Abstract
It has been discovered recently that toll-like receptors (TLRs) are key mediators of tissue injury in response to stroke. This revelation has identified a new target critical to understanding the underlying mechanisms of stroke injury and potential therapies. Much of the interest in TLRs centers around their ability to self regulate – a process commonly referred to as “tolerance,” wherein prior exposure to low level TLR activation induces protection against a subsequent challenge that would otherwise cause damage. This endogenous process has been exploited in the setting of stroke. Recent studies show that TLR pathways can be reprogrammed via prior exposure to TLR ligands leading to decreased infarct size and improved neurological outcomes in response to ischemic injury. Efforts to understand the molecular mechanisms of TLR reprogramming have led to the identification of multiple routes of TLR regulation including inhibitors that target signaling mediators, microRNAs that suppress genes post-transcriptionally, and epigenetic changes in chromatin remodeling that affect global gene regulation. In this review, we discuss the role of TLRs in mediating injury due to stroke, evidence for TLR preconditioning-induced TLR reprogramming in response to stroke, and possible mechanisms of TLR-induced neuroprotection.
Keywords: Toll-like receptors, endotoxin tolerance, stroke, neuroprotection
Brief Introduction to Toll-like Receptors
Toll-like receptors (TLRs) are an evolutionary conserved family of receptors considered to be a major component of innate immunity. There are 13 TLR family members characterized structurally as single membrane spanning type I glycoproteins [1]. The extracellular domains of the TLRs contain leucine-rich repeats that recognize pathogen associated molecular patterns (PAMPs) [1]. Association with its cognate PAMP leads to TLR activation and recruitment of adaptor molecules that associate with the intracellular Toll/interleukin-1 receptor (TIR) domain of the TLR to initiate signal transduction. Two major adaptor molecules known to associate with TLRs are myeloid differentiation factor-88 (MyD88) and TIR-domain-containing adaptor inducing IFNβ (TRIF). MyD88 associates with all TLRs, except for TLR3, which exclusively associates with TRIF. TLR4 has unique signaling properties due to its ability to associate with both MyD88 and TRIF. TLR signaling culminates in NFκB and IRF transcription, although, the degree and temporal profile of activation through the individual receptor depends on several factors including ligand characteristics and cell type (for extended review on TLR signaling [2]). NFκB activation promotes an inflammatory response that leads to the production of pro-inflammatory cytokines including TNFα, IL-1, and IL-6. Activation of IRF transcription leads to the production of anti-inflammatory molecules such as IL-10 and TGFβ and the induction of Type I IFN-associated molecules including IFNβ. While these TLR signaling cascades were first described as defensive responses against foreign pathogens, recent evidence also implicates TLR signaling in response to other danger signals such as tissue injury.
TLRs and Injury
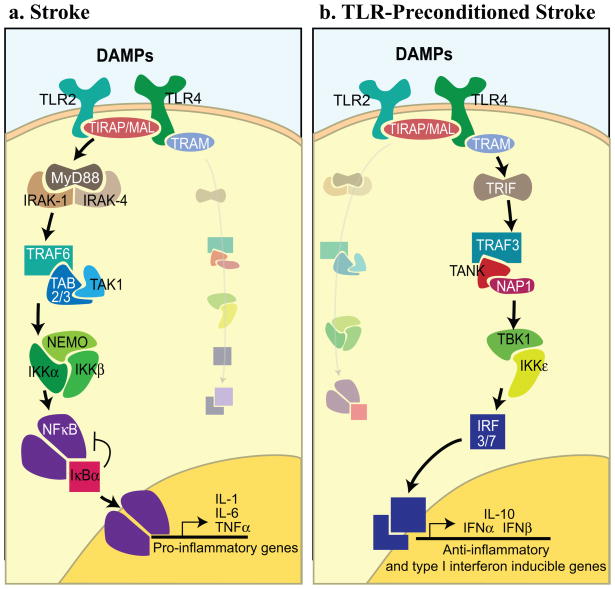
Tissue injury induces the release of endogenous molecules that contain damage associated molecular patterns (DAMPs). Evidence suggests that TLRs associate with DAMPs to initiate a robust inflammatory response that exacerbates tissue damage [3–6], although which DAMPs are involved remains unclear [7–10] (Fig. 1A). Of interest, TLRs have been shown to mediate ischemic injury in tissues including the kidney, liver, heart, and brain [3–6].
Figure 1.
Schematic of TLR signaling in response to stroke. A. TLR4 and TLR2 are activated in response to endogenous mediators, known as DAMPs, released by damaged tissue during stroke. TLR4 and TLR2 signal through MyD88 and promote NFκB nuclear translocation and induction of pro-inflammatory cytokines known to worsen tissue injury. B. TLR preconditioning leads to dampened signaling through TLR4 and TLR2 in the setting of stroke. MyD88 signal transduction is suppressed while the TRIF signaling cascade is amplified promoting activation of the IRF3 and IRF7 transcription factors that produce anti-inflammatory and Type I IFN-associated responses.
TLRs: Mediators of Ischemic Injury
A common theme of ischemic injury is the rapid induction of NFκB activity and production of potent inflammatory mediators including TNFα, IL-6, and IL-1β (Fig. 1A) [11–13]. TLRs have become the center of intense scrutiny as a major component of ischemic tissue damage. For example, several studies with TLR4 knockout mice in multiple models of ischemia have shown decreased tissue damage that corresponds with decreased NFκB activity and suppression of pro-inflammatory cytokines [3, 4, 6]. The role of TLRs in ischemic brain injury is the primary focus of this review.
