Abstract
Objective
To determine the fraction of individuals with high total serum cholesterol who get diagnosed and effectively treated in eight high- and middle-income countries.
Methods
Using data from nationally representative health examination surveys conducted in 1998–2007, we studied a probability sample of 79 039 adults aged 40–79 years from England, Germany, Japan, Jordan, Mexico, Scotland, Thailand and the United States of America. For each country we calculated the prevalence of high total serum cholesterol (total serum cholesterol ≥ 6.2 mmol/l or ≥ 240 mg/dl) and the mean total serum cholesterol level. We also determined the fractions of individuals being diagnosed, treated with cholesterol-lowering medication and effectively controlled (total serum cholesterol < 6.2 mmol/l or < 240 mg/dl).
Findings
The proportion of undiagnosed individuals was highest in Thailand (78%; 95% confidence interval, CI: 74–82) and lowest in the United States (16%; 95% CI: 13–19). The fraction diagnosed but untreated ranged from 9% in Thailand (95% CI: 8–11) to 53% in Japan (95% CI: 50–57). The proportion being treated who had attained evidence of control ranged from 4% in Germany (95% CI: 3–5) to 58% in Mexico (95% CI: 54–63). Time series estimates showed improved control of high total serum cholesterol over the past two decades in England and the United States.
Conclusion
The percentage of people with high total serum cholesterol who are effectively treated remains small in selected high- and middle-income countries. Many of those affected are unaware of their condition. Untreated high blood cholesterol represents a missed opportunity in the face of a global epidemic of chronic diseases.
Resumé
Objectif
Déterminer la proportion d’individus souffrant d’un taux de cholestérol sérique total élevé, qui font l’objet d’un diagnostic et qui reçoivent un traitement efficace dans huit pays à revenu moyen ou élevé.
Méthodes
En nous appuyant sur des données provenant d’enquêtes sur les examens de santé, représentatives du niveau national et menées de 1998 à 2007, nous avons étudié un échantillon aléatoire de 79 039 adultes âgés de 40 à 79 ans originaires d’Angleterre, d’Allemagne, du Japon, de Jordanie, du Mexique, d’Écosse, de Thaïlande et des États-Unis d’Amérique. Pour chacun de ces pays, nous avons calculé la prévalence de cholestérol sérique total élevé (cholestérol sérique total ≥ 6,2 mmol/l ou ≥ 240 mg/dl) et le niveau moyen de cholestérol sérique total. Nous avons également déterminé la proportion des individus ayant fait l’objet d’un diagnostic et ayant reçu un traitement hypocholestérolémiant effectivement contrôlé (cholestérol sérique total < 6,2 mmol/l ou < 240 mg/dl).
Résultats
La proportion des individus non diagnostiqués était la plus forte en Thaïlande (78%; 95% intervalle de confiance, IC: 74–82) et la plus faible aux États-Unis (16%; 95% IC: 13–19). Le pourcentage de personnes ayant fait l’objet d’un diagnostic, mais non d’une thérapie, était compris entre 9% en Thaïlande (95% IC: 8–11) et 53% au Japon (95% IC: 50–57). La proportion des individus sous traitement ayant obtenu une attestation de contrôle variait de 4% en Allemagne (95% IC: 3–5) à 58% au Mexique (95% IC: 54–63). Les estimations des séries chronologiques ont témoigné d’un meilleur contrôle de l’hypercholestérolémie en Angleterre et aux États-Unis lors des deux dernières décennies.
Conclusion
Le pourcentage de personnes présentant un cholestérol sérique total élevé et qui sont effectivement traitées demeure faible dans les pays à revenu moyen ou élevé retenus. Bon nombre des personnes atteintes n’ont pas connaissance de leur état. Un taux de cholestérol plasmatique élevé non soigné représente une opportunité manquée face à une épidémie mondiale de maladies chroniques.
Resumen
Objetivo
Determinar la fracción de individuos diagnosticados con una concentración sérica elevada de colesterol total y que hayan recibido un tratamiento eficaz en ocho países de ingresos medios y elevados.
Métodos
Con los datos de las encuestas de vigilancia sanitaria, representativas a nivel nacional y realizadas entre 1998 y 2007, se estudió una muestra basada en la probabilidad de 79 039 adultos con edades comprendidas entre los 40 y 79 años en Alemania, Escocia, Estados Unidos de América, Inglaterra, Japón, Jordania, México y Tailandia. Se calculó la prevalencia de la hipercolesterolemia (colesterol sérico total ≥6,2 mmol/l o ≥240 mg/dl) y el nivel medio de colesterol sérico total para cada país. También se determinaron las fracciones de individuos que fueron diagnosticados y tratados con hipocolesterolemiantes y controlados eficazmente (colesterol sérico total <6,2 mmol/l o <240 mg/dl).
Resultados
La proporción de individuos sin diagnosticar fue mayor en Tailandia (78%; intervalo de confianza del 95%, IC: 74-82) y menor en los Estados Unidos de América (16%; IC del 95%: 13-19). La fracción de personas diagnosticadas que no recibieron tratamiento varió entre el 9% de Tailandia (IC del 95%: 8-11) y el 53% de Japón (IC del 95%: 50-57). La proporción de pacientes en tratamiento, con resultados que evidenciaban haber conseguido controlar la enfermedad, osciló entre el 4% en Alemania (IC del 95%: 3-5) y el 58% en Japón (IC del 95%: 54-63). Las estimaciones de las series temporales mostraron una mejoría en el control de las concentraciones de colesterol sérico total en las últimas dos décadas en Inglaterra y los Estados Unidos.
Conclusión
El porcentaje de personas con concentraciones elevadas de colesterol sérico total que reciben un tratamiento eficaz sigue siendo pequeño en los países seleccionados de ingresos medios y elevados. Muchos de los afectados no son conscientes de su enfermedad. La hipercolesterolemia sin tratar supone una oportunidad perdida, a tenor de la epidemia mundial de las enfermedades crónicas.
ملخص
الغرض
تحديد نسبة المصابين بارتفاع الكوليستيرول المصلي الكلي وتم تشخيصهم ومعالجتهم بفعالية في ثمانية بلدان مرتفعة ومتوسطة الدخل.
