Abstract
Outcomes for 77 cataractous eyes were compared after each eye underwent no treatment, topical medical treatment only, or phacoemulsification with intraocular lens implantation. Median follow-up time for all dogs was 2.3 y. Failure occurred in all untreated eyes and the rate of failure was 65 and 255 times higher than in medically and surgically treated eyes, respectively. The failure rate was 4 times higher in dogs receiving only medical treatment compared with dogs that received surgery. Across all groups, the success rate for mature and hypermature cataracts was lower than for immature cataracts. Regardless of cataract stage, the chance of success was higher for eyes undergoing phacoemulsification than for eyes that received medical management only. Results of this study support prompt referral for phacoemulsification when cataracts are diagnosed in dogs or, if referral is not possible, topical anti-inflammatory therapy.
Résumé
Cataractes chez 44 chiens (77 yeux) : Une comparaison des résultats pour l’absence de traitement, la gestion médicale topique ou la phaco-émulsification avec l’implantation d’une lentille intraoculaire. Les résultats pour 77 yeux avec cataracte ont été comparés après que chaque œil ait soit subi aucun traitement, un traitement médical topique seulement ou une phaco-émulsification avec l’implantation d’une lentille intra-oculaire. Le temps de suivi médian pour tous les chiens était de 2,3 ans. Un échec est survenu dans tous les yeux non traités et le taux d’échec était de 65 et de 255 fois supérieur que pour les yeux médicalement et chirurgicalement traités, respectivement. Le taux d’échec était de 4 fois supérieur chez les chiens qui avaient reçu seulement un traitement médical comparativement aux chiens qui avaient subi la chirurgie. Parmi tous les groupes, le taux de succès pour les cataractes mûres et hypermûres était inférieur à celui des cataractes immatures. Sans égard au stade de la cataracte, le taux de succès était supérieur pour les yeux subissant une phaco-émulsification que pour ceux qui recevaient seulement une gestion médicale. Les résultats de cette étude appuient la recommandation de promptement référé l’animal pour une phaco-émulsification lorsque des cataractes sont diagnostiquées chez les chiens ou, s’il n’est pas possible de référer le patient, d’instaurer une thérapie anti-inflammatoire topique.
(Traduit par Isabelle Vallières)
Introduction
Cataracts occur commonly in dogs and affected dogs are presented frequently to veterinary ophthalmologists for evaluation. Underlying causes may include genetic mutations, diabetes mellitus, uveitis, congenital anomaly, trauma, toxins, and dietary deficiency (1). Surgical extraction represents the only method by which cataracts can be effectively treated. Although surgical success rates have increased over time with refinements of surgical technique, surgical success is not guaranteed. Surgery is considered to have failed when dogs develop painful and/or blinding complications such as endophthalmitis, retinal detachment, or glaucoma (2). Reported success rates, based on limited follow-up times, exceed 85% to 90% (3,4); however, these numbers decline over time (2–5).
Although phacoemulsification with intraocular lens implantation is the accepted standard, many dogs do not undergo surgery due to owner financial status, concurrent ophthalmic disease such as retinal degeneration, or concurrent systemic disease which may preclude general anesthesia. In addition, when presented with the potential complications of phacoemulsification, some owners are more comfortable opting for medical management or no treatment at all. Several studies have examined the complications arising after phacoemulsification (2,5–8); however, the authors are not aware of any studies that have assessed the complication rate for dogs with cataracts that are managed medically, or those that do not receive any therapy. The authors are also not aware of any studies comparing the outcomes of surgical versus nonsurgical management strategies. Such information is useful from a prognostic standpoint and will improve the ability of ophthalmologists and general practitioners to guide treatment decisions by owners.
The perception at our practice is that the rate of globe-threatening complications is much lower in dogs undergoing phacoemulsification and intraocular lens implantation compared with dogs receiving topical medical treatment only, or dogs receiving no treatment. Therefore, the primary objective of this study was to compare the occurrence of treatment failure for 3 categories: dogs for which neither medical nor surgical therapy was instituted, those receiving topical medical therapies only, and those undergoing phacoemulsification with intraocular lens implantation. The second objective was to document the most common complications associated with treatment failure, defined as globe or vision-threatening complications, in this practice.
