Abstract
Objective
To explore the relationship between homestead distance to hospital and access to care and to estimate the sensitivity of hospital-based surveillance in Kilifi district, Kenya.
Methods
In 2002–2006, clinical information was obtained from all children admitted to Kilifi District Hospital and linked to demographic surveillance data. Travel times to the hospital were calculated using geographic information systems and regression models were constructed to examine the relationships between travel time, cause-specific hospitalization rates and probability of death in hospital. Access to care ratios relating hospitalization rates to community mortality rates were computed and used to estimate surveillance sensitivity.
Findings
The analysis included 7200 admissions (64 per 1000 child–years). Median pedestrian and vehicular travel times to hospital were 237 and 61 minutes, respectively. Hospitalization rates decreased by 21% per hour of travel by foot and 28% per half hour of travel by vehicle. Distance decay was steeper for meningitis than for pneumonia, for females than for males, and for areas where mothers had less education on average. Distance was positively associated with the probability of dying in hospital. Overall access to care ratios, which represent the probability that a child in need of hospitalization will have access to care at the hospital, were 51–58% for pneumonia and 66–70% for meningitis.
Conclusion
In this setting, hospital utilization rates decreased and the severity of cases admitted to hospital increased as distance between homestead and hospital increased. Access to hospital care for children living in remote areas was low, particularly for those with less severe conditions. Distance decay was attenuated by increased levels of maternal education. Hospital-based surveillance underestimated pneumonia and meningitis incidence by more than 45% and 30%, respectively.
摘要
目的
旨在探讨住宅离医院的距离和获取医疗服务机会之间的关系并评价肯尼亚基利菲区基于医院监测的灵敏度。
方法
我们获取了2002–2006年间基利菲区所有住院儿童的临床信息,并将该信息与人口统计学监测数据相联系。运用地理信息系统计算该区居民前往医院的次数,同时构建回归模型以考察行程时间、各种原因的住院率和在医院的死亡概率。对关系到住院率与社区死亡率的获取医疗服务机会的比率也进行了计算,并用来评估监测的灵敏度。
发现
分析中包括了7200个住院案例(所述年份中每1000名儿童中64例)。步行和乘坐车辆前往医院的平均时间分别为237和61分钟。每徒步旅行一小时,住院率下降21%,每乘坐交通工具半小时,住院率下降28%。患脑膜炎与患肺炎相比,女性与男性相比,前者距离衰减幅度更大,并且在母亲平均教育水平较低的地区距离衰减幅度也更大。距离和在医院的死亡概率呈正相关。关于总的获取医疗服务机会的比例(代表需要住院的孩子有机会在医院得到医疗服务的概率),肺炎为51%-58%,脑膜炎为66%-70%。
结论
这种情况下医院使用率降低,随着住宅和医院间距离的增加,住院病例的严重性也在增加。住在偏远地区的儿童获取医院医疗服务的机会较低,特别是那些病情不太严重的儿童。随着母亲教育水平的提高,距离衰减减弱。基于医院的监测低估了肺炎和脑膜炎发病率,分别超过45%和30%。
Résumé
Objectif
Explorer la relation entre la distance du domicile à l’hôpital et l’accès aux soins, mais aussi évaluer la sensibilité de la surveillance hospitalière dans le district de Kilifi au Kenya.
Méthodes
Sur la période 2002–2006, des informations cliniques ont été obtenues pour tous les enfants admis au Kilifi District Hospital, puis elles ont été liées aux données relatives à la surveillance démographique. Les temps de trajet vers l’hôpital ont été calculés à l’aide de systèmes d’information géographique, et des modèles de régression ont été créés afin d’examiner les relations entre le temps de trajet, les taux d’hospitalisation par cause et la probabilité de décès à l’hôpital. Les taux d'accès aux soins reliant les taux d’hospitalisation aux taux de mortalité de la communauté ont été calculés et utilisés afin d’évaluer la sensibilité de la surveillance.
Résultats
L’analyse a inclus 7 200 admissions (64 pour 1 000 enfants–années). Les temps de trajet moyens à pied et en véhicule vers l’hôpital étaient respectivement de 237 et de 61 minutes. Les taux d’hospitalisation ont diminué de 21 % par heure de trajet à pied et de 28 % par demi-heure de trajet en véhicule. L'impact de la distance a été plus élevé pour la méningite que pour la pneumonie, pour les filles que pour les garçons, mais aussi pour les zones où l’éducation des mères était en moyenne inférieure. La distance était formellement associée à la probabilité de mourir à l’hôpital. Les taux globaux de l’accès aux soins, qui représentent la probabilité qu’un enfant nécessitant une hospitalisation puisse accéder aux soins hospitaliers, étaient de 51–58 % pour la pneumonie et de 66–70 % pour la méningite.
Conclusion
Dans ce contexte, les taux d’utilisation de l’hôpital ont diminué et la gravité des cas admis à l’hôpital a augmenté lorsque la distance entre le domicile et l’hôpital augmentait. L’accès aux soins hospitaliers pour les enfants vivant dans les zones éloignées était faible, en particulier pour ceux dont l’état de santé était grave. L'impact de la distance a été atténué par l'élévation des niveaux d’éducation maternelle. La surveillance hospitalière a sous-estimé l’incidence de la pneumonie et de la méningite de plus de 45 % et 30 %, respectivement.
Resumen
Objetivo
Investigar la relación existente entre la distancia desde el hogar del paciente al hospital y el acceso a la asistencia. Valorar la sensibilidad de la vigilancia hospitalaria en el distrito de Kilifi, Kenya.
Métodos
Entre 2002 y 2006 se obtuvo la información clínica de todos los niños ingresados en el Hospital del Distrito de Kilifi y dicha información se vinculó a los datos de vigilancia demográfica. Se calcularon los trayectos al hospital, empleando los sistemas de información geográfica, y se diseñaron modelos de regresión para analizar las relaciones entre la duración del trayecto, las tasas de hospitalización para cada causa específica y la probabilidad de muerte hospitalaria. Los porcentajes de acceso a la asistencia, que relacionaban las tasas de hospitalización con las tasas de mortalidad en la comunidad, se informatizaron y se emplearon para calcular la sensibilidad de la vigilancia.