الطريقة
باستخدام معطيات فحص المسوحات الصحية الممثلة للسكان والتي أجريت في الأعوام 1998-2007، درس الباحثون عينة احتمالية مكونة من 79039 راشداً في عمر 40-79 سنة من إنكلترا، وألمانيا، واليابان، والأردن، والمكسيك، وسكوتلاند، وتايلاند، والولايات المتحدة الأمريكية. وحسب الباحثون، لكل بلد، معدل انتشار ارتفاع الكوليستيرول المصلي الكلي (أي أن يكون الكوليستيرول المصلي الكلي أعلى من أو يساوي 6.2 ملي مول باللتر أو أعلى من أو يساوي 240 ملي غرام بالديسي لتر) وحسبوا متوسط مستوى الكوليستيرول المصلي الكلي. كما حددوا نسبة من جرى تشخيصهم، وإعطاؤهم أدوية خفض الكوليستيرول، وجرى تضبيطه لهم بفعالية (أي أصبح الكوليستيرول المصلي الكلي اقل من 6.2 ملي مول باللتر أو أقل من 240 ملي غرام بالديسي لتر).
النتائج
كانت أعلى نسبة لمن لم يتم تشخيصهم في تايلاند (وبلغت 78%؛ فاصلة الثقة 95%: 7§5-82)، وكانت أقل نسبة في الولايات المتحدة (16%؛ فاصلة الثقة 95%: 13-19). وتراوحت نسبة من تم تشخيصهم ولم يتم علاجهم من 9% في تايلاند (فاصلة الثقة 95%: 8-11) إلى 53% في اليابان (فاصلة الثقة 95%: 50-57). وتراوحت نسبة من عولجوا واستُدِل على تضبيط المستوى لديهم من 4% في ألمانيا (فاصلة الثقة 95%: 3-5) إلى 58% في المكسيك (فاصلة الثقة 95%: 54-63). وأوضحت تقديرات التسلسل الزمني تحسناً في تضبيط ارتفاع الكوليستيرول المصلي الكلي خلال العقدين الأخيرين في إنكلترا والولايات المتحدة.
الاستنتاج
مازالت النسبة المئوية للمصابين بارتفاع الكوليستيرول المصلي الكلي وعولجوا بفعالية نسبة صغيرة في البلدان المرتفعة والمتوسطة الدخل التي جرى انتقاؤها. ولا يدرك كثير من المصابين شيئاً عن حالتهم. ويشكّل ارتفاع كوليستيرول الدم غير المعالج فرصةً مهدرةً في التصدي للجائحة العالمية للأمراض المزمنة.
Резюме
Цель
Определить долю больных с высоким общим холестерином сыворотки, которым поставлен диагноз заболевания и предоставляется эффективное лечение, в восьми странах с высоким и средним доходом.
Методы
Используя данные национально-репрезентативных опросов по изучению здоровья, проведенных в 1998–2007 гг., мы исследовали вероятностную выборку из 79 039 взрослых в возрасте 40–79 лет из Англии, Германии, Иордании, Мексики, Соединенных Штатов Америки, Таиланда, Шотландии и Японии. Для каждой страны мы вычислили распространенность высокой концентрации общего холестерина в сыворотке крови (общий холестерин сыворотки ≥ 6.2 ммоль/л или ≥ 240 мг/дл) и средний уровень общего холестерина сыворотки. Мы также определили процентные доли больных, которым был поставлен диагноз заболевания, проводилась терапия медикаментами, снижающими уровень холестерина, и у которых были достигнуты положительные результаты лечения (общий холестерин сыворотки < 6,2 ммоль/л или < 240 мг/дл).
Результаты
Доля больных, которым не был поставлен диагноз, была выше всего в Таиланде (78%; 95%-ный доверительный интервал, ДИ: 74–82) и ниже всего в США (16%; 95% ДИ: 13–19). Доля больных с поставленным диагнозом, не получавших лечения, колебалась от 9% в Таиланде (95% ДИ: 8–11) до 53% в Японии (95% ДИ: 50–57). Доля больных, получавших лечение, у которых достигнуты положительные результаты, колебалась от 4% в Германии (95% ДИ: 3–5) до 58% в Мексике (95% ДИ: 54–63). Временные статистические ряды оценок показали, что за последние два десятилетия контроль высокой концентрации общего холестерина сыворотки улучшился в Англии и США.
Вывод
В выбранных странах с высоким и средним доходом процентная доля людей с высокой концентрацией общего холестерина сыворотки, у которых достигнуты положительные результаты лечения, остается незначительной. Многие больные не знают о своем состоянии. Непредоставление лечения больным с высокой концентрацией холестерина в крови выглядит упущенной возможностью ввиду глобальной эпидемии хронических болезней.
