Abstract
Hypofractionation for prostate cancer was originally carried out in the pursuit of efficiency and convenience, but has now attracted greatly renewed interest based upon a hypothesis that prostate cancers have a higher sensitivity to fraction size, reflected in a low α/β ratio, then do late responding organs at risk such as the rectum or bladder.
Tumor control and acceptable toxicity outcomes from several hypofractionation or brachytherapy analyses do in fact support an α/β ratio for prostate cancer that is low, perhaps even lower that that for the normal organs that ordinarily constrain the delivery of radiation therapy. However, many of these studies lack sufficient patient numbers and follow-up, are clouded by dose inhomogeneity issues in the case of brachytherapy, or delivered effective doses that were too low by contemporary standards. Thus, the clinical efficacy of the approach has yet to be fully validated.
However, a number of newer prospective trials, some randomized, are underway or have reached accrual await sufficient follow-up for analysis. These studies, which cover a wide range of doses per fraction, should ultimately be capable of validating the utility of prostate hypofractionation and the models that predict its effects. With hypofractionation’s significant potential for therapeutic gain, cost savings and improved patient convenience, the future management of localized prostate cancer could be profoundly altered in the process.
Keywords: prostate cancer, hypofractionation, stereotactic body radiotherapy, fractionation
Introduction
Dose escalation, which has been demonstrated to improve biochemical control, can be accomplished with acceptably low toxicity using conformal radiotherapy techniques, but at the expense and inconvenience of delivering large number of fractions, often more than 40. An unusual prostate tumor radiobiology, however, an uncharacteristically high sensitivity to large fractions of radiation, may allow a radically different, radiobiologically-based approach to dose escalation.
The majority of results from clinical trials involving altered fraction size argue for a low α/β ratio (a high fraction size sensitivity) for prostate cancer on the order of 1-3 Gy, a value lower than or similar to values typically ascribed to the adjacent organs at risk such as bladder and rectum. Such a relationship implies that the therapeutic ratio could be improved by treating prostate cancers with fewer but larger fractions of radiation, a hypofractionation approach.
This survey will discuss the rationale for prostate hypofractionation, review ongoing and completed clinical trials and describe promising future directions.
The Case for Hypofractionation
What is the fractionation response of prostate cancer?
Conventional fractionation schemes employing fraction sizes of 1.8-2.0 Gy are based upon the premise that tumors typically are less responsive to fraction size than are late-responding normal tissues. The α/β ratio is a measure of fractionation response, with low ratios (high α/β’s) associated with late responding normal tissues. A low α/β is consistent with a greater capacity for repair between fractions, with an accompanying greater relative sparing with small fraction sizes, than for tumors with their typically higher α/β ratios. Under these conditions, an improved therapeutic ratio is achieved with multiple small fractions for most types of tumors. The α/β ratios thought to be associated with tumors, however, are typically 8 or greater, whereas for late responding normal tissues, values on the order of 3 or 4 or somewhat less for CNS are suggested from the analyses of numerous experimental and some clinical outcome studies.
Tumors other than prostate cancer have shown stronger than expected fraction size dependencies (low α/β ratios) as well, including melanomas1 and some sarcomas2.. Slow proliferation may be a hallmark of such a response and, in the case of prostate cancer, there is ample evidence for slow proliferation, based both upon direct measurement of potential doubling times and labeling indices3 and upon analysis of the kinetics of rising PSA during tumor recurrence.4 What is uncertain is whether all prostate cancers, particularly those with high grade and having possibly higher growth rates, share this characteristic.
A number of earlier analyses and reviews of clinical outcomes after brachytherapy argue for a low α/β ratio for prostate cancer.5, 6 Brenner and Hall5, for example, analyzed dose response data for external beam radiation compared with I-125 brachytherapy data and estimated a very low α/β ratio of 1.5 Gy for prostate cancer. Duschene and Peters6 concluded in analogous fashion that the α/β ratio for prostate cancer may be low and more similar to that expected for late responding normal tissue than for the typical, more rapidly proliferating tumor. These studies involved very simple calculational approaches comparing 145 Gy given at low dose rate to 70–74 Gy at fractionated high dose rates for patients with similar initial PSA levels and Gleason scores.
Fowler, Chappell and Ritter7 also conducted a comprehensive analysis of clinical outcome in patients treated with external beam radiotherapy versus I-125 or Pd-103 implants in order to further test the above analyses. An α/β ratio for prostate cancer well below 2 Gy was also estimated.
These perminent brachytherapy implant versus external beam comparisons are potentially weakened by questions about brachytherapy dose heterogeneity, effective RBE and repair rates during protracted exposure, but there is more rigorous evidence for a low α/β in studies such as that of Martinez at al8 in which patients were treated with a standard external beam course of treatment followed by high dose rate temporary implant boost doses which were escalated by decreasing fraction number from 3 to 2 and by increasing fraction size from 5.5 to 10.5 Gy. Patients were grouped according to prognostic factors and biochemical control was modeled versus equivalent dose, as calculated via a linear quadratic model. An estimated α/β ratio of 1.2 (95% CI: 0.03, 4.1 Gy) was derived, again very lowand potentially more reliable given that all patients were treated by the same modalities.
