuscitation efforts prior to transport.
Variation in initiation of resuscitation
It is important to quantify those who are dead and not treated by EMS to better understand the true impact of cardiac arrest on communities and EMS systems. There is a paucity of data outside ROC examining initiation of EMS treatment in OOHCA. In 2008, Nichol et al reported that resuscitation efforts were initiated for 58% of EMS-assessed patients in ten ROC communities, while resuscitation was not attempted for the remaining 42 percent.1 In this analysis, we also noted initiation of resuscitation in 58% of EMS-assessed patients, varying from a high of 69% in Vancouver, Canada to a low of 36% in Alabama. This variation could not be explained by differences in the standard Utstein covariates such as location, witnessed status, initial rhythm, and highest level of care (ALS vs. BLS). Other factors such as local protocols and regulations regarding the criteria for starting resuscitation likely play a role and merit further study.
Variation in transport and survival
A National Association of EMS Physicians position statement recommends that termination of resuscitation (TOR) be considered for adult non-traumatic OOHCA patients who have received CPR, airway management, intravenous access and at least 20 minutes of resuscitative efforts who remain in asystole or pulseless electrical activity without ROSC.24 There is evidence that paramedics and families are accepting of field TOR.25-27 Previously published ALS and BLS TOR rules have recently been validated with 98.7% and 99.4% specificity respectively.7, 9, 24, 28-36 Emergent transports also generate a demonstrated risk to public and EMS safety with potential ambulance crashes.37 Despite the availability of validated TOR rules, and known potential risk from crashes, we observed that sites reported initiation of transport from the scene for the majority of EMS-treated OOHCA patients, and in most instances transport was initiated without first achieving documented ROSC. These findings are similar to a recent study in which more than half (56%) of OOHCA patients meeting TOR criteria were transported.38 However, transporting a larger proportion of patients does not appear to yield increased survival. In fact, the site reporting the highest proportion of survivors among both EMS-treated patients and the subgroup of patients transported in the absence of documented ROSC (Seattle/King County, WA) also reports the lowest proportion of transported patients (49%) and the lowest proportion of patients transported in the absence of ROSC (14%). Conversely, the Alabama site reports the highest proportion of both overall transport (88%) and transport in the absence of ROSC (95%), with the lowest proportion of survivors in both groups (1.9% and 1.0%, respectively).
Identification of patients likely to survive may help guide transport decisions, especially in the absence of ROSC. The models presented (Figure 2) indicate that patients with initial rhythms of VF/pVT/AED-shock are more likely to be both transported in the absence of ROSC (OR: 3.56) as well as to survive to discharge (OR: 8.54). As expected, patients with these shockable initial rhythms made up a larger proportion of survivors in both groups (Table 2). However, a larger proportion of patients who were initially asystolic were transported in the absence of ROSC (30.1% overall) than those with a shockable initial rhythm (27.4% overall). The site initiating transport without ROSC for the smallest proportion of initially asystolic patients (Seattle/King County, WA, 16.1%) reports the largest proportion of patients whose transport was initiated without ROSC to survive to discharge.
While two recent reports found that transport time was not related to OOHCA survival, little data has been reported regarding scene time (defined as the interval between first EMS unit arrival and either termination of resuscitation or transport initiation) and survival.39, 40 Across sites, the median scene time interval was 21.5 minutes for patients transported in the absence of ROSC , but the site reporting the longest median scene time (33.8 minutes) (Seattle/King County, WA) reported the highest survival, while the site that reported the least scene time (Alabama, median 15.0 minutes) reported the lowest proportion of survival in this subgroup. This variation suggests that longer scene times prior to transport may be an effective strategy for OOHCA.
Our findings, along with others, suggest inconsistency in the initiation and duration of treatment, the determination of which patients to transport, and, potentially, in the application of protocols regarding TOR among ROC sites. It is important to note that site-specific protocols were not available for this analysis. This inconsistency across EMS systems can affect survival calculations.41 If all EMS-assessed patients are used as a denominator for reporting survival, systems that initiate treatment for the majority of patients will have lower reported survival than those initiating fewer OOHCA resuscitations. Many ROC sites report transporting the majority of patients for whom resuscitation is initiated whereas others appear more selective. Sites transporting fewer patients, especially fewer patients for whom transport is initiated without documented ROSC, as well as sites spending more time on scene prior to determining transport appear to yield higher proportions of survival to hospital discharge in both EMS-treated and transported OOHCA patients.
