Abstract
Objective
To test the impact of a novel psychosocial intervention to improve antidepressant adherence and depression outcomes among older adults prescribed pharmacotherapy by their primary care physician.
Design
A randomized controlled pilot study was conducted to examine the usefulness of the Treatment Initiation and Participation (TIP) program as an intervention to improve antidepressant adherence and depression outcomes.
Setting
The study was conducted at two primary care clinics in New York City; one clinic served geriatric adults, and the second clinic served a diverse group of mixed aged adults.
Participants
The sample consisted of adults aged 60 and older with major depression who were recommended antidepressant therapy by their primary care physicians.
Intervention
All participants were prescribed antidepressant therapy and randomly assigned to either the intervention (TIP) or the treatment as usual (TAU) group. The TIP intervention identifies and targets psychological, barriers to depression care, especially stigma, as well as fears and misconceptions of depression and its treatment. TIP participants are encouraged to develop a treatment goal and create an adherence strategy.
Measurement
Study participants were assessed at entry, 6, 12, and 24 weeks later. Adherence was measured based on self-report with chart verification. Depression severity was measured using the Hamilton Depression Rating Scale.
Results
Participants in TIP were significantly more adherent to their antidepressant pharmacotherapy at all time points and had a significantly greater decrease in depressive symptoms than older adults who received treatment as usual.
Conclusion
The results provide support for the usefulness of TIP as a brief intervention to improve adherence to depression medication treatment provided in primary care settings.
Objective
Depression in later life is prevalent; it is expected that depression will become the second leading cause of disability worldwide in the next decade. [1] Later-life depression is associated with increased disability, [2] poor medical outcomes, risk of decline in cognition, and compromised quality of life. [3, 4] Depression, specifically, worsens the outcomes of many medical disorders and increases the risk of falls [5], suicide[6] and non-suicide mortality.[7] Effective treatment has a positive outcome beyond just the amelioration of depressive symptoms; it is associated with improved physical functioning, reduced disabilities in day to day functioning , [8] improved self-efficacy, [9] and reduced mortality. [10]
Primary care physicians provide the majority of treatment for later-life depressive illness. [11] Antidepressant therapy is safe, tolerable, easy to prescribe and can be considered the evidence-based depression treatment for older adults in primary care. [11-13] However, nonadherence to depression treatment is common with estimates ranging from 40% to 75%. [14] Key risk factors for non-adherence related to poor outcomes in the elderly include: lack of a medication administration routine, therapeutic duplication, hoarding, confusion over generic and trade names, discontinued medications retained, and multiple storage locations. [15] Medication adherence problems increase with the total number of drugs prescribed. [16] The average older American takes three prescription and four over-the-counter medications daily, and those with depression may take more medications than those without depression. [17] Even in successful controlled intervention studies for depressed older adults, nonadherence was a challenge. [18]
Attitudes and beliefs, especially perceived stigma at the initiation of care predict poor medication adherence and higher rates of mental health treatment discontinuation among depressed elderly three months later. [19-21] Perceptions of stigma are associated with feelings of social exclusion and poorer quality of life in older adults. [22] For older adults, the sense of inclusion in family and social activities is associated with quality of life. Adults in outpatient mental health treatment who perceive their social network as supportive of mental health care are significantly more likely to remain in treatment. [23, 24] While it may not be possible to eliminate stigma in the older person’s environment, it is possible to identify ways of coping with fears of stigma and disclosure, and addressing stigma as a barrier to initiating care.
While nonadherence is problematic throughout the treatment course, the early phase of treatment (first six weeks) is a particularly critical period with an increased risk of treatment drop-out, medication discontinuation, [19, 20] and vulnerability to suicide. [25] There is evidence that early antidepressant adequacy and adherence are associated with recovery from depression. Datto et al., found that early antidepressant adherence (6 weeks) predicted depression outcomes. [26, 27]
The Treatment Initiation and Participation Program (TIP)[28] in primary care is a brief, individualized intervention model program designed as an adjunct to pharmacotherapy prescribed by a primary care physician for depression treatment. The development of the TIP intervention was informed by the Theory of Reasoned Action, a health behavior model that categorizes potential factors impacting patient adherence based upon their modifiability—e.g. how specialized interventions might modify various barriers to adherence. [29] (See Figure 1). TIP specifically targets modifiable factors such as psychological barriers (e.g., stigma, beliefs about treatment self-efficacy, resignation about limitations), concerns about treatment, fears of antidepressants and attributions regarding depression etiology, and attribution of depressive symptoms to other causes which would make treatment unnecessary. While older adults face tangible barriers (e.g. transportation, medication co-payments, mobility), often it is the attitudes and beliefs that contribute to these barriers becoming insurmountable. We recognize that there are barriers to effective depression care at the provider and systemic levels, [30] and this administration of TIP did not target illness barriers such as co-morbid substance abuse or significant memory impairment. TIP is designed to focus on collaboration to empower the older adult to self-manage his/her medication treatment.
