Abstract
Introduction
We assessed the prevalence of perceived stigma among persons with mental disorders and chronic physical conditions in an international study.
Methods
Perceived stigma (reporting health-related embarrassment and discrimination) was assessed to adults reporting significant disability. Mental disorders were assessed with CIDI 3.0. Chronic conditions were ascertained by self-report. 80,737 household-residing adults participated in 17 population surveys in 16 countries.
Results
Perceived stigma was present in 13.5% (22.1% in developing and 11.7% in developed countries). Suffering from a depressive or an anxiety disorder (vs. no mental disorder) was associated with about a two-fold increase in the likelihood of stigma, while comorbid depression and anxiety was even more strongly associated (OR= 4.0, 95%CI= 3.1, 5.4). Chronic physical conditions showed a lower association.
Conclusion
Perceived stigma is frequent and strongly associated with mental disorders worldwide. Efforts to alleviate stigma among individuals with comorbid depression and anxiety are needed.
Keywords: Mental Disorders, Stereotyping/Stigmatization, Disability Evaluation, Epidemiology, Health Surveys
Introduction
Mental and behavioural disorders are estimated to account for 12% of the global burden of disease worldwide(1–3). Persons with mental disorders must not only cope with the debilitating symptoms of their disease, but also with the stigma that accompanies mental illness. Stigma may have negative consequences for management of mental disorders, including delay in seeking care, or less adequate care, as well as an overall decline in quality of life(4;5). A US national survey on respondents with mental disorders found that one in four reported stigma(6). Information on the occurrence of stigma among those suffering from mental disorders in the general population is limited as most studies have been based on clinical populations(5;6), or persons with one specific disorder or severe mental illness(4–6).
The general public seems to disapprove of persons with mental illness more than persons with physical disabilities(4;7–11). But stigmatizing attitudes are not confined only to mental illness. Infectious diseases such as HIV/AIDS, tuberculosis, and leprosy have been associated with considerable stigma[Van Brakel, 2006 12723 /id]. Perceived stigma among persons with non-infectious chronic disease has not received much attention in general population samples. Nevertheless, important stigma combating initiatives have been launched in the last decade(12)(13)(14).
Stigma is a complex concept for which there exists many definitions and measures(15). Since Erving Goffman’s first notes on stigma in 1963(16), the focus on components of stigma has progressively shifted towards a social perspective(17). Key components of stigma include discrimination, embarrassment regarding impairments, perceptions of attitudes of others by persons experiencing illness, treatment-related stigma, and internalization of these attitudes by the patient[Van Brakel, 2006 12723 /id]. Among these elements, embarrassment, emotional reactions, and perceived discrimination are among the most frequently identified components used to characterize perceived stigma(15)(18)(4).
Although the social roots, concomitants and consequences of stigma are likely to vary across communities(17), no international surveys of representative population samples have addressed the extent to which persons with mental and physical disorders experience perceived stigma. Based on population-wide data from 16 countries involved in the World Mental Health Survey Initiative, this report addresses two questions: 1) Among adults with significant activity limitations, what is the prevalence of perceived stigma among persons with mental disorders and chronic physical diseases? And 2) What is the association between the report of stigma and these disorders, after controlling for demographic differences (age, sex, education) within each survey sample?
Methods
The methods employed in the World Mental Health Surveys relevant to this report have been described previously(19). Here we provide a brief overview of the key methodological features of these surveys most relevant to this report.
Samples
Seventeen surveys were carried out in 16 countries in the Americas (Colombia, Mexico, United States), Europe (Belgium, France, Germany, Italy, Netherlands, Spain, Ukraine), the Middle East (Israel, Lebanon), Africa (Nigeria), Asia (Japan, separate surveys in Beijing and Shanghai in the People's Republic of China), and the South Pacific (New Zealand). As shown in Table 1, sample sizes ranged from 2,372 (the Netherlands) to 12,992 (New Zealand), with a total of 80,737 participating adults. Response rates averaged 70 % (see Table 1). The institutional review board of the organization that coordinated the survey in each country approved and monitored compliance with procedures for obtaining informed consent and protecting human subjects.
Table 1.
Sample characteristics and population estimates of the prevalence of perceived stigma, chronic physical condition and mental disorder by country. The World Mental Health (WMH) Surveys.