Resultados
El análisis incluyó 7 200 ingresos (64 por cada 1000 niños–años). La duración media de los trayectos al hospital fue de 237 minutos caminando y de 61 minutos en coche u otro vehículo. Las tasas de hospitalización descendieron en un 21% por cada hora de trayecto a pie y en un 28% por cada hora de trayecto en coche u otro vehículo. La influencia de la distancia fue más pronunciada para la meningitis que para la neumonía, para las mujeres que para los hombres y para las áreas en las que las madres contaban con un nivel inferior de educación. La distancia se asoció categóricamente con la probabilidad de morir en el hospital. Los porcentajes generales de acceso a la asistencia, que representan la probabilidad de que un niño que requiera hospitalización tenga acceso a la asistencia hospitalaria, fueron de un 51–58% para la neumonía y de un 66–70% para la meningitis.
Conclusión
En esta situación, las tasas de utilización del hospital descendieron y la gravedad de los casos de los ingresados en el hospital aumentó conforme aumentaba la distancia entre el hogar del paciente y el hospital. El acceso a la asistencia hospitalaria de los niños que vivían en las áreas alejadas fue bajo, especialmente para aquellos que presentaban afecciones de menor gravedad. La influencia de la distancia se atenuó por el aumento del nivel de educación materna. La vigilancia hospitalaria infravaloró la incidencia de la neumonía y de la meningitis en más de un 45% y de un 30%, respectivamente.
Резюме
Цель
Исследовать зависимость между расстоянием от фермы до больницы и доступом к медицинской помощи и оценить чувствительность амбулаторного наблюдения в округе Килифи (Кения).
Методы
В 2002–2006 гг. от всех детей, госпитализированных в больницу округа Килифи, была получена клиническая информация, которая была сопоставлена с данными демографического наблюдения. Рассчитывалось время в пути до больницы с использованием систем географической информации и составлялись модели регрессии для исследования зависимости между временем в пути, показателями госпитализации с разбивкой по причинам и вероятностью смерти в больнице. Для оценки чувствительности наблюдения были рассчитаны коэффициенты доступа к медицинской помощи, представлявшие собой отношение показателей госпитализации к показателям смертности в общинах.
Результаты
Анализ охватывал 7200 госпитализаций (64 на 1000 лет жизни детей). Медианное время в пути до больницы пешком и на автотранспорте составляло 237 и 61 минуту, соответственно. Число госпитализаций снизилось на 21% в пересчете на 1 час в пути пешком и на 28% в пересчете на 1 час пути на автотранспорте. Убывание при увеличении расстояния проявлялось сильнее для менингита, чем для пневмонии, для женщин, чем для мужчин, а также в районах, где уровень образования у матерей в среднем был более низким. Наблюдалась положительная корреляция между расстоянием и вероятностью смерти в больнице. Суммарные показатели доступа к медицинской помощи, отражающие вероятность того, что ребенок, нуждающийся в госпитализации, получит доступ к медицинской помощи в больнице, составили 51–58% для пневмонии и 66–70% для менингита.
Вывод
В данных условиях показатели пользования больницей снижались, а тяжесть состояния больных при госпитализации повышалась по мере увеличения расстояния между фермой и больницей. Доступ к больничной помощи для детей, проживающих в отдаленных районах, был низким, особенно для менее тяжелых состояний. Убывание при увеличении расстояния снижалось по мере повышения уровня образования матерей. Данные амбулаторного наблюдения по пневмонии и менингиту были занижены более чем на 45 и 30%, соответственно.
ملخص
الغرض: استكشاف العلاقة بين المسافة الفاصلة بين منزل الأسرة والمستشفى والقدرة على الوصول إلى الرعاية، وتقدير حساسية الترصد المستند على المستشفى في مقاطعة كيليفي في كينيا.
الطريقة: في الأعوام 2002 حتى 2006، جُمِعَت معلومات إكلينيكية من جميع الأطفال الذين أُدخلوا للعلاج في مستشفى مقاطعة كيليفي وتم ربطها بمعطيات الترصد الديموغرافي. وحُسِبَ الوقتُ المستغرق في الانتقال إلى المستشفى باستخدام نظم معلومات جغرافية، وأُعِدَت نماذج تحوُّف لفحص العلاقة بين الوقت المستغرق في الانتقال ومعدلات المعالجة في المستشفى الخاصة بسبب معيّن، واحتمال الوفاة في المستشفى. وحُسِبَت نسب الوصول إلى الرعاية التي تربط علاقة معدلات المعالجة في المستشفى بمعدلات الوفيات المجتمعية واستخدمت لتقدير حساسية الترصد.
الموجودات: ضم التحليل 7200 إدخالٍ في المستشفى (64 إدخال لكل 1000 طفل–لتلك السنوات). وكان وسيط الزمن المستغرق في الوصول إلى المستشفى سيراً على الأقدام هو 237 دقيقة، وركوباً للسيارات هو 61 دقيقة. انخفضت معدلات المعالجة في المستشفى بنسبة 21% لقاء كل ساعة تستغرق للانتقال سيراً على الأقدام، وبنسبة 28% لكل نصف ساعة تستغرق للانتقال ركوباً للسيارات. كان التأثير السلبي للمسافة أشد وضوحاً في حالات الالتهاب السحائي عنه في الالتهاب الرئوي، ولدى الإناث عنه لدى الذكور، وفي المناطق التي لم تحظ فيها الأمهات في المتوسط إلا بقدر أقل من التعليم. وارتبطت المسافة ارتباطاً إيجابياً باحتمال الوفاة في المستشفى. وبلغت النسب الكلية للوصول إلى الرعاية، والتي تمثل احتمال وصول الطفل المحتاج للعلاج في المستشفى إلى الرعاية في المستشفى، 51-58% للالتهاب الرئوي، و 66-70% للالتهاب السحائي.
الاستنتاج: في هذا الموقع، انخفضت معدلات الاستفادة من المستشفى وازدادت وخامة الحالات التي أدخلت المستشفى كلما ازدادت المسافة بين منزل الأسرة والمستشفى. وكان وصول الأطفال الذين يعيشون في مناطق نائية إلى الرعاية في المستشفى منخفضاً، ولاسيما الأطفال الذين يعانون من حالات أقل وخامة. وقل التأثير السلبي للمسافة بزيادة المستوى التعليمي للأمهات. وقد قلّل الترصد المستند على المستشفى من تقدير معدل وقوع الالتهاب الرئوي بأكثر من 45% ومن معدل وقوع التهاب السحايا بأكثر من 30%.