摘要
目的
旨在确定八个中高收入国家患有高血清总胆固醇的个人获得诊断和有效治疗的比例。
方法
我们运用1998到2007年间进行的全国典型健康体检调查得到的数据,研究了来自英格兰、德国、日本、约旦、墨西哥、苏格兰、泰国和美国79 039名40-79岁成年人组成的概率样本。对于每一国家,我们计算了高血清总胆固醇的流行程度(血清总胆固醇≥6.2 mmol/l或≥240 mg/dl)和平均血清总胆固醇的水平。我们还确定了得到诊断、用降胆固醇药物进行治疗和病情得到有效控制(血清总胆固醇< 6.2 mmol/l或< 240 mg/dl)的个人比例。
结果
未诊断个人的比例泰国最高(78%,95%置信区间CI:74-82),美国最低(16%,95%置信区间CI:13-19)。确诊但未治疗的比例从泰国的9%(95%置信区间CI:8-11)到日本的53%(95%置信区间CI:50-57)。接受治疗并且得到明显控制的比例从德国的4%(95%置信区间CI:3-5)到墨西哥的58%(95%置信区间CI:54-63)。时间序列估算显示过去的二十年中英格兰和美国的高血清总胆固醇控制得到改善。
结论
在所选定的中高收入国家中,患有高血清总胆固醇并且得到有效治疗的人群的比例仍然很小。很多患者并未察觉他们自身的病情。在全球流行的慢性病面前,未经治疗的高血胆固醇代表着错失良机。
Introduction
Cardiovascular disease caused over 18 million deaths in the world in 2005.1 Of these deaths, eight million (44%) occurred in people under 60 years of age and 80% took place in low- and middle-income countries.1,2 In response, the World Health Organization (WHO) has set a goal of reducing the global rate of death from chronic diseases by 2% a year up to 2015.3 This goal rests on the recognition that throughout the world deaths from cardiovascular causes are attributable to a few modifiable risk factors, most importantly high blood pressure, smoking and high total serum cholesterol.4,5
Lowering total serum cholesterol levels is an ideal strategy for reducing the burden of cardiovascular disease. Potent, safe and highly effective cholesterol-lowering medication is available in the form of statins,6 and there are many low-cost methods for identifying those who need to lower their serum cholesterol.7,8 Modelling studies suggest that lowering total serum cholesterol, either by treating elevated total serum cholesterol alone or by managing multiple risk factors, is cost-effective in many low- and middle-income countries.9
While the use of cholesterol-lowering medication is considered important in reducing the burden of cardiovascular disease, differences in the way various health systems are implementing this strategy are not well understood.10,11 Comparing individual studies is difficult because the definition of a high blood cholesterol level varies among studies and, until recently, population-wide data has been lacking for many places. The growing number of national health examination surveys that measure total serum cholesterol provides an opportunity to ascertain how well cholesterol-lowering medication is being delivered to populations at risk of cardiovascular disease.12 Using microdata from multiple national health examination surveys in eight countries, we have estimated the proportion of the population diagnosed with high total serum cholesterol, on treatment with cholesterol-lowering medication, and with evidence of therapeutic control.
Methods
Search strategy
In 2008, we systematically searched the following for nationally representative health examination surveys performed since 1997: Google Scholar and PubMed (using relevant keywords), the WHO Global Infobase,13 the WHO STEPwise approach to surveillance database14 and the European Health Interview Surveys and Health Examination Surveys database.15 We identified surveys that measured total serum cholesterol and that asked respondents if they used cholesterol-lowering medication. Individual-level data was downloaded from agency web sites when publicly available or obtained through formal application procedures and by contacting study authors.
Survey characteristics
The following national health examination surveys met our criteria: Germany (1998), Japan (2000), Scotland (2003), Thailand (2004), the United States of America (2005–2006), England (2006), Mexico (2006) and Jordan (Jordan Ministry of Health, unpublished data, 2007).16–22 Our study included five high-income countries, one upper-middle-income country and two lower-middle-income countries. Table 1 shows the year in which the surveys were conducted, the questions used in these surveys for the self-reported diagnosis of high total serum cholesterol and the self-reported use of cholesterol-lowering medication. Most surveys did not differentiate between prescribed and over-the-counter medications or between statin and non-statin medication.
Table 1. Assessment of high total serum cholesterol and use of cholesterol-lowering drugs among respondents of national health examination surveys in eight countries, 1998–2007.
| Countrya | Survey year | Diagnostic question | Determination of medication use |
|---|---|---|---|
| Germany | 1998 | The last time your blood cholesterol level was measured, were you told it was high? | Nurse manually reviews pills. |
| Japan | 2000 | Have you ever been told by a medical doctor that your serum cholesterol is high? | Do you take medication to lower total serum cholesterol? |
| Scotland | 2003 | Thinking about the last time your blood cholesterol level was measured, were you told it was higher than normal? | Nurse manually reviews pills. |
| Thailand | 2004 | Has a medical doctor told you that you had hypercholesterolaemia in the last year? | Have you used a cholesterol-lowering drug in the last 2 weeks? |
| United States | 2005–06 | Have you ever been told by a doctor or other health professional that your blood cholesterol level was high? | Have you ever been told by a doctor or other health professional to take a prescribed medicine to lower your blood cholesterol? Are you now following this advice to take prescribed medicine? |
| England | 2006 | Thinking about the last time your blood cholesterol level was measured, were you told it was high? | Nurse manually reviews pills? |
| Mexico | 2006 | Has any doctor said you have high cholesterol? | Have you been treated for high cholesterol with drugs? |
| Jordan | 2007 | Have you ever been told by a health facility that your blood cholesterol is high? | Are you currently taking medicine for your high blood cholesterol? |
a These countries belong to different World Bank income categories.
Enzyme-based automated methods were used in all surveys to measure total serum cholesterol levels. The guidelines of the United States Centers for Disease Control and Prevention and WHO were followed in all countries except Germany and Thailand, where national guidelines were observed. Blood tests were performed in a central laboratory in all countries except Thailand, which relied on five regional university laboratories.
Definitions
For each country, we calculated mean total serum cholesterol and the prevalence of high total serum cholesterol, conservatively defined as ≥ 6.2 millimoles per litre (mmol/l) (240 milligrams per decilitre, mg/dl), for adults from 40 to 79 years of age. To determine whether countries are delivering cholesterol-lowering medication and effectively lowering blood cholesterol levels, we assigned all individuals with high total serum cholesterol to one of four mutually exclusive categories: undiagnosed, diagnosed but untreated, treated but not controlled, and treated and controlled. A person considered “undiagnosed” was one who reported never having been given a diagnosis of high total serum cholesterol but whose total serum cholesterol as measured during the survey was ≥ 6.2 mmol/l. A person considered “diagnosed but untreated” was one who reported having been diagnosed with high blood cholesterol, who had a total serum cholesterol level ≥ 6.2 mmol/l during the survey and who did not report using cholesterol-lowering medication. A person considered “treated but not controlled” was one who reported using cholesterol-lowering medication but whose total serum cholesterol during the survey was ≥ 6.2 mmol/l. A person considered “treated and controlled” was one who reported using cholesterol-lowering medication and whose total serum cholesterol during the survey was < 6.2 mmol/l.