| Among people with significant activity limitation | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Country | Sample Size N |
Response Rate % |
Activity Limitation |
Embarrassment (%) |
Discrimination (%) |
Perceived Stigma* (%) |
Chronic physical condition (%) |
Mental disorder (%) |
|
| N | % | ||||||||
| The Ameritas | |||||||||
| Colombia | 4426 | 87.7 | 173 | 5.0 | 33.6 | 23.8 | 17.8 | 37.8 | 29.8 |
| Mexico | 5782 | 76.6 | 185 | 4.6 | 45.1 | 25.6 | 21.0 | 27.3 | 32.2 |
| United States | 9282 | 70.9 | 1154 | 16.2 | 31.1 | 13.8 | 8.5 | 53.2 | 36.5 |
| Asia | |||||||||
| Japan | 2436 | 56.4 | 97 | 7.5 | 48.4 | 9.9 | 8.7 | 39.7 | 11.2 |
| Beijing | 2633 | 74.8 | 69 | 5.0 | 36.2 | 20.2 | 12.4 | 39.4 | 17.7 |
| Shanghai | 2568 | 74.6 | 41 | 6.5 | 44.3 | 37.7 | 22.4 | 49.6 | 5.2 |
| Lebanon | 2857 | 70.0 | 198 | 13.5 | 25.3 | 14.8 | 9.2 | 28.3 | 20.4 |
| Israel | 4859 | 79.3 | 1089 | 22.6 | 53.8 | 24.6 | 20.2 | 49.4 | 20.4 |
| Oceania | |||||||||
| New Zealand | 12,992 | 73.3 | 1393 | 14.5 | 31.9 | 14.6 | 8.7 | 46.9 | 28.2 |
| Europe | |||||||||
| Belgium | 2419 | 50.6 | 205 | 13.7 | 37.7 | 14.8 | 12.5 | 38.2 | 22.1 |
| France | 2894 | 45.9 | 244 | 13.1 | 76.7 | 13.0 | 12.8 | 31.8 | 25.9 |
| Germany | 3555 | 57.8 | 219 | 13.5 | 19.6 | 6.2 | 3.2 | 49.3 | 13.6 |
| Italy | 4712 | 71.3 | 215 | 10.0 | 37.8 | 13.5 | 13.1 | 35.3 | 18.9 |
| Netherlands | 2372 | 56.4 | 291 | 20.3 | 20.7 | 15.3 | 6.7 | 45.7 | 20.2 |
| Spain | 5473 | 78.6 | 376 | 10.3 | 15.2 | 11.7 | 8.2 | 41.4 | 20.5 |
| Ukraine | 4725 | 78.3 | 506 | 24.1 | 87.4 | 32.4 | 32.1 | 59.2 | 28.6 |
| Africa | |||||||||
| Nigeria | 6752 | 79.3 | 1089 | 22.6 | 4.4 | 17.5 | 9.7 | 25.3 | 7.8 |
| All countries | 6574 | 13.5 | 41.0 | 18.0 | 13.5 | 46.6 | 25.5 | ||
| Developing countries | 1291 | 8.6 | 56.0 | 26.2 | 22.1 | 44.4 | 24.7 | ||
| Developed countries | 5283 | 15.5 | 37.8 | 16.3 | 11.7 | 47.1 | 25.6 | ||
Stigma was considered present when both embarrassment and discrimination were reported.
The questionnaire was divided in two parts. Part 1, administered to all respondents, included screening questions on psychopathology and additional questions for the assessment of some mood and anxiety disorders as well as health status, health services utilization and main demographic characteristics. Persons who had positive responses to selected screener questions concerning mental disorders, and a probability sample of persons with no positive responses to the screener questions, participated in Part 2 of the interview. Part 2 of the interview included questions on chronic conditions, disability, and two questions concerning perceived stigma. Selection probabilities for Part 2 of the interview were incorporated into sample analysis weights so that survey estimates provide unbiased estimates for the populations surveyed.
Mental disorders
All surveys used the World Mental Health Survey version of the WHO Composite International Diagnostic Interview(19), a fully structured diagnostic interview, to assess disorders and treatment. Substantial cross-cultural work was done before producing the national versions of the instrument. We do not have empirical data, however, that show the equivalence of assessment of mental disorders across the participating countries. Nevertheless, the validity of the CIDI and its concordance with diagnoses based on follow up clinical interviews were assessed in the US and some European countries and showed acceptable values(20). Disorders considered in this paper include anxiety disorders (generalized anxiety disorder, panic disorder and/or agoraphobia, posttraumatic stress disorder, and social phobia) and mood disorders (dysthymia and major depressive disorder). Disorders were assessed using the definitions and criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV)(21). The analyses in this paper concern persons with: 1) an anxiety disorder in the absence of comorbid mood disorder; 2) a mood disorder in the absence of comorbid anxiety disorder; or 3) comorbid mood and anxiety disorder. All disorders considered referred to the 12 months prior to the interview.
Chronic physical conditions
Using a standard chronic disorders checklist(22) respondents were asked whether they had ever been told by a doctor they had: stroke, heart attack or heart disease, asthma or COPD, diabetes, ulcer, HIV/AIDS, epilepsy, tuberculosis and cancer. The number of chronic physical disorders were grouped as 0, 1, and 2+, (heart attack and heart disease were counted as one condition, and asthma and COPD as well).
Perceived Stigma
Stigma was assessed with two items from the WHODAS II(23): “How much embarrassment did you experience because of your health problems during the past 30 days?” and “How much discrimination or unfair treatment did you experience because of your heath problems during the past 30 days?”. For both questions, response options included: “None, a little, some, a lot, or extreme”. Individuals endorsing at least ‘A little’ embarrassment and at least ‘A little’ discrimination were considered to have perceived stigma. Because perceived stigma related to health problems is most relevant to persons with significant health problems, the stigma questions were only administered to individuals who reported significant activity limitation due to health problems in the month prior to the interview. To qualify as having significant activity limitation, a respondent was required to report at least moderate difficulty with 2 or more items in the following WHODAS-II domains: cognition, mobility, self care, and social.
Analyses
Odds ratios for the association of chronic physical conditions and mental disorders with stigma were estimated via logistic regression, with perceived stigma as the dependent variable. Predictors included age (4 levels), gender, education level (completed secondary education or not), number of chronic physical conditions (0, 1, 2+) and number and type of mental disorders (none; only mood, only anxiety; and comorbid mood and anxiety). Information on education was not available for France. We did not perform logistic regression analyses for countries if fewer than 20 people reported stigma.