Further Directions
Better knowledge of protocols guiding EMS initiation, timing, and termination of resuscitation, along with transport practices, both overall and in relation to documented ROSC, is critical for understanding OOHCA survival. Systematic research is needed to compare these protocols and practices with a better understanding of ROSC documentation in the prehospital setting to identify patients who are most likely to achieve ROSC either on scene or en route to continued care, and ultimately survive. It is also important to further study the relationship between treatment time on scene, prehospital ROSC, the decision to transport, and overall OOHCA survival. Understanding the barriers to consistent implementation of treatment protocols and termination of resuscitation rules is a critical area for further research. Finally, we need to explore the impact of ALS and BLS composition of systems on resuscitation protocols and practices.
Limitations
ROC Epistry–Cardiac Arrest records the first out-of-hospital ROSC of any duration, and is unable to distinguish sustained from intermittent ROSC. Timing of ROSC and transport were determined using reported time of first documented ROSC and recorded time of transport from the scene. To be included in this analysis, all cases were required to have the time of transport recorded. Those cases with no time of first ROSC were considered to have no documented ROSC. Only the initial cardiac arrest rhythm is known, not subsequent rhythms before transport initiation or TOR. Survival is defined only as discharge from hospital, with no measure of neurologic function. Only cases with known hospital outcome were included in this analysis, thus excluding 120 cases overall. Patients for whom EMS was summoned before a cardiac arrest occurred (EMS-witnessed) included in this analysis may not have gone into cardiac arrest until after transport was initiated, which could falsely increase the proportion of patients transported without documented ROSC. There are also potential interactions among all covariates analyzed that could impact the adjusted odds of transport and survival in patients without documented ROSC. Finally, EMS OOHCA protocols across ROC agencies are not standardized, nor were they available for review.
Conclusions
There is marked site variation in the initiation of resuscitation of OOHCA by EMS, which could affect the overall reported survival rates in communities. Similarly, the proportion and type of patients transported without ROSC varies widely. Finally, the site-level variation in survival following transport initiation without documented ROSC is also significant. There is a critical need for further investigation of this variation for the interpretation of reported OOHCA resuscitation and transport practices as both EMS and communities work towards improving survival from out-of-hospital cardiac arrest.
Acknowledgments
Funding Sources: The ROC is supported by a series of cooperative agreements to 10 regional clinical centers and one Data Coordinating Center (5U01HL077863, HL077881, HL077871 HL077872, HL077866, HL077908, HL077867, HL077885, HL077887, HL077873, HL077865) from the National Heart, Lung and Blood Institute in partnership with the National Institute of Neurological Disorders and Stroke, U.S. Army Medical Research & Material Command, The Canadian Institutes of Health Research (CIHR) - Institute of Circulatory and Respiratory Health, Defence Research and Development Canada, the American Heart Association and the Heart and Stroke Foundation of Canada.
Footnotes
Conflict of Interest Statement: No authors had potential conflicts of interest relevant to the subject matter of this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Nichol G, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300(12):1423–31. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rea TD, et al. Incidence of out-of-hospital cardiac arrest. American Journal of Cardiology. 2004;93(12):1455–60. doi: 10.1016/j.amjcard.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 3.Rea TD, et al. Incidence of EMS-treated out-of-hospital cardiac arrest in the United States. Resuscitation. 2004;63(1):17–24. doi: 10.1016/j.resuscitation.2004.03.025. [DOI] [PubMed] [Google Scholar]
- 4.Nichol G, et al. Effectiveness of emergency medical services for victims of out-of-hospital cardiac arrest: a metaanalysis. Annals of Emergency Medicine. 1996;27(6):700–10. doi: 10.1016/s0196-0644(96)70187-7. [DOI] [PubMed] [Google Scholar]