Statistical analysis
We used the svy command in Stata, release 10 (StataCorp LP, College Station, United States of America) to analyse individual-level data taking into account the complex survey design and applying sample weights for each survey. Missing data were handled by listwise deletion.23 We estimated the total population with high total serum cholesterol in each country (including individuals using lipid-lowering medication) by multiplying the age- and sex-specific prevalence figures from each survey by the age- and sex-specific population estimates from the United Nations Population Division for each survey year.24 To standardize our figures for medication delivery by age and sex we used the population aged 40–79 years with high total serum cholesterol pooled across all surveys. This was done to ensure a standard population that reflected the rightward shift in age structure of the population with high total serum cholesterol levels. We converted total serum cholesterol levels from milligrams per decilitre to millimoles per litre, as prescribed by the International System of Units, using a conversion factor of 0.02586.25
Sensitivity analyses were performed for different definitions of high total serum cholesterol, including total serum cholesterol values of 5.0, 5.2 and 6.5 mmol/l.
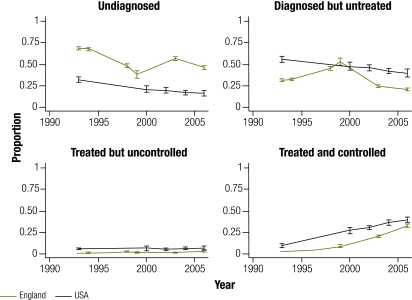
For countries with sufficient data (England and the United States) we compared secular trends in diagnosis, medication coverage and control. Data from the National Health and Nutrition Examination Survey III (NHANES) of the United States,20 conducted from 1988 to 1994, are shown in Fig. 1 as a time point for 1993 and treated as a comparator for the 1993 Health Survey for England.21 To account for possible variation in age structure between these countries over time, we age-standardized these time series cross-sectional rates to the population of the United States aged 40–79 with high total serum cholesterol in 2006.
Fig. 1.
Diagnosis, coverage and control of high total serum cholesterol in Englanda and the United States of America (USA) among the population aged 40–79 years, 1993–2006
a Time series cross-sectional rates were sex- and age-standardized to the hypercholesterolaemic population aged 40–79 years of the United States. The United States National Health and Nutrition Examination Survey III, represented here as a time point for 1993, was conducted from 1988 to 2004.
This analysis received a certificate of exemption from the Institutional Review Board at the University of Washington in Seattle, United States (HSD No. 35660).
Results
The eight surveys included in this analysis provided a representative probability sample from a multi-country population of approximately 147 000 000 individuals with high total serum cholesterol. Table 2 shows, for each survey, the country in which it was conducted, the country’s World Bank income class, sample size, mean total serum cholesterol and the size of the population with hypercholesterolaemia. We were unable to calculate measures of central tendency for the Mexican survey because total cholesterol < 3.88 mmol/l was reported as a level equal to 3.88 mmol/l in the data set.
Table 2. Mean total serum cholesterol in adults aged 40–79 years and number and fraction of these adults with high total serum cholesterol in eight countries belonging to different World Bank income categories.
| Country | Income category | Surveyed adults |
Total serum cholesterol in surveyed adults |
Total population aged 40–79 years with high total serum cholesterol |
|||||
|---|---|---|---|---|---|---|---|---|---|
| No. | Mean (mmol/l) | SD | No. | % | 95% CI | ||||
| Germany | High | 4285 | 6.46 | 0.02 | 41 000 000 | 61.6 | 59.0–64.2 | ||
| Japan | High | 6463 | 5.35 | 0.02 | 22 500 000 | 23.7 | 21.8–25.5 | ||
| Scotland | High | 5141 | 5.86 | 0.03 | 1 665 917 | 42.6 | 39.7–45.6 | ||
| Thailand | Lower middle | 28 899 | 5.34 | 0.04 | 10 600 000 | 27.7 | 25.0–30.3 | ||
| United States | High | 2662 | 5.26 | 0.02 | 46 700 000 | 23.7 | 21.4–26.0 | ||
| England | High | 8521 | 5.63 | 0.02 | 14 700 000 | 35.2 | 33.3–37.1 | ||
| Mexico | Upper middle | 21 262 | NA | NA | 9 003 425 | 19.2 | 17.3–21.2 | ||
| Jordan | Lower middle | 1806 | 5.06 | 0.07 | 696 212 | 30.4 | 24.5–36.2 | ||
CI, confidence interval; NA, not available; SD, standard deviation.
Data derived from national health examination surveys conducted from 1998 to 2007.
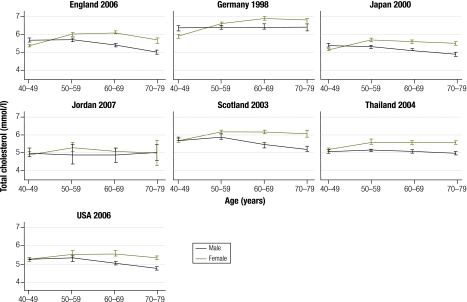
Mean total serum cholesterol ranged from 5.06 mmol/l (SD 0.07) in Jordan to 6.46 mmol/l (SD 0.02) in Germany. The prevalence of a total serum cholesterol ≥ 6.2 mmol/l or the use of cholesterol-lowering medication ranged from 19.2% (95% confidence interval, CI: 17.3–21.2) in Mexico to 61.6% (95% CI: 59.0–64.2) in Germany. Fig. 2 shows the mean total serum cholesterol levels and their 95% CIs, stratified by age and sex. Mean total serum cholesterol levels were significantly higher for younger men in England, Germany and Japan and for older women in England, Japan, Scotland, Thailand and the United States.
Fig. 2.
Mean total serum cholesterol, by age group and sex, in seven countries (Mexico excluded)a with different income levels, 1998–2007
USA, United States of America.
a Measures of central tendency for the Mexican survey were not calculated because a total cholesterol level < 3.88 mmol/l was reported as being equal to 3.88 mmol/l in the available survey data set.