Materials and methods
Medical records of dogs diagnosed with cataracts at the Western College of Veterinary Medicine between 1995 and 2005 were reviewed. Criteria for inclusion in the study were the following: examination by a veterinary ophthalmologist with confirmation of the diagnosis by complete ophthalmic examination including tonometry, slit lamp biomicroscopy, and indirect ophthalmoscopy; and a diagnosis of immature, mature, or hypermature cataracts. Dogs were excluded from the study if lens luxation and persistent hyperplastic primary vitreous/tunica vasculosa lentis were present at the time of initial examination. Dogs were also excluded from the study if medical records indicated less than 6 months’ follow-up by a veterinary ophthalmologist.
The dogs were divided into 3 groups. Group 1 included dogs that did not receive any medical or surgical treatment for cataracts. Group 2 consisted of dogs that received topical medical treatment only, in the form of ophthalmic anti-inflammatory drugs, with or without additional mydriatic therapy. Group 3 included dogs that underwent phacoemulsification with intra-ocular lens implantation.
Due to caseload bias and the tendency for ophthalmologists in this practice to prescribe topical anti-inflammatory therapy for most non-incipient cataracts, dogs that did not receive either surgical or medical therapy for cataracts were uncommon. However, a small number of such cases were identified, in which owners either refused treatment recommendations or were unaware that treatment was available.
For groups 1 and 2, success was defined as a comfortable, non-inflamed, non-glaucomatous eye at the time of last follow-up. For cases in group 3, the eye also had to be visual in order for the outcome to be defined as successful; therefore, for group 3, all eyes that became blind after surgery, regardless of cause, were considered to be failures. For all groups, a globe was considered to be a failure if it developed a painful condition, such as glaucoma or lens luxation, for which enucleation or evisceration was recommended. In addition to globes that were enucleated or eviscerated, eyes of dogs that were euthanatized were also considered to be failures.
Information for each case was summarized in a commercial spreadsheet program (Microsoft Office Excel 2003; Microsoft, Redmond, Washington, USA). Because the length of the follow-up period varied for each dog, the occurrence of treatment failure was compared across treatment options using the Cox proportional hazards model (Stata/SE 10.1 for Windows, StataCorp LP, College Station, Texas, USA). Because the unit of analysis was the individual eye and the data include more than 1 eye for many of the dogs in this study, the analysis adjusted for clustering or lack of independence of outcomes within individual animals. Other risk factors that were considered in the analysis included signalment (age, sex, and breed type), as well as pre-existing systemic and ocular conditions, and post-treatment complications that were identified in at least 5% of the study population (Table 1).
Table 1.
Cataract stage, concurrent conditions, complications, and outcomes associated with dogs undergoing surgery, medical management, or no treatment for cataracts (77 eyes from 44 dogs)
| Group | No treatment Number of eyes (dogs) 8 (n = 5) | Medical treatment Number of eyes (dogs) 35 (n = 20) | Surgical treatment Number of eyes (dogs) 34 (n = 19) |
|---|---|---|---|
| Cataract stage | |||
| Immature cataracts | 5 (3) | 16 (10) | 20 (12) |
| Mature cataracts | 3 (2) | 15 (8) | 6 (4) |
| Hypermature cataracts | 0 (0) | 4 (2) | 8 (6) |
| Concurrent condition | |||
| Diabetes mellitus | 3 (2) | 4 (6) | 6 (12) |
| Lens-induced uveitis | 1 (1) | 12 (8) | 17 (10) |
| Viterous degeneration | 0 (0) | 4 (3) | 0 (0) |
| Retinal degeneration | 0 (0) | 13 (7) | 0 (0) |
| Retinal detachmenta | 1 (1) | 0 (0) | 1 (1)b |
| Corneal disease | 2 (1) | 3 (2) | 0 (0) |
| Lens instability | 2 (2) | 0 (0) | 0 (0) |
| Glaucoma | 3 (2) | 0 (0) | 0 (0) |
| Complications | |||
| Preoperative or intraoperative capsule compromisea | 0 (0) | 0 (0) | 2 (2) |
| Intraoperative hyphema | 0 (0) | 0 (0) | 19 (13) |
| Corneal disease | 0 (0) | 9 (6) | 27 (19) |
| Glaucoma | 1 (1) | 9 (5) | 13 (8) |
| Retinal detachment | 0 (0) | 1 (1) | 6 (4) |
| Vitreous changes | 0 (0) | 1 (1) | 12 (7) |
| Lens/IOL instability | 0 (0) | 7 (5) | 1 (1) |
| Persistent uveitis | 0 (0) | 12 (8) | 4 (3) |
| Cataract progression | 0 (0) | 23 (14) | 0 (0) |
| Outcome | |||
| Success | 0 (0) | 15 (9) | 27 (16) |
| Evisceration and prosthesis/enucleation | 7 (4) | 9 (6) | 5 (3) |
| Blind, no treatment | 0 (0) | 0 (0) | 2 (1) |
| Euthanasia | 1 (1) | 11 (6) | 0 (0) |
n = total number in group.