Ischemic Brain Injury
TLR4 and TLR2 are the most extensively studied TLRs in ischemic brain injury (Figure 1A). Expression of TLR4 has been shown to be upregulated on glial cells in vitro and in vivo in response to hypoxic conditions or ischemia, respectively [4, 14]. Microglia cultured in vitro had increased levels of TLR4 mRNA and protein in response to exposure to varying durations of hypoxia [14]. A model of permanent middle cerebral artery occlusion (pMCAO) showed increased TLR4 on microglia and astrocytes 24 hours post occlusion compared to controls [4]. Mouse models of pMCAO and transient MCAO (tMCAO) result in significantly smaller infarcts and improved behavioral outcomes at several timepoints measured post occlusion in TLR4 null mutants compared to wild type mice [4, 15–17]. These TLR4 deficient mice also demonstrated significant suppression of IκB phosphorylation, NFκB activity, and pro-inflammatory cytokines including TNFα and IL-6 [16, 17]. Several additional major known mediators of brain damage were also reduced in TLR4 deficient mice including inducible nitric oxide synthase (iNOS), cyclooxygenase-2 (COX-2), and matrix metalloproteinase-9 (MMP9) [4, 15].
Similar to TLR4, expression of TLR2 mRNA and protein are upregulated in cerebral ischemia but TLR2 has been reported to be upregulated to a greater extent than TLR4 [18]. In particular, TLR2 protein expression is observed on neurons, astrocytes, endothelial cells, and most extensively on lesion-associated microglia following stroke [18, 19]. TLR2 deficient mice had significantly decreased infarct size in response to MCAO compared to wild type mice [18, 19]. Interestingly, TLR2 deficiency did not affect infiltration of peripheral cells to the site of injury [19], suggesting that TLR2 in the CNS is the direct source of the damaging signal.
Collectively, this evidence implicates TLR4 and TLR2 as critical mediators of injury induced by cerebral ischemia; thus, these two receptors are potential therapeutic targets.
TLR Tolerance
TLR tolerance has been studied for decades and is characterized as the induction of a hyporesponsive state following low dose stimulation with a TLR ligand. TLR tolerance can be in the form of either homotolerance or hetertolerance. Homotolerance occurs when a TLR is primed by its ligand and becomes hyporesponsive to the same ligand, best exemplified by endotoxin tolerance whereby prior endotoxin exposure leads to tolerance to subsequent endotoxin. Hetertolerance is induced by stimulating a TLR with its specific ligand to promote hyporesponsiveness in response to a different TLR and ligand, illustrated by treatment with the TLR9 ligand CpG to decrease TNFα secretion in response to the TLR4 ligand LPS [20]. Both tolerant states result in a reduction of pro-inflammatory signaling that can be protective against detrimental outcomes such as shock or injury.
Signaling in TLR Tolerance
TLR tolerance has been observed in multiple systems in vitro and in vivo [20–26]. A major premise of TLR tolerance is the that pro-inflammatory cytokines associated with NFκB activation including TNFα, IL-6, and IL-1β are downregulated during the hyporesponsive or “tolerized” state while anti-inflammatory genes associated with IRF activation including IL-10, TGFβ, and Type I IFNs are upregulated [27]. These changes in the TLR cytokine profile are attributed to reprogramming of the TLR signaling cascade; however, this reprogrammed TLR response has yet to be fully defined. Many investigators have suggested a key role for the TRIF-mediated TLR signaling cascade in tolerance [20, 21]. One study suggests that priming TLR-4, 5, 7, or 9 with their respective ligands promoted signaling initially through MyD88, while the secondary stimulation with a high dose of LPS resulted in reduced MyD88 signaling and enhanced TRIF signal transduction leading to an increased production of IFNβ [20]. Research suggests that this initial TLR response via MyD88 is required to prime the system to create the reprogrammed TLR signaling through TRIF [20, 28]. Further evidence for a key role of TRIF-signaling in TLR tolerance is demonstrated by the lack of TNFα suppression in TRIF and IRF3 knockout animals in endotoxin tolerance [21]. Reduction of MyD88 dependent TLR signaling is a possible mechanism for the decreased NFκB activity and pro-inflammatory cytokines observed in tolerance while enhanced TRIF signaling would increase IRF activity promoting an increase in anti-inflammatory and Type I IFN-associated genes.
TLR Tolerance in Ischemic Brain Injury
We and others have taken advantage of the concepts of TLR tolerance to study the role of TLRs in promoting neuroprotection in cerebral ischemia. TLR-induced homotolerance and heterotolerance can be induced to attenuate the damaging response of TLR2 and TLR4 in stroke. Stimulating TLRs with a low dose of ligand prior to stroke has led to a decrease in infarct size and improved neurological outcome. To date, exogenous preconditioning stimuli that utilize TLRs include the ligands for TLR4, TLR2, and TLR9. Furthermore, recent evidence suggests that the robust endogenous stimulus of short-lived ischemia mediates preconditioning through TLR4 [29] although, the nature of the endogenous ligand that activates TLR4 in this setting is unclear.
TLR4
TLR4-induced neuroprotection was first demonstrated with a low dose of LPS that decreased infarct size in a model of pMCAO in rats [30]. This neuroprotection depends on TNFα [30] and its downstream mediator, ceramide [31]. Studies with LPS preconditioning demonstrated that blocking TNFα inhibits neuroprotection[30]. In addition, TNFα knockout mice were not protected by LPS in a model of tMCAO [32], further implicating TNFα. Quantification of circulating levels of TNFα and TNFα convertase (TACE) activity show significant increases following administration of a low dose of LPS [32]. However, following tMCAO, levels of circulating TNFα and neuronal TNF receptor 1 were both significantly reduced compared to controls [32]. These data suggest that increased NFκB activity and inflammation prior to stroke may be necessary to establish neuroprotection, but following stroke in preconditioned mice, NFκB activity is decreased and inflammation is reduced. Microarray analysis of genes induced by preconditioning with LPS indicated that 50% of the primary genes upregulated were associated with a defense/inflammatory response [24]. In contrast, following stroke, LPS-preconditioned animals exhibited a pattern of gene expression where Type I IFN-associated transcriptional regulatory elements (TREs) were overrepresented [24]. Many of these Type I IFN-associated genes are controlled by IRFs, which are downstream of the TRIF signaling pathway. Interestingly, IRF3 knockout mice are not protected by LPS-preconditioning, which suggest that IRF3 transcription is necessary for TLR4-induced neuroprotection [24]. Taken together, these data indicate that following LPS stimulation, the MyD88-NFκB pathway is initiated leading to upregulation of TNFα and other pro-inflammatory genes. Subsequently, TLR signaling in response to cerebral ischemia is predominantly mediated through the TRIF-IRF pathway initiating transcription of Type I IFN-associated genes and downregulation of proinflammatory cytokines, such as TNFα.