Data are presented for each individual country and for all the countries, developing countries, that is those with a World Development Index <0.90 (i.e. Beijing, Colombia, Lebanon, Mexico, Nigeria, Ukraine, and Shanghai) and developed countries. All analyses employed weighted data to adjust for sample selection probabilities. Ninety-five percent confidence intervals for the odds ratios were estimated using the Taylor Series method(24) with SUDAAN software(25) to adjust for clustering and weighting. Pooled estimates for surveys in developed and developing countries, and for all surveys combined, take into account clustering within each survey sample.
Results
Table 1 shows the weighted proportion of the adult population with significant activity limitations as well as the proportions reporting health-related embarrassment, health-related discrimination, and overall perceived stigma (the presence of both embarrassment and discrimination). Also, the prevalence of physical and mental disorders is presented. The prevalence of significant activity limitation ranged from 4.4% to 24.1%. Among those with significant activity limitations, embarrassment (range 15.2 to 87.4%) was more common than discrimination (range 6.2% to 37.7%). Table 1 also shows that among persons with significant activity limitations, perceived stigma was relatively common: 13.5% in the overall sample (22,1% in developing and 11.7% in developed countries)
Mean age was similar among those with and without perceived stigma. Male gender and lower education levels tended to be more common among persons reporting perceived stigma than among those not reporting it. The prevalence of perceived stigma among persons with and without chronic physical disease, and among persons with and without a mental disorder, is shown in Table 2. Except in three countries with small numbers of respondents with significant activity limitations (Beijing, Shanghai, Lebanon), the prevalence of health related stigma was greater among persons with a mental disorder (prevalence for all countries: 21.9%) than among persons without a mental disorder (10.6%). In contrast, there was no clear difference in the prevalence of perceived stigma among persons with a chronic physical condition (15.5%) relative to those without (11.8%). Of course, comparison of prevalence rates of perceived stigma among persons with and without chronic physical disease and persons with and without a mental disorder is not meaningful without controlling for differences in age, sex, educational attainment and comorbidity.
Table 2.
Percent prevalence (and 95% confidence intervals) of perceived stigma according to chronic physical condition and mental disorder status among persons with significant activity limitation. The World Mental Health (WMH) Surveys.
| Chronic Physical Condition |
Mental Disorder |
|||
|---|---|---|---|---|
| Country | Absent % (95% CI) |
Present % (95% CI) |
Absent % (95% CI) |
Present % (95% CI) |
| The Americas | ||||
| Colombia | 12.5 (7.8, 19.6) | 26.6 (17.1, 38.8) | 12.1 (6.2, 22.3) | 31.4 (18.9, 47.3) |