Figure 1.
Impact of TIP Intervention on Patient-Level Barriers to Depression Care in Older Adults
For this study, we hypothesized that older adults with major depression randomly assigned to TIP would have greater adherence at 6, 12, and 24 weeks after initial antidepressant prescription than those elders who received treatment as usual (TAU). Additionally, we hypothesized that TIP patients would have a greater reduction of depressive symptoms at follow-up assessments than those patients receiving usual care.
Methods
The study received approval from the Weill Cornell Medical College IRB. The study participants were recruited between July 2003 and March 2008 from two urban primary care clinics located in New York City. Potential subjects were older adults (age ≥60) with major depression seen in the participating primary care clinics and newly recommended antidepressant treatment by their primary care physicians. Subjects were either referred directly by the physician prescribing an antidepressant or identified through the medical record. Study staff contacted the patient directly to discuss the study. The initial study call was made within 24 hours of obtaining physician consent. Patients who had active suicidal ideation, psychotic depression, a history of mania, cognitive impairment (MMSE <24) or were unable to communicate in English were excluded. Participants who met study criteria were randomly assigned to either pharmacotherapy as usual (TAU) or pharmacotherapy with the Treatment Initiation and Participation (TIP) program.
Research Assessments
Research assessments were conducted with study participants at entry and 6 (at the end of the intervention), and at 12 and 24 weeks later (6 and 12 weeks after the completion of the intervention) to evaluate the impact of the TIP intervention on adherence and depressive symptoms. Assessments were conducted by trained Research Assistants who were unaware of group assignment. All subjects signed informed consent prior to participation. A structured diagnostic interview (SCID IV) at baseline confirmed the diagnosis of Major Depressive Disorder (MDD), and all study participants had a score of 14 or greater on the 24-item Hamilton Depression Rating Scale (HDRS). Overall functioning was assessed using the World Health Organization Disability Assessment Schedule (WHODAS). Adherence was assessed using a self-report measure of adherence: the Medication and Nonmedication Treatment Compliance Data form. [31] This instrument rates the proportion of doses taken on a scale from 1-6 (6=100% adherence, 5=85-80%, 4=67%, 3= 50%, 2=25% or very inconsistent, 1=nonadherent) and previously has been compared to chart blood levels of antidepressants.[19] At study completion, a chart review recorded the duration of antidepressant treatment and verified a prescription was on record for those clients who indicated they were taking antidepressant medication. Use of mental health services was recorded at 12 and 24 weeks using the Cornell Services Index. [32]
TIP Intervention
The TIP intervention format is three 30-minute individual meetings with the patient during the first six weeks of pharmacotherapy, followed by two follow-up telephone calls at 8 and 10 weeks after study entry. The three sessions allow the TIP Counselor and older adult participant to establish an alliance and work together on barriers to adherence together. However, the brevity: 1) keeps independence as the goal; 2) contrasts with psychotherapy; and 3) decreases potential dependency. There are six steps to the TIP intervention: 1) review symptoms and antidepressant therapy regimen, and conduct a barriers assessment; 2) define a personal goal that could be achieved with adherence, 3) provide education about depression and antidepressant therapy; 4) collaborate to address barriers to treatment participation; 5) create an adherence strategy; and 6) facilitate and empower the older adult to talk directly with the PCP about the treatment. A “contact sheet” which lists barriers in each domain and specific intervention techniques serves as the guide for sessions and a record of the interventions administered. This guide helps standardize the intervention while providing an opportunity to personalize the intervention to the patients’ barriers. For this pilot study, two non-physician clinicians (the PI and a senior social worker) administered the TIP intervention. For training purposes, the second clinician learned TIP by observing interventions conducted by the PI, then the PI observed the second clinician conducting two full interventions. After training was completed, the PI provided supervision through case review and review of the contact sheet.