TLR2
Preconditioning with the TLR2 ligand, Pam3CysSerLys4 (Pam3CSK4), has been shown to be neuroprotective [33]. In this study, preconditioning with Pam3CSK4 24 hours prior to tMCAO significantly decreased infarct size and mortality while improving neurological outcome in mice. Interestingly, the Pam3CSK4 preconditioned animals showed decreased blood-brain-barrier (BBB) permeability that correlated with increased maintenance of endothelial cell tight junctions [33]. While the signaling cascades have not been fully elucidated in this system, IFNβ has been shown by others to protect the integrity of the BBB [34, 35]. Thus, neuroprotection induced by TLR2 preconditioning may also be associated with a robust Type I IFN response.
TLR9
It has been demonstrated that preconditioning with the TLR9 ligand, unmethylated CpG oligodeoxynucleotides (ODNs), is neuroprotective in tMCAO [36]. Like TLR4, TLR9 preconditioning increases TNFα levels prior to tMCAO, and TNFα is required for CpG-ODN-induced neuroprotection [36]. Genomic expression analysis revealed that CpG ODN preconditioning induced transcriptional changes following tMCAO in blood leukocytes and the brain that favored the TREs GATA-3 and Type I IFN, respectively [37]. In the blood, GATA-3 is associated with natural killer (NK) cell development [38], suggesting that there is increased NK cell activity in CpG ODN-preconditioning following stroke. In the brain, the increase in Type I IFN-associated signaling is linked to IRF activity [37]. This is similar to TLR4 and further implicates the TRIF-IRF pathway as a dominant player in TLR preconditioning-induced neuroprotection.
Ischemic Preconditioning (IPC)
Preconditioning by exposure to a brief period of ischemia prior to a longer period of ischemia leads to robust neuroprotection. The induction of NFκB activation prior to stroke appears to be critical to initiate neuroprotection associated with IPC [39]. A major role for TNFα has also been suggested in IPC, demonstrated by significant upregulation of TACE/ADAM17 that increased systemic TNFα levels following IPC in a rat model of tMCAO [40]. Inhibition of TACE blocked IPC-induced neuroprotection [40]. IPC dependence on NFκB activity and TNFα resembles TLR4 and TLR9 preconditioning suggesting that IPC may be mediated by TLR MyD88-NFκB signaling. Consistent with this idea, TLR4 knockout mice show decreased neuroprotection induced by IPC in response to pMCAO [29]. TLR4 knockout mice subjected to IPC had reduced NFκB activity and pro-inflammatory responses, including TNFα, COX-2, and iNOS, prior to stroke [29]. This suggests that TLR4 activation leading to an NFκB dependent pro-inflammatory response is required prior to stroke to set up a neuroprotective state induced by IPC.
Summary of TLR Preconditioning
The examples of TLR-dependent preconditioning described above suggest two major features of TLR-preconditioning induced neuroprotection. First, signaling through NFκB to promote a modest pro-inflammatory response is required prior to stroke to induce neuroprotection. Second, following stroke, the TLR response to cerebral ischemic injury is reprogrammed to preferentially promote a Type I IFN-dominant response, possibly through enhanced TRIF-IRF signaling (Figure 1B). These features are shared between TLR preconditioning in the brain and classical TLR tolerance, which suggests that the molecular mechanisms that govern these two processes may overlap.
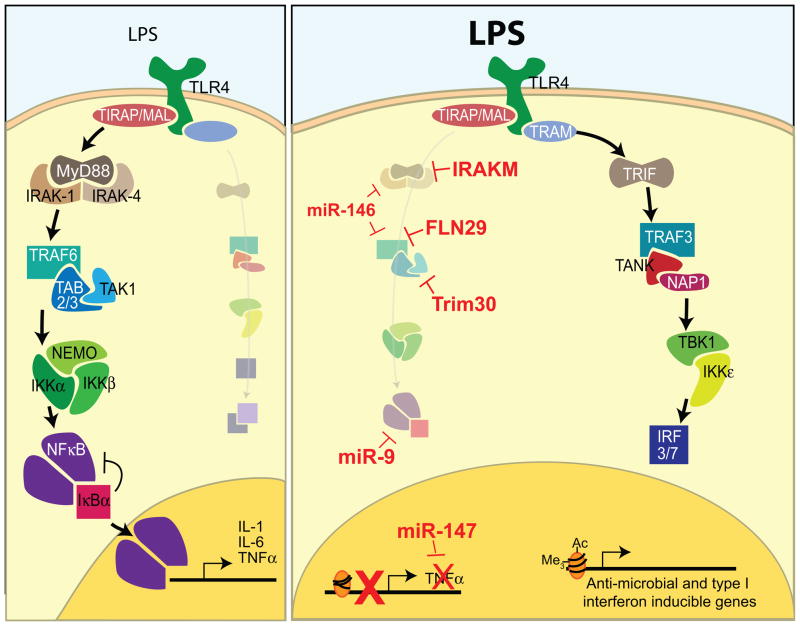
Mechanisms of TLR Reprogramming
Regulation of TLR reprogramming is complex and likely relies on multiple mechanisms to promote the altered TLR response seen in tolerance and preconditioning-induced neuroprotection. We believe that the knowledge gathered from extensive research on the molecular mechanisms of classical endotoxin tolerance can be applied to TLR preconditioning and stroke to understand the mechanisms of neuroprotection. Several possible mechanisms of TLR regulation have been described and can be classified into three major categories: (1) negative feedback systems targeting TLR signal transduction, (2) post-transcriptional gene regulation, and (3) globally orchestrated epigenetic changes (Figure 2). It is notable that the majority of mechanisms described to date target inhibition or reduction of the MyD88 signaling cascade and NFκB activity suggesting the existence of an evolutionarily conserved endogenous system within the cell designed to control pro-inflammatory responses.