Pretreatment retinal detachment was not examined as a risk factor in the analysis because of the infrequent (< 5%) occurrence of this condition.
Concurrent retinal detachment was present in the fellow eye, which did not undergo surgery.
All risk factors that were unconditionally associated with the rate of treatment failure (P ≤ 0.25) were considered for inclusion in the final model examining the association between treatment group (surgical, medical, or no treatment) and rate of failure. Backwards elimination was used to establish the final model that included only the risk factors that were significantly associated (P < 0.05) with the rate of failure or were important confounders (removing the variable from the model changed the effect estimate for treatment by more than 10%). Biologically sensible first-order interactions were examined where more than 2 variables were statistically significant (P < 0.05) in the final model.
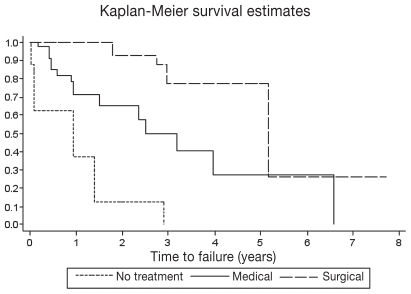
The time to failure in each treatment group was also graphed and compared across treatment groups using a log-rank test (Stata/SE 10.1 for Windows, StataCorp LP).
Results
A total of 44 dogs (77 eyes) met the inclusion criteria for the study (Table 1). There were 21 male and 23 female dogs that were presented at an average age of 8.0 y [standard deviation (s) = 3.8]. Breeds included purebred and mixed breed cocker spaniels (n = 8), toy and miniature poodles (n = 6), bichon frisés (n = 6), Boston terriers (n = 3), shih tzus (n = 3), Labrador retrievers (n = 3), Yorkshire terriers (n = 3), miniature schnauzers (n = 3), border collie (n = 1), Chihuahua (n = 1), English springer spaniel (n = 1), Siberian husky (n = 1), Jack Russell terrier (n = 1), rottweiler (n = 1), German shepherd (n = 1), Lhasa apso (n = 1), and silky terrier (n = 1).
Of these, 8 eyes from 5 dogs were not treated (Group 1). The average age at diagnosis for these dogs was 7.9 y (s = 1.9). One of the untreated dogs had unilateral disease while 4 had bilateral disease. The outcome was failure for all of the untreated eyes (Table 1).
Thirty-five eyes from 20 dogs were treated medically (Group 2). The average age at diagnosis was 8.9 y (s = 3.6). The average time from diagnosis to treatment was 32 d (s = 76). Five dogs had unilateral disease while 15 dogs had bilateral disease. A successful outcome was seen in 15 eyes of 9 dogs. Failure occurred in 20 eyes of 12 dogs (Table 1).
Thirty-four eyes from 19 dogs were surgically treated (Group 3). The average age at diagnosis was 7.4 y (s = 3.4). The average time from diagnosis to treatment was 84 d (s = 104). Four dogs had unilateral disease while 15 dogs had bilateral disease. A successful outcome was seen in 27 eyes of 16 dogs. Failure was seen in 7 eyes of 4 dogs (Table 1).