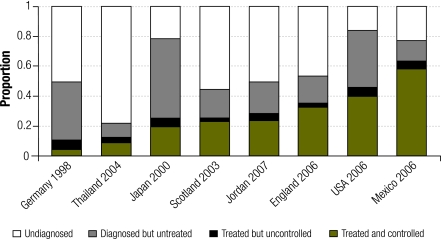
Diagnosis, treatment and control
Fig. 3 shows figures for medication coverage and control of high total serum cholesterol for all surveys. The proportion of people with undiagnosed high total serum cholesterol was highest in Thailand (78%; 95% CI: 74–82) and lowest in the United States (16%; 95% CI: 13–19). The proportion of individuals who were diagnosed but untreated ranged from 9% in Thailand (95% CI: 8–11) to 53% in Japan (95% CI: 50–57). The proportion of individuals who were treated but did not achieve control ranged from 2% in Scotland (95% CI: 1–3) to 6% in Germany (95% CI: 5–7). The proportion of individuals who were treated and controlled ranged from 4% in Germany (95% CI: 3–5) to 58% in Mexico (95% CI: 54–63). Within the treated population, the proportion of individuals under control was low in Germany (40.7%) but much higher in all other countries (range: 77.9–92.9%).
Fig. 3.
Diagnosis, treatment and control of high total serum cholesterol in the population aged 40–79 years in eight countries with different income levels, 1998–2007a
USA, United States of America.
a Treatment coverage figures were age- and sex-standardized to a pooled high-cholesterol population aged 40–79 years drawn from all surveys.
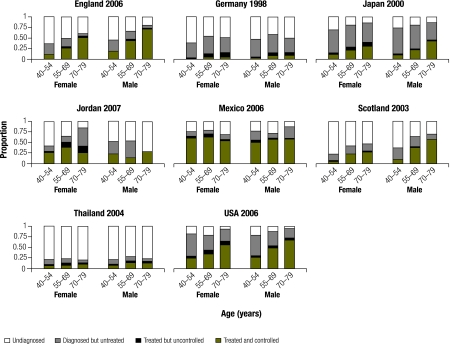
Fig. 4 shows the proportions of people who were diagnosed, treated with cholesterol-lowering medication and successfully controlled, stratified by age and sex. The prevalence of undiagnosed high total serum cholesterol decreased with age in England, Japan and Scotland in both men and women, and only in men in the United States. These differences reached statistical significance in England for both sexes, and in Scotland for men. The prevalence of undiagnosed high total serum cholesterol differed significantly by sex for all age categories in Scotland and for individuals 55–79 years of age in England. The proportion of individuals who were diagnosed but untreated decreased with age in all countries except Germany, Jordan and Mexico. The proportion of individuals who were treated and achieved evidence of control increased with age in England among men and women and in Japan, Scotland and the United States among men alone. Control rates differed significantly by sex for all age groups in England and for individuals 55–79 years of age in Scotland.
Fig. 4.
Diagnosis, treatment and control of high total serum cholesterol, by age group and sex, in eight countries with different income levels, 1998–2007
USA, United States of America.
Trends over time
Secular trends in England and the United States demonstrated a decline during the past two decades in the proportion of men and women with undiagnosed high total serum cholesterol (Fig. 1). In England, the decline in males was from 61.9% (95% CI: 59.5–64.2) to 42.4% (95% CI: 39.3–45.5), and in females it was from 75.1% (95% CI: 73.3–77) to 53% (95% CI: 50.2–56). Rates fell more gradually in the United States. In males, the proportion dropped from 30.4% (95% CI: 26.4–34.5) to 25.1% (95% CI: 18.2–32.1), and in females it fell from 33.0% (95% CI: 29.0–37.0) to 26.5% (95% CI: 20.6–32.5). In both countries, the proportion of individuals diagnosed but untreated decreased, whereas the proportion who achieved therapeutic control increased steadily. In England in 2006, 35.5% of men (95% CI: 32.8–38.3) and 25.7% of women (95% CI: 23.4–28.1) with high total serum cholesterol were on cholesterol-lowering medication and had achieved good control, as opposed to 0.6% of men (95% CI: 0.3–1.3) and 0.4% of women (95% CI: 0.1–0.7% in 1993. In the United States in 2006, 54.0% of men (95% CI: 47.6–60.4) and 49.7% of women (95% CI: 44.3–55.0) with high total serum cholesterol were on cholesterol-lowering medication and had evidence of control, as opposed to 10.8% of men (95% CI: 8.0–13.6) and 8.6% (95% CI: 6.7–10.6) of women in 1993. The proportion of individuals who were treated but uncontrolled remained essentially unchanged after 1993 in both England and the United States: 2.6% (95% CI: 1.9–3.2) and 9.1% (95% CI: 5.9–12.2), respectively.
Sensitivity analysis
The cut-off value of total serum cholesterol that we used to diagnose hypercholesterolaemia and to define therapeutic control (6.2 mmol/l) was highly conservative. In essence, we assumed that any elevated blood cholesterol level below this cut-off represented the effect of lipid-lowering medication among those who were on treatment for very high total serum cholesterol. As shown in Appendix A (available at: http://www.healthmetricsandevaluation.org/data/2010/national_health/Webappendix_1.pdf), when we dropped the cut-off value to 5.2 mmol/l, our estimated proportion of individuals on treatment who were adequately controlled decreased by approximately 50%. As expected, coverage estimates are highly sensitive to the definition of disease state and treatment goals.
Discussion
Our study reveals that in countries with different income levels, a large proportion of individuals who would benefit from cholesterol-lowering medication remain unaware of this opportunity to reduce their risk for cardiovascular disease, or they remain untreated despite being aware of their condition. For instance, the limited use of cholesterol-lowering medication in Jordan and Thailand is alarming because high serum cholesterol is common among adults in both countries. These findings support the growing recognition that cardiovascular diseases are not merely “diseases of affluence” and that some middle-income countries are beginning to face a double burden of both chronic and communicable diseases.26,27
Effective delivery of cholesterol-lowering medication has increased threefold in England and fivefold in the United States over the past two decades. Our analysis suggests that this is associated with the increased use of medication among the diagnosed population rather than an increase in the fraction of the population that is diagnosed. Thus, efforts to screen more people and make them aware of their high serum cholesterol levels have been less successful than efforts to deliver treatment to those who know they are hypercholesterolaemic.