Figure 2.
Mechanisms of endotoxin tolerance. Left: Model of the primary TLR4 signaling cascade initiated in response to a low dose of LPS. Signaling commences through the MyD88 adaptor leading to NFκB activation producing a low level inflammatory response. Evidence suggests that this primary signaling cascade is required to induce a “tolerized” state. Right: Schematic of the TRIF-dominated response of TLR4 in endotoxin tolerance. Many inhibitors are in place to reduce MyD88 signaling and NFκB activity. The mechanisms that are utilized to create this reprogrammed TLR response include targeted inhibition of signal transduction (IRAKM, FLN29, TRIM30), microRNAs that regulate post transcriptional gene regulation (miR-9, 146, 157), and chromatin remodeling that promotes or suppresses gene expression.
Negative Feedback
TLRs respond to low doses of ligand by producing several negative inhibitors of TLR signaling. Many of the negative inhibitors discovered thus far target the MyD88 signaling cascade and NFκB although a role for TRIF inhibitors is beginning to emerge. The negative inhibitors IRAK-M, FLN29, and TRIM30 target signal transduction at distinct points in the MyD88 signaling cascade (Figure 2). IRAK-M acts as a dominant negative form of IRAK-1, displacing IRAK-1 to prevent further signaling [41, 42]. FLN29 interacts with and inhibits TRAF6 [43]. TRIM30 acts as a negative inhibitor by promoting the degradation of TAB2 and TAB3 [44]. Interestingly, TRIM30 is upregulated in the brain following stroke in LPS-preconditioned animals [24]. Inhibitors of TRIF signaling SARM and TAG have been identified but their role in TLR tolerance is incompletely understood. SARM has been shown to associate with and inhibit TRIF [45]. TAG displaces TRAM from TRIF, preventing TRIF-mediated signaling [46].
Post-Transcriptional Gene Regulation
MicroRNAs (miRNA) are endogenous non-coding RNAs that function in post-transcriptional gene regulation. Mature miRNA is made up of approximately 22 nucleotides and associates with the RNA-induced silencing complex that, with the help of accessory proteins, guides miRNA for the targeted degradation of mRNA transcripts and inhibition of protein translation [47]. Thus far, several miRNAs have been identified as inducible by TLR activation, and each function to inhibit MyD88 signaling and NFκB activity. In particular, in response to LPS, miR-146 is induced by NFκB and functions to inhibit production of IRAK-1 and TRAF6 [48]. Multiple TLRs have been shown to induce miR-9 and miR-147 [49, 50]. Upregulation of miR-9 targets NFKB1, a precursor to the NFκB subunit p50, for degradation at the level of mRNA and protein translation [49]. The induction of miR-147 requires both NFκB and IRF3 activity and results in a diminished inflammatory cytokine profile [50]. In contrast, miRNA expression can also function to promote an inflammatory response. The coordinated upregulation of miR-155 and downregulation of miR-125b have been shown to promote the induction of TNFα production immediately following LPS stimulation [51]. A role for miRNAs in preconditioning and cerebral ischemia is already beginning to be established showing that miRNAs are differentially regulated by stroke in the presence or absence of IPC [52, 53].
Epigenetics
Epigenetic changes focus on the chromosomal level of gene regulation mediated by chromatin remodeling. Nucleosome repositioning and histone modifications are two mechanisms of epigenetic changes that affect gene expression.
A recent study investigated the repositioning of the two proximal nucleosomes that make up the TNFα promoter during endotoxin tolerance [54]. TLR4 stimulation with LPS led to repositioning of the two nucleosomes to allow access to the κB binding site of the promoter leading to the induction of TNFα [54]. In contrast, in a “tolerized” state, the nucleosomes are positioned in a repressive manner that blocks the κB binding site of the promoter [54]. Nucleosome repositioning is mediated by chromatin remodeling complexes, including NAP1 and BAF [54]. These data indicate that one mechanism of TLR reprogramming may be through induction of nucleosome repositioning to specifically promote or repress transcription by modulating access to the promoter region of specific genes.
Histone modification is another mechanism by which chromatin remodeling affects gene expression. Acetylated or methylated histones indicate transcriptionally active chromatin while deacetylated or histones lacking methylation are markers of chromatin inactivation [55]. A recent study investigating histone modification in endotoxin tolerance established two classes of genes: (1) tolerizable genes, which are not induced in the reprogrammed TLR4 response and (2) non-tolerizable genes, which are induced in the reprogrammed TLR4 response. Both identified genes sets were acetylated at histone protein 4 upon the first stimulation of LPS, but only non-tolerizable genes were re-acetylated during the second LPS stimulation [55]. Additionally, methylation of histone protein 3 was lost on tolerizable genes but maintained on non-tolerizable genes in endotoxin tolerance [55]. These changes in histone modification translated to a shift in the TLR4 response in endotoxin tolerance, where non-tolerizable genes became the primary genes induced by TLR4 signaling in response to the second challenge with LPS. Interestingly, the tolerizable class of genes are primarily related to inflammation while the non-tolerizable class of genes are mainly anti-microbial, many of which are Type I IFN-associated genes [55]. Thus, histone modifications in endotoxin tolerance create conditions in which pro-inflammatory gene transcription is inactivated and anti-microbial/IFN-associated gene transcription is preferentially activated. These types of epigenetic changes may orchestrate the preconditioning-induced shift in TLR signaling towards a neuroprotective response to stroke.