The sex (P = 0.31) of the dog and the location of the affected eye (P = 0.78) were not associated with the rate of failure for any group. Other factors not associated with the rate of failure for any group in this sample (P > 0.25) (Table 1) included preexisting vitreous degeneration (P = 0.77), glaucoma after diagnosis and treatment (P = 0.31), retinal detachment (P = 0.89), postoperative vitreous disease (P = 0.41), and postoperative uveitis (P = 0.94).
Factors that were unconditionally associated (P ≤ 0.25) with the rate of failure, and therefore considered in the development of subsequent models, were: treatment type (P = 0.0001), age at diagnosis in years (P = 0.001), breed (P < 0.0001), breed size (P = 0.25), cataract stage (P = 0.01), diabetes mellitus (P = 0.18), pre-existing lens-induced uveitis (P = 0.04), retinal degeneration (P = 0.08), preexisting corneal disease (P = 0.03), pre-existing glaucoma (P = 0.001), lens instability (P < 0.001), intraoperative hyphema (P = 0.18), postoperative corneal disease (P = 0.18), intraocular lens instability (P = 0.001), and cataract progression (P = 0.02).
After accounting for other important risk factors listed below, the rate of failure for dogs that received no treatment was 64.5 times [95% confidence interval (CI) 9.7 to 403; P < 0.0001] higher than in dogs receiving medical treatment and 255 times (95% CI, 28 to 2369; P = 0.0001) higher than in dogs receiving surgical treatment. The rate of failure for dogs receiving medical treatment alone was 4.0 times higher (95% CI, 1.0 to 15; P = 0.047) than for dogs undergoing surgery.
In the final model examining differences among treatment groups, only cataract stage (P = 0.004), age at diagnosis (P = 0.003), breed size (P = 0.03), and an interaction between age and breed size (P = 0.0001) were associated with the failure rate.
Across all groups, failure rates were higher in eyes with mature (HR, 12, 95% CI, 2.8 to 52; P = 0.001) and hypermature (HR, 4.0, 95% CI, 1.1 to 15; P = 0.04) cataracts than in eyes with immature cataracts. There was no difference in the failure rate between eyes with mature and hypermature cataracts (P = 0.11).
Due to low numbers of individuals per breed, there was insufficient power to examine breed-specific differences. Instead, dogs were categorized into groups based on breed size. Small breed dogs included Boston terrier, bichon frisé, Jack Russell terrier, Yorkshire terrier, miniature schnauzer, silky terrier, shih tzu, Lhasa apso, and Chihuahua. The cocker spaniel and the English springer spaniel were considered to be medium-sized dogs, and the border collie, Siberian husky, rottweiler, German shepherd, and Laborador retrievers were considered to be large breed dogs. Small–sized breeds > 8 y old had a higher failure rate (P = 0.003) than younger small breed dogs. There was no significant age difference in the failure rate for medium (P = 0.83) or large dogs (P = 0.09). For dogs < 8 y old, the failure rate was higher for large breed dogs (P = 0.02) and for medium breed dogs (P = 0.014) than for small breed dogs. There was no significant difference between medium and large breed groups for young dogs (P = 0.99). For dogs > 8 y old, the failure rate was higher for both small (P = 0.03) and medium breeds (P = 0.001) than for large breed dogs. There was no significant difference in the failure rate between small and medium breeds for older dogs (P = 0.67).
The median time from diagnosis of the cataract to failure was significantly different among dogs receiving no treatment and dogs receiving either medical or surgical treatment (P = 0.0001) (Figure 1). Overall, the most common complications seen in this study were cataract progression, postoperative corneal disease (consisting mainly of deep corneal ulceration and keratoconjunctivitis sicca), and intraoperative hyphema. The median time to failure in dogs receiving no treatment was 0.9 y. The most common complications in this group were persistent uveitis and glaucoma. The most common complications associated with medical treatment were cataract progression, persistent uveitis, corneal disease, and glaucoma, with the median time to failure being 1.5 y. The most common complications in the surgery group were postoperative corneal disease, intraoperative hyphema, and postoperative glaucoma (defined as an elevation in intraocular pressure above 30 mmHg after the immediate 72 h following surgery, requiring medical intervention in order to decrease the intraocular pressure). Median time to failure for dogs undergoing phacoemulsification was 2.9 y.
