Measurement of malaria mortality is a public health challenge that has been met with various solutions. Outside Africa, these estimates usually rely on governmental recorded deaths, which have been adjusted in various ways to account for incomplete reporting.1 In The Lancet today, Neeraj Dhingra and colleagues2 use the results of verbal autopsies to provide estimates for malaria mortality in India; non-medical field workers did verbal autopsies for 122 291 community deaths across 6671 sites in India between 2001 and 2003. The fieldworkers used verbal autopsies to identify the cause and severity of fever. Two trained physicians coded the results for cause of death, and disagreements were anonymously adjudicated if a consensus could not be reached. After adjudication, the investigators recorded that 3·6% of deaths between 1 month and 70 years of age were a result of malaria. The deaths that were initially attributed to malaria by one of the two physicians (3·8%) were used as a plausible upper bound, and those immediately scored by both physicians were used as the lower bound (1·7%).
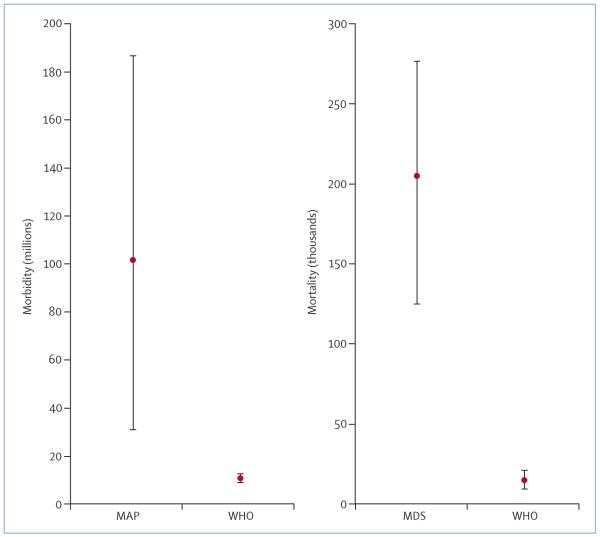
When scaled up to the national level, the investigators estimated that 205 000 deaths per year could be attributed directly to malaria with lower and upper limits of 125 000 and 277 000, respectively (figure). These estimates are strikingly different from the estimates provided by WHO,1 who report that only 15 000 malaria deaths per year (95% CI 9600–21 000) were likely to have occurred in India in 2006 (figure).
Figure. Comparison of morbidity and mortality estimates for India.
Estimates of malaria morbidity (clinical cases per year) made by the Malaria Atlas Project (MAP)3 and by WHO1 (left-hand panel), and estimates of malaria mortality made by Dhingra and colleagues’ Million Death Study (MDS)2 and by WHO1 for all ages (right-hand panel). In each case, bars show 95% uncertainty intervals and red circles are point estimates.
Despite the use of verbal autopsies by Dhingra and colleagues and many UN agencies,4 they remain an imperfect method for the estimation of malaria mortality,5 and the unexpected findings reported today therefore require further investigation.
Dhingra and colleagues offered several arguments in support of their observations. First, there was a strong geographical correlation with state-reported malaria mortality statistics; second, the malaria mortality data showed credible temporal trends with peaks after the wet season in every district; third, there was striking correspondence with malaria transmission-rates calculated independently at the district level; and fourth, this spatial correlation was not seen in three other diseases whose symptoms are often confused with malaria (dengue, typhoid, and meningitis).
We have developed maps of the spatial extents and intensity of Plasmodium falciparum transmission,5 and used these improved denominators to estimate the P falciparum clinical burden in India in 2007.6 406 million Indians were at risk of stable P falciparum transmission in 2007 with an uncertainty point estimate of 101·5 million clinical cases (95% CI 31·0–187·0 million cases; figure). Despite the uncertainty in these estimates, our lower confidence interval was three times higher than estimates provided by WHO for combined P falciparum and Plasmodium vivax clinical burden in 2006 (figure).