Another study utilizing both external beam and brachytherapy data is that of Williams et al9, who used a proportional hazards model to estimate the α/β ratio from data on 3756 external beam and 185 high dose rate brachytherapy boost patients. An estimated ratio of 2.6 Gy was determined, but with a wide 95% confidence interval of 0.9 to 4.8 Gy. The limited range of external beam fraction sizes as well as patient and prescription dose heterogeneity restricted the precision with which the α/β ratio could be estimated. Other efforts to estimate the α/β ratio from published clinical outcomes of purely external beam studies will be described in detail later.
Challenges have been raised, however, regarding the low estimates of the α/β ratio for prostate cancer. Some relate to the potential uncertainties surrounding permanent implant dosimetry 10, as previously mentioned, others focus on the potential confounding role of tumor cell repopulation, 11 and still others suggest a confounding role of tumor hypoxia upon the estimation of α/β 12. There are arguments that at least partially counter these concerns, however, and, with all information considered, a low α/β ratio for prostate cancer remains an attractive hypothesis supported by several lines of evidence. While clinical data supporting a low α/β ratio is becoming more plentiful, derived estimates are still characterized by wide confidence intervals. These uncertainties will ultimately not be resolved until biochemical control data from large, preferably randomized hypofractionation studies with 5 or more years of follow-up become available.
Hyupofractionation has the potential for improving therapeutic ratio
If, contrary to most other tumors, prostate cancer has a lower α/β ratio than late-responding normal tissue, the potential exists for hypofractionation to significantly improve the therapeutic ratio. The relationship between fraction size and therapeutic ratio can best be illustrated, at least over a range of fraction sizes between 1 and around 6 Gy, through use of linear quadratic modeling, which allows calculation of an equivalent dose delivered in 2 Gy fractions (EQD2) for any total dose, D, dose per fraction, d, and alpha-beta ratio, α/β :
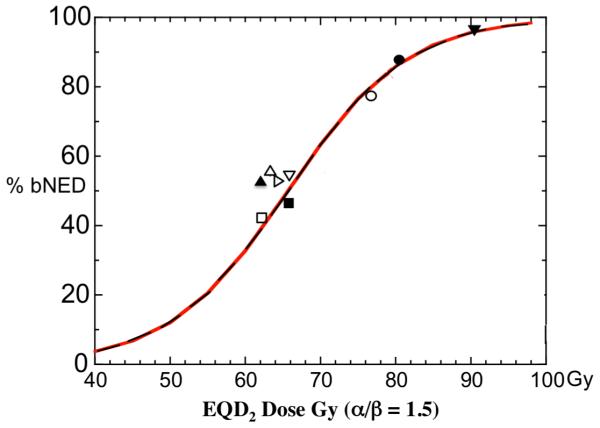
An α/β ratio for tumor less than that for at-risk normal tissues predicts an improved therapeutic ratio with hypofractionation. For example, the ratio of the EQD2 doses for tumor (with an assumed α/β of 1.5) to late normal tissue (an assumed α/β = 3) can be plotted as a function of increasing fraction size, while limiting total dose to maintain acceptable side effect risks. This therapeutic ratio is plotted as a function of fraction size in figure 1.
Figure 1. Increasing therapeutic advantage with increasing hypofractionation.
The equivalent total doses if delivered in 2 Gy fractions for prostate tumor (α/β = 1.5) and normal tissue late effects (α/β = 3) are shown versus fraction size-number combinations that preserve similar late effect levels, as would be predicted by the linear quadratic model. A reduction in total dose is required with increasing hypofractionation to maintain similar predicted late effects. The difference between the solid lines and dotted extensions on the right indicate in non-quantitative fashion a potential, over-prediction of biological effect by the linear quadratic model for very large fraction sizes.
There are several uncertainties that potentially limit the reliability of such models, however. The first, as previously discussed, is uncertainty over the tumor α/β. If prostate cancer and late normal tissue damage α/β ratios that were equal, for example, there would be no hypofractionation-related gain in therapeutic gain, although improvements in convenience and cost efficiency could still ensue.
Secondly, while the applicability of the linear quadratic model to fraction sizes ranging up to 5-6 Gy seems fairly secure, that is not the case for still larger dose fractions, a key factor when considering ultra hypofractionated, stereotactic body radiation therapy approaches. There is some support for applicability to very large fraction sizes, even 20-30 Gy13, 14, particularly with modifications as needed to account for processes such as reoxygenation and redistribution15. Other analyses, however, suggest thatapplication of the model to larger fraction sizes could under predict the total dose required to produce a given effect.16, resulting in a less toxic but also less effective treatment. Other uncertainties cited above such as reoxygenation and redistribution are also particularly relevant as the total number of fractions in a treatment course diminishes.
In spite of a significant number of remaining uncertainties, however, there remains sufficient supporting evidence to justify continuing to test the hypothesis that larger radiation fraction sizes will will be effective and safe. Although many were planned before prostate cancer’s unusual large-fraction radiobiology was suspected, a number of prostate hypofractionation trials have been carried out and information regarding the efficacy and safety of such an approach is emerging. These trials will be detailed later.