Figure 1.
Comparison of ocular survival times between dogs receiving surgical treatment (34 eyes from 19 dogs), medical treatment (35 eyes from 20 dogs), or no treatment (8 eyes from 5 dogs). Note that the y-axis represents the probability of eye survival at the time indicated on the x-axis.
Discussion
This study brings new information to the literature and reinforces previously published information. A higher rate of success occurred in dogs undergoing cataract surgery compared with medical management or no treatment at all in the current study. Although the success rate for hypermature and mature cataracts was less than for immature cataracts, the chances of success were still higher for all eyes undergoing phacoemulsification and intraocular lens implantation, regardless of stage, than for eyes that did not receive surgery.
The overall proportion of surgical success (79%) in this study is slightly lower than success rates from other studies in which average follow-up times ranged from 6 to 23 wk after surgery (3,5,9). Follow-up times likely influenced our success rate. In this study, mean follow-up time was 2.3 y, which is higher than the average follow-up time in other studies (3,5,9). Differences may be attributable to variations in surgical technique, postoperative treatment regimens, and study methodology. The rate of surgical success is known to decline over time (2–5). The most common complications for dogs undergoing phacoemulsification in this study were corneal disease (79.4%), intraoperative hyphema (55.9%), and glaucoma (38.2%). This is in agreement with previous findings that eyes experiencing intraoperative hemorrhage are at higher risk of surgical failure (6) and that glaucoma is a common postoperative complication (2,6,8,10). In contrast, Davidson et al (5) found retinal detachment to be the most common post-surgical complication, occurring in 4.7% of dogs. In a more recent study, 16.8% of dogs undergoing phacoemulsification developed glaucoma, while 0% to 1.25% developed retinal detachments (2).
The incidence of post-operative glaucoma (38.2%) in this study is higher than in others (2,5,8,10). The differences in follow-up times are likely to have contributed to the differences between this and other studies; however, criteria for diagnosis of glaucoma may also have played a role in the disparities. In other studies, glaucoma was generally defined as an increase in intraocular pressure accompanied by intraocular changes arising during the immediate postoperative period, up to 72 h following surgery (2,8). In this study, all eyes in which intra-ocular pressures rose above 30 mmHg during this time period were given the diagnosis of glaucoma. While all eyes with postoperative glaucoma required medications to lower intraocular pressure, a number of these cases were successfully weaned off anti-glaucoma medications after several weeks of treatment, did not have clinically detectable sequelae, and did not lose vision. It is not known if cases such as these were included within the glaucoma groups of other studies.
In this study, deep corneal ulcers and keratoconjunctivitis sicca (KCS) represented the majority of corneal diseases and were seen in both the surgically treated and medically treated groups. The development of KCS in many dogs is not surprising given that diabetic dogs, comprising a high proportion of the dogs in this study, tend to have decreased tear production compared with normal dogs (11), and that diabetic dogs with cataracts have lower tear production than non-diabetic dogs without cataracts (12). The presence of KCS may have predisposed these dogs to corneal ulceration. Another potential explanation for the high incidence of corneal ulcers may relate to the medications applied to the eyes. Chronic use of ophthalmic steroids, as is routine following cataract surgery, impairs corneal wound healing and may predispose to the development of bacterial keratitis (13,14). Additionally, medications in this study were dispensed in multidose vials, necessitating the use of ophthalmic preservatives, known to be the toxic to the corneal epithelium (15). Chronic exposure to ophthalmic preservatives may have compromised corneal health in the long-term, especially in combination with topical application of steroids and reduced aqueous tear production. This supports the higher incidence of corneal disease in the surgically treated group compared with the medically treated group (19 of 34 compared to 9 of 35), as eyes undergoing phacoemulsification typically receive many more medications, and therefore more exposure to preservatives, than eyes receiving medical management only. It is not known why the incidence of post-operative corneal disease in this study is higher than in previous studies (2,7); however, postoperative treatment protocols likely play a significant role in these differences.