TLR Therapeutic Potential
TLR preconditioning offers a promising prophylactic treatment for high risk patients to promote neuroprotection through endogenous mechanisms. High risk patients that could benefit from prophylactic TLR agonists are those with significant risk of suffering from a stroke within a predictable timeframe, such as patients that have had a transient ischemic attack (TIA) or are undergoing cardiovascular surgery. Approximately 300,000 people experience a TIA each year in the United States [56]. Within 90 days following a TIA, 10.5% of these patients will suffer from a severe stroke, the majority of which occur within 2 days of the primary TIA [56]. Research indicates that more than 99% of individuals diagnosed with a TIA arrived at the hospital within 1 day of the onset of their symptoms [56]. Thus, these patients are prime candidates for TLR preconditioning to protect the brain against a subsequent debilitating stroke. Others that would benefit from prophylactic TLR therapy are those undergoing cardiovascular surgery such as coronary artery bypass grafting (CABG) [57–60], of which approximately 43% would be expected to experience new ischemic lesions postoperatively that can contribute to increased cognitive decline [60] and mortality [57]. The majority of cerebral ischemia associated with CABG or other cardiovascular surgical procedures occur by postoperative day 2 [57]. Administration of TLR agonists prior to surgery would be able to provide a neuroprotective window for several days thereby minimizing the risk of significant tissue damage due to ischemia.
Additionally, the study of TLR-mediated neuroprotective mechanisms may lead to the identification of promising therapeutic targets for acute treatment. For example, much of the evidence cited in this review centers on the dominance of TRIF-mediated signaling in neuroprotection induced by TLR preconditioning. Thus, treatment that can activate TRIF signaling may prove to be neuroprotective. Support for this lies in the finding that primary cortical cells treated with PolyI:C, the TLR3 ligand which signals exclusively through TRIF, are protected from cell death in the setting of ischemia modeled in vitro [24]. Furthermore, the endogenous mechanisms utilized to promote the reprogrammed TLR response, such as miRNA, through regulation of gene and protein expression, may be a promising avenue for dampening damaging TLR signaling while promoting neuroprotective responses at the time of stroke. Taken together, TLRs are a promising strategy to promote neuroprotection that is clinically relevant. TLRs offer an important platform for the study of endogenous mechanisms of neuroprotection that are critical to our understanding and long-term treatment of stroke.
Perspectives
This article addresses new data that identifies a key role for TLRs in mediating damage due to injury. The extension of TLR function beyond sensors of foreign pathogens to internal surveillance receptors for endogenous signals of cell damage fundamentally changes our understanding of injury and disease. Importantly, preconditioning can be used to manipulate TLRs to respond to damage in a protective manner. This implies that there is an evolutionarily conserved molecular switch between TLR activation of injurious pro-inflammatory responses to protective anti-inflammatory responses. Promoting this molecular switch using TLR preconditioning is a promising antecedent therapy for patients at high risk for stroke. As we move forward in our efforts to characterize the TLR-preconditioning induced protective phenotype, two major components of neuroprotective signal transduction have become evident. First, NFκB suppression and subsequent attenuation of inflammation appears to be required for protection. Second, an anti-inflammatory and Type I IFN response is predominant in the preconditioning-induced neuroprotection, suggesting enhancement of the TRIF branch of TLR signaling. How TLR-preconditioning reprograms the TLR response still remains unclear, but the established mechanisms of endotoxin tolerance provide promising leads for this line of investigation. Delineating the mechanisms that regulate this protective TLR cascade offers great promise for the development of an acute stroke therapy that will directly induce a neuroprotective TLR signaling program.
Acknowledgments
The authors wish to acknowledge the support from the National Institute of Neurological Disorders and Stroke (NS062381). We would like to thank Tiffani Howard for the graphics.
References
- 1.Jin MS, Lee JO. Structures of the toll-like receptor family and its ligand complexes. Immunity. 2008 Aug 15;29(2):182–91. doi: 10.1016/j.immuni.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 2.Akira S, Takeda K. Toll-like receptor signalling. Nat Rev Immunol. 2004 Jul;4(7):499–511. doi: 10.1038/nri1391. [DOI] [PubMed] [Google Scholar]
- 3.Wang H, Li ZY, Wu HS, Wang Y, Jiang CF, Zheng QC, et al. Endogenous danger signals trigger hepatic ischemia/reperfusion injury through toll-like receptor 4/nuclearfactor-kappa B pathway. Chinese medical journal. 2007 Mar 20;120(6):509–14. [PubMed] [Google Scholar]