Clinical approaches using hypofractionation
Two types of hypofractionation designs can be considered, using the linear quadratic model as a basis, that would exploit the hypothesized radiobiological advantages and increase the therapeutic ratio. Hypofractionation could be designed with the intent of either reducing the normal tissue toxicity while maintaining the same tumor control, or of increasing tumor control while maintaining constant toxicity risk.
Figure 1, presented earlier, is an example of the latter approach in which increasingly more effective tumor doses can be delivered while a constant level of side effect risk is maintained. Most hypofractionation studies to date have employed this type of design.
Hypofractionation for Prostate Cancer – Clinical Experience
There are a number of older, published experiences with hypofractionated, external beam radiotherapy for prostate cancer, particularly in the UK.17-19 These treatments were generally well tolerated, but overall efficacy is difficult to assess, given the largely pre-PSA era these trials were conducted in. A number of more contemporary hypofractionation trials have either now been published or are currently underway. These are listed in Table I. In order to permit at least approximate comparisons of such diverse treatment schedules, EQD2 doses were calculated and are shown in Table 1 for assumed α/β ratios of 1.5 and 3 for prostate cancer and late responding normal tissue, respectively. It is apparent that although most of these trials have only modestly hypofractionated schedules, the EQD2 doses range between about 4 and 8 % higher for tumor than for normal tissue, illustrating the potential for therapeutic gain even with relatively modest hypofractionation if prostate cancers indeed have a lower α/β ratio than that for normal tissue.
Table 1.
Hypofractionation Trials: Schedules and Equivalent Doses in 2 Gy fractions
| Equivalent Dose in 2 Gy fractions (EQD2) |
Intermed. risk |
≥ Grade 2 Late Toxicity (%) |
||||||
|---|---|---|---|---|---|---|---|---|
| REFERENCE | No. PTS | Dose/fx size/# fxs | α/β = 1.5 (tumor) |
α/β = 3 (late effects) |
Med .F/U (mo.) |
% bPFS | GI | GU |
| Livsey et al22 Manchester |
705 | 50 Gy/3.13 Gy/16 fx | 66 Gy | 61.3 Gy | 60 | 56 (5 yr) | 5 | 9 |
| Akimoto et al35 Gumma |
52 | 69 Gy/3 Gy/23 fx | 88.7 Gy | 82.8 Gy | 33 | --- | 25 | --- |
| Tsuji et al24 Chiba |
201 | 66 GyE/2/3 GyE/20 fx (carbon ions) |
90.5 Gy | 83.1 Gy | 30 | 97 | 2 | 6 |
| Higgins et al33 Edinburgh |
300 | 52.5Gy/2.625Gy/20 fx | 61.9 Gy | 59.1 Gy | 12 | 55 | --- | --- |
| Soete et al36 Jette, Belgium |
36 | 56 Gy/3.5 Gy/16 | 80 Gy | 72.8 Gy | --- | --- | --- | --- |
| Martin et al20 Princess Margaret |
92 | 60 Gy/3 Gy/20 fx | 77.2 Gy | 72 Gy | 36 | 85 | 4 | 3 |
| Kupelian et al21, 37 Cleveland Clinic |
770 | 70 Gy/2.5 Gy/28 fx | 80 Gy | 77 Gy | 45 | 85 | 4.5 | 5.3 |
| Ritter et al28 Wisconsin |
100 100 80 (active) |
64.7 Gy/2.94Gy/22 fx 58.1 Gy/3.63Gy/16 fx 51.6 Gy/4.3Gy/12 fx |
82.6 Gy 85.1 Gy 85.5 Gy |
77 Gy 77 Gy 75 Gy |
38 24 14 |
95 | 8.5 | 1 |
| Lukka et al23 NCIC |
466 470 |
52.5/2.625 Gy/20 fx 66 Gy/2 Gy/33 fx |
61.9 Gy 66 Gy |
59.1 Gy 66 Gy |
68 | 40 | 1.3 | 1.9 |
| Yeoh et al38 Adelaid |
108 109 |
55 Gy/2.75 Gy/20 fx 64 Gy/2 Gy/32 fx |
66.8 Gy 64 Gy |
63.2 Gy 64 Gy |
48 | 57.4 55.5 |
Alternate scoring |
Alternate scoring |
| Pollack et al39 Fox Chase |
150 150 |
70.2 Gy/2.7Gy/26 fx 76 Gy/2 Gy/38 fx |
84.2 Gy 76 Gy |
80 Gy 76 Gy |
--- | --- | --- | --- |
| RTOG www.rtog.org/members/protocols/0415/0415.pdf |
Ongoing (to 1067 pts) |
70 Gy/2.5 Gy/28 fx 73.8 Gy/1.8 Gy/41 fx |
80 Gy 69.6 Gy |
77 Gy 70.8 Gy |
--- | --- | --- | --- |
| Khoo et al40 MRC |
Ongoing (to 2100 pts) |
57 Gy/3 Gy/19 fx 60 Gy/3 Gy/20 fx |
73.3 Gy 77.2 Gy |
68.4 Gy 72 Gy |
--- | --- | --- | --- |
The Princess Margaret20, Cleveland Clinic21, Manchester22, NCI-Canada23 and Chiba carbon ion24 trials are the only contemporary trial with published results that have sufficient numbers of patients and sufficient although still relatively short follow-up to enable preliminary estimates of biochemical control and toxicity. Of these, only the Princess Margaret, Cleveland Clinic and Chiba carbon ion trials delivered what would now be considered adequate EQD2 doses and had sufficient patient numbers and follow-up to adequately estimate late toxicity.