Previous work has shown lens-induced uveitis to be present at all stages of cataract, regardless of clinical evidence of uveitis (16–18). The finding that clinically detectable pre-operative lens-induced uveitis did not influence outcome was therefore expected. In this study, the rates of failure for mature and hypermature cataracts were not significantly different, but were higher than the failure rate for immature cataracts. The finding of lowest success rates for mature and hypermature cataracts in this study is in agreement with others (2,5,8) and suggests the rate of surgical success declines with increasing chronicity of lens-induced uveitis. One explanation for this may be the obstruction of aqueous outflow by preiridal fibrovascular membranes, which are known to occur in the presence of persistent intraocular inflammation (19).
The lower success rate in dogs receiving medical therapy was expected. Secondary glaucoma occurs more frequently in eyes with cataract than in eyes that have undergone phacoemulsification (10,20). It is thought that approximately 20% of cataractous eyes will develop glaucoma (10). Medical treatment is aimed at reducing phacolytic uveitis, present at all stages of cataract, but cannot eliminate it because the underlying cause remains (10,16,18). Further, medical treatment does not inhibit secondary changes such as preiridal fibrovascular membrane formation (21). Intraocular pathology related to chronic uveitis would therefore be expected to increase with cataract progression and over time. Although not specifically examined in this study, owner compliance with recheck examinations may also have played a role in the decreased success rate of medical management. Owners of dogs undergoing surgery are typically highly motivated and are extensively counseled on the importance of intensive postoperative monitoring for maintaining vision. By contrast, owners of blind dogs may not see the value of administering medications long-term and re-examination of these dogs may be less often than for dogs that have undergone surgery. This hypothesis may be supported by the follow-up times in this study, which were highest for group 3 (2.5 y), followed by group 2 (1.9 y), and group 1 (0.92 y).
The finding that older small dogs were more likely to experience failure was not surprising, although this contrasts with another study in which age was not a factor in surgical outcome (4). The reasons for the findings herein likely include the fact that older dogs probably have less robust healing responses compared with younger animals. An additional factor, though not specifically examined in this study, may be a higher prevalence of more advanced cataracts and the associated secondary pathologies in older dogs.
The reason for breed-related differences in failure rates is not clear. There were insufficient numbers in this study to analyze failure rates for each breed individually; however, we were able to divide the breeds by size — small, medium, and large. For dogs < 8 y old, large and medium breeds were more likely to experience failure than small breeds, while for dogs > 8 y old, medium and small breeds were more likely to experience failure than large breeds. The variation of outcomes by breed is consistent with the literature, which reports a wide variety of breeds as being more susceptible to various postoperative complications. For example, a disproportionately high rate of glaucoma has been documented for the Boston terrier (6) while a high incidence of retinal detachment is seen in the bichon frisé following cataract surgery (22). Other studies examining secondary glaucoma, including that developing after phacoemulsification, have found a variety of breeds to be overrepresented (10,20). Labrador retrievers were over-represented in a study examining spontaneous lens rupture in diabetic dogs (23).
Due to the small number of untreated dogs (group 1), the ability to analyze these data was limited. However, due to the presence of lens-induced uveitis for all stages of cataract, untreated inflammation could have led to the development of complications requiring enucleation or evisceration and intrascleral prosthesis. This hypothesis is supported by previous work that documents phacolytic uveitis as one of the most common causes of secondary glaucoma, which was one of the more common complications in the untreated eyes (10,20). Given the poor outcomes for all affected eyes, it is apparent that anti-inflammatory treatment is the minimum accepted standard for dogs diagnosed with cataracts.
Blindness and decreased quality of life was given as the primary reason by owners of 4 of the 7 dogs who chose euthanasia following medical or no treatment. This is similar to findings of a previous study, in which approximately 10% of blind dogs were euthanized due to problems associated with blindness (24). This suggests that phacoemulsification is important not only for maximizing the chances of retaining a comfortable eye, but also for overall welfare of the dog. Restoration of vision, when possible, is clearly superior to blindness. Although blindness is still a potential outcome following phacoemulsification, a median time of 2.9 y before failure represents a significant portion of a dog’s lifespan.