England, in particular, appears to have made rapid gains in the therapeutic coverage and control of people with high serum cholesterol during a time when barriers to treatment have decreased. In the United Kingdom of Great Britain and Northern Ireland, patent protection for simvastatin expired in May 2003 and over-the-counter simvastatin became available in July 2004.28 This contrasts sharply with the situation in Thailand, where in 2004 simvastatin was found in fewer than 5% of pharmacies.29 The past decade has seen significant changes in the global availability of simvastatin in particular. There are now over 100 manufacturers of this potent cholesterol-lowering medication, including many in China and India.30 In 2007, the drug was added to the WHO’s list of essential medicines. In some regions, treatment with simvastatin (40 mg) and with lovastatin (20 mg) costs less than US$ 30 and US$ 3 per year, respectively.31 These changes have probably led to improved adherence to statins, as well as to broader screening and prescribing.
The guidelines for screening and for the treatment of people with high serum cholesterol show variations that warrant further mention. For instance, medication coverage and therapeutic control increase significantly with advancing age and are higher among males than among females in England and Scotland, where screening and treatment guidelines have remained, until recently, relatively conservative.32,33 In contrast, rapid gains in lowering serum cholesterol were seen in the United States following the publication of the 1993 Adult Treatment Panel recommendation to use low-density lipoprotein (LDL) as a primary measure of cholesterol and to target a level < 2.6 mmol/l (100 mg/dl) among those with elevated cardiovascular risk. Unfortunately, any analysis of the effect of treatment guidelines is confounded by the fact that physicians in certain countries have been shown to rely on differing guidelines, including those from other countries.34 Further work is required to determine the effect of cholesterol screening policy and of guidelines on the delivery of cholesterol-lowering medication.
Most surprising perhaps is the high medication coverage seen in Mexico. Although it is encouraging, its cause is unclear. The direct benefits of health reform efforts conducted in the past decade by the Mexican government have been difficult to establish.35 Cross-national comparisons among developing countries with similar disease burdens can reveal striking differences in health system investment. For example, Mexico and Thailand are similar in population size and in the prevalence of high serum cholesterol. However, Mexico invests more than twice as much as Thailand in physicians per capita, whereas Thailand spends twice as much as Mexico on medications.35 To further understand medication coverage in Mexico and indeed in all countries, more research into how health resources are allocated by governments to curb cardiovascular diseases is required.
Strengths and limitations
Our analysis is based on several nationally-representative surveys of individuals with high serum cholesterol. Previous multinational comparisons have relied on subnational surveys conducted around selected urban areas and may have overestimated true intervention coverage.36–39 Our results are in line with prior estimates from country-level surveys in Mexico and Germany.40,41
This analysis has several limitations. To assess diagnosis and medication use we relied on self-reported responses whose validity, reliability and comparability are unknown. All surveys enquired about a previous diagnosis of high blood cholesterol and medication use, but the phrasing of the questions was not identical. Available data often came from different time periods. Because it was not possible to adjust for these differences, comparisons across countries may be confounded. These issues highlight the need to standardize health examination surveys to allow for more robust comparisons across countries and more frequent comparisons across time. We had to limit our analysis to total serum cholesterol because this was the only biomarker common to all surveys. Total serum cholesterol is a reliable indicator of elevated blood lipid levels because it correlates highly (r > 0.9) with LDL but is less susceptible than LDL to the effects of recent meals.42 Despite this, total serum cholesterol measurements overestimate cardiovascular risk by ignoring the protective effect of high-density lipoprotein (HDL) in people with high total serum cholesterol.
Following previous cross-country comparisons of population levels of high total serum cholesterol, we defined high total serum cholesterol as a serum level of total cholesterol ≥ 6.2 mmol/l (240 mg/dl).43 This cut-off level is considerably higher than optimal, but it is one at which most guidelines would consider medication therapy appropriate. Thus, it allowed us to cover all individuals who could reasonably be expected to receive cholesterol-lowering medication. The association between blood cholesterol levels and cardiovascular risk is curvilinear and modified by the presence or absence of other risk factors. Thus, there is no biological threshold for conferring high risk from blood cholesterol levels.44
Recommendations
Programmes designed to achieve higher detection and control of high blood cholesterol should be developed and implemented. Dried blood spot technology offers a new and affordable approach to screening in low-income settings.45 At the same time, better chronic disease surveillance is needed to monitor and guide these programmes. The standardized chronic disease modules developed as part of WHO’s STEPwise approach to surveillance are a good example, and similar modules emphasizing medication delivery require broader adoption. Finally, surveys should be repeated at regular intervals so that countries can track their progress towards achieving health goals, as England and the United States are doing. These intervention coverage metrics will play an important role in reducing the burden of chronic diseases as global goals are increased beyond the current, highly conservative goal of a 2% decrease per year.
Conclusion
Our findings support the growing consensus that the global burden of cardiovascular disease, which is the leading cause of death in most countries, requires immediate action. The recent announcement of a Global Alliance for Chronic Disease is heartening and suggests that the global burden of cardiovascular diseases is beginning to be viewed with the same urgency formerly reserved for infectious diseases. Cholesterol-lowering medication is widely available, highly effective and can play an essential role in reducing cardiovascular disease around the world. Despite these facts, effective medication coverage for control of high cholesterol remains disappointingly low.
Acknowledgements
The analysis of Japan was based on data prepared for research projects supported by Grants-in-Aid for Scientific Research from the Japan Ministry of Health, Labour and Welfare (PI: Toshihiko Hasegawa; H12-iryo-002, H14-kenko-010 and H16-kenko-001). The Mexico data analysed in this publication is from the National Survey of Health and Nutrition 2006, designed and conducted by Mexico's National Institute of Public Health. The original creators, depositors and copyright holders of the England and Scotland data and the UK Data Archive bear no responsibility for this analysis. Crown copyright material is reproduced with the permission of the Controller of HMSO and the Queen's Printer for Scotland.
Funding:
This study was supported by funding to the Institute for Health Metrics and Evaluation from the Bill & Melinda Gates Foundation and the state of Washington, United States. The sponsor had no role in the study design, data gathering and analysis, or in the interpretation or writing of this report. The corresponding author had full access to all data and had final responsibility for the decision to submit for publication.