Introduction
In addition to a focus on the Millennium Development Goals – specifically Goal 4, which aims for a two-thirds reduction in under-5 mortality between 1990 and 2015 – the child survival agenda in developing countries is increasingly driven by equity considerations.1,2 Regional and country-level analyses have investigated the socioeconomic and spatial determinants of health inequities and have demonstrated that lower-income and rural populations frequently experience worse child survival rates than their wealthier, more urban counterparts.3–6 However, limited data are available at the district level to help identify geographic inequities in health outcomes and target the delivery of services to disadvantaged populations.7,8
In rural settings with a low density of health facilities, physical access to sources of care is a known determinant of health-care utilization, with substantial decreases in rates of clinic attendance observed with increasing distance from the homestead to the clinic;9–19 this phenomenon is frequently termed “distance decay.” However, studies have not directly linked distance to health facilities to morbidity rates in the community. High utilization rates in areas close to clinics could therefore partially reflect higher rates of disease rather than better access, as would be the case, for example, if deliberately or coincidentally sicker people lived closer to clinics or if clinics were located in areas of higher disease risk.
Moreover, distance decay is generally less marked for hospitals providing inpatient services than for primary care clinics,11,15,20 suggesting that disease severity may modulate the effect of distance on care-seeking and ultimately limit its impact on mortality. In Kilifi district, Kenya, we found no effect of distance to hospitals or vaccine clinics on child mortality,21 a finding consistent with the results of a study from the Gambia22 but not with analyses from rural areas of Burkina Faso,23 the Democratic Republic of the Congo24 or the United Republic of Tanzania.25
Regardless of their impact on mortality, physical and other barriers to health care seeking are widely assumed to lead to incomplete disease ascertainment in hospital and to limit the sensitivity of hospital-based surveillance. Disease incidence rates observed in sentinel surveillance systems therefore systematically underestimate the true incidence of disease, and this complicates national and global disease burden estimation. Measuring access to care may enable us to evaluate the sensitivity of surveillance and improve on current estimates of disease burden.
In this study we aimed to characterize spatial variations in hospitalization rates in Kilifi district for several diseases, identify areas with low utilization of inpatient services, and link this information to mortality rates to define access to care parameters by health condition and geographic area and estimate the sensitivity of hospital-based surveillance.
Methods
This analysis relied on data collected routinely by the Epidemiologic and Demographic Surveillance System (Epi-DSS) of the KEMRI–Wellcome Trust Research Programme in Kilifi district, Kenya. The Epi-DSS includes a demographic surveillance system covering an area measuring 900 km2 around Kilifi District Hospital (KDH) linked to hospital-based epidemiological surveillance.
Study site
Kilifi district is a poor, primarily rural district on the Indian Ocean coast of Kenya that enjoys a tropical climate, with two rainy seasons and two dry seasons each year. Mortality in children less than 5 years of age has decreased in recent years but remains high at 65 deaths per 1000 live births.21 KDH serves as a primary care centre and first-level referral facility for the entire district. Inpatient care is available at three other hospitals in Kilifi district, at Malindi District Hospital in Malindi and at Coast Provincial General Hospital in Mombasa. For most residents of the study area, KDH is the nearest facility offering inpatient care.
Demographic and clinical data
Demographic surveillance was initiated in 2000 to track births, deaths and migrations in a target population of 250 000 people. After the initial census, two to three enumeration rounds were conducted each year. Each resident received a unique personal identifier. From 16 April 2002 onwards, hospital and laboratory records including standard clinical data for all admitted children were linked to demographic records for Epi-DSS area residents based on personal identifier. This enabled us to determine the exact residency of each patient at the time of hospitalization. All data were entered into FileMaker 5.5 (FileMaker Inc., Santa Clara, United States of America), and cleaned in Stata 9.2 (StataCorp LP, College Station, USA).
Mapping and travel time
The Epi-DSS area was mapped using Magellan (Magellan Navigation Inc., Santa Clara, USA) and e-Trex (Garmin Ltd, Olathe, USA) geographic positioning systems (GPS) technology, which provided information on topography, footpaths and roads and on the human occupation of the area, including the coordinates of all homesteads. We mapped the seven matatu (local bus) routes in January 2007 and collected information on matatu speeds. All geographic data were imported via Datasend (Magellan Navigation Inc., Santa Clara, USA), Map Source (Garmin Ltd, Olathe, USA), or DNRGarmin (Minesotta Dept of Natural Resources, St Paul, USA) software into ArcGIS 9.2 (Esri, Redlands, USA) for mapping and analysis.
Pedestrian and vehicular travel times to KDH were calculated using an ArcGIS cost-distance algorithm, which determines the shortest path from each homestead to the hospital assuming speeds of 5 km/h on roads and footpaths and of 2.5 km/h off-road in the pedestrian model, and matatu speeds on matatu routes and pedestrian speeds elsewhere in the vehicular model (i.e. individuals walk from home to the nearest matatu stage, then travel by matatu to hospital). Details of this method have been described previously.21 In stratified analyses, we used one-hour strata for pedestrian travel time and half-hour strata for vehicular travel time.
Other variables of interest
Other variables of interest were ethnicity, maternal education, migration and time. Ethnicity data were collected routinely by the Epi-DSS. The majority ethnic groups in Kilifi district are of Mijikenda origin and include the Giriama and the Chonyi. Ethnic groups with less than 40 deaths during the study period were combined under the category “other.” Maternal education data were collected from all residents in 2004. We calculated the proportion of women 15–49 years old with any schooling in each administrative sublocation and used it to generate a sublocation-level categorical variable (proportion of mothers with any education < 0.5; 0.5 to < 0.6; 0.6 to < 0.7; and ≥ 0.7), which was then applied to individuals based on their residence. For migration, children whose mothers had migrated at least once from outside the Epi-DSS area between 2000 and 2006 were considered migrants. Finally, we analysed seasonal and annual trends in hospitalizations. Mean daily rainfall in Kilifi during the rainy season (April to June and October to November) was ≥ 5 mm between 2000 and 2006.
