SUMMARY
Reinke’s Space Oedema is characterized by a subepithelial collection of fluid and pseudo-myxomatous tissue within the lamina propria superficialis of the vocal cord. We have observed, in a number of cases, the phenomenon of bilobular and/or centrally located Reinke’s Space Oedema. Bilobular oedema occurs when the sub-epithelial oedema is organised as a double bulge of the vocal cord in the superoinferior plane due to adhesions or sulcus at the free edge of the vocal cord. Herewith, a simple, yet easily reproducible, modified technique is presented of an “M” shaped microflap for the treatment of bilobular and also centrally located Reinke’s Space Oedema of the vocal cords, using Carbon Dioxide laser and/or cold micro instruments allowing maintenance of an appropriate amount of lamina propria superficialis and easy coverage of the potentially exposed part of the ligament. Our technique involves removal of the upper bulge of the affected vocal cord with Carbon Dioxide laser or cold instruments, followed by an “M” shaped remodelling of the microflap so that the mucosa can be effectively draped over the lamina propria superficialis and vocal ligament.
KEY WORDS: Vocal cords, Reinke’s Space Oedema, Microflap, Polypoid degeneration of the vocal cords, Phonosurgery
RIASSUNTO
L’edema dello spazio di Reinke è in genere caratterizzato dall’accumulo subepiteliale di fluido all’interno della lamina propria superficiale e degenerazione ialina cui può associarsi proliferazione fibroblastica. L’edema può essere monolaterale, bilaterale, semplice o complesso, talvolta associato a lesioni come sulcus, vergeture, polipi o lesioni precancerose. Abbiamo notato in diversi casi il fenomeno di