- 5.Handel DA, et al. Prehospital cardiac arrest in a paramedic first-responder system using the Utstein style. Prehospital Emergency Care. 2005;9(4):398–404. doi: 10.1080/10903120500255867. [DOI] [PubMed] [Google Scholar]
- 6.Eisenberg MS, et al. Cardiac arrest and resuscitation: a tale of 29 cities. Annals of Emergency Medicine. 1990;19(2):179–86. doi: 10.1016/s0196-0644(05)81805-0. [DOI] [PubMed] [Google Scholar]
- 7.Grudzen C. Out-of-hospital resuscitation: have we gone too far? Prehospital & Disaster Medicine. 2006;21(6):445–50. doi: 10.1017/s1049023x00004180. [DOI] [PubMed] [Google Scholar]
- 8.Liu JM, et al. Hospital variability of out-of-hospital cardiac arrest survival. Prehospital Emergency Care. 2008;12(3):339–46. doi: 10.1080/10903120802101330. [DOI] [PubMed] [Google Scholar]
- 9.Sasson C, et al. Prehospital termination of resuscitation in cases of refractory out-of-hospital cardiac arrest. JAMA. 2008;300(12):1432–8. doi: 10.1001/jama.300.12.1432. [DOI] [PubMed] [Google Scholar]
- 10.Spaite DW, et al. Prehospital cardiac arrest: the impact of witnessed collapse and bystander CPR in a metropolitan EMS system with short response times. Annals of Emergency Medicine. 1990;19(11):1264–9. doi: 10.1016/s0196-0644(05)82285-1. [DOI] [PubMed] [Google Scholar]
- 11.Stiell IG, et al. Modifiable factors associated with improved cardiac arrest survival in a multicenter basic life support/defibrillation system: OPALS Study Phase I results. Ontario Prehospital Advanced Life Support. Annals of Emergency Medicine. 1999;33(1):44–50. doi: 10.1016/s0196-0644(99)70415-4. [DOI] [PubMed] [Google Scholar]
- 12.Stueven HA, et al. Prehospital cardiac arrest--a critical analysis of factors affecting survival. Resuscitation. 1989;17(3):251–9. doi: 10.1016/0300-9572(89)90041-5. [DOI] [PubMed] [Google Scholar]
- 13.Vukmir RB. Survival from prehospital cardiac arrest is critically dependent upon response time. Resuscitation. 2006;69(2):229–34. doi: 10.1016/j.resuscitation.2005.08.014. [DOI] [PubMed] [Google Scholar]
- 14.Vukmir RB G. Sodium Bicarbonate Study. Witnessed arrest, but not delayed bystander cardiopulmonary resuscitation improves prehospital cardiac arrest survival. Emergency Medicine Journal. 2004;21(3):370–3. doi: 10.1136/emj.2003.008383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Layon AJ, et al. Utstein style analysis of rural out-of-hospital cardiac arrest OOHCA: total cardiopulmonary resuscitation (CPR) time inversely correlates with hospital discharge rate. Resuscitation. 2003;56(1):59–66. doi: 10.1016/s0300-9572(02)00273-3. [DOI] [PubMed] [Google Scholar]
- 16.Larsen MP, et al. Predicting survival from out-of-hospital cardiac arrest: a graphic model. Annals of Emergency Medicine. 1993;22(11):1652–8. doi: 10.1016/s0196-0644(05)81302-2. [DOI] [PubMed] [Google Scholar]
- 17.Kass LE, et al. One-year survival after prehospital cardiac arrest: the Utstein style applied to a rural-suburban system. American Journal of Emergency Medicine. 1994;12(1):17–20. doi: 10.1016/0735-6757(94)90190-2. [DOI] [PubMed] [Google Scholar]
- 18.Hallstrom AP, Cobb LA, Yu BH. Influence of comorbidity on the outcome of patients treated for out-of-hospital ventricular fibrillation. Circulation. 1996;93(11):2019–22. doi: 10.1161/01.cir.93.11.2019. [DOI] [PubMed] [Google Scholar]
- 19.Sanders AB, Kern KB. Surviving cardiac arrest: location, location, location.comment. JAMA. 2008;300(12):1462–3. doi: 10.1001/jama.300.12.1462. [DOI] [PubMed] [Google Scholar]
- 20.Eisenberg MS, Cummins RO, Larsen MP. Numerators, denominators, and survival rates: reporting survival from out-of-hospital cardiac arrest. American Journal of Emergency Medicine. 1991;9(6):544–6. doi: 10.1016/0735-6757(91)90108-v. [DOI] [PubMed] [Google Scholar]
- 21.Sayre MR, et al. Measuring survival rates from sudden cardiac arrest: the elusive definition. Resuscitation. 2004;62(1):25–34. doi: 10.1016/j.resuscitation.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 22.Davis DP, et al. A descriptive analysis of Emergency Medical Service Systems participating in the Resuscitation Outcomes Consortium (ROC) network. Prehospital Emergency Care. 2007;11(4):369–82. doi: 10.1080/10903120701537147. [DOI] [PubMed] [Google Scholar]