Endpoints and case definitions
We investigated the effects of travel time to KDH on all-cause hospitalization and on hospitalizations for pneumonia and suspected meningitis. Pneumonia was categorized as mild, severe or very severe. Mild pneumonia was defined as a history of acute cough or difficulty breathing plus an elevated respiratory rate (RR) for age (RR ≥ 50 breaths per min in children 0 to 11 months old and ≥ 40 breaths per min in those 12 to 59 months old), severe pneumonia as a history of cough or difficulty breathing plus lower chest wall indrawing, and very severe pneumonia as a history of cough or difficulty breathing plus hypoxia, lethargy, loss of consciousness, prostration or a history of convulsions.26 Suspected meningitis required one or more of the following signs: stiff neck, bulging fontanelle in children < 1 year of age, lethargy, loss of consciousness, prostration or history of convulsions (any seizure in children < 6 months of age; any partial seizure or at least two generalized seizures over the previous 24 hours in children 6–59 months of age).
Data analysis
For each condition, we calculated admission rates per 1000 child–years (allowing multiple admissions per child) by pedestrian and vehicular travel time to hospital and by administrative location, as well as by sex, ethnic group, maternal education, migrant status, season and year for children < 5 years of age. We constructed log-linear regression models to identify predictors of the incidence of admission to KDH and logistic regression models to investigate risk factors for death in admitted children. To account for spatial clustering of disease events in these models, we used a spatial bootstrap method with 50 repetitions, randomly selecting 40 sublocations (with replacement) and estimating the regression model on all data from the selected sublocations in each repetition. The incidence analysis was restricted to 2004 through 2006, a period for which ascertainment of person–time by the Epi-DSS was complete. The case fatality ratio analysis used data from 2002 onwards, since it did not require population-based denominators. All analyses were conducted in Stata 9.2.
For each pedestrian and vehicular travel time stratum we computed the ratios of both the pneumonia and the suspected meningitis hospitalization rate to the all-cause mortality rate measured in the community by the Epi-DSS (Rp = pneumonia admission rate/all-cause mortality rate and Rm = suspected meningitis admission rate/all-cause mortality rate). Assuming that children in the lowest stratum (stratum 0) had “perfect” access to care (e.g. that all pneumonia and meningitis cases requiring hospitalization presented to KDH and were admitted) and that the incidence of pneumonia and meningitis requiring hospitalization was directly proportional to the incidence of death, we calculated the stratum-specific probability that a child in need of hospitalization would access care at KDH (“access to care ratios”) as R[travel time stratum]/R[stratum 0] for pneumonia and suspected meningitis separately. We obtained 95% confidence intervals (CIs) by applying the delta method for variance calculation to successive log-transformations of these ratios, under the assumption that stratum-specific rates were independent. We compared the trends in pneumonia and meningitis ratios across travel time strata using the Cuzick extension to the Wilcoxon rank sum test.27 Access to care ratios for the entire Epi-DSS area were calculated as a weighted average of stratum-specific ratios, with person–years of observation as weights.
Ethical approval
The Kenya Medical Research Institute Ethical Review Committee and the Johns Hopkins Bloomberg School of Public Health Institutional Review Board approved this study.
Results
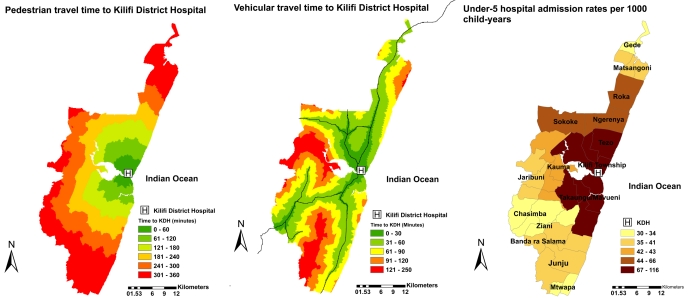
Median pedestrian and vehicular travel times to hospital were 237 minutes (range 0–514 minutes) and 61 minutes (range: 0–247 minutes), respectively, and 90% of children lived less than 6.5 hours on foot or 2 hours by vehicle from KDH (Fig. 1).
Fig. 1.
Pedestrian and vehicular travel time to Kilifi District Hospital and incidence of hospitalization for Kilifi Epi-DSS residents less than 5 years of age, by administrative location, Kilifi district, Kenya, 2004–2006
Epi-DSS, Epidemiologic and Demographic Surveillance System.
Source of map: KEMRI/Wellcome Trust Epi-DSS in Kilifi.
Hospitalization rates
Between 2004 and 2006, 7200 current Epi-DSS residents less than 5 years of age were admitted to KDH (64 per 1000 child–years), and of these children, 3273 (29 per 1000) had pneumonia and 1758 (16 per 1000) had suspected meningitis. Maps of hospitalization rates by location showed high rates of admission in Kilifi Township (115/1000) and in the two immediately adjacent locations to the north and south (95/1000), accessible by the main coastal road. Hospitalization incidence decreased with increasing distance from the hospital and was lowest in the far northern and southern areas (30 to 35 per 1000). Overall, locations to the north of Kilifi township had higher hospitalization rates than locations to the south. These patterns were replicated for each of the admission endpoints and are reflected in simple graphics of incidence by travel time (Fig. 2).
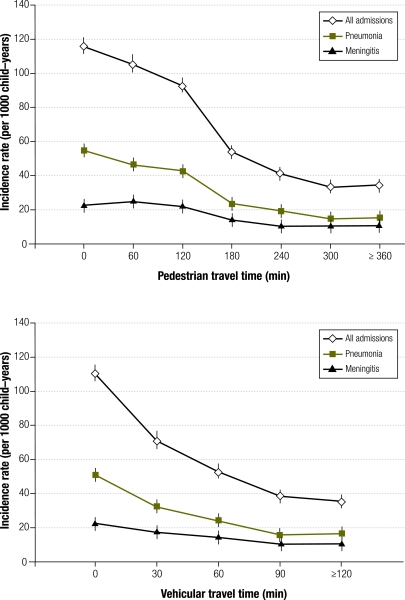
Fig. 2.