- 4.Caso JR, Pradillo JM, Hurtado O, Lorenzo P, Moro MA, Lizasoain I. Toll-like receptor 4 is involved in brain damage and inflammation after experimental stroke. Circulation. 2007 Mar 27;115(12):1599–608. doi: 10.1161/CIRCULATIONAHA.106.603431. [DOI] [PubMed] [Google Scholar]
- 5.Zhang B, Ramesh G, Uematsu S, Akira S, Reeves WB. TLR4 signaling mediates inflammation and tissue injury in nephrotoxicity. J Am Soc Nephrol. 2008 May;19(5):923–32. doi: 10.1681/ASN.2007090982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chong AJ, Shimamoto A, Hampton CR, Takayama H, Spring DJ, Rothnie CL, et al. Toll-like receptor 4 mediates ischemia/reperfusion injury of the heart. J Thorac Cardiovasc Surg. 2004 Aug;128(2):170–9. doi: 10.1016/j.jtcvs.2003.11.036. [DOI] [PubMed] [Google Scholar]
- 7.Lee KM, Seong SY. Partial role of TLR4 as a receptor responding to damage-associated molecular pattern. Immunology letters. 2009 Jun 30;125(1):31–9. doi: 10.1016/j.imlet.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 8.Erridge C. Endogenous ligands of TLR2 and TLR4: agonists or assistants? J Leukoc Biol. Feb 23; doi: 10.1189/jlb.1209775. [DOI] [PubMed] [Google Scholar]
- 9.Zhang Q, Raoof M, Chen Y, Sumi Y, Sursal T, Junger W, et al. Circulating mitochondrial DAMPs cause inflammatory responses to injury. Nature. Mar 4;464(7285):104–7. doi: 10.1038/nature08780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smiley ST, King JA, Hancock WW. Fibrinogen stimulates macrophage chemokine secretion through toll-like receptor 4. J Immunol. 2001 Sep 1;167(5):2887–94. doi: 10.4049/jimmunol.167.5.2887. [DOI] [PubMed] [Google Scholar]
- 11.Huang J, Upadhyay UM, Tamargo RJ. Inflammation in stroke and focal cerebral ischemia. Surgical neurology. 2006 Sep;66(3):232–45. doi: 10.1016/j.surneu.2005.12.028. [DOI] [PubMed] [Google Scholar]
- 12.Hill J, Gunion-Rinker L, Kulhanek D, Lessov N, Kim S, Clark W, et al. Temporal modulation of cytokine expression following focal cerebral ischemia in mice. Brain Res. 1999;820:45–54. doi: 10.1016/s0006-8993(98)01140-8. [DOI] [PubMed] [Google Scholar]
- 13.Saito K, Suyama K, Nishida K, Sei Y, Basile AS. Early increases in TNFalpha, IL6, and IL-1beta levels following transient cerebral ischemia in gerbil brain. Neurosci Lett. 1996;206:149–52. doi: 10.1016/s0304-3940(96)12460-5. [DOI] [PubMed] [Google Scholar]
- 14.Ock J, Jeong J, Choi WS, Lee WH, Kim SH, Kim IK, et al. Regulation of Toll-like receptor 4 expression and its signaling by hypoxia in cultured microglia. J Neurosci Res. 2007 Jul;85(9):1989–95. doi: 10.1002/jnr.21322. [DOI] [PubMed] [Google Scholar]
- 15.Caso JR, Pradillo JM, Hurtado O, Leza JC, Moro MA, Lizasoain I. Toll-like receptor4 is involved in subacute stress-induced neuroinflammation and in the worsening of experimental stroke. Stroke. 2008 Apr;39(4):1314–20. doi: 10.1161/STROKEAHA.107.498212. [DOI] [PubMed] [Google Scholar]
- 16.Cao CX, Yang QW, Lv FL, Cui J, Fu HB, Wang JZ. Reduced cerebral ischemia-reperfusion injury in Toll-like receptor 4 deficient mice. Biochem Biophys Res Comm. 2007 Feb 9;353(2):509–14. doi: 10.1016/j.bbrc.2006.12.057. [DOI] [PubMed] [Google Scholar]
- 17.Hua F, Ma J, Ha T, Xia Y, Kelley J, Williams DL, et al. Activation of Toll-like receptor 4 signaling contributes to hippocampal neuronal death following global cerebral ischemia/reperfusion. J Neuroimmunol. 2007 Oct;190(1–2):101–11. doi: 10.1016/j.jneuroim.2007.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ziegler G, Harhausen D, Schepers C, Hoffmann O, Rohr C, Prinz V, et al. TLR2 has a detrimental role in mouse transient focal cerebral ischemia. Biochem Biophys Res Comm. 2007 Aug 3;359(3):574–9. doi: 10.1016/j.bbrc.2007.05.157. [DOI] [PubMed] [Google Scholar]
- 19.Lehnardt S, Lehmann S, Kaul D, Tschimmel K, Hoffmann O, Cho S, et al. Toll-like receptor 2 mediates CNS injury in focal cerebral ischemia. J Neuroimmunol. 2007 Oct;190(1–2):28–33. doi: 10.1016/j.jneuroim.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 20.Broad A, Kirby JA, Jones DE. Toll-like receptor interactions: tolerance of MyD88-dependent cytokines but enhancement of MyD88-independent interferon-beta production. Immunology. 2007 Jan;120(1):103–11. doi: 10.1111/j.1365-2567.2006.02485.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Biswas SK, Bist P, Dhillon MK, Kajiji T, Del Fresno C, Yamamoto M, et al. Role for MyD88-independent, TRIF pathway in lipid A/TLR4-induced endotoxin tolerance. J Immunol. 2007 Sep 15;179(6):4083–92. doi: 10.4049/jimmunol.179.6.4083. [DOI] [PubMed] [Google Scholar]
- 22.Rowland RT, Meng X, Cleveland JC, Meldrum DR, Harken AH, Brown JM. LPS-induced delayed myocardial adaptation enhances acute preconditioning to optimize postischemic cardiac function. Am J Physiol. 1997;272:H2708–15. doi: 10.1152/ajpheart.1997.272.6.H2708. [DOI] [PubMed] [Google Scholar]
- 23.Obermaier R, Drognitz O, Grub A, Dobschuetz Ev, Schareck W, Hopt UT, et al. Endotoxin preconditioning in pancreatic ischemia/reperfusion injury. Pancreas. 2003;27(3):e51–6. doi: 10.1097/00006676-200310000-00020. [DOI] [PubMed] [Google Scholar]