Who is the target of the TIP intervention?
Mrs. B is a 73-year-old African-American widow who lives alone in NYC. She supports herself with Social Security, but is financially strained and worries about being able to make ends meet. She has diabetes and had hip surgery one year ago. She has an adult son who lives in Baltimore but stays in regular contact. When seen by her primary care physician (PCP), she discussed her financial worries and appeared hopeless. She reported having difficulty falling asleep, waking frequently, spending more time alone and less time reading due to difficulties concentrating. Mrs. B was not feeling well, but thought “nothing can be done”, as she saw the hip surgery as the “beginning of the end.” Upon inquiry, she reported having no real appetite, often until dinner time. Her greatest concern was that she would be unable to get around and would lose her independence. Mrs. B’s PCP identified her symptoms as major depressive disorder and prescribed her an antidepressant.
What did TIP do?
The TIP counselor met with Mrs. B, who was reluctant to take a medication. She did not see herself as depressed, attributing much of her unhappiness to her financial strain. She believed her “low moods,” decreased energy, and sleep difficulties were a natural outcome of aging. Mrs. B was worried that the medication would be addictive and was concerned that her friends would think she was “crazy.”
The TIP counselor reviewed Mrs. B’s concerns, offered information about her profile of symptoms of depression and suggested that Mrs. B’s distress might have additional origins. The counselor told Mrs. B that many people endorse the myth that depressive symptoms are “a natural part of aging.” She acknowledged Mrs. B’s concerns about stigma and her shame about needing assistance. In review of her recent history, Mrs. B was able to say that prior to her hip surgery, she did not feel so “hopeless and old.” This recollection gave her a different perspective on her symptoms. The counselor helped Mrs. B to distinguish realistic concerns about finances from hopeless thoughts. While Mrs. B was initially skeptical about treatment, she acknowledged that she would like to laugh more and enjoy visits from her neighbor more than she had. She agreed to give the medication “a try.” Mrs. B was able to build a collaborative relation with the TIP counselor and consider the information the counselor provided. This gave Mrs. B the initial impetus to try the antidepressant. Mrs. B was not sure if she was going to tell her friends about her depression or taking the medication, but she realized that disclosure was her choice. This made it easier to cope with her fears about stigma.
Data Analysis
The study groups were compared to identify any sociodemographic, functional or clinical differences using Student’s t-tests and Chi-square comparisons. An intent-to-treat Mixed Effects model with all available cases was employed to examine the changes in adherence (the percentage of doses taken as recommended) and depression severity (HDRS scores) at each follow-up point. For the analysis of depression outcomes, baseline HDRS was included as a covariate to adjust for potential differences at study entry between the two groups.
Results
Sample Characteristics
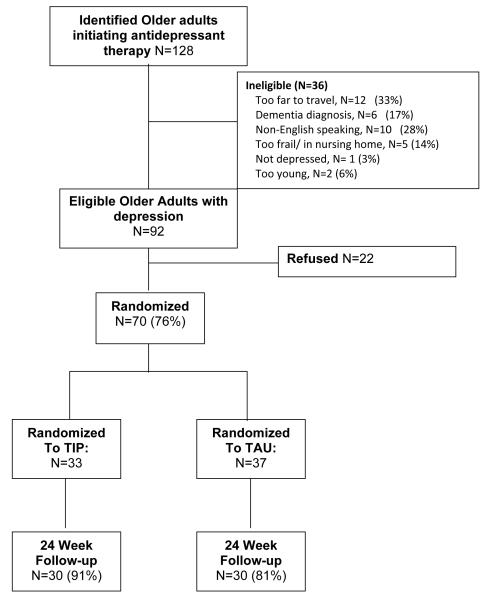
Study participants were recruited from both a geriatric primary care site (57%) and a mixed aged primary care site (43%) in New York City. Of all patients eligible for the study (N=92), 76% agreed to participate and were interviewed within 7-10 days of the referral. (See consort chart in Figure 2.) Those patients who could not be contacted within two weeks were excluded. The study consented and completed baseline assessments on 70 participants. Both TIP and TAU groups had adequate 24-week study completion (91% TIP) and (81% TAU).