Reported toxicity in these three, higher effective dose trials was low, with the actuarial RTOG Grade ≥ 2 late rectal and genitourinary toxicity rates all generally 6% or less (Table 1). Efficacy has been consistent with expectations for conventionally dose escalated radiation therapy. For intermediate risk patients, the Cleveland clinic trial yielded a 5 year biochemical control rate of 85%, similar to that attained with that institution’s prior standard of 78 Gy in 2 Gy fractions.21 The Chiba carbon ion trial24 found a biochemical control rate of 97% at 5 years in intermediate risk patients and the Princess Margaret study20, reported a 36 month biochemical control rate of 85%, again in intermediate risk patients.
The Manchester study22, delivered an equivalent an EQD2 of 66 Gy that, by today’s standards, would be considered low and, accordingly, produced low late toxicities and relatively poor biochemical control rates. Similarly, the NCI-Canada and Edinburgh trials, each with an EQD2 of only about 62 Gy, yielded biochemical control rates and toxicities that were were correspondingly low as well. However, results from these trials as well as the higher dose Princess Margaret, Chiba and Cleveland Clinic studies, provide a range of fraction size data, allowing valuable testing of α/β ratio assumptions and of linear quadratic modeling.
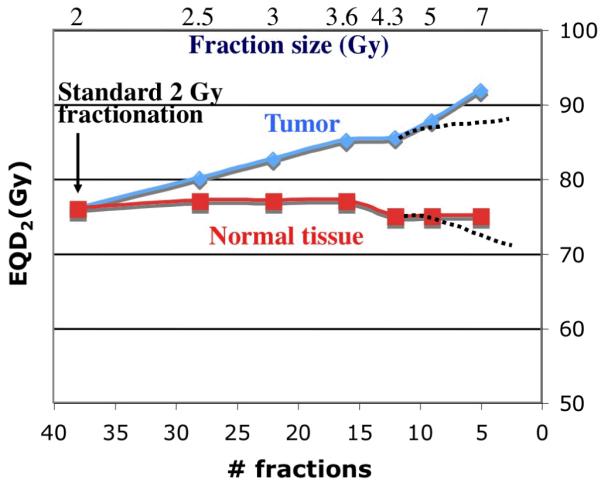
Figure 2 is a graphical representation of biochemical control rates versus equivalent dose from these six studies (for intermediate risk prostate cancer, when specifically reported). Represented are 3-5 year actuarial bDFS rates using the ASTRO definition, the only definition uniformly available in these reports. The solid, dose response curve for radiation delivered in 2 Gy fractions is adapted from Fowler et al25 and is based upon 5 year biochemical control data for intermediate risk patients from 5 conventionally fractionated prostate cancer trials. Biochemical control points from each hypofractionation trials are plotted relative to their equivalent dose (EQD2) for an assumed α/β ratio of 1.5. If higher α/β ratios had been assumed, all points would be plotted significantly further to the left of their indicated loations. The ratio of 1.5 produces plotted points that fit the standard fractionation curve reasonably well. However, there are many unaccounted for variables that prevent this from becoming a rigorous comparison, including potentially non-equivalent prognostic characteristics, treatment technique differences and variable use of androgen deprivation. Still, the degree of outcomes agreement between hypofractionated and conventional regimens when an α/β of 1.5 is assumed does suggest that prostate cancer response can in fact be characterized by a low α/β ratio.
Figure 2.
Biochemical disease-free survival (bDFS) rates versus equivalent doses from six hypofractionation studies identified in Table 1 (for intermediate risk prostate cancer, when separately reported in the publications). Shown are 3-5 year actuarial bDFS rates using the ASTRO definition, which was the only method consistently available for all reports. The solid line dose response curve for radiation delivered in 2 Gy fractions is adapted from Fowler et al18 and is based upon 3-5 year biochemical control data for intermediate risk patients from 5 conventionally fractionated prostate cancer trials. Biochemical control points from the hypofractionation trials are plotted relative to their equivalent dose for an assumed prostate cancer α/β ratio of 1.5.
Legend: NCIC32: Hypofx □, Standard ■; Edinburgh33: ▲; Adelaid34: Hypofrx △, Standard ▷; Manchester22: ▽; Princess Margaret20: ○; Cleveland Clinic21: ●; Chiba24: △.