Incidence of hospitalization with any syndrome, pneumonia and suspected meningitis by pedestrian and vehicular travel time to the Kilifi District Hospital in Kilifi Epi-DSS residents less than 5 years of age, Kilifi district, Kenya, 2004–2006
Epi-DSS, Epidemiologic and Demographic Surveillance System.
In univariate log-linear models, the incidence of hospitalization decreased by 15 to 21% per hour of pedestrian travel time to KDH and by 23 to 28% per half hour of vehicular travel time, depending on the endpoint (Table 1). This “distance decay” was less marked for suspected meningitis than for pneumonia.
Table 1. Univariate all-cause and cause-specific hospitalization rate ratios (RRs) for continuous travel time variables and categorical covariates among children less than 5 years of age admitted to Kilifi District Hospital, Kilifi district, Kenya, 2004–2006.
| Variable | RR (95% CI) | ||
|---|---|---|---|
| All admissions | Pneumonia | Suspected meningitis | |
| Travel time | |||
| Pedestrian (60 m) | 0.79 (0.76–0.84) | 0.79 (0.76–0.82) | 0.85 (0.80–0.90) |
| Vehicular (30 m) | 0.73 (0.68–0.79) | 0.72 (0.67–0.77) | 0.77 (0.70–0.84) |
| Sex (baseline: Female) | |||
| Male | 1.22 (1.15–1.30) | 1.17 (1.06–1.28) | 1.25 (1.15–1.36) |
| Ethnic group (baseline: Giriama) | |||
| Chonyi | 0.63 (0.49–0.82) | 0.61 (0.47–0.77) | 0.66 (0.53–0.84) |
| Kauma | 0.93 (0.73–1.20) | 0.88 (0.70–1.11) | 0.93 (0.71–1.22) |
| Luo | 1.13 (0.81–1.58) | 1.07 (0.73–1.60) | 1.23 (0.79–1.93) |
| Duruma | 0.70 (0.50–0.98) | 0.76 (0.53–1.11) | 0.71 (0.47–1.08) |
| Jibana | 0.51 (0.36–0.71) | 0.59 (0.37–0.95) | 0.61 (0.34–1.11) |
| Other | 1.02 (0.82–1.29) | 0.99 (0.78–1.28) | 0.93 (0.74–1.17) |
| Maternal educationa (baseline: < 0.5) | |||
| 0.5 to < 0.6 | 0.58 (0.33–1.02) | 0.59 (0.33–1.06) | 0.59 (0.35–1.03) |
| 0.6 to < 0.7 | 0.62 (0.35–1.12) | 0.68 (0.13–1.31) | 0.62 (0.36–1.06) |
| ≥ 0.7 | 1.21 (0.81–1.82) | 1.39 (0.90–2.16) | 0.95 (0.58–1.55) |
| Migrant status (baseline: non-migrant) | |||
| Migrant | 0.87 (0.80–0.96) | 0.85 (0.75–0.97) | 0.91 (0.76–1.07) |
| Season (baseline: dry) | |||
| Rainy | 0.83 (0.78–0.88) | 0.75 (0.70–0.81) | 0.82 (0.73–0.92) |
| Year (baseline: 2004) | |||
| 2005 | 0.85 (0.81–0.91) | 0.75 (0.68–0.83) | 0.76 (0.69–0.85) |
| 2006 | 1.10 (1.01–1.20) | 1.01 (0.89–1.16) | 1.06 (0.93–1.21) |
CI, confidence interval.
a Categories represent the proportion of women with any education in a child’s sublocation of residence.
Admission rates varied by ethnic group and were significantly lower in females, migrants and the rainy season than in males, non-migrants and the dry season, respectively (Table 1).
We constructed multivariable models including the statistically significant main effects and interaction effects of each covariate on the incidence of all-cause, pneumonia and suspected meningitis hospitalization (Table 2). Pedestrian travel time models included interaction terms for maternal education only (all-cause and pneumonia admissions) and both maternal education and sex (suspected meningitis admissions). For all-cause hospitalization, overall rate ratios (RRs) (incorporating effect modification) for pedestrian travel time increased from 0.65 (95% CI: 0.60–0.69) to 0.79 (95% CI: 0.73–0.85), 0.83 (95% CI: 0.77–0.90) and 1.57 (95% CI: 0.87–2.83) per hour with increasing education levels: the distance decay effect disappeared in the areas where average maternal education was highest. Similar results were obtained for pneumonia distance decay and for meningitis distance decay, irrespective of sex. In vehicular models, boys had 1.05- to 1.11-fold higher rate ratios for travel time than girls, which indicates that they experienced lower decay of admission rates with distance.
Table 2. All-cause and cause-specific hospitalization rate ratios (RRs) for main effects and interaction effects of travel time to Kilifi District Hospital among children less than 5 years of age, Kilifi district, Kenya, 2004–2006.
| Models | RR (95% CI) | ||
|---|---|---|---|
| All admissionsa | Pneumoniab | Suspected meningitisc | |
| Pedestrian (per 60 minutes) | |||
| Travel time | 0.65 (0.58–0.74) | 0.63 (0.57–0.71) | 0.62 (0.53–0.73) |
| Male sex × travel time | 1.06 (1.02–1.10) | ||
| Maternal educationd 0.5 to < 0.6 × travel time | 1.21 (1.03–1.41) | 1.26 (1.10–1.45) | 1.33 (1.11–1.59) |
| Maternal education 0.6 to < 0.7 × travel time | 1.27 (1.10–1.48) | 1.28 (1.12–1.46) | 1.40 (1.19–1.64) |
| Maternal education ≥ 0.7 × travel time | 2.40 (1.31–4.42) | 1.68 (0.29–9.84) | 2.42 (0.83–7.04) |
| Vehicular (per 30 minutes) | |||
| Travel time | 0.71 (0.64–0.79) | 0.71 (0.64–0.78) | 0.75 (0.68–0.83) |
| Male sex × travel time | 1.07 (1.02–1.12) | 1.05 (0.97–1.14) | 1.11 (1.04–1.18) |
CI, confidence interval.
a Final models included main effects of sex, ethnic group, maternal education, migrant status and year and interaction effects of maternal education (pedestrian) or sex (vehicular).
b Final models included main effects of sex, ethnic group, maternal education, migrant status, year and season and interaction effects of maternal education (pedestrian) or sex (vehicular).
c Final models included main effects of sex, ethnic group, maternal education, migrant status, year and season and interaction effects of sex and maternal education (pedestrian) or sex alone (vehicular).
d Categories represent the proportion of women with any education in a child’s sublocation of residence.