Figure 2.
Flow Chart of Study Participants
The study sample was 77% female (51/66) and 71% Caucasian (47/66). Almost 14 percent (9/66) were African American or Caribbean American. An additional 14% (9/66) of the sample were of Hispanic origin. The mean age was 76 years (SD=9.0, range= 60-95). Almost one quarter (24%; 16/66) of the patients were married. There were no differences between the TIP and TAU groups on demographic characteristics (gender, age, race, education, marital status), functioning on the World Health Organization Disability Assessment Schedule (WHODAS) or adherence at baseline. Both study groups had comparable levels of depression severity on the HDRS (TIP=20.6, SD=6.7 and TAU=20.8, SD=4.1) and number of previous episodes of depression.
Impact of the TIP Intervention
To examine the impact of TIP, we conducted separate analyses with adherence and depressive symptoms as outcomes, and an exploratory analysis of the impact of adherence on outcome.
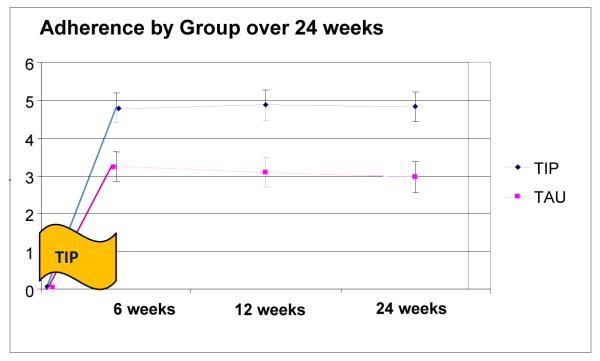
TIP participants had higher rates of adherence than TAU participants at all of the follow-up assessments (Figure 3). At the 12 week follow-up (6 weeks after the in-person intervention meetings were completed), the majority (82%) of TIP participants were adherent at the 80% level or above, as compared to only 43% of the TAU participants. A mixed-effects model of adherence found significant group differences at 6 weeks that were maintained at 12 and 24 weeks (F=13.27, df=1, 57.2, p<.001). When entered into the model, age, gender, and baseline depression severity did not modify the level of significance.
Figure 3.
Mixed Effects Model of group Adherence Scores over 24 weeks (with standard error)1
1Group effect: F=13.27, df 1,57.2, p<.001
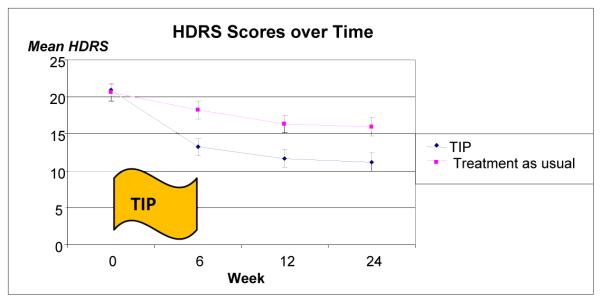
To examine the impact of TIP on depressive symptoms we conducted a mixed-effects model controlling for baseline depression severity (TIP=20.6, sd=6.6 vs. TAU=20.8, sd=5.0). Older adults in the TIP group showed a greater decrease in depressive symptoms than those elders receiving usual care (F=10.89, df=1, 55.1, p<.01). The change occurred during the early treatment period (during the TIP intervention visits weeks 1-6) and was sustained until 24 weeks. (See Figure 4)
Figure 4.
Mixed Effects Model of Depressivie Symptoms by Group over 24 weeks (with standard error)2
2Mixed Effects model F=10.89, df=1,55.1, p<.01
To explore the relation of adherence to depression outcome, we conducted two post-hoc analyses. First, we combined the TIP and TAU groups and divided the sample into those participants who were fully adherent (scores of 6 on the adherence scale) at the 6- and 12-week follow-up assessments and those who reported variable adherence or nonadherence. In a mixed-effects model, the adherent participants (across both TIP and TAU groups) had lower HDRS scores at follow-up comparison points and over time (adherence group by week F=3.92, df=3, 154 p<.01). Second we examined the rates of remission (50% reduction of 24 item HDRS score) in TIP and TAU groups at 12 and 24 weeks. At both points, a greater percentage of TIP participants showed remission than TAU participants (12 week TIP=40% vs. TAU=27%; 24 week TIP=48% and TAU=25%). Remission rates difference showed trends towards group differences at 24 weeks, but were not significantly different.
