Summary
Two cases of melanotic neuroectodermal tumour of infancy (MNTI), otherwise known as melanotic progonoma, both arising from the maxilla are presented here. The two infants both presented within three months of each other and though clinically Burkitt's lymphoma was stated as a possible diagnosis, the correct diagnosis was made on biopsy specimens. Radical surgery consisting of wide resection of the tumour with margins of healthy tissue via hemi-maxillectomy was performed in each case as an initial method of treatment. At follow up four months later, both infants appeared clinically well. One infant was then lost to follow up thereafter but the other was reviewed three years later, and apart from slight facial asymmetry, there was no evidence of tumour recurrence.
Keywords: Melanotic neuroectodermal tumour of infancy, melanotic progonoma, radical maxillary surgery
Introduction
Melanotic neuroectodermal tumour of infancy (MNTI), also known as melanotic progonoma melanoameloblastoma or retinal anlage tumour is a rare locally aggressive tumour arising most frequently from the maxilla during infancy.1–4 Infrequently, this tumour does, however, occur in the mandible and cranial vault with significant intracranial extension.2 The tumour contains melanin and is said to be derived from neural crest cells. Melanocytes have been found in the human dental primordium in fetuses of 12–18 weeks gestation pointing to involvement of neural crest cells in tooth formation.4 The occurrence of melanocytes in the dental anlage may also explain the histogenesis of pigmented lesions such as melanotic progonoma, calcifying odontogenic cysts, and the pigmented odontogenic tumour of Richardson, found in the jaws.5
Although MNTI is generally considered benign, it is known to be locally aggressive and has a potential to recur easily following surgery; as such, radical surgery is the recommended form of treatment.1, 2, 6, 7 After over 5 years follow up after radical surgery, no tumour recurrence has been reported in some cases.8 No adjuvant chemotherapy is currently recommended1 although chemotherapy has been tried in some cases that were not surgically resectable with varying response.9, 10,11. Two cases of MNTI managed successfully with surgical excision alone are presented here.
Case One
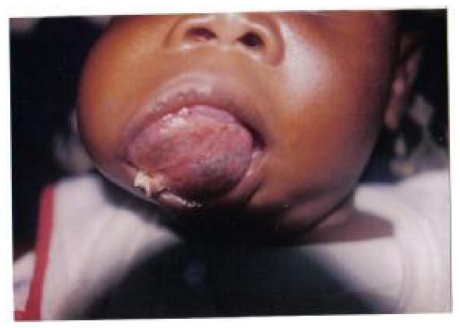
In May 2000, a 4 month-old male infant, AA, was referred to the paediatric unit of the Korle Bu Teaching Hospital, Accra, Ghana, with a large maxillary tumour. The child was normal at delivery until 1 month later when the parents noticed a swelling on the upper jaw. Over the next three months, the swelling increased rapidly in size, thus preventing the baby from being able to suck, and as such, was cup fed formula milk. On examination, he weighed 6.4kg, appeared pale and had a large tumour approximately 6cm in diameter occupying the left maxilla with protrusion into the oral cavity (Figure 1). The swelling appeared firm, was not warm to touch, and was neither tender nor mobile. Initial investigations conducted on him revealed an Hb of 6.4gm/dl and WBC count of 7.2x109/L. An initial diagnosis of possible Burkitt's Lymphoma was made but as the age at presentation was not typical, the baby was referred to the Maxillofacial unit for biopsy.
Figure 1.
Pre-operative picture of Case 1
The result of an incision biopsy indicated the lesion was a melanotic neuroectodermal tumour of infancy. Under general anaesthesia, the maxillofacial surgeon with the neurosurgeon assisting undertook a total excision of the tumour. The tumour was exposed via a Fergusson's incision and resected from the left infraorbital margin to the posterior limit of the maxilla. Remnant tumour was traced upward and completely excised from the cranial base. Histology confirmed that the surgical margins were free of tumour. His postoperative course was uneventful. He was discharged home on the tenth day post-operatively.
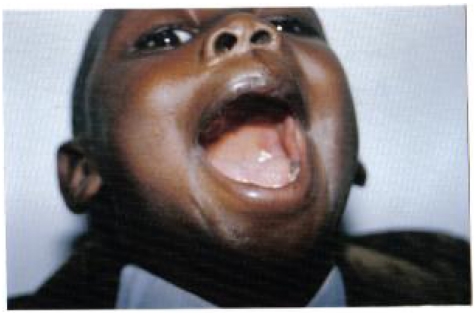
At follow-up 4 months later, he appeared well and was feeding well. Three years postoperatively, A.A. was reviewed and apart from slight facial asymmetry there was no clinical evidence of tumour recurrence (Figure 2).
Figure 2.
Case 1 three years after surgery
Case Two
Another 4 month-old male infant, I.Q., presented with a two-week history of a rapidly growing swelling in the right maxilla. On examination he weighed 5.5Kg, was not pale, had no lymphadenopathy and had a firm tumour of the right alveolar bone, between the midline and the right maxillary tuberosity, extending into the pre-maxillary bone. He was otherwise not ill looking and systems examination was normal. He was referred to the maxillofacial unit where he underwent a total resection of the tumour under general anaesthesia. A histological diagnosis of MNTI was made on the excised specimen and the surgical margins were free of tumour. No postoperative complications were encountered and he was discharged home on the fifth day. At follow-up review four months later, he was noted to be of normal development with no clinical evidence of tumour recurrence.