In-hospital death risk and travel time
Of the 10 819 admissions to KDH occurring between 2002 and 2006, 647 (6%) resulted in death, as shown in Table 3. Case fatality ratios reached 7.6% for pneumonia and 11.6% for suspected meningitis. The odds of a child dying in the hospital increased by 12% per hour of pedestrian travel time to KDH (odds ratio, OR: 1.12; 95% CI: 1.06–1.18) and 10% per half-hour of vehicular travel time (OR: 1.10; 95% CI: 1.02–1.19). Other covariates affecting the odds of death included age, ethnic group and season. Adjusted ORs for travel time were similar to unadjusted ORs.
Table 3. Risk of death from all causes in children less than 5 years of age admitted to Kilifi District Hospital, Kilifi district, Kenya, 2002–2006.
| Variablea | Unadjusted OR (95% CI) | Adjusted OR, pedestrian (95% CI) | Adjusted OR, vehicular (95% CI) |
|---|---|---|---|
| Travel time to Kilifi District Hospital | |||
| Pedestrian (per 60 m) | 1.12 (1.07–1.18) | 1.14 (1.09–1.19) | – |
| Vehicular (per 30 m) | 1.10 (1.03–1.18) | – | 1.16 (1.07–1.26) |
| Age (baseline: < 1 year old) | |||
| 1–4 year old | 0.35 (0.29–0.41) | 0.34 (0.29–0.41) | 0.34 (0.28–0.42) |
| Ethnic group (baseline: Giriama) | |||
| Chonyi | 1.07 (0.88–1.29) | 0.91 (0.72–1.15) | 0.89 (0.67–1.19) |
| Kauma | 0.70 (0.52–0.95) | 0.71 (0.46–1.08) | 0.63 (0.37–1.07) |
| Luo | 2.73 (1.61–4.61) | 2.88 (1.48–5.59) | 2.88 (1.57–5.26) |
| Duruma | 1.49 (0.82–2.71) | 1.45 (0.81–2.60) | 1.45 (0.79–2.66) |
| Jibana | 1.20 (0.58–2.48) | 0.90 (0.41–1.94) | 0.91 (0.43–1.94) |
| Other | 1.02 (0.74–1.40) | 1.12 (0.77–1.63) | 1.07 (0.72–1.60) |
| Season (baseline: dry) | |||
| Rainy | 1.21 (1.03–1.42) | 1.21 (1.05–1.40) | 1.21 (1.02–1.44) |
CI, confidence interval; OR, odds ratio.
a Sex, maternal education and migrant status were not significant in univariate or multivariable models and are not presented here.
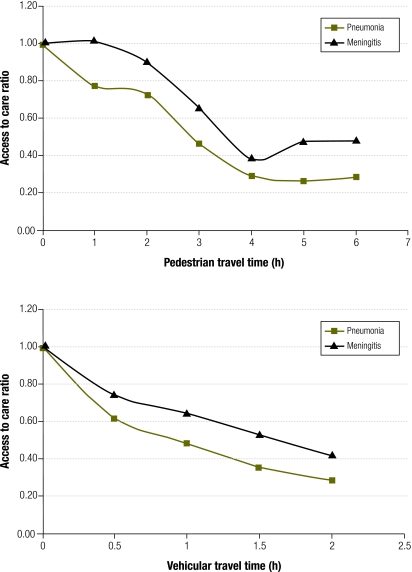
Access to care ratios
Community mortality rates in children aged less than 5 years ranged from 11.9 to 15.3 per 1000 and from 11.6 to 13.6 per 1000 across pedestrian and vehicular travel time strata, respectively.21 Pneumonia hospitalization rates varied from 14.5 to 54.9 per 1000 over pedestrian travel time categories and from 15.8 to 50.7 per 1000 over vehicular travel time categories. The corresponding values for suspected meningitis were 10.5 to 25.1 per 1000 and 10.5 to 22.6 per 1000, respectively (Fig. 2). Access to care ratios for pneumonia and meningitis decreased with travel time to hospital (Fig. 3). Access to care ratios were larger for suspected meningitis than for pneumonia and declined less steeply with travel time (P = 0.05). Overall access to care ratios for the Epi-DSS area, obtained as weighted averages of the stratum-specific ratios, were 0.51 (pedestrian) and 0.58 (vehicular) for pneumonia and 0.66 (pedestrian) and 0.70 (vehicular) for meningitis.
Fig. 3.
Pneumonia and meningitis access to care ratios by pedestrian and vehicular travel time from homestead to Kilifi District Hospital for Kilifi Epi-DSS residents less than 5 years of age, Kilifi district, Kenya, 2004–2006
Epi-DSS, Epidemiologic and Demographic Surveillance System.
Discussion
In this study, we used geographic information system methods to estimate pedestrian and vehicular travel time to the main referral hospital in Kilifi district and examined the relationship between travel time, hospital attendance and disease severity in children less than 5 years of age. We established that hospital admission rates in the Kilifi Epi-DSS decrease roughly exponentially with increases in both pedestrian and vehicular travel time, in line with earlier findings from developing country settings.10,11,15,28 In a similar study in rural Nigeria, Stock et al.11 observed a distance decay gradient of 9% per kilometre for inpatient care, which equates to 24% per hour of walking off roads or 45% per hour on roads using our impedance assumptions. This gradient is steeper than the 21% decrease obtained in our pedestrian model, which suggests that children in Kilifi travel farther to access inpatient care. This could be a function of the perceived high quality of services provided at KDH.11,13,29,30 Alternately, our travel time analysis may be more accurate than a simple Euclidian distance analysis, as it more closely reflects the physical barriers experienced by families seeking care for a sick child.15,17
We found that three important factors influenced the rate of distance decay in our population. The gradient was steeper for children with pneumonia than for those with suspected meningitis, suggesting that the effect of travel time on hospital care-seeking decreases with increasing disease severity. The findings for meningitis are surprising in a context where 43% of mothers of children with convulsions reported visiting a traditional healer as a first resort, before seeking biomedical therapy.31 However, if this behaviour were independent of travel time, it would tend to affect overall hospitalization rates for meningitis without biasing the relative rates.