Conclusions
The data generated from this pilot study of a novel intervention provide initial support for the usefulness of the Treatment Initiation Program (TIP) in improving early adherence to antidepressant therapy provided in primary care settings. Participants in the TIP program reported greater adherence directly after the intervention as well as 6 and 12 weeks later. In addition, those participants who met with the TIP counselor showed a greater decrease in depressive symptoms. The key to the intervention, the Treatment Initiation and Participation (TIP) program, is the engagement and participation of the older adult in creating an adherence strategy tailored to his/her barriers and needs. The intervention is brief and is designed to address collaboratively the individual barriers that can contribute to antidepressant non-adherence among depressed older adults
TIP is different from other adherence interventions in two ways. First, the target barriers (e.g., patient perceptions of stigma, illness severity, and concerns about treatment) have been empirically identified in earlier research finding.[20, 28, 33, 34] Secondly, the profile of barriers addressed in the TIP program is personalized and directly informed by an assessment conducted with the older adult. Each participant identifies the barriers or challenges that are relevant to him/her. TIP goes beyond rational decision-making by helping the older adult articulate a treatment goal, identify underlying beliefs and concerns that guide treatment adherence decisions, and develop an adherence strategy that fits his/her lifestyle. The TIP intervention helps the senior articulate the often ‘irrational’ fears that s/he may be self-conscious about admitting to the PCP or even him/herself, but nonetheless become the basis for their health decisions. Although the TIP intervention is not a psychotherapy, the intervention uses a number of different techniques such as motivational interviewing, problem-solving tasks and psychoeducation. Working collaboratively with a counselor to learn about depression and its treatment, to identify and address barriers, to set treatment goals, and to plan an adherence strategy may increase the acceptability and feasibility of the depression treatment.
To date, there is little evidence in the literature that brief adherence interventions augmenting pharmacotherapy improve adherence outcomes. [35] Therefore, the study goal was to demonstrate an effect above and beyond treatment as usual (TAU). As a result of this design, a limitation of this study is that the effects of attention cannot be separated from the impact of TIP. Future work could consider the impact of TIP as compared to other attention interventions.
There are limitations to the interpretation of our findings. The small sample drawn from urban clinics is ethnically diverse, but limits the generalizability to suburban and rural older adults. Additionally, this study uses a self-report measure with good reliability. However, different measures (e.g. electronic monitoring, pill counts) yield different information that electronic monitoring and pill counts. We chose a measure that would not increase attention to adherence behaviors and might potentially serve as an intervention in itself. However, those individuals who deny their nonadherence or are unintentionally nonadherent may be underrepresented in a sample of nonadherent older adults who are self-identified. [21] This administration of TIP used both a barriers assessment and an intervention guide developed for this study. Both measures serve to standardize the administration of the intervention, but should be used in other settings and populations.
Future work should conduct the TIP intervention in different geographic areas and target other factors that may be less modifiable including common illness barriers such as somatic anxiety, alcohol use, and cognitive impairment. Increased understanding of the impact on adherence of these co-morbid conditions would increase the usefulness of the intervention in other settings. The TIP model offers a framework for exploring and improving adherence in different settings where depression in older adults is being treated.
Acknowledgements
The authors gratefully acknowledge the participating patients and the physicians from Weill Cornell Internal Medicine Associates (WCIMA) and The Wright Center, especially Robert Meyer, M.D., Mark Lachs, MD, Ron Adelman, M.D., and Cary Reid, M.D. The study was supported by NIMH K23 66381 (Sirey). The authors wish to thank Susan Friedman, C.S.W., Mooseong Heo, Ph.D., Patrick Raue, Ph.D., Dora Kanellopoulos, Pria Talwar, Nina Finkel, and Julie Ames for their contributions.