| Mexico | 20.4 (12.6, 31.2) | 22.6 (14.7, 33.2) | 12.3 (6.6, 21.7) | 39.2 (27.8, 52.0) |
| United States | 6.8 (4.9, 9.4) | 10.0 (7.2, 13.8) | 3.7 (2.2, 6.2) | 16.9 (12.9, 21.9) |
| Asia | ||||
| Japan | 9.1 (4.3, 18.5) | 8.0 (2.3, 24.6) | 6.3 (3.3, 11.7) | 27.8 (11.2, 54.0) |
| Beijing | 11.5 (4.8, 25.1) | 13.8 (5.3, 31.8) | 12.6 (6.2, 23.9) | 11.5 (3.4, 32.8) |
| Shanghai | 2.9 (0.4, 17.0) | 42.2 (10.1, 82.6) | 22.5 (6.9, 53.1) | 21.9 (2.4, 75.8) |
| Lebanon | 9.4 (3.3, 24.0) | 5.7 (1.8, 16.9) | 10.8 (6.0, 18.7) | 2.9 (1.0, 8.1) |
| Israel | 17.1 (14.0, 20.7) | 23.4 (19.8, 27.3) | 17.4 (14.9, 20.3) | 30.9 (24.7, 7.8) |
| Oceania | ||||
| New Zealand | 9.1 (6.6, 12.6) | 8.1 (5.8, 11.3) | 5.8 (3.9, 8.6) | 16.0 (12.2, 20.5) |
| Europe | ||||
| Belgium | 12.7 (6.9, 22.2) | 12.1 (5.3, 25.4) | 10.2 (5.1, 19.4) | 20.6 (10.2, 37.1) |
| France | 7.6 (3.4, 16.4) | 24.0 (10.0, 47.4) | 9.2 (3.0, 25.1) | 23.2 (11.9, 40.3) |
| Germany | 3.6 (1.8, 7.3) | 2.9 (1.1, 7.6) | 0.7 (0.4, 1.5) | 19.3 (9.9, 34.4) |
| Italy | 12.0 (6.7, 20.5) | 15.0 (8.0, 26.3) | 10.3 (5.6, 18.3) | 24.9 (15.4, 37.6) |
| Netherlands | 7.7 (3.3, 16.9) | 5.5 (2.6, 11.3) | 6.0 (2.6, 13.2) | 9.3 (4.4, 18.7) |
| Spain | 8.5 (4.6, 15.2) | 7.7 (3.4, 16.4) | 5.5 (2.5, 11.4) | 18.7 (12.5, 26.9) |
| Ukraine | 30.3 (21.1, 41.3) | 33.4 (26.4, 41.3) | 30.0 (22.1, 39.3) | 37.5 (31.1, 44.4) |
| Africa | ||||
| Nigeria | 9.9 (5.7, 16.5) | 9.2 (2.7, 26.8) | 7.6 (4.2, 13.4) | 35.2 (13.8, 64.7) |
| All countries | 11.8 (10.6, 13.3) | 15.5 (13.8, 17.3) | 10.6 (9.4, 12.0) | 21.9 (19.8, 24.1) |
| Developing countries | 18.3 (14.6, 22.7) | 28.2 (22.9, 34.2) | 19.2 (15.4, 23.6) | 31.2 (26.8, 36.0) |
| Developed countries | 10.5 (9.2, 12.0) | 13.0 (11.5, 14.8) | 8.8 (7.7, 10.1) | 20.0 (17.7, 22.5) |
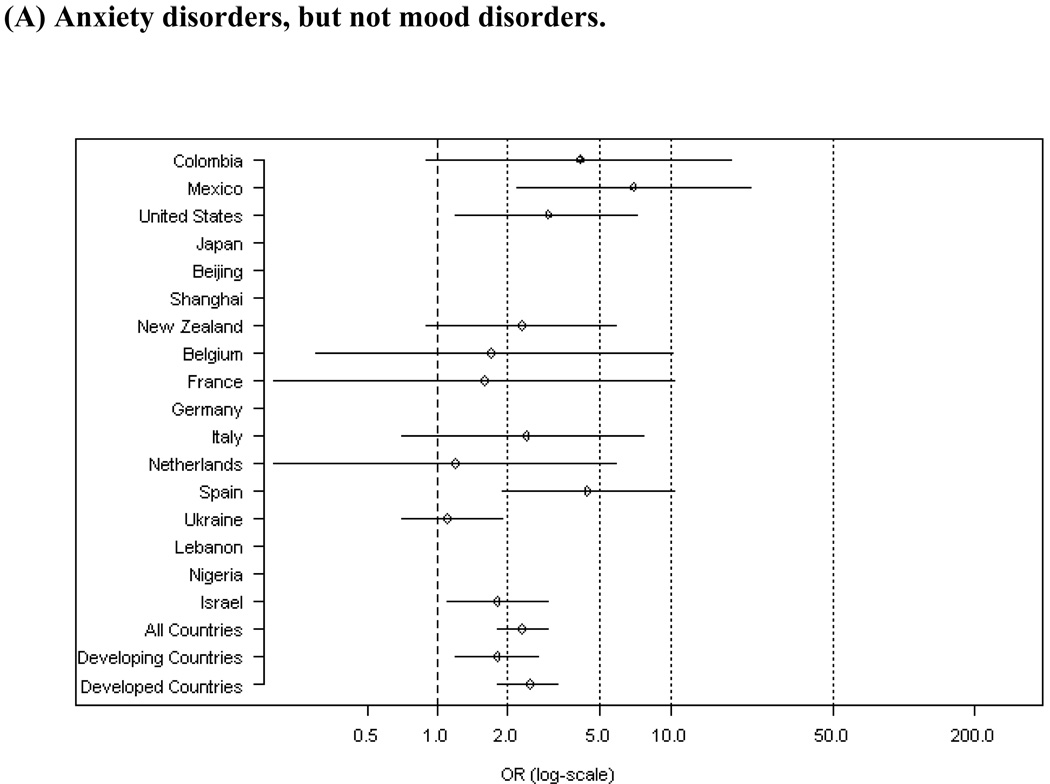
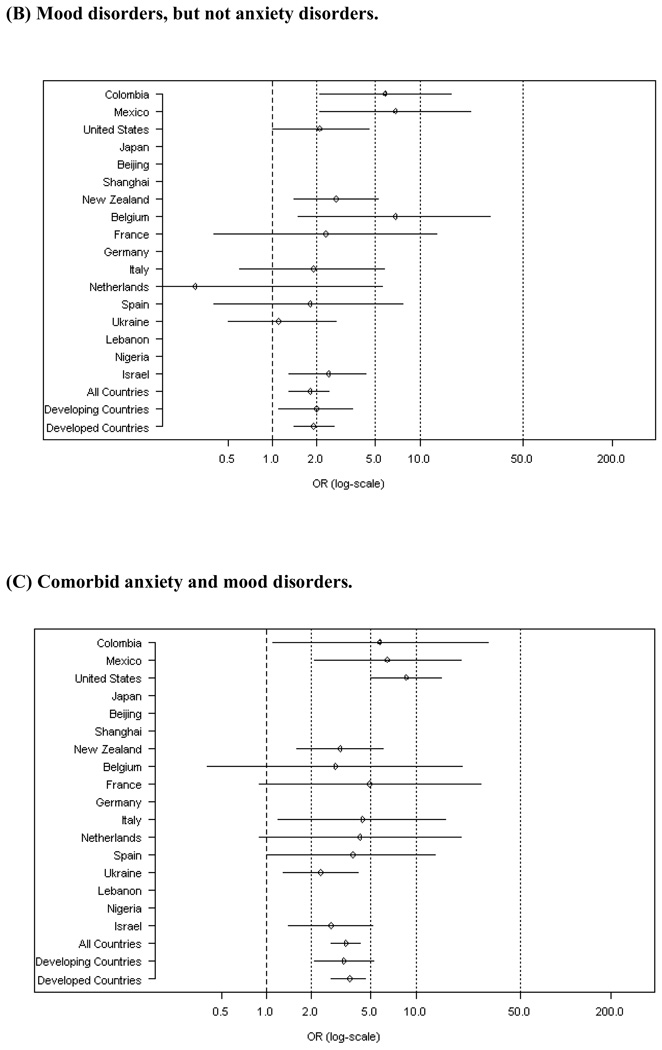
The association of chronic physical disease and mental disorder status with perceived stigma, controlling for age, sex, education and for comorbidity, is presented in Table 3. Compared to those without a chronic physical condition, perceived stigma was somewhat more likely to be reported by those with 2 or more chronic physical conditions (pooled odds ratios of 1.3 for a single chronic condition and 1.4 p<.05 for multiple chronic conditions, p<.05 for both). In contrast, perceived stigma was much more likely to occur among individuals with mental disorders in comparison to those without mental disorders. As shown in Table 4 and Figure (A), there was an increased occurrence of stigma for persons with an anxiety disorder in the absence of a mood disorder (OR= 1.8, p<.05, Figure A) and for persons with a mood disorder in the absence of an anxiety disorder (OR= 2.3, p<.05). Among persons with comorbid mood and anxiety mental disorders, the increased risk of stigma was greater still (OR= 3.4, p<.05, Figure C). The pattern of association of perceived stigma with anxiety and depressive disorders was similar in both developed and developing countries.
Table 3.