There were several limitations in this study. We included only dogs with more than 6 months of follow-up. This may have negatively biased the success rate, as dogs with persistent complications are more likely to be returned for follow-up care compared with dogs for which no problems are detected. In addition, the dogs presenting to a referral institution are only a small subset of the population as a whole, and these results do not account for the individuals that are never presented to a veterinary ophthalmologist. Finally, the retrospective nature of this study limits the ability to obtain detailed clinical information from all records as well as the ability to control for multiple variables. However, differences in clinical management were minimized, as only 2 ophthalmologists managed the patients in this study and a standard postoperative treatment protocol is used at this institution.
The results of this study show a superior success rate for surgery when compared with other modes of cataract management, especially when performed early in the disease process. This should encourage general practitioners to recommend phacoemulsification more often and to refer more promptly after initial presentation. This study also underscores the grave prognosis for cataractous eyes when no treatment is instituted. This information should therefore reinforce to practitioners that when phacoemulsification is not possible, doing nothing is unacceptable and, at minimum, anti-inflammatory therapy and continued monitoring are essential for maintenance of ocular health. CVJ
Footnotes
Reprints will not be available from the authors.
Use of this article is limited to a single copy for personal study. Anyone interested in obtaining reprints should contact the CVMA office (hbroughton@cvma-acmv.org) for additional copies or permission to use this material elsewhere.
References
- 1.Davidson MG, Nelms SR. Diseases of the canine lens and cataract formation. In: Gelatt KN, editor. Veterinary Ophthalmology. 4 ed. 2 . Ames, Iowa: Blackwell Publ; 2007. pp. 859–887. [Google Scholar]
- 2.Sigle KJ, Nasisse MP. Long-term complications after phacoemulsification for cataract removal in dogs: 172 cases (1995–2002) J Am Vet Med Assoc. 2006;228:74–79. doi: 10.2460/javma.228.1.74. [DOI] [PubMed] [Google Scholar]
- 3.Davidson MG, Nasisse MP, Rusnak IM, Corbett WT, English RV. Success rates of unilateral vs bilateral cataract extraction in dogs. Vet Surg. 1990;19:232–236. doi: 10.1111/j.1532-950x.1990.tb01176.x. [DOI] [PubMed] [Google Scholar]
- 4.Miller TR, Whitley RD, Meek LA, Garcia GA, Wilson MC, Rawls BH. Phacofragmentation and aspiration for cataract extraction in dogs: 56 cases (1980–1984) J Am Vet Med Assoc. 1987;190:1577–1580. [PubMed] [Google Scholar]
- 5.Davidson MG, Nasisse MP, Jamieson VE, English RV, Olivero DK. Phacoemulsification and intraocular lens implantation: A study of surgical results in 182 dogs. Prog Vet Comp Ophthalmol. 1991;1:233–238. [Google Scholar]
- 6.Lannek EB, Miller PE. Development of glaucoma after phacoemulsification for removal of cataracts in dogs: 22 cases (1987–1997) J Am Vet Med Assoc. 2001;218:70–76. doi: 10.2460/javma.2001.218.70. [DOI] [PubMed] [Google Scholar]
- 7.Moore DL, McLellan GJ, Dubielzig RR. A study of the morphology of canine eyes enucleated or eviscerated due to complications following phacoemulsification. Vet Ophthalmol. 2003;6:219–226. doi: 10.1046/j.1463-5224.2003.00297.x. [DOI] [PubMed] [Google Scholar]