Footnotes
Data presented at the Annual Meeting of the Association of Geriatric Psychiatry in Orlando, Florida on March 13-17, 2008
Contributor Information
Jo Anne Sirey, Department of Psychiatry, Weill Cornell Medical College of Cornell University
Martha L. Bruce, Department of Psychiatry, Weill Cornell Medical College of Cornell University
Helen C. Kales, Department of Psychiatry, University of Michigan
References
- 1.Murray CJL, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. The Lancet. 1997;349(9064):1498–1504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 2.Bruce ML. Depression and disability in late life: directions for future research. Am J Geriatr Psychiatry. 2001;9(2):102–12. [PubMed] [Google Scholar]
- 3.USDHHS . Mental Health: A Report of the Surgeon General. United States Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health; Rockville, MD: 1999. [Google Scholar]
- 4.Bruce ML, et al. The impact of depressive symptomatology on physical disability: MacArthur Studies of Successful Aging. American Journal of Public Health. 1994;84:1796–1799. doi: 10.2105/ajph.84.11.1796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sheeran T, et al. Does depression predict falls among home health patients? Using a clinical-research partnership to improve the quality of geriatric care. Home Healthc Nurse. 2004;22(6):384–9. doi: 10.1097/00004045-200406000-00007. quiz 390-1. [DOI] [PubMed] [Google Scholar]
- 6.Voaklander DC, et al. Medical illness, medication use and suicide in seniors: a population-based case control study. J Epidemiol Community Health. 2008;62(2):138–46. doi: 10.1136/jech.2006.055533. [DOI] [PubMed] [Google Scholar]
- 7.Gallo JJ, et al. The effect of a primary care practice-based depression intervention on mortality in older adults: a randomized trial. Ann Intern Med. 2007;146(10):689–98. doi: 10.7326/0003-4819-146-10-200705150-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Callahan CM, et al. Treatment of depression improves physical functioning in older adults. J Am Geriatr Soc. 2005;53(3):367–73. doi: 10.1111/j.1532-5415.2005.53151.x. [DOI] [PubMed] [Google Scholar]
- 9.Hunkeler EM, et al. Long term outcomes from the IMPACT randomised trial for depressed elderly patients in primary care. BMJ. 2006 doi: 10.1136/bmj.38683.710255.BE. p. bmj.38683.710255.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gallo JJ, B. H, Morales KH, Post EP, Lin JY, Bruce ML. Interrupting the pathway between depression and death: A randomized controlled trial of a depression treatment program for older adults based in primary care (PROSPECT) Under review. [DOI] [PMC free article] [PubMed]
- 11.Arean PA, Cook BL. Psychotherapy and combined psychotherapy/pharmacotherapy for late life depression. Biol Psychiatry. 2002;52(3):293–303. doi: 10.1016/s0006-3223(02)01371-9. [DOI] [PubMed] [Google Scholar]
- 12.Alexopoulos GS. Depression in the elderly. Lancet. 2005;365(9475):1961–70. doi: 10.1016/S0140-6736(05)66665-2. [DOI] [PubMed] [Google Scholar]
- 13.Bartels SJ, Drake RE. Evidence-Based Geriatric Psychiatry: An Overview. Psychiatric Clinics of North America. 2005;28(4):763–784. doi: 10.1016/j.psc.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 14.Pampallona S, et al. Patient adherence in the treatment of depression. Br J Psychiatry. 2002;180:104–9. doi: 10.1192/bjp.180.2.104. [DOI] [PubMed] [Google Scholar]
- 15.Sorensen L, et al. Medication management at home: medication-related risk factors associated with poor health outcomes. Age and Ageing. 2005;34(6):626–32. doi: 10.1093/ageing/afi202. [DOI] [PubMed] [Google Scholar]
- 16.Barat I, Andreasen F, Damsgaard EM. Drug therapy in the elderly: what doctors believe and patients actually do. Br J Clin Pharmacol. 2001;51(6):615–22. doi: 10.1046/j.0306-5251.2001.01401.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lotrich FE, Pollock BG. Aging and clinical pharmacology: implications for antidepressants. J Clin Pharmacol. 2005;45(10):1106–22. doi: 10.1177/0091270005280297. [DOI] [PubMed] [Google Scholar]