Odds ratios (and confidence intervals) for perceived stigma according to the number of chronic physical conditions and mental disorder status, controlling for age, sex and education, among people with significant activity limitation. The World Mental Health (WMH) Surveys.
| Chronic Physical Condition (reference= none) |
Mental Disorder (reference= none) |
||||
|---|---|---|---|---|---|
| country | one | 2+ | Anxiety only | Mood only | Comorbid mood & anxiety |
| All countries | 1.3 (1.0, 1.6) * | 1.4 (1.1, 1.8) * | 1.8 (1.3, 2.4) * | 2.3 (1.8, 3.0) * | 3.4 (2.7, 4.2) *† |
| Developing countries | 1.7 (1.0, 2.8) * | 1.3 (0.8, 2.1) | 2.0 (1.1, 3.5) * | 1.8 (1.2, 2.7) * | 3.3 (2.1, 5.2) * |
| Developed countries | 1.1 (0.9, 1.5) | 1.6 (1.2, 2.1) * | 1.9 (1.4, 2.6) * | 2.5 (1.8, 3.3) * | 3.6 (2.7, 4.6) * |
p< 0.05
Country not included if fewer than 20 people have stigma
Pooled odds ratios (ORs) for comorbid mood and anxiety disorders are significantly greater than the pooled OR for non-comorbid mood and non-comorbid anxiety.
Figure 1.
Odds ratios (ORs) for the effect of having certain mental disorders (versus having no mental disorder) on perceived stigma, controlling for age, sex, education and chronic physical conditions.
We assessed whether the presence of comorbid mood and anxiety disorder was more strongly associated with perceived stigma than non-comorbid mood and non-comorbid anxiety disorder (results not shown). In the pooled analysis, the risk of perceived stigma was significantly lower (OR= 0.7, 95% CI= 0.5 to 0.9) for persons with mood disorder only and for persons with anxiety disorder only (OR= 0.5, 95% confidence interval of 0.4 to 0.7) relative to persons with comorbid mood and anxiety. Thus, the presence of comorbid mood and anxiety disorder was associated with significantly greater likelihood of perceived stigma than among persons with non-comorbid mood or anxiety disorders. We also assessed whether persons with a mental disorder without a comorbid physical disorder were more likely to report perceived stigma than persons with a physical disorder without a mental disorder. In a pooled analysis, persons with a mood or an anxiety that was not comorbid with a physical disorder were more likely to report stigma (OR= 1.9, 95% CI= 1.2 to 2.4) relative to persons with a chronic physical disorder that was not comorbid with a mental disorder.
Discussion
Our results show that among persons with significant activity limitations, perceived stigma is commonly reported, where stigma is defined by the presence of both embarrassment and perceived discrimination. Despite between-country variation in the prevalence of perceived stigma, mental disorders and particularly comorbid depression and anxiety showed a robust association with stigma, while chronic physical disorders showed a relatively weak association. Thus, mental disorders appear to be a considerably more important correlate of perceived stigma than chronic physical conditions among persons in the general population with significant activity limitations in both developed and developing countries.