Maternal education was also a key determinant of distance decay: the pedestrian gradient decreased with increasing education and disappeared in the areas with the highest maternal education levels. Finally, among boys distance decay was less steep than among girls in the vehicular models. Sex was not an explanatory factor in the modelling of access to care ratios for pneumonia and meningitis. Access to care ratios were based on local mortality rates and throughout the area males had higher mortality than females. The sex differential in mortality rates increased with distance from hospital. Therefore, the relative distance decay by sex may simply reflect worsening male health relative to female health with distance from hospital rather than a decrease in the willingness of parents with female children to present them to hospital. Unlike other studies, ours identified no differences in distance decay by age group (infants versus older children) or by sex when pedestrian travel was considered. Detailed, individual-level socioeconomic data are required to examine possible interactions between travel time and socioeconomic factors that influence care-seeking behaviour, including the effect of wealth on mode of transport choice.32,33 Such data are not currently available for our study area, justifying our use of sublocation-level maternal education variables as the best available proxy: this is an important limitation in a setting where household finances are likely to be a key determinant of access to hospital care. We do not expect any confounding by immunization status given the high levels and limited geographic variations in vaccination coverage in Kilifi.34
This study allowed us to assess whether the decrease in admission rates associated with travel time to hospital could reflect lower rates of disease in outlying areas, rather than a lower propensity to seek care. We found that distance to hospital correlated with disease severity in admitted children, as evidenced by increases in the odds of dying with increasing travel time: delays in care-seeking may lead to more severe disease in children who ultimately reach the hospital; alternately, families may be more willing to travel to hospital for more severe conditions. Access to care ratios decreased with distance to hospital and was higher for suspected meningitis than pneumonia, buttressing the concept of distance as a barrier to health care utilization particularly for less severe syndromes. Based on these ratios, we estimated that over 45% of pneumonia cases and over 30% of suspected meningitis cases in the Epi-DSS area would be missed using hospital surveillance alone. Though our analysis included only children less than 5 years of age, previous studies suggest that our conclusions may also hold true among adults.11,17
In this detailed analysis of linked hospitalization and demographic surveillance data sets from the Kilifi Epi-DSS, we showed that pneumonia admission rates decline exponentially with travel time to hospital and drop by three-quarters at six or more hours of travel on foot (or two or more hours of travel by vehicle) compared to baseline against nearly constant background mortality. The effect is less pronounced for meningitis, but there is nevertheless a twofold decline in admission rates over the observed range of travel times. This suggests that a substantial proportion of children with severe diseases fail to present to hospital for life-saving treatment, at least in part because of geographic access barriers. Our approach to calculating surveillance sensitivity can be applied to other settings with data on both hospital morbidity rates and community mortality rates. These novel findings and the accompanying methodology can help scientists and public health practitioners interpret sentinel surveillance data and improve on current disease burden estimates for policy decision-making.
Acknowledgements
The authors thank the Epi-DSS field team, led by Arthurnas Ngala, for diligent work in collecting the demographic data; Christopher Nyundo for help with geographic information system mapping; Mike Kahindi for support with Epi-DSS data management and cleaning; and Scott Zeger for expert advice on the statistical analysis. This study is published with the permission of the director of the Kenya Medical Research Institute (KEMRI), Nairobi.
Funding:
The Kilifi Epi-DSS is part of the INDEPTH network of demographic surveillance sites and is supported by the Wellcome Trust. The study sponsors played no role in designing the study, collecting and analysing the data, writing the final report or deciding to submit for publication.
Competing interests:
None declared.
References
- 1.Victora CG, Wagstaff A, Schellenberg JA, Gwatkin D, Claeson M, Habicht JP. Applying an equity lens to child health and mortality: more of the same is not enough. Lancet. 2003;362:233–41. doi: 10.1016/S0140-6736(03)13917-7. [DOI] [PubMed] [Google Scholar]
- 2.Health, nutrition and population sector strategy Washington: The World Bank; 1997. [Google Scholar]
- 3.Castro-Leal F, Dayton J, Demery L, Mehra K. Public spending on health care in Africa: do the poor benefit? Bull World Health Organ. 2000;78:66–74. [PMC free article] [PubMed] [Google Scholar]
- 4.Wagstaff A. Poverty and health sector inequalities. Bull World Health Organ. 2002;80:97–105. [PMC free article] [PubMed] [Google Scholar]
- 5.Wagstaff A. Socioeconomic inequalities in child mortality: comparisons across nine developing countries. Bull World Health Organ. 2000;78:19–29. [PMC free article] [PubMed] [Google Scholar]
- 6.Kenya Demographic and Health Survey 2003: final report Nairobi: Central Bureau of Statistics, Ministry of Health; 2003.