- 18.Bogner HR, Lin JY, Morales KH. Patterns of Early Adherence to the Antidepressant Citalopram Among Older Primary Care Patients: The Prospect Study* Int’l. J. Psychiatry in Medicine. 2006;36(1):103–119. doi: 10.2190/DJH3-Y4R0-R3KG-JYCC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sirey JA, et al. Stigma as a barrier to recovery: Perceived stigma and patient-rated severity of illness as predictors of antidepressant drug adherence. Psychiatr Serv. 2001;52(12):1615–20. doi: 10.1176/appi.ps.52.12.1615. [DOI] [PubMed] [Google Scholar]
- 20.Sirey JA, et al. Perceived stigma as a predictor of treatment discontinuation in young and older outpatients with depression. Am J Psychiatry. 2001;158(3):479–81. doi: 10.1176/appi.ajp.158.3.479. [DOI] [PubMed] [Google Scholar]
- 21.Ayalon L, Arean PA, Alvidrez J. Adherence to antidepressant medications in black and Latino elderly patients. Am J Geriatr Psychiatry. 2005;13(7):572–80. doi: 10.1176/appi.ajgp.13.7.572. [DOI] [PubMed] [Google Scholar]
- 22.Depla MF, et al. The role of stigma in the quality of life of older adults with severe mental illness. Int J Geriatr Psychiatry. 2005;20(2):146–53. doi: 10.1002/gps.1264. [DOI] [PubMed] [Google Scholar]
- 23.Compton MT, Esterberg ML. Treatment delay in first-episode nonaffective psychosis: a pilot study with African American family members and the theory of planned behavior. Compr Psychiatry. 2005;46(4):291–5. doi: 10.1016/j.comppsych.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 24.DiBenedetto A. Department of Psychology. Yeshiva University; New York: 2005. The Impact of patient and social attitudes about depression. [Google Scholar]
- 25.Valenstein M, et al. Higher-risk periods for suicide among VA patients receiving depression treatment: prioritizing suicide prevention efforts. J Affect Disord. 2009;112(1-3):50–8. doi: 10.1016/j.jad.2008.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Datto CJ, Thompson R, Horowitz D, Disbot M, Bogner H, Katz I. Do Clinician and Patient Adherence Predict Outcome in a Depression Disease Management Program? JCOM. 2003;10(2):6. [Google Scholar]
- 27.Meyers BS, et al. Predictors of Early Recovery From Major Depression Among Persons Admitted to Community-Based Clinics: An Observational Study. Arch Gen Psychiatry. 2002;59(8):729–735. doi: 10.1001/archpsyc.59.8.729. [DOI] [PubMed] [Google Scholar]
- 28.Sirey JA, Bruce ML, Alexopoulos GS. The Treatment Initiation Program: An Intervention to Improve Depression Outcomes in Older Adults. Am J Psychiatry. 2005;162(1):184–186. doi: 10.1176/appi.ajp.162.1.184. [DOI] [PubMed] [Google Scholar]
- 29.Zivin K, K. H. Adherence to depression treatment in older adults. Drugs Aging. 2008;25(7):559–571. doi: 10.2165/00002512-200825070-00003. [DOI] [PubMed] [Google Scholar]
- 30.Collins KA, et al. Gaps in accessing treatment for anxiety and depression: challenges for the delivery of care. Clin Psychol Rev. 2004;24(5):583–616. doi: 10.1016/j.cpr.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 31.Glick ID, et al. A controlled evaluation of inpatient family intervention. I. Preliminary results of the six-month follow-up. Arch Gen Psychiatry. 1985;42(9):882–6. doi: 10.1001/archpsyc.1985.01790320054007. [DOI] [PubMed] [Google Scholar]
- 32.Sirey JA, et al. The Cornell Service Index as a Measure of Health Service Use. Psychiatr Serv. 2005;56(12):1564–1569. doi: 10.1176/appi.ps.56.12.1564. [DOI] [PubMed] [Google Scholar]
- 33.Sirey JA, et al. Predictors of antidepressant prescription and early use among depressed outpatients. Am J Psychiatry. 1999;156(5):690–6. doi: 10.1176/ajp.156.5.690. [DOI] [PubMed] [Google Scholar]
- 34.Sirey JA, Raue PJ, Alexopoulos GS. An intervention to improve depression care in older adults with COPD. Int J Geriatr Psychiatry. 2007;22(2):154–9. doi: 10.1002/gps.1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bosmans JE, et al. Cost effectiveness of pharmacy-based coaching programme to improve adherence to antidepressants. Pharmacoeconomics. 2007;25(1):25–37. doi: 10.2165/00019053-200725010-00004. [DOI] [PubMed] [Google Scholar]