More formalized estimates of the α/β ratio from clinical data do, in fact, reveal the inherent uncertainties involved. Analysis by Bentzen and Ritter26 of one of these trials, the NCI-Canada study23, estimated a quite low α/β ratio of 1.2 Gy, but with a wide 95% confidence interval of from −3.3 to 5.6 Gy. Another study by Williams et al, 9 a retrospective analysis of 3756 patients treated with a modest range of external beam fraction sizes or with high dose rate brachytherapy, used a proportional hazards model stratified by risk severity to estimate an α/β ratio of 2.6 Gy, but with a 95% confidence interval of from 0.9 to 4.8 Gy. A review by Dasu27 extensively reviews α/β analyses from a number of such clinical trials. It demonstrates significant variability and large confidence intervals, but again, does suggest that the ratio is low, on the order of 2 Gy or less. Thus, many studies have suggested a low α/β ratio, but the relatively narrow range of fraction sizes employed in these external beam studies has significantly limited the accuracy with which it can be measured. Low dose rate or high dose rate brachytherapy studies have employed much larger fraction sizes but, from a modeling standpoint, are plagued by a concerns over dose inhomogeneity and, in the case of low dose brachytherapy, relative biological effectiveness.
One study that, when mature, may provide a more useful range of fraction sizes is the final non-randomized study listed in Table 1, which is a multi-institutional trial (University of Wisconsin, M.D. Anderson-Orlando, Wayne State University, Medical college of Wisconsin and JT Vucurevich Cancer Inst., Rapid City). This is a phase I/II study28 that escalates dose-per-fraction in three steps, with late rectal bleeding the escalation-limiting factor. The design results in predicted late effects expected to remain relatively constant (at a level consistent with about 76 Gy delivered in 2 Gy fractions) even as fraction size escalates. The trial design also includes a nested fractions-per-week escalation/de-escalation to monitor for and prevent unacceptable acute toxicities that might result from too extreme a shortening of treatment duration and that might lead to consequential late toxicities.25
Preliminary results from this phase I/II trial28 have indicated acceptably low rates of GI and GU toxicity (2 years grade 2 GI and GU toxicity rates of 8.8 and 3%, respectively, and preliminary biochemical control rates that are high and in the expected range. The trial is nearing completion with 280 of a target 300 patients accrued. Centrally analyzed dose-volume data and the trial’s wide range of doses-per-fraction may permit solid estimates of α/β ratios both for prostate cancer as well as for adjacent organs at risk.
Thus, outcomes from a variety of hypofractionation trials provide support for a low α/β ratio for prostate cancer and justify further investigation of large fraction sizes, preferably via randomized clinical trials. Several such randomized trial that deliver acceptably high EQD2 doses have either recently completed accrual and are awaiting reporting or are currently underway (Table I), and should provide a rigorous evaluation of this treatment approach. Collection within such trials of detailed dose-volume information should be encouraged as well to permit as well an accurate analysis of the fractionation response of regional organs at risk.
Extreme Hypofractionation
Shorter hypofractionation schedules, consisting of only 4-5 fractions, are now also beginning to be explored, although not always exclusively within the context of clinical trials. Five total fractions have typically been used with fraction sizes of greater than 6-7.5 Gy are typically given, although significantly higher doses per fractions have been used in some cases. A number of uncertainties, however, make it essential that such efforts be carried in a clinical trial setting so that monitoring and reporting guidelines are established and met. Efforts to so shorten the treatment depend to some extent upon extrapolation from results obtained using more modest hypofractionation which, themselves, are not yet fully mature. In addition, significant uncertainties remain over the validity of the linear quadratic model, modified or otherwise, for predicting the biological effectiveness of these higher doses per fraction. For example, the relative contribution of differing radiation damage mechanisms likely changes with increasing fraction size29, rendering predictions from standard models unreliable.
Furthermore, in theory, the potential tumor control enhancing contributions of reoxygenation and redistribution could diminish as the number of fractions decreases and treatment duration shortens. In addition, treatment delivery accuracy-associated quality control issues such as immobilization, target motion and image guidance must be given increasing attention as the number of delivered treatments decreases,. These requirements can best be addressed in the context of prospective trials that ensure patient safety and proper documentation ofoutcomes..
Several prospective trials of extreme hypofractionation are currently underway. Five are listed in Table 2, with only the Madsen et al trial 30 having sufficient follow-up (median 48 months) to allow meaningful evaluation of biochemical control. Reported outcomes from this trial were acceptable, with actuarial late GU and GI grade 2 toxicities at 48 months of 16.1 and 9.4% respectively, and an actuarial freedom from biochemical relapse at 48 months of 90% (nadir plus 2). The Tang et al phase I/II trial31 has only reported on 30 patients and only on acute toxicities, which were acceptably low. The Timmerman et al study listed in Table 2, is an ongoing phase I/II study notable for the higher dose fractions it employs, specifically 5 fractions of either 9.5, 10 or 10.5 Gy each. Another study recently opened, this one industry sponsored ( ClinicalTrials.gov Identifier: NCT00643617), delivers 38 Gy in 4 fractions of 9.5 Gy each using Cyberknife delivery. Were standard linear quadratic modeling to remain valid at these much larger fraction sizes, these regimens could produce extraordinarily high tumor and normal tissue EQD2 doses. There is evidence, however, that the linear quadratic model significantly overestimates biological effect at very large fraction sizes16. Furthermore, normal tissue volume restrictions during treatment planning could also reduce the potential for toxicity from these high dose fractions, although, unlike some tumors such as the mid-lung, for example, the prostate has an unavoidable organ at risk, the urethra, tolerance for which must be considered.
Table 2.