Could WHO’s estimates of malaria mortality and morbidity be so wrong? WHO morbidity estimates used routine data for confirmed malaria cases, adjusted for under-reporting by facilities, and a care-seeking fraction derived from national survey data on childhood fevers that were registered by formal health-care facilities. Deaths were then estimated from this total with a fixed case-fatality rate.
A startling result reported in today’s work is that 86% of deaths from malaria were not in any formal health-care facility, suggesting that deaths from malaria are predominantly unnoticed by the health-reporting system. Many workers have also noted that the health-management information system in India is not fit for purpose for the recording of malaria morbidity and mortality.7
Additionally, deaths and clinical events related to P falciparum might represent only a fraction of the total malaria disease burden in India. Dhingra and colleagues did not estimate the comorbid consequences of malaria infection—notably, the consequences associated with birth outcomes and maternal mortality, which are important in India8—nor has there been a systematic and independent review in India of the severe clinical consequences resulting from infection by P vivax.
The true effect of the malaria burden in India remains uncertain, but evidence is increasing that the scale of the burden has been greatly under-estimated—which is particularly surprising for a country that boasts a space programme and is an emerging global economic leader.
Today’s study and growing evidence from other sources should give the Indian authorities, WHO, and those who incorporate these statistics in their work4 pause for thought. Beyond India, this evidence emphasises the inadequacies in the way WHO reports global malaria cases, a process that depends heavily on routine health-reporting data. Similar disparities in WHO malaria statistics and epidemiologically derived estimates of disease burden could exist in other heavily populated, remote regions that are exposed to malaria and have unreliable access to health care, such as Burma, Bangladesh, Pakistan, Afghanistan, and Indonesia. As countries strive to improve their measurement of diseases and deaths attributable to malaria, independent studies play a crucial part in drawing attention to the inadequacies of national statistics.
Acknowledgments
SIH is funded by a Senior Research Fellowship from the Wellcome Trust (#079091) that also supports PWG. RWS is a recipient of a Wellcome Trust Principal Research Fellowship (#079080). Our work forms part of the output of the Malaria Atlas Project, mainly funded by the Wellcome Trust.
Footnotes
RWS declares that he has no conflicts of interest.
References
- 1.WHO World malaria report 2008. [accessed June 4, 2010]. 2008. http://whqlibdoc.who.int/publications/2008/9789241563697_eng.pdf.
- 2.Dhingra N, Jha P, Sharma VP, et al. the Million Death Study Collaborators Adult and child malaria mortality in India: a nationally representative mortality survey. Lancet. 2010 doi: 10.1016/S0140-6736(10)60831-8. published online Oct 21. DOI:10.1016/S0140-6736(10)60831-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hay SI, Okiro EA, Gething PW, et al. Estimating the global clinical burden of Plasmodium falciparum malaria in 2007. PLoS Med. 2010;7:e1000290. doi: 10.1371/journal.pmed.1000290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Black RE, Cousens S, Johnson HL, et al. the Child Health Epidemiology Reference Group of WHO and UNICEF Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010;375:1969–87. doi: 10.1016/S0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]
- 5.Snow RW, Armstrong JRM, Forster D, et al. Childhood deaths in Africa: uses and limitations of verbal autopsies. Lancet. 1992;340:351–55. doi: 10.1016/0140-6736(92)91414-4. [DOI] [PubMed] [Google Scholar]
- 6.Hay SI, Guerra CA, Gething PW, et al. A world malaria map: Plasmodium falciparum endemicity in 2007. PLoS Med. 2009;6:e1000048. doi: 10.1371/journal.pmed.1000048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dash AP. Estimation of true malaria burden in India: a profile of National Institute of Malaria Research. 2nd edn. National Institute of Malaria Research; New Delhi, India: 2009. pp. 91–99. [Google Scholar]
- 8.Diamond-Smith N, Singh N, Gupta RK, et al. Estimating the burden of malaria in pregnancy: a case study from rural Madhya Pradesh, India. Malar J. 2009;8:24. doi: 10.1186/1475-2875-8-24. [DOI] [PMC free article] [PubMed] [Google Scholar]