- 24.Marsh B, Stevens SL, Packard AE, Gopalan B, Hunter B, Leung PY, et al. Systemic lipopolysaccharide protects the brain from ischemic injury by reprogramming the response of the brain to stroke: a critical role for IRF3. J Neurosci. 2009 Aug 5;29(31):9839–49. doi: 10.1523/JNEUROSCI.2496-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marsh B, Rosenzweig HL, Stevens SL, Hillary B, Gopalan B, Cannon W, et al. LPS induced preconditioning in the brain: a seminal role for NFkB in the establishment of tolerance to ischemic injury. Abstract, Society for Neuroscience Meeting; Washington, DC. 2005. [Google Scholar]
- 26.Lastres-Becker I, Carmell T, Molina-Holgado F. Endotoxin preconditioning protects neurons from in vitro ischemia: Role of endogenous IL-1beta and TNF-alpha. J Neuroimmunol. 2006;173:108–16. doi: 10.1016/j.jneuroim.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 27.Biswas SK, Lopez-Collazo E. Endotoxin tolerance: new mechanisms, molecules and clinical significance. Trends Immunol. 2009 Oct;30(10):475–87. doi: 10.1016/j.it.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 28.Bagchi A, Herrup EA, Warren HS, Trigilio J, Shin HS, Valentine C, et al. MyD88-dependent and MyD88-independent pathways in synergy, priming, and tolerance between TLR agonists. J Immunol. 2007 Jan 15;178(2):1164–71. doi: 10.4049/jimmunol.178.2.1164. [DOI] [PubMed] [Google Scholar]
- 29.Pradillo JM, Fernandez-Lopez D, Garcia-Yebenes I, Sobrado M, Hurtado O, Moro MA, et al. Toll-like receptor 4 is involved in neuroprotection afforded by ischemic preconditioning. J Neurochem. 2009 Apr;109(1):287–94. doi: 10.1111/j.1471-4159.2009.05972.x. [DOI] [PubMed] [Google Scholar]
- 30.Tasaki K, Ruetzler CA, Ohtsuki T, Martin D, Nawashiro H, Hallenbeck JM. Lipopolysaccharide pre-treatment induces resistance against subsequent focal cerebral ischemic damage in spontaneously hypertensive rats. Brain Res. 1997;748(1–2):267–70. doi: 10.1016/s0006-8993(96)01383-2. [DOI] [PubMed] [Google Scholar]
- 31.Furuya K, Ginis I, Takeda H, Chen Y, Hallenbeck J. Cell permeable exogenous ceramide reduces infarct size in spontaneously hypertensive rats supporting in vitro studies that have implicated ceramide in induction of tolerance to ischemia. J Cereb Blood Flow Metab. 2001;21:226–32. doi: 10.1097/00004647-200103000-00006. [DOI] [PubMed] [Google Scholar]
- 32.Rosenzweig HL, Minami M, Lessov NS, Coste SC, Stevens SL, Henshall DC, et al. Endotoxin preconditioning protects against the cytotoxic effects of TNFa after stroke: a novel role for TNFa in LPS-ischemic tolerance. J Cereb Blood Flow Metab. 2007;27:1663–74. doi: 10.1038/sj.jcbfm.9600464. [DOI] [PubMed] [Google Scholar]
- 33.Hua F, Ma J, Ha T, Kelley J, Williams DL, Kao RL, et al. Preconditioning with a TLR2 specific ligand increases resistance to cerebral ischemia/reperfusion injury. J Neuroimmunol. 2008 Aug 13;199(1–2):75–82. doi: 10.1016/j.jneuroim.2008.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kraus J, Voigt K, Schuller AM, Scholz M, Kim KS, Schilling M, et al. Interferon-beta stabilizes barrier characteristics of the blood-brain barrier in four different species in vitro. Multiple sclerosis (Houndmills, Basingstoke, England) 2008 Jul;14(6):843–52. doi: 10.1177/1352458508088940. [DOI] [PubMed] [Google Scholar]
- 35.Minagar A, Long A, Ma T, Jackson TH, Kelley RE, Ostanin DV, et al. Interferon (IFN)-beta 1a and IFN-beta 1b block IFN-gamma-induced disintegration of endothelial junction integrity and barrier. Endothelium. 2003;10(6):299–307. doi: 10.1080/10623320390272299. [DOI] [PubMed] [Google Scholar]
- 36.Stevens SL, Ciesielski TM, Marsh BJ, Yang T, Homen DS, Boule JL, et al. Toll-like receptor 9: a new target of ischemic preconditioning in the brain. J Cereb Blood Flow Metab. 2008;28(5):1040–7. doi: 10.1038/sj.jcbfm.9600606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marsh BJ, Stevens SL, Hunter B, Stenzel-Poore MP. Inflammation and the emerging role of the toll-like receptor system in acute brain ischemia. Stroke. 2009 Mar;40(3 Suppl):S34–7. doi: 10.1161/STROKEAHA.108.534917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim PJ, Pai SY, Brigl M, Besra GS, Gumperz J, Ho IC. GATA-3 regulates the development and function of invariant NKT cells. J Immunol. 2006 Nov 15;177(10):6650–9. doi: 10.4049/jimmunol.177.10.6650. [DOI] [PubMed] [Google Scholar]
- 39.Blondeau N, Widmann C, Lazdunsk M, Heurteaux C. Activation of the nuclear factor-kappaB is a key event in brain tolerance. J Neurosci. 2001;21(13):4668–77. doi: 10.1523/JNEUROSCI.21-13-04668.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cardenas A, Moro MA, Leza JC, O’Shea E, Davalos A, Castillo J, et al. Upregulation of TACE/ADAM17 after ischemic preconditioning is involved in brain tolerance. J Cereb Blood Flow Metab. 2002 Nov;22(11):1297–302. doi: 10.1097/01.WCB.0000033968.83623.D0. [DOI] [PubMed] [Google Scholar]
- 41.Escoll P, del Fresno C, Garcia L, Valles G, Lendinez MJ, Arnalich F, et al. Rapid up-regulation of IRAK-M expression following a second endotoxin challenge in human monocytes and in monocytes isolated from septic patients. Biochem Biophys Res Comm. 2003 Nov 14;311(2):465–72. doi: 10.1016/j.bbrc.2003.10.019. [DOI] [PubMed] [Google Scholar]