Phase I/II Ultra-hypofractionation trials: Schedules and equivalent total doses in 2 Gy fractions
| Total Equivalent Dose in 2 Gy fractions (EQD2) |
≥ Grade 2 Late Toxicity (%) |
||||||
|---|---|---|---|---|---|---|---|
| REFERENCE | No. PTS | Dose/fx size/# fxs | α/β = 1.5 (tumor) |
α/β = 3 (late effects) |
Med. F/U (mo.) |
GI | GU |
| Madsen et al30 Virginia Mason |
40 | 33.5 Gy/6.7 Gy/5 fx | 78 Gy | 64.9 Gy | 41 | 7.5 | 20 |
| King et al41 Stanford |
41 | 36.25 Gy/7.25 Gy/5 fx | 90.6 Gy | 74.3 Gy | 33 | 15 | 29 |
| Widmark (personal communication, 2008) Umea |
105 | 42.7 Gy/6.1 Gy/7 fx | 92.7 Gy | 77.7 Gy | --- | --- | --- |
| Tang et al31 Univ. Toronto |
30 | 35 Gy/7 Gy/5 fx | 85.1 Gy | 70 Gy | 12 | 13 | 13 |
| Timmerman (personal communication, 2008) |
15 10 (ongoing) --- |
47.5 Gy/9.5 Gy/5 fx 50 Gy/10 Gy/5 fx 52 .5 Gy/10.5 Gy/5 fx |
149 Gy * 164 Gy 180 Gy |
118 Gy 130 Gy 142 Gy |
---- | --- | |
NTD calculations are based upon standard linear quadratic modeling, which may over predict NTD doses for large fraction sizes such as used in the UTSW trial.
Conclusions
A number of hypofractionation trials have suggested a low α/β ratio for prostate cancer that increases the therapeutic ratio when radiation fraction size is increased beyond the typical 1.8 to 2 Gy. However, precise determination of the α/β ratio both for prostate cancer and for late responding normal tissue remains difficult, while uncertainties also exist in models that seek to extrapolate biological effects seen at lower fraction sizes to the larger doses per fraction that are seeing an increasing investigational focus. Given that standard fraction size radiation therapy is already highly effective when given to sufficiently high doses, it is imperative that ongoing and future studies of hypofractionation be carried out in prospective and, ideally randomized fashion. Several such randomized trials are underway or ahave completed accrual and are awaiting sufficient follow-up for analysis. Studies such as these will have the power to ultimately validate the utility of prostate hypofractionation, making available its potential for significant therapeutic gain, cost savings and improved patient convenience. The future management of localized prostate cancer could be profoundly altered as a result.
Acknowledgments
This work was partially supported in part by NIH grants: CA106835 and CA88960
References
- 1.Bentzen SM, Overgaard J, Thames HD, et al. Clinical radiobiology of malignant melanoma. Radiother Oncol. 1989;16:169–182. doi: 10.1016/0167-8140(89)90017-0. [DOI] [PubMed] [Google Scholar]
- 2.Thames HD, Suit HD. Tumor radioresponsiveness versus fractionation sensitivity. Int J Radiat Oncol Biol Phys. 1986;12:687–691. doi: 10.1016/0360-3016(86)90081-7. [DOI] [PubMed] [Google Scholar]
- 3.Haustermans KM, Hofland I, VP H, et al. Cell kinetic measurements in prostate cancer. Int J Radiat Oncol Biol Phys. 1997;37:1067–1070. doi: 10.1016/s0360-3016(96)00579-2. [DOI] [PubMed] [Google Scholar]
- 4.Pollack A, Zagars GK, Kavadi VS. Prostate specific antigen doubling time and disease relapse after radiotherapy for prostate cancer. Cancer. 1994;74:670–678. doi: 10.1002/1097-0142(19940715)74:2<670::aid-cncr2820740220>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 5.Brenner DJ, Hall EJ. Fractionation and protraction for radiotherapy of prostate carcinoma. Int J Radiat Oncol Biol Phys. 1999;43:1095–1101. doi: 10.1016/s0360-3016(98)00438-6. [DOI] [PubMed] [Google Scholar]
- 6.Duchesne GM, Peters LJ. What is the alpha/beta ratio for prostate cancer? Rationale for hypofractionated high-dose-rate brachytherapy. Int J Radiat Oncol Biol Phys. 1999;44:747–748. doi: 10.1016/s0360-3016(99)00024-3. editorial. [DOI] [PubMed] [Google Scholar]
- 7.Fowler J, Chappell R, Ritter M. Is alpha/beta for prostate tumors really low? Int J Radiat Oncol Biol Phys. 2001;50:1021–1031. doi: 10.1016/s0360-3016(01)01607-8. [DOI] [PubMed] [Google Scholar]
- 8.Brenner DJ, Martinez AA, Edmundson GK, et al. Direct evidence that prostate tumors show high sensitivity to fractionation (low alpha/beta ratio), similar to late-responding normal tissue. Int J Radiat Oncol Biol Phys. 2002;52:6–13. doi: 10.1016/s0360-3016(01)02664-5. [DOI] [PubMed] [Google Scholar]