Competing interests:
None declared.
References
- 1.Strong K, Mathers C, Leeder S, Beaglehole R. Preventing chronic diseases: how many lives can we save? Lancet. 2005;366:1578–82. doi: 10.1016/S0140-6736(05)67341-2. [DOI] [PubMed] [Google Scholar]
- 2.Abegunde DO, Mathers CD, Adam T, Ortegon M, Strong K. The burden and costs of chronic diseases in low-income and middle-income countries. Lancet. 2007;370:1929–38. doi: 10.1016/S0140-6736(07)61696-1. [DOI] [PubMed] [Google Scholar]
- 3.Preventing chronic diseases: a vital investment: WHO global report Geneva: World Health Organization; 2005. [Google Scholar]
- 4.Ezzati M. Comparative quantification of health risks global and regional burden of disease attributable to selected major risk factors Geneva: World Health Organization; 2004. [Google Scholar]
- 5.Yusuf S, Hawken S, Ôunpuu S, Dans T, Avezum A, Lanas F, et al. INTERHEART Study Investigators Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–52. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 6.Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, et al. Cholesterol Treatment Trialists’ (CTT) Collaborators Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366:1267–78. doi: 10.1016/S0140-6736(05)67394-1. [DOI] [PubMed] [Google Scholar]
- 7.Mendis S, Lindholm LH, Mancia G, Whitworth J, Alderman M, Lim S, et al. World Health Organization (WHO) and International Society of Hypertension (ISH) risk prediction charts: assessment of cardiovascular risk for prevention and control of cardiovascular disease in low and middle-income countries. J Hypertens. 2007;25:1578–82. doi: 10.1097/HJH.0b013e3282861fd3. [DOI] [PubMed] [Google Scholar]
- 8.Gaziano TA, Young CR, Fitzmaurice G, Atwood S, Gaziano JM. Laboratory-based versus non-laboratory-based method for assessment of cardiovascular disease risk: the NHANES I Follow-up Study cohort. Lancet. 2008;371:923–31. doi: 10.1016/S0140-6736(08)60418-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murray CJL, Lauer JA, Hutubessy RCW, Niessen L, Tomijima N, Rodgers A, et al. Effectiveness and costs of interventions to lower systolic blood pressure and cholesterol: a global and regional analysis on reduction of cardiovascular-disease risk. Lancet. 2003;361:717–25. doi: 10.1016/S0140-6736(03)12655-4. [DOI] [PubMed] [Google Scholar]
- 10.Primatesta P, Poulter NR. Lipid levels and the use of lipid-lowering agents in England and Scotland. Eur J Cardiovasc Prev Rehabil. 2004;11:484–8. doi: 10.1097/00149831-200412000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Ford ES, Li C, Pearson WS, Zhao G, Mokdad AH. Trends in hypercholesterolemia, treatment and control among United States adults. Int J Cardiol. 2010;140:226–35. doi: 10.1016/j.ijcard.2008.11.033. [DOI] [PubMed] [Google Scholar]
- 12.Fisher G, Pappas G, Limb M. Prospects, problems, and prerequisites for national health examination surveys in developing countries. Soc Sci Med. 1996;42:1639–50. doi: 10.1016/0277-9536(95)00319-3. [DOI] [PubMed] [Google Scholar]
- 13.WHO Global InfoBase (Internet). Geneva: World Health Organization; 2010. Available from: https://apps.who.int/infobase/ [accessed 26 August 2010].
- 14.STEPwise approach to surveillance (STEPS) (Internet). Geneva: World Health Organization; 2010. Available from: http://www.who.int/chp/steps/en/ [accessed 26 August 2010].
- 15.Aromaa A, Koponen P, Tafforeau J, Vermeire C, HIS/HES Core Group Evaluation of Health Interview Surveys and Health Examination Surveys in the European Union. Eur J Public Health. 2003;13(Suppl):67–72. doi: 10.1093/eurpub/13.suppl_1.67. [DOI] [PubMed] [Google Scholar]
- 16.German National Health Examination and Interview Survey 1998 Berlin: Robert Koch Institute; 2000.
- 17.Ministry of Health. Labor and Welfare. Annual report of the National Nutrition Survey in Japan, 2000 Tokyo: Daiichi Shuppan Publishing Co.; 2002. Japanese. [Google Scholar]
- 18.Scottish Health Survey Edinburgh: The Scottish Government; 2008. Available from: http://www.scotland.gov.uk/Publications/2009/09/28102003/0 [accessed 26 August 2010].
- 19.Aekplakorn W, Abbott-Klafter J, Khonputsa P, Tatsanavivat P, Chongsuvivatwong V, Chariyalertsak S, et al. Prevalence and management of prehypertension and hypertension by geographic regions of Thailand: the Third National Health Examination Survey, 2004. J Hypertens. 2008;26:191–8. doi: 10.1097/HJH.0b013e3282f09f57. [DOI] [PubMed] [Google Scholar]
- 20.National Health and Nutrition Examination Survey III Hyattsville: National Center for Health Statistics, US Department of Health and Human Services; 2009. Available from: http://www.cdc.gov/nchs/nhanes.htm [accessed 26 August 2010]
- 21.1991–2006 Health Survey for England London: Health and Social Surveys Research Group, University College London; 2009. Available from: http://www.ucl.ac.uk/hssrg/hse.html [accessed 26 August 2010].
- 22.Encuesta Nacional de Salud y Nutrición 2006 [National Health and Nutrition Survey 2006]. Mexico City: Instituto Nacional de Salud Pública; 2009. Available from: http://www.insp.mx/ensanut/ [accessed 26 August 2010]. Spanish.
- 23.Buhi ER, Goodson P, Neilands TB. Out of sight, not out of mind: strategies for handling missing data. Am J Health Behav. 2008;32:83–92. doi: 10.5555/ajhb.2008.32.1.83. [DOI] [PubMed] [Google Scholar]
- 24.World population prospects: the 2006 revision [Internet database]. New York: Population Division, Department of Economic and Social Affairs, United Nations. Available from: http://esa.un.org/unpp [accessed 26 August 2010].