- 8.Biros DJ, Gelatt KN, Brooks DE, et al. Development of glaucoma after cataract surgery in dogs: 200 cases (1987–1998) J Am Vet Med Assoc. 2000;216:1780–1786. doi: 10.2460/javma.2000.216.1780. [DOI] [PubMed] [Google Scholar]
- 9.Bagley LH, Lavach J. Comparison of postoperative phacoemulsification results in dogs with and without diabetes mellitus: 153 cases (1991–1992) J Am Vet Med Assoc. 1994;205:1165–1169. [PubMed] [Google Scholar]
- 10.Gelatt KN, MacKay EO. Secondary glaucomas in the dog in North America. Vet Ophthalmol. 2004;7:245–259. doi: 10.1111/j.1463-5224.2004.04034.x. [DOI] [PubMed] [Google Scholar]
- 11.Williams D, Pierce V, Mellor P, Heath M. Reduced tear production in three canine endocrinopathies. J Small Anim Pract. 2007;48:252–256. doi: 10.1111/j.1748-5827.2007.00349.x. [DOI] [PubMed] [Google Scholar]
- 12.Cullen CL, Ihle SL, Webb AA, McCarville C. Keratoconjunctival effects of diabetes mellitus in dogs. Vet Ophthalmol. 2005;8:215–224. doi: 10.1111/j.1463-5224.2005.00389.x. [DOI] [PubMed] [Google Scholar]
- 13.Cohn LA. The influence of corticosteroids on host defence mechanisms. J Vet Intern Med. 1991;5:95–104. doi: 10.1111/j.1939-1676.1991.tb00939.x. [DOI] [PubMed] [Google Scholar]
- 14.Petroutsos G, Guimaraes R, Giraud J, Pouliquen Y. Corticosteroids and corneal epithelial wound healing. Br J Ophthalmol. 1982;66:705–708. doi: 10.1136/bjo.66.11.705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Burstein N. Preservative cytotoxic threshold for benzalkonium chloride and chlorhexidine digluconate in cat and rabbit corneas. Invest Ophthalmol Vis Sci. 1980;19:308–313. [PubMed] [Google Scholar]
- 16.Dziezyc J, Millichamp NJ, Smith WB. Fluorescein concentrations in the aqueous of dogs with cataracts. Prog Vet Comp Ophthalmol. 1997;7:267–270. [Google Scholar]
- 17.Leasure J, Gelatt KN, MacKay EO. The relationship of cataract maturity to intraocular pressure in dogs. Vet Ophthalmol. 2001;4:273–276. doi: 10.1046/j.1463-5216.2001.00199.x. [DOI] [PubMed] [Google Scholar]
- 18.Krohne SG, Krohne DT, Lindley DM, Will MT. Use of laser flaremetry to measure aqueous humor protein concentration in dogs. J Am Anim Hosp Assoc. 1995;206:1167–1172. [PubMed] [Google Scholar]
- 19.Peiffer R, Wilcock B, Yin H. The pathogenesis and significance of preiridal fibrovascular membrane in domestic animals. Vet Pathol. 1990;27:41–45. doi: 10.1177/030098589002700106. [DOI] [PubMed] [Google Scholar]
- 20.Johnsen DA, Maggs DJ. Evaluation of risk factors for development of secondary glaucoma in dogs: 156 cases (1999–2004) J Am Vet Med Assoc. 2006;229:1270–1274. doi: 10.2460/javma.229.8.1270. [DOI] [PubMed] [Google Scholar]
- 21.Grahn BH, Barnes LD, Breaux CB, Sandmeyer LS. Chronic retinal detachment and giant retinal tears in 34 dogs: Outcome comparison of no treatment, topical medical therapy, and retinal reattachment after vitrectomy. Can Vet J. 2007;48:1031–1039. [PMC free article] [PubMed] [Google Scholar]
- 22.Gelatt KN, Wallace MR, Andrew SE, MacKay EO, Samuelson DA. Cataracts in the Bichon Frise. Vet Ophthalmol. 2003;6:3–9. doi: 10.1046/j.1463-5224.2003.00258.x. [DOI] [PubMed] [Google Scholar]
- 23.Wilkie D, Gemensky-Metzler A, Colitz C, et al. Canine cataracts, diabetes mellitus and spontaneous lens capsule rupture: A retrospective study of 18 dogs. Vet Ophthalmol. 2006;9:328–334. doi: 10.1111/j.1463-5224.2006.00490.x. [DOI] [PubMed] [Google Scholar]
- 24.Van der Linden D, Bentley E, Miller P. Abstract no. 4: Assessment of quality of life in blind dogs. Vet Ophthalmol. 2002;5:283–301. [Google Scholar]