Discussion
Oral and maxillofacial tumours rarely occur in the paediatric population compared with the adult population. Most jaw swellings that occur in the infant are usually benign odontogenic cysts or tumours including Langerhans Cell Histiocytosis. However, some, like that reported here, though benign, tend to have alarming growth rates. There is therefore the tendency to misdiagnose them clinically as malignant lesions, especially in the African population because of the frequent occurrence of Burkitt's lymphoma of the jaws in children. It is therefore not surprising that the initial clinical diagnosis in the two cases reported here was Burkitt's lymphoma.
The importance of making the correct diagnosis based on histology of surgical specimens cannot be over emphasized. This is necessary to avoid inappropriate chemotherapy, which is very effective in the management of many other childhood malignancies. Radical surgery is the primary modality of treatment for MNTI but chemotherapy has been used in some cases with varied results after incomplete resection.
In the two cases reported here, surgery was radical, and is likely to be curative. On review four months after surgery, both patients were clinically well with no evidence of tumour recurrence. Although one was subsequently lost to follow up, the other is in clinical remission three years after surgery.
Conclusion
Two cases of MNTI, both of the maxilla in two infants, were histologically diagnosed and successfully managed by radical surgery. Though a seemingly malignant tumour by virtue of its rapid growth and local aggressiveness, MNTI is benign and radical surgery may be associated with a favourable outcome offering the potential for long-term cure. The importance of obtaining the correct histopathological diagnoses of tumours is emphasized here as this will ensure optimal management of such cases.
References
- 1.Dashti SR, Cohen ML, Cohen AR. Role of radical surgery for Intracranial melanotic neuroectodermal tumour of infancy: case report. Neurosurg. 1999;45(1):175–178. doi: 10.1097/00006123-199907000-00042. [DOI] [PubMed] [Google Scholar]
- 2.Hoeffel C, Vignaud JM, Clement A, Chelle C, Hoeffel JC. Melanotic neuroectodermal tumour of infancy. Klinische Padiatrie. 1998;210(3):99–101. doi: 10.1055/s-2008-1043868. [DOI] [PubMed] [Google Scholar]
- 3.Kaya S, Unal OF, Sarac S, Gedikoglu G. Melanotic neuroectodermal tumour of infancy: report of two cases and review of literature. Int J Pediatr Otorhinolaryngol. 2000;52(2):169–172. doi: 10.1016/s0165-5876(99)00302-x. [DOI] [PubMed] [Google Scholar]
- 4.Patel RV, Balar NN. Melanotic neuroectodermal tumour of infancy (Progonoma) Indian J Dent Research. 1991;2(3–4):54–56. [PubMed] [Google Scholar]
- 5.Lawson W, Abaci IF, Zak FG. Studies on melanocytes. V. The presence of melanocytes in the human dental primordium: an explanation of pigmented lesions of the jaws. Oral Surg Oral Med Oral Pathol. 1976;42(3):375–380. doi: 10.1016/0030-4220(76)90171-7. [DOI] [PubMed] [Google Scholar]
- 6.Gupta A, Trehan A, Marwaha RK, Nijhawan R. Melanotic neuroectodermal tumour in an infant. Indian J Pediatr. 2002;69(8):725–726. doi: 10.1007/BF02722714. [DOI] [PubMed] [Google Scholar]
- 7.Chidzonga MM. Congenital neuroectodermal tumour of infancy: report of a case. Central African J of Medicine. 1996;42(2):53–55. [PubMed] [Google Scholar]
- 8.Eckart A, Swennen G, Teltzrow T. Melanotic neuroectodermal tumour involving the mandible: 7-year follow-up after hemimandibulectomy and costochondral graft reconstruction. J craniofac Surg. 2001;12(4):349–364. doi: 10.1097/00001665-200107000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Woessmann W, Neugebauer M, Gossen R, Blutters-Sawatzki R, Reiter A. Successful chemotherapy for melanotic neuroectodermal tumor of infancy in a baby. Med Pediatr Oncol. 2003;40:198–199. doi: 10.1002/mpo.10135. [DOI] [PubMed] [Google Scholar]
- 10.Kumari TP, Venugopal M, Mathews A, Kusumakumary P. Effectiveness of chemotherapy in melanotic neuroectodermal tumor of infancy. Pediatr Hematol Oncol. 2005;22:199–206. doi: 10.1080/08880010590921450. [DOI] [PubMed] [Google Scholar]
- 11.Neven J, Hulsberghen-van der Kaa C, Grootloonen J, de Wilde PC, Merkx MA. Recurrent melanotic neuroectodermal tumour of infancy: a proposal for treatment protocol with surgery and adjuvant chemotherapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106(4):493–496. doi: 10.1016/j.tripleo.2008.02.001. [DOI] [PubMed] [Google Scholar]