The results presented here must be interpreted in the context of several limitations. First, the questions about perceived stigma were administered only to those individuals who reported significant activity limitation in the month before the interview. The underlying assumption was that questions about perceived stigma are not particularly salient to individuals who do not experience activity limitations. Second, we evaluated perceived stigma using only two items instead of more complex measures used in studies focused largely on perceived stigma(26). This might render comparability with other studies difficult. Had we studied it in more detail, we likely would have found a higher prevalence of stigma. Given the scope of the World Mental Health Surveys, the number of questions that could be devoted to assessing stigma was necessarily limited, which can have implications for measurement error in assessment of perceived stigma(27). Generalizability may be further hindered because of the low response rates in some other countries, although many countries had response rates well over the expected 70%. Third, although the entire questionnaire was cross-culturally adapted using state-of-the-art methods, there is inevitably some uncertainty about the cross-cultural equivalence of the items used to assess stigma. We did a blind, independent back-translation of the embarrassment item and found high equivalence with the original version in all countries except France, where there was some ambiguity in meaning. This may explain the relatively high prevalence of embarrassment in that country (the prevalence of perceived stigma in France was intermediate). Fourth, schizophrenia and other psychotic mental disorders associated with high levels of perceived stigma were not included in our study. Therefore we may have underestimated the prevalence of stigma and its association with mental disorders. Underestimation of stigma could also occur because one consequence of embarrassment about a symptom or health problem may be not to report it to interviewers. This would render our estimates of prevalence of perceived stigma conservative. Finally, it might be argued that the high association of stigma with mental disorders is due to the fact that self-perceived embarrassment and discrimination are a symptom of psychopathology rather than the consequence of mental disorders. However, there is evidence that stigma persists after the alleviation of psychological symptoms(28). In addition, we recognize that stigma can also be relevant for families, friends, and even health care providers of people with stigmatizing conditions. But the investigation of these instances is beyond the scope of our current investigation.
To our knowledge, these are the first international, population-based results on the relationship between mental disorders and stigma. In general, our findings are consistent with prior research, which had used quite different methods and populations from those employed in the World Mental Health Surveys(4;7;8). Individuals reporting stigma were more frequently male and had lower education than those not reporting stigma. These characteristics have been associated with a lower use of the health services for mental disorders(29). It has been pointed out that stigma has negative behavioural consequences, such as not seeking help when it is needed(4). It is therefore important to reduce stigma to diminish the burden of mental disorders. Stigma reducing efforts might specifically consider the male and the lower educated individuals with mental disorders.
We found considerable cross-country variation in the prevalence of perceived stigma among persons with significant activity limitations.. In particular, perceived stigma was more common in developing countries. This seems to contradict the limited pre-existing reports(30) but results might be not strictly comparable. But the strong association of mental disorders with stigma was similar in both types of countries. To our knowledge, there are not prior cross-national studies of persons experiencing stigma to put these findings in context. One international study did investigate the attitudes of the general public towards stigma and social distance in reference to other individuals with mental disorders(31). That study showed that stigmatizing attitudes towards people with mental disorders were common in different countries. If general public attitudes against mental disorders are similar, in zones with a high prevalence of perceived stigma such as Ukraine, Shanghai, or Israel there is a pressing need for programs to address stigma. Across all countries, the high prevalence of perceived stigma associated with mental disorders should be taken into account when caring for individuals with mental disorders.
Our finding that perceived stigma is common among persons with significant activity limitations in general, and among persons with mental disorders in particular have significant implications. First, this suggests that health care providers should be aware that individuals with significant health problems, particularly those with mental disorders, are likely to experience embarrassment about their health condition and to perceive discrimination on the basis of their health condition. This is especially prevalent among individuals with comorbid mood and anxiety disorders. Also, more research is needed on the whole spectrum of social exclusion among those suffering from mental disorders. Finally, our results also indicate that it may be of interest to investigate social, cultural and health services characteristics that differentiate countries in which patients feel less excluded from countries in which patients are more likely to report perceived stigma.
Significant Outcomes
Perceived stigma is strongly associated to common mental disorders, particularly to comorbid mood and anxiety.
Although perceived stigma is more frequent, its association with mental disorders is universal in the developing countries considered in our study.
Special efforts to alleviate stigma are needed for individuals with common mental disorders.
Noteworthy Limitations
Only two items (health-related embarrassment and discrimination) were used to assess perceived stigma.
Perceived stigma was assessed only to individuals with significant disability in the previous month.