- 9.Williams SG, Taylor JM, Liu N, et al. Use of individual fraction size data from 3756 patients to directly determine the alpha/beta ratio of prostate cancer. Int J Radiat Oncol Biol Phys. 2007;68:24–33. doi: 10.1016/j.ijrobp.2006.12.036. [DOI] [PubMed] [Google Scholar]
- 10.D’Souza WD, Thames HD. Is the α/β ratio for prostate cancer low? Int J Radiat Biol Oncol Phys. 2001;51:1–3. doi: 10.1016/s0360-3016(01)01650-9. [DOI] [PubMed] [Google Scholar]
- 11.Wang JZ, Guerrero M, Li XA. How low is the alpha/beta ratio for prostate cancer? Int J Radiat Oncol Biol Phys. 2003;55:194–203. doi: 10.1016/s0360-3016(02)03828-2. [DOI] [PubMed] [Google Scholar]
- 12.Nahum AE, Movsas B, Horwitz EM, et al. Incorporating clinical measurements of hypoxia into tumor local control modeling of prostate cancer: implications for the alpha/beta ratio. Int J Radiat Oncol Biol Phys. 2003;57:391–401. doi: 10.1016/s0360-3016(03)00534-0. [DOI] [PubMed] [Google Scholar]
- 13.Douglas BG, Fowler JF. The effect of multiple small doses of x rays on skin reactions in the mouse and a basic interpretation. Radiat Res. 1976;66:401–426. [PubMed] [Google Scholar]
- 14.Hall EJ, Brenner DJ. Extrapolating hypofractionated radiation schemes from radiosurgery data: regarding Hall et al. IJROBP. 1991;21:819–824. doi: 10.1016/0360-3016(95)91425-R. and Hall, Brenner IJROBP. 1993;25:381–385. doi: 10.1016/0360-3016(93)90367-5. Int J Radiat Oncol Biol Phys. 1995;32:275–276.
- 15.Brenner DJ, Hlatky LR, Hahnfeldt PJ, et al. A convenient extension of the linear-quadratic model to include redistribution and reoxygenation. Int J Radiat Oncol Biol Phys. 1995;32:379–390. doi: 10.1016/0360-3016(95)00544-9. [DOI] [PubMed] [Google Scholar]
- 16.Guerrero M, Li XA. Extending the linear-quadratic model for large fraction doses pertinent to stereotactic radiotherapy. Phys Med Biol. 2004;49:4825–4835. doi: 10.1088/0031-9155/49/20/012. [DOI] [PubMed] [Google Scholar]
- 17.Collins CD, Lloyd-Davies RW, Swan AV. Radical external beam radiotherapy for localised carcinoma of the prostate using a hypofractionation technique. Clin Oncol (R Coll Radiol) 1991;3:127–132. doi: 10.1016/s0936-6555(05)80831-3. [DOI] [PubMed] [Google Scholar]
- 18.Duncan W, Warde P, Catton CN, et al. Carcinoma of the prostate: results of radical radiotherapy (1970-1985) Int J Radiat Oncol Biol Phys. 1993;26:203–210. doi: 10.1016/0360-3016(93)90198-5. [DOI] [PubMed] [Google Scholar]
- 19.Read G, Pointon RC. Retrospective study of radiotherapy in early carcinoma of the prostate. Br J Urol. 1989;63:191–195. doi: 10.1111/j.1464-410x.1989.tb05163.x. [DOI] [PubMed] [Google Scholar]
- 20.Martin JM, Rosewall T, Bayley A, et al. Phase II trial of hypofractionated image-guided intensity-modulated radiotherapy for localized prostate adenocarcinoma. Int J Radiat Oncol Biol Phys. 2007;69:1084–1089. doi: 10.1016/j.ijrobp.2007.04.049. [DOI] [PubMed] [Google Scholar]
- 21.Kupelian PA, Willoughby TR, Reddy CA, et al. Hypofractionated intensity-modulated radiotherapy (70 Gy at 2.5 Gy per fraction) for localized prostate cancer: Cleveland Clinic experience. Int J Radiat Oncol Biol Phys. 2007;68:1424–1430. doi: 10.1016/j.ijrobp.2007.01.067. [DOI] [PubMed] [Google Scholar]
- 22.Livsey JE, Cowan RA, Wylie JP, et al. Hypofractionated conformal radiotherapy in carcinoma of the prostate: five-year outcome analysis. Int J Radiat Oncol Biol Phys. 2003;57:1254–1259. doi: 10.1016/s0360-3016(03)00752-1. [DOI] [PubMed] [Google Scholar]
- 23.Lukka H, Hayter C, Julian JA, et al. Randomized trial comparing two fractionation schedules for patients with localized prostate cancer. J Clin Oncol. 2005;23:6132–6138. doi: 10.1200/JCO.2005.06.153. [DOI] [PubMed] [Google Scholar]
- 24.Tsuji H, Yanagi T, Ishikawa H, et al. Hypofractionated radiotherapy with carbon ion beams for prostate cancer. Int J Radiat Oncol Biol Phys. 2005;63:1153–1160. doi: 10.1016/j.ijrobp.2005.04.022. [DOI] [PubMed] [Google Scholar]
- 25.Fowler JF, Ritter MA, Chappell RJ, et al. What hypofractionated protocols should be tested for prostate cancer? Int J Radiat Oncol Biol Phys. 2003;56:1093–1104. doi: 10.1016/s0360-3016(03)00132-9. [DOI] [PubMed] [Google Scholar]