- 25.Young D. Implementation of SI units for clinical laboratory data. J Gen Intern Med. 1988;3:103–18. doi: 10.1007/BF02595774. [DOI] [Google Scholar]
- 26.Ezzati M, Vander Hoorn S, Lawes CM, Leach R, James WP, Lopez AD, et al. Rethinking the “diseases of affluence” paradigm: global patterns of nutritional risks in relation to economic development. PLoS Med. 2005;2:e133. doi: 10.1371/journal.pmed.0020133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Frenk J. Bridging the divide: global lessons from evidence-based health policy in Mexico. Lancet. 2006;368:954–61. doi: 10.1016/S0140-6736(06)69376-8. [DOI] [PubMed] [Google Scholar]
- 28.Nash DB, Nash SA.Reclassification of simvastatin to over-the-counter status in the United Kingdom: a primary prevention strategy. Am J Cardiol 200494Suppl 135–9.[REMOVED HYPERLINK FIELD] 10.1016/j.amjcard.2004.07.053 [DOI] [PubMed] [Google Scholar]
- 29.Sooksriwong CO. Medicine pricing, availability and affordability in Thailand Bangkok: Office of Food and Drug Administration, Ministry of Public Health; 2007. Available from: http://www.haiweb.org/medicineprices/surveys/200610TH/sdocs/survey_report.pdf [accessed 26 August 2010]. [Google Scholar]
- 30.Kishore SP, Herbstman BJ. Adding a medicine to the WHO model list of essential medicines. Clin Pharmacol Ther. 2009;85:237–9. doi: 10.1038/clpt.2008.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.International Drug Price Indicator Guide [Internet database]. Cambridge: Management Sciences for Health; 2007. Available from: http://erc.msh.org/mainpage.cfm?file=1.0.htm&id=1&temptitle=Introduction&module=DMP&language=English [accessed 26 August 2010].
- 32.Robson J. Lipid modification: cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease. Heart. 2008;94:1331–2. doi: 10.1136/hrt.2008.150979. [DOI] [PubMed] [Google Scholar]
- 33.Hockley T, Gemmill M. European cholesterol guidelines report London: London School of Economics, Policy Analysis Centre; 2007. Available from: http://www.policy-centre.com/downloads/European-Cholesterol-Guidelines07.pdf [accessed 26 August 2010]. [Google Scholar]
- 34.Erhardt LR, Hobbs FD. A global survey of physicians’ perceptions on cholesterol management: the From The Heart study. Int J Clin Pract. 2007;61:1078–85. doi: 10.1111/j.1742-1241.2007.01420.x. [DOI] [PubMed] [Google Scholar]
- 35.King G, Gakidou E, Imai K, Lakin J, Moore RT, Nall C, et al. Public policy for the poor? A randomised assessment of the Mexican universal health insurance programme. Lancet. 2009;373:1447–54. doi: 10.1016/S0140-6736(09)60239-7. [DOI] [PubMed] [Google Scholar]
- 36.The world health report 2000 –. health systems: improving performance Geneva: World Health Organization; 2000. [Google Scholar]
- 37.Kotseva K, Wood D, De Backer G, De Bacquer D, Pyörälä K, Keil U, EUROASPIRE Study Group Cardiovascular prevention guidelines in daily practice: a comparison of EUROASPIRE I, II, and III surveys in eight European countries. Lancet. 2009;373:929–40. doi: 10.1016/S0140-6736(09)60330-5. [DOI] [PubMed] [Google Scholar]
- 38.Mendis S, Abegunde D, Yusuf S, Ebrahim S, Shaper G, Ghannem H, et al. WHO study on prevention of recurrences of myocardial infarction and stroke (WHO–PREMISE). Bull World Health Organ. 2005;83:820–9. [PMC free article] [PubMed] [Google Scholar]
- 39.Joshi R, Chow CK, Raju PK, Raju R, Reddy KS, Macmahon S, et al. Fatal and nonfatal cardiovascular disease and the use of therapies for secondary prevention in a rural region of India. Circulation. 2009;119:1950–5. doi: 10.1161/CIRCULATIONAHA.108.819201. [DOI] [PubMed] [Google Scholar]
- 40.Posadas-Romero C, Tapia-Conyer R, Lerman-Garber I, Zamora-González J, Cardoso-Saldaña G, Salvatierra-Izaba B, et al. Cholesterol levels and prevalence of hypercholesterolemia in a Mexican adult population. Atherosclerosis. 1995;118:275–84. doi: 10.1016/0021-9150(95)05615-7. [DOI] [PubMed] [Google Scholar]
- 41.Steinhagen-Thiessen E, Bramlage P, Lösch C, Hauner H, Schunkert H, Vogt A, et al. Dyslipidemia in primary care–prevalence, recognition, treatment and control: data from the German Metabolic and Cardiovascular Risk Project (GEMCAS). Cardiovasc Diabetol. 2008;7:31. doi: 10.1186/1475-2840-7-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.National Cholesterol Education Program Working Group on Lipoprotein Measurement. National Cholesterol Education Program recommendations for lipoprotein measurement Bethesda: National Heart, Lung and Blood Institute; 1995. [Google Scholar]
- 43.Jackevicius CA, Tu JV, Ross JS, Ko DT, Krumholz HM. Use of ezetimibe in the United States and Canada. N Engl J Med. 2008;358:1819–28. doi: 10.1056/NEJMsa0801461. [DOI] [PubMed] [Google Scholar]
- 44.Grundy SM, Cleeman JI, Merz CN, Brewer HB, Jr, Clark LT, Hunninghake DB, et al. Coordinating Committee of the National Cholesterol Education Program Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. J Am Coll Cardiol. 2004;44:720–32. doi: 10.1016/j.jacc.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 45.McDade TW, Williams S, Snodgrass JJ. What a drop can do: dried blood spots as a minimally invasive method for integrating biomarkers into population-based research. Demography. 2007;44:899–925. doi: 10.1353/dem.2007.0038. [DOI] [PubMed] [Google Scholar]