- 42.van’t Veer C, van den Pangaart PS, van Zoelen MA, de Kruif M, Birjmohun RS, Stroes ES, et al. Induction of IRAK-M is associated with lipopolysaccharide tolerance in a human endotoxemia model. J Immunol. 2007 Nov 15;179(10):7110–20. doi: 10.4049/jimmunol.179.10.7110. [DOI] [PubMed] [Google Scholar]
- 43.Mashima R, Saeki K, Aki D, Minoda Y, Takaki H, Sanada T, et al. FLN29, a novel interferon-and LPS-inducible gene acting as a negative regulator of toll-like receptor signaling. J Biol Chem. 2005 Dec 16;280(50):41289–97. doi: 10.1074/jbc.M508221200. [DOI] [PubMed] [Google Scholar]
- 44.Shi M, Deng W, Bi E, Mao K, Ji Y, Lin G, et al. TRIM30 alpha negatively regulates TLR-mediated NF-kappa B activation by targeting TAB2 and TAB3 for degradation. Nat Immunol. 2008 Apr;9(4):369–77. doi: 10.1038/ni1577. [DOI] [PubMed] [Google Scholar]
- 45.Carty M, Goodbody R, Schroder M, Stack J, Moynagh PN, Bowie AG. The human adaptor SARM negatively regulates adaptor protein TRIF-dependent Toll-like receptor signaling. Nat Immunol. 2006 Oct;7(10):1074–81. doi: 10.1038/ni1382. [DOI] [PubMed] [Google Scholar]
- 46.Palsson-McDermott EM, Doyle SL, McGettrick AF, Hardy M, Husebye H, Banahan K, et al. TAG, a splice variant of the adaptor TRAM, negatively regulates the adaptor MyD88-independent TLR4 pathway. Nat Immunol. 2009 Jun;10(6):579–86. doi: 10.1038/ni.1727. [DOI] [PubMed] [Google Scholar]
- 47.Carthew RW, Sontheimer EJ. Origins and Mechanisms of miRNAs and siRNAs. Cell. 2009 Feb 20;136(4):642–55. doi: 10.1016/j.cell.2009.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Taganov KD, Boldin MP, Chang KJ, Baltimore D. NF-kappaB-dependent induction of microRNA miR-146, an inhibitor targeted to signaling proteins of innate immune responses. Proc Natl Acad Sci U S A. 2006 Aug 15;103(33):12481–6. doi: 10.1073/pnas.0605298103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bazzoni F, Rossato M, Fabbri M, Gaudiosi D, Mirolo M, Mori L, et al. Induction and regulatory function of miR-9 in human monocytes and neutrophils exposed to proinflammatory signals. Proc Natl Acad Sci U S A. 2009 Mar 31;106(13):5282–7. doi: 10.1073/pnas.0810909106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liu G, Friggeri A, Yang Y, Park YJ, Tsuruta Y, Abraham E. miR-147, a microRNA that is induced upon Toll-like receptor stimulation, regulates murine macrophage inflammatory responses. Proc Natl Acad Sci U S A. 2009 Sep 15;106(37):15819–24. doi: 10.1073/pnas.0901216106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tili E, Michaille JJ, Cimino A, Costinean S, Dumitru CD, Adair B, et al. Modulation of miR-155 and miR-125b levels following lipopolysaccharide/TNF-alpha stimulation and their possible roles in regulating the response to endotoxin shock. J Immunol. 2007 Oct 15;179(8):5082–9. doi: 10.4049/jimmunol.179.8.5082. [DOI] [PubMed] [Google Scholar]
- 52.Lusardi TA, Farr CD, Faulkner CL, Pignataro G, Yang T, Lan J, et al. Ischemic preconditioning regulates expression of microRNAs and a predicted target, MeCP2, in mouse cortex. J Cereb Blood Flow Metab. Apr;30(4):744–56. doi: 10.1038/jcbfm.2009.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jeyaseelan K, Lim KY, Armugam A. MicroRNA expression in the blood and brain of rats subjected to transient focal ischemia by middle cerebral artery occlusion. Stroke. 2008 Mar;39(3):959–66. doi: 10.1161/STROKEAHA.107.500736. [DOI] [PubMed] [Google Scholar]
- 54.El Gazzar M, Liu T, Yoza BK, McCall CE. Dynamic and selective nucleosome repositioning during endotoxin tolerance. J Biol Chem. Jan 8;285(2):1259–71. doi: 10.1074/jbc.M109.067330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Foster SL, Hargreaves DC, Medzhitov R. Gene-specific control of inflammation by TLR-induced chromatin modifications. Nature. 2007 Jun 21;447(7147):972–8. doi: 10.1038/nature05836. [DOI] [PubMed] [Google Scholar]
- 56.Johnston SC, Gress DR, Browner WS, Sidney S. Short-term prognosis after emergency department diagnosis of TIA. J Am Med Assoc. 2000 Dec 13;284(22):2901–6. doi: 10.1001/jama.284.22.2901. [DOI] [PubMed] [Google Scholar]
- 57.McKhann GM, Grega MA, Borowicz LM, Jr, Baumgartner WA, Selnes OA. Stroke and encephalopathy after cardiac surgery: an update. Stroke. 2006 Feb;37(2):562–71. doi: 10.1161/01.STR.0000199032.78782.6c. [DOI] [PubMed] [Google Scholar]
- 58.Bond R, Rerkasem K, Shearman CP, Rothwell PM. Time trends in the published risks of stroke and death due to endarterectomy for symptomatic carotid stenosis. Cerebrovasc Dis. 2004;18(1):37–46. doi: 10.1159/000078606. [DOI] [PubMed] [Google Scholar]
- 59.Bucerius J, Gummert JF, Borger MA, Walther T, Doll N, Onnasch JF, et al. Stroke after cardiac surgery: a risk factor analysis of 16,184 consecutive adult patients. Ann Thorac Surg. 2003 Feb;75(2):472–8. doi: 10.1016/s0003-4975(02)04370-9. [DOI] [PubMed] [Google Scholar]
- 60.Barber PA, Darby DG, Desmond PM, Gerraty RP, Yang Q, Li T, et al. Identification of major ischemic change. Diffusion-weighted imaging versus computed tomography. Stroke. 1999 Oct;30(10):2059–65. doi: 10.1161/01.str.30.10.2059. [DOI] [PubMed] [Google Scholar]