No information about psychotic disorders, typically associated with high levels of stigma, was included in our study
Acknowledgements
The surveys included in this report were carried out in conjunction with the World Health Organization World Mental Health (WMH) Survey Initiative. We thank the WMH staff for assistance with instrumentation, fieldwork, and data analysis. These activities were supported by the United States National Institute of Mental Health (R01MH070884), the John D. and Catherine T. MacArthur Foundation, the Pfizer Foundation, the US Public Health Service (R13-MH066849, R01-MH069864, and R01 DA016558), the Fogarty International Center (FIRCA R01-TW006481), the Pan American Health Organization, Eli Lilly and Company, Ortho-McNeil Pharmaceutical, Inc., GlaxoSmithKline, and Bristol-Myers Squibb. A complete list of WMH publications can be found at http://www.hcp.med.harvard.edu/wmh/. The Mexican National Comorbidity Survey (MNCS) is supported by The National Institute of Psychiatry Ramon de la Fuente (INPRFMDIES 4280) and by the National Council on Science and Technology (CONACyT-G30544- H), with supplemental support from the PanAmerican Health Organization (PAHO). The Lebanese survey is supported by the Lebanese Ministry of Public Health, the WHO (Lebanon) and unrestricted grants from Janssen Cilag, Eli Lilly, GlaxoSmithKline, Roche, Novartis and anonymous donations. The ESEMeD project was funded by the European Commission (Contracts QLG5-1999-01042; SANCO 2004123), the Piedmont Region (Italy), Fondo de Investigación Sanitaria, Instituto de Salud Carlos III, Spain (FIS 00/0028), Ministerio de Ciencia y Tecnología, Spain (SAF 2000-158-CE), Departament de Salut, Generalitat de Catalunya, Spain, and other local agencies and by an unrestricted educational grant from GlaxoSmithKline. The Chinese World Mental Health Survey Initiative is supported by the Pfizer Foundation. The Colombian National Study of Mental Health (NSMH) is supported by the Ministry of Social Protection, with supplemental support from the Saldarriaga Concha Foundation. The Israel National Health Survey is funded by the Ministry of Health with support from the Israel National Institute for Health Policy and Health Services Research and the National Insurance Institute of Israel. The World Mental Health Japan (WMHJ) Survey is supported by the Grant for Research on Psychiatric and Neurological Diseases and Mental Health (H13-SHOGAI-023, H14-TOKUBETSU-026, H16-KOKORO-013) from the Japan Ministry of Health, Labour and Welfare. The New Zealand Mental Health Survey (NZMHS) is supported by the New Zealand Ministry of Health, Alcohol Advisory Council, and the Health Research Council. The Nigerian Survey of Mental Health and Wellbeing (NSMHW) is supported by the WHO (Geneva), the WHO (Nigeria), and the Federal Ministry of Health, Abuja, Nigeria. The South Africa Stress and Health Study (SASH) is supported by the US National Institute of Mental Health (R01-MH059575) and National Institute of Drug Abuse with supplemental funding from the South African Department of Health and the University of Michigan. The Ukraine Comorbid Mental Disorders during Periods of Social Disruption (CMDPSD) study is funded by the US National Institute of Mental Health (RO1-MH61905). The US National Comorbidity Survey Replication (NCS-R) is supported by the National Institute of Mental Health (NIMH; U01-MH60220) with supplemental support from the National Institute of Drug Abuse (NIDA), the Substance Abuse and Mental Health Services Administration (SAMHSA), the Robert Wood Johnson Foundation (RWJF; Grant 044708), and the John W. Alden Trust.
Contributor Information
Jordi Alonso, Email: jalonso@imim.es.
Andrea Buron, Email: aburon@imas.imim.es.
Ronny Bruffaerts, Email: ronny.bruffaerts@uz.kuleuven.ac.be.
Yanling He, Email: heyl2001@yahoo.com.cn.
José Posada-Villa, Email: latos98@yahoo.com.
Jean-Pierre Lepine, Email: jean-pierre.lepine@lrb.aphp.fr.
Mattias C. Angermeyer, Email: angermeyer@aon.at.
Daphna Levinson, Email: daphna.levinson@moh.health.gov.il.
Giovanni de Girolamo, Email: giovanni.degirolamo@ausl.bologna.it.
Hisateru Tachimori, Email: tachi@ncnp-k.go.jp.
Zeina N. Mneimneh, Email: zeinam@umich.edu.
Ma Elena Medina-Mora, Email: medinam@imp.edu.mx.
Johan Ormel, Email: J.Ormel@med.umcg.nl.
Kate Margaret Scott, Email: kate.scott@otago.ac.nz.
Oye Gureje, Email: ogureje@comui.edu.ng.
Josep Maria Haro, Email: jmharo@sjd-ssm.com.
Semyon Gluzman, Email: upa2@i.com.ua.
Sing Lee, Email: singlee@cuhk.edu.hk.
Gemma Vilagut, Email: gvialgut@imim.es.
Ronald C. Kessler, Email: kessler@hcp.med.harvard.edu.
Michael Von Korff, Email: vonkorff.m@ghc.org.
References
- 1.World Health Organization. The World Health Report 2001 Mental Health: New understanding, new hope. Geneve: WHO Library Cataloguing; 2001
- 2.Wait S, Harding E. Moving to social integration of people with severe mental illness: from policy to practice. United Kingdom: International Longevity Centre; 2006. [Google Scholar]
- 3.Wittchen HU, Jacobi F. Size and burden of mental disorders in Europe--a critical review and appraisal of 27 studies. Eur Neuropsychopharmacol. 2005;15(4):357–376. doi: 10.1016/j.euroneuro.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 4.Rusch N, Angermeyer MC, Corrigan PW. Mental illness stigma: concepts, consequences, and initiatives to reduce stigma. Eur Psychiatry. 2005;20(8):529–539. doi: 10.1016/j.eurpsy.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 5.Sirey JA, Bruce ML, Alexopoulos GS, Perlick DA, Friedman SJ, Meyers BS. Stigma as a barrier to recovery: Perceived stigma and patient-rated severity of illness as predictors of antidepressant drug adherence. Psychiatr Serv. 2001;52(12):1615–1620. doi: 10.1176/appi.ps.52.12.1615. [DOI] [PubMed] [Google Scholar]