- 7.Schellenberg JA, Victora CG, Mushi A, de Savigny D, Schellenberg D, Mshinda H, et al. Tanzania Integrated Management of Childhood Illness MCE Baseline Household Survey Study Group Inequities among the very poor: health care for children in rural southern Tanzania. Lancet. 2003;361:561–6. doi: 10.1016/S0140-6736(03)12515-9. [DOI] [PubMed] [Google Scholar]
- 8.Mariam DH, Fantahun M, Molla M, Worku A, Tesfaye F, Emmelin A, et al. Assessment of inequalities in morbidity and mortality in rural Ethiopia: the case of Butajira demographic surveillance site Accra: INDEPTH Network; 2005. [Google Scholar]
- 9.Arcury TA, Gesler WM, Preisser JS, Sherman J, Spencer J, Perin J. The effects of geography and spatial behavior on health care utilization among the residents of a rural region. Health Serv Res. 2005;40:135–55. doi: 10.1111/j.1475-6773.2005.00346.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Müller I, Smith T, Mellor S, Rare L, Genton B. The effect of distance from home on attendance at a small rural health centre in Papua New Guinea. Int J Epidemiol. 1998;27:878–84. doi: 10.1093/ije/27.5.878. [DOI] [PubMed] [Google Scholar]
- 11.Stock R. Distance and the utilization of health facilities in rural Nigeria. Soc Sci Med. 1983;17:563–70. doi: 10.1016/0277-9536(83)90298-8. [DOI] [PubMed] [Google Scholar]
- 12.Rahaman MM, Aziz KM, Munshi MH, Patwari Y, Rahman M. A diarrhea clinic in rural Bangladesh: influence of distance, age, and sex on attendance and diarrheal mortality. Am J Public Health. 1982;72:1124–8. doi: 10.2105/AJPH.72.10.1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gething PW, Noor AM, Zurovac D, Atkinson PM, Hay SI, Nixon MS, et al. Empirical modelling of government health service use by children with fevers in Kenya. Acta Trop. 2004;91:227–37. doi: 10.1016/j.actatropica.2004.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Noor AM, Zurovac D, Hay SI, Ochola SA, Snow RW. Defining equity in physical access to clinical services using geographical information systems as part of malaria planning and monitoring in Kenya. Trop Med Int Health. 2003;8:917–26. doi: 10.1046/j.1365-3156.2003.01112.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Noor AM, Amin AA, Gething PW, Atkinson PM, Hay SI, Snow RW. Modelling distances travelled to government health services in Kenya. Trop Med Int Health. 2006;11:188–96. doi: 10.1111/j.1365-3156.2005.01555.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tanser F, Hosegood V, Benzler J, Solarsh G. New approaches to spatially analyse primary health care usage patterns in rural South Africa. Trop Med Int Health. 2001;6:826–38. doi: 10.1046/j.1365-3156.2001.00794.x. [DOI] [PubMed] [Google Scholar]
- 17.Tanser F, Gijsbertsen B, Herbst K. Modelling and understanding primary health care accessibility and utilization in rural South Africa: an exploration using a geographical information system. Soc Sci Med. 2006;63:691–705. doi: 10.1016/j.socscimed.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 18.Feikin DR, Nguyen LM, Adazu K, Ombok M, Audi A, Slutsker L, et al. The impact of distance of residence from a peripheral health facility on pediatric health utilisation in rural western Kenya. Trop Med Int Health. 2009;14:54–61. doi: 10.1111/j.1365-3156.2008.02193.x. [DOI] [PubMed] [Google Scholar]
- 19.Weber MW, Milligan P, Sanneh M, Awemoyi A, Dakour R, Schneider G, et al. An epidemiological study of RSV infection in the Gambia. Bull World Health Organ. 2002;80:562–8. [PMC free article] [PubMed] [Google Scholar]
- 20.Kloos H. Utilization of selected hospitals, health centres and health stations in central, southern and western Ethiopia. Soc Sci Med. 1990;31:101–14. doi: 10.1016/0277-9536(90)90052-T. [DOI] [PubMed] [Google Scholar]
- 21.Moïsi JC, Gatakaa H, Noor AM, Williams TN, Bauni E, Tsofa B, et al. Geographic access to care is not a determinant of child mortality in a rural Kenyan setting with high health facility density. BMC Public Health. 2010;10:142. doi: 10.1186/1471-2458-10-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rutherford ME, Dockerty JD, Jasseh M, Howie SR, Herbison P, Jeffries DJ, et al. Access to health care and mortality of children under 5 years of age in the Gambia: a case-control study. Bull World Health Organ. 2009;87:216–24. doi: 10.2471/BLT.08.052175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Becher H, Müller O, Jahn A, Gbangou A, Kynast-Wolf G, Kouyaté B. Risk factors of infant and child mortality in rural Burkina Faso. Bull World Health Organ. 2004;82:265–73. [PMC free article] [PubMed] [Google Scholar]
- 24.Van den Broeck J, Eeckels R, Massa G. Maternal determinants of child survival in a rural African community. Int J Epidemiol. 1996;25:998–1004. doi: 10.1093/ije/25.5.998. [DOI] [PubMed] [Google Scholar]
- 25.Armstrong Schellenberg JR, Mrisho M, Manzi F, Shirima K, Mbuya C, Mushi AK, et al. Health and survival of young children in southern Tanzania. BMC Public Health. 2008;8:194. doi: 10.1186/1471-2458-8-194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Handbook: IMCI integrated management of childhood illness Geneva: World Health Organization and United Nations Children’s Fund; 2005.
- 27.Cuzick JAA. A Wilcoxon-type test for trend. Stat Med. 1985;4:87–90. doi: 10.1002/sim.4780040112. [DOI] [PubMed] [Google Scholar]
- 28.Buor D. Analysing the primacy of distance in the utilization of health services in the Ahafo-Ano South district, Ghana. Int J Health Plann Manage. 2003;18:293–311. doi: 10.1002/hpm.729. [DOI] [PubMed] [Google Scholar]
- 29.Mwabu G, Ainsworth M, Nyamete A. Quality of medical care and choice of medical treatment in Kenya: an empirical analysis. J Hum Resour. 1993;28:838–62. doi: 10.2307/146295. [DOI] [Google Scholar]
- 30.Acharya LB, Cleland J. Maternal and child health services in rural Nepal: does access or quality matter more? Health Policy Plan. 2000;15:223–9. doi: 10.1093/heapol/15.2.223. [DOI] [PubMed] [Google Scholar]
- 31.Molyneux CS, Murira G, Masha J, Snow RW. Intra-household relations and treatment decision-making for childhood illness: a Kenyan case study. J Biosoc Sci. 2002;34:109–31. [PubMed] [Google Scholar]
- 32.Chuma J, Gilson L, Molyneux C. Treatment-seeking behaviour, cost burdens and coping strategies among rural and urban households in Coastal Kenya: an equity analysis. Trop Med Int Health. 2007;12:673–86. doi: 10.1111/j.1365-3156.2007.01825.x. [DOI] [PubMed] [Google Scholar]
- 33.Noor AM, Omumbo JA, Amin AA, Zurovac D, Snow RW. Wealth, mother’s education and physical access as determinants of retail sector net use in rural Kenya. Malar J. 2006;5:5. doi: 10.1186/1475-2875-5-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moïsi JC, Kabuka J, Mitingi D, Levine OS, Scott JAG. Spatial and socio-demographic predictors of time-to-immunization in a rural area in Kenya: Is equity attainable? Vaccine. 2010;28:5725–30. doi: 10.1016/j.vaccine.2010.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]