- 23.Morrison LJ, et al. Rationale, development and implementation of the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Resuscitation. 2008;78(2):161–9. doi: 10.1016/j.resuscitation.2008.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bailey ED, Wydro GC, Cone DC. Termination of resuscitation in the prehospital setting for adult patients suffering nontraumatic cardiac arrest. National Association of EMS Physicians Standards and Clinical Practice Committee. Prehospital Emergency Care. 2000;4(2):190–5. doi: 10.1080/10903120090941498. [DOI] [PubMed] [Google Scholar]
- 25.Delbridge TR, et al. Field termination of unsuccessful out-of-hospital cardiac arrest resuscitation: acceptance by family members. Annals of Emergency Medicine. 1996;27(5):649–54. doi: 10.1016/s0196-0644(96)70170-1. [DOI] [PubMed] [Google Scholar]
- 26.Schmidt TA, Harrahill MA. Family response to out-of-hospital death. Academic Emergency Medicine. 1995;2(6):513–8. doi: 10.1111/j.1553-2712.1995.tb03250.x. [DOI] [PubMed] [Google Scholar]
- 27.Marco CA, Schears RM. Prehospital resuscitation practices: a survey of prehospital providers. Journal of Emergency Medicine. 2003;24(1):101–6. doi: 10.1016/s0736-4679(02)00688-1. [DOI] [PubMed] [Google Scholar]
- 28.Morrison LJ, et al. Derivation and evaluation of a termination of resuscitation clinical prediction rule for advanced life support providers. Resuscitation. 2007;74(2):266–75. doi: 10.1016/j.resuscitation.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 29.Grudzen CR, L R, Hoffman JR, Koenig W, Lorenz KA, Asch SM. Developing quality indicators for the appropriateness of resuscitation in prehospital atraumatic cardiac arrest. Prehospital Emergency Care. 2007;11(4):434–442. doi: 10.1080/10903120701536925. [DOI] [PubMed] [Google Scholar]
- 30.Morrison LJ, et al. Validation of a rule for termination of resuscitation in out-of-hospital cardiac arrest. New England Journal of Medicine. 2006;355(5):478–87. doi: 10.1056/NEJMoa052620. [DOI] [PubMed] [Google Scholar]
- 31.Verbeek PR, et al. Derivation of a termination-of-resuscitation guideline for emergency medical technicians using automated external defibrillators. Academic Emergency Medicine. 2002;9(7):671–8. doi: 10.1111/j.1553-2712.2002.tb02144.x. [DOI] [PubMed] [Google Scholar]
- 32.Larkin GL. Termination of resuscitation: the art of clinical decision making. Current Opinion in Critical Care. 2002;8(3):224–9. doi: 10.1097/00075198-200206000-00005. [DOI] [PubMed] [Google Scholar]
- 33.Bonnin MJ, et al. Distinct criteria for termination of resuscitation in the out-of-hospital setting. JAMA. 1993;270(12):1457–62. [PubMed] [Google Scholar]
- 34.Feder S, et al. Withholding resuscitation: a new approach to prehospital end-of-life decisions. Annals of Internal Medicine. 2006;144(9):634–40. doi: 10.7326/0003-4819-144-9-200605020-00006. [DOI] [PubMed] [Google Scholar]
- 35.Cone DC, Bailey ED, Spackman AB. The safety of a field termination-of-resuscitation protocol. Prehospital Emergency Care. 2005;9(3):276–81. doi: 10.1080/10903120590961996. [DOI] [PubMed] [Google Scholar]
- 36.Pepe PE, et al. Resuscitation in the out-of-hospital setting: medical futility criteria for on-scene pronouncement of death. Prehospital Emergency Care. 2001;5(1):79–87. doi: 10.1080/10903120190940399. [DOI] [PubMed] [Google Scholar]
- 37.Pirrallo RG, Swor RA. Characteristics of fatal ambulance crashes during emergency and non-emergency operation. Prehosp Disaster Med. 1994 Apr-Jun;9(2):125–32. 37. doi: 10.1017/s1049023x00041029. [DOI] [PubMed] [Google Scholar]
- 38.O’Brien E, Hendricks D, Cone DC. Field termination of resuscitation: analysis of a newly implemented protocol. Prehospital Emergency Care. 2008;12(1):57–61. doi: 10.1080/10903120701707989. [DOI] [PubMed] [Google Scholar]
- 39.Davis DP, et al. The feasibility of a regional cardiac arrest receiving system. Resuscitation. 2007;74(1):44–51. doi: 10.1016/j.resuscitation.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 40.Spaite DW, et al. The impact of prehospital transport interval on survival in out-of-hospital cardiac arrest: implications for regionalization of post-resuscitation care. Resuscitation. 2008;79(1):61–6. doi: 10.1016/j.resuscitation.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 41.Sasson C, et al. A Qualitative Study to Identify Barriers to Local Implementation of Prehospital Termination of Resuscitation Protocols. Circulation: Cardiovascular Quality and Outcomes. 2009;(2):361–368. doi: 10.1161/CIRCOUTCOMES.108.830398. [DOI] [PubMed] [Google Scholar]