- 26.Bentzen SM, Ritter MA. The alpha/beta ratio for prostate cancer: what is it, really? Radiother Oncol. 2005;76:1–3. doi: 10.1016/j.radonc.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 27.Dasu A. Is the alpha/beta value for prostate tumours low enough to be safely used in clinical trials? Clin Oncol (R Coll Radiol) 2007;19:289–301. doi: 10.1016/j.clon.2007.02.007. [DOI] [PubMed] [Google Scholar]
- 28.Ritter MA, Forman JD, Kupelian PA, et al. A phase I/II trial of dose-per-fraction escalation for prostate cancer. Int J Radiat Oncol Biol Phys. 2007;69:S174. [Google Scholar]
- 29.Brown JM, Koong AC. High-dose single-fraction radiotherapy: exploiting a new biology? Int J Radiat Oncol Biol Phys. 2008;71:324–325. doi: 10.1016/j.ijrobp.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 30.Madsen BL, Hsi RA, Pham HT, et al. Stereotactic hypofractionated accurate radiotherapy of the prostate (SHARP), 33.5 Gy in five fractions for localized disease: first clinical trial results. Int J Radiat Oncol Biol Phys. 2007;67:1099–1105. doi: 10.1016/j.ijrobp.2006.10.050. [DOI] [PubMed] [Google Scholar]
- 31.Tang CI, Loblaw DA, Cheung P, et al. Phase I/II Study of a Five-fraction Hypofractionated Accelerated Radiotherapy Treatment for Low-risk Localised Prostate Cancer: Early Results of pHART3. Clin Oncol (R Coll Radiol) 2008 doi: 10.1016/j.clon.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 32.Lukka H, Hayter C, Warde P, et al. A Randomized Trial Comparing Two Fractionation Schedules for Patients with Localized Prostate Cancer. Int J Radiat Biol Oncol Phys. 2003;57:126. doi: 10.1200/JCO.2005.06.153. [DOI] [PubMed] [Google Scholar]
- 33.Higgins GS, McLaren DB, Kerr GR, et al. Outcome analysis of 300 prostate cancer patients treated with neoadjuvant androgen deprivation and hypofractionated radiotherapy. Int J Radiat Oncol Biol Phys. 2006;65:982–989. doi: 10.1016/j.ijrobp.2006.02.029. [DOI] [PubMed] [Google Scholar]
- 34.Yeoh EE, Fraser RJ, McGowan RE, et al. Evidence for efficacy without increased toxicity of hypofractionated radiotherapy for prostate carcinoma: early results of a Phase III randomized trial. Int J Radiat Oncol Biol Phys. 2003;55:943–955. doi: 10.1016/s0360-3016(02)04146-9. [DOI] [PubMed] [Google Scholar]
- 35.Akimoto T, Muramatsu H, Takahashi M, et al. Rectal bleeding after hypofractionated radiotherapy for prostate cancer: correlation between clinical and dosimetric parameters and the incidence of grade 2 or worse rectal bleeding. Int J Radiat Oncol Biol Phys. 2004;60:1033–1039. doi: 10.1016/j.ijrobp.2004.07.695. [DOI] [PubMed] [Google Scholar]
- 36.Soete G, Arcangeli S, De Meerleer G, et al. Phase II study of a four-week hypofractionated external beam radiotherapy regimen for prostate cancer: report on acute toxicity. Radiother Oncol. 2006;80:78–81. doi: 10.1016/j.radonc.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 37.Kupelian PA, Reddy CA, Carlson TP, et al. Preliminary observations on biochemical relapse-free survival rates after short-course intensity-modulated radiotherapy (70 Gy at 2.5 Gy/fraction) for localized prostate cancer. Int J Radiat Oncol Biol Phys. 2002;53:904–912. doi: 10.1016/s0360-3016(02)02836-5. [DOI] [PubMed] [Google Scholar]
- 38.Yeoh EE, Holloway RH, Fraser RJ, et al. Hypofractionated versus conventionally fractionated radiation therapy for prostate carcinoma: updated results of a phase III randomized trial. Int J Radiat Oncol Biol Phys. 2006;66:1072–1083. doi: 10.1016/j.ijrobp.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 39.Pollack A, Hanlon AL, Horwitz EM, et al. Dosimetry and preliminary acute toxicity in the first 100 men treated for prostate cancer on a randomized hypofractionation dose escalation trial. Int J Radiat Oncol Biol Phys. 2006;64:518–526. doi: 10.1016/j.ijrobp.2005.07.970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Khoo VS, Dearnaley DP. Question of Dose, Fractionation and Technique: Ingredients for Testing Hypofractionation in Prostate Cancer - the CHHiP Trial. Clin Oncol (R Coll Radiol) 2007 doi: 10.1016/j.clon.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 41.King CR, Brooks JD, Gill H, et al. Stereotactic Body Radiotherapy for Localized Prostate Cancer: Interim Results of a Prospective Phase II Clinical Trial. Int J Radiat Oncol Biol Phys. 2008 doi: 10.1016/j.ijrobp.2008.05.059. [DOI] [PubMed] [Google Scholar]