- 6.Wahl OF. Mental health consumers' experience of stigma. Schizophr Bull. 1999;25(3):467–478. doi: 10.1093/oxfordjournals.schbul.a033394. [DOI] [PubMed] [Google Scholar]
- 7.Corrigan PW, River LP, Lundin RK, Wasowki KU, Campion J, Mathisen J, et al. Stigmatizing attributions about mental illness. J Community Psychol. 2000;28(1):91–102. [Google Scholar]
- 8.Corrigan P, Thompson V, Lambert D, Sangster Y, Noel JG, Campbell J. Perceptions of discrimination among persons with serious mental illness. Psychiatr Serv. 2003;54(8):1105–1110. doi: 10.1176/appi.ps.54.8.1105. [DOI] [PubMed] [Google Scholar]
- 9.Pescosolido BA, Monahan J, Link BG, Stueve A, Kikuzawa S. The public's view of the competence, dangerousness, and need for legal coercion of persons with mental health problems. Am J Public Health. 1999;89(9):1339–1345. doi: 10.2105/ajph.89.9.1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Perry BL, Pescosolido BA, Martin JK, McLeod JD, Jensen PS. Comparison of public attributions, attitudes, and stigma in regard to depression among children and adults. Psychiatr Serv. 2007;58(5):632–635. doi: 10.1176/ps.2007.58.5.632. [DOI] [PubMed] [Google Scholar]
- 11.Thornicroft G, Rose D, Kassam A, Sartorius N. Stigma: ignorance, prejudice or discrimination? Br J Psychiatry. 2007;190:192–193. doi: 10.1192/bjp.bp.106.025791. [DOI] [PubMed] [Google Scholar]
- 12.Sartorius N. Lessons from a 10-year global programme against stigma and discrimination because of an illness. Psychol Health Med. 2006;11(3):383–388. doi: 10.1080/13548500600595418. [DOI] [PubMed] [Google Scholar]
- 13.Sartorius N, Schultze H. Reducing the stigma of mental illness: a report from a global association. Cambridge: Cambridge University Press; 2005. [Google Scholar]
- 14.Corrigan PW. Target-specific stigma change: a strategy for impacting mental illness stigma. Psychiatr Rehabil J. 2004;28(2):113–121. doi: 10.2975/28.2004.113.121. [DOI] [PubMed] [Google Scholar]
- 15.Link BG, Phelan JC. Conceptualizing Stigma. Annu Rev Sociol. 2001;27:363–385. [Google Scholar]
- 16.Goffman E. Stigma. Notes on the management of spoiled identity. New Jersey: Prentice-Hall; 1963. [Google Scholar]
- 17.Yang L, Kleinman A, Link B, Phelan JC, Good B, Lee S. Culture and Stigma: Adding Moral Experience to Stigma Theory. Soc Sci Med. doi: 10.1016/j.socscimed.2006.11.013. In press. [DOI] [PubMed] [Google Scholar]
- 18.Van Brakel WH. Measuring health-related stigma--a literature review. Psychol Health Med. 2006;11(3):307–334. doi: 10.1080/13548500600595160. [DOI] [PubMed] [Google Scholar]
- 19.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13(2):93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Haro JM, Arbabzadeh-Bouchez S, Brugha TS, de Girolamo G, Guyer ME, Jin R, et al. Concordance of the Composite International Diagnostic Interview Version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health surveys. Int J Methods Psychiatr Res. 2006;15(4):167–180. doi: 10.1002/mpr.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 22.NCHS. Evaluation of National Health Interview Survey diagnostic reporting. Vital Health Stat 2. 1994;120:1–116. [PubMed] [Google Scholar]
- 23.Epping-Jordan J, Ustun T. The WHODAS II: levelling the playing field for all disorders. WHO Bulletin of Mental Health. 2000 Available from: URL: http://www.who.int/icidh/who.das/generalinfo.html.
- 24.Wolter KM. Introduction to Variance Estimation. New York: Springer-Verlag; 1985. [Google Scholar]
- 25.Research Triangle Institute. SUDAAN Language Manual, Release 9.0. North Carolina: Research Triangle Institute, NC; 2004. Available from: URL: http://www.rti.org/sudaan. [Google Scholar]
- 26.Link BG, Cullen FT, Struening E, Shrout PE, Dohrenwend BP. A Modified Labeling Theory Approach to Mental Disorders: An Empirical Assessment. Am Sociol Rev. 1989;54:400–423. [Google Scholar]
- 27.Bowling A. Just one question: If one question works, why ask several? J Epidemiol Community Health. 2005;59(5):342–345. doi: 10.1136/jech.2004.021204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Link BG, Struening EL, Rahav M, Phelan JC, Nuttbrock L. On stigma and its consequences: evidence from a longitudinal study of men with dual diagnoses of mental illness and substance abuse. J Health Soc Behav. 1997;38(2):177–190. [PubMed] [Google Scholar]
- 29.Alonso J, Codony M, Kovess-Masfety V, Angermeyer MC, Katz SJ, Haro JM, et al. Population level of unmet need for mental health care in Europe. Results from the European Study of Epidemiology of Mental Disorders (ESEMeD) Project. Br J Psychiatry. 2007;190:299–306. doi: 10.1192/bjp.bp.106.022004. [DOI] [PubMed] [Google Scholar]
- 30.Corrigan PW, Watson AC. Understanding the impact of stigma on people with mental illness. World Psychiatry. 2002;1(1):16–20. [PMC free article] [PubMed] [Google Scholar]
- 31.Dietrich S, Beck M, Bujantugs B, Kenzine D, Matschinger H, Angermeyer MC. The relationship between public causal beliefs and social distance toward mentally ill people. Aust N Z J Psychiatry. 2004;38(5):348–354. doi: 10.1080/j.1440-1614.2004.01363.x. [DOI] [PubMed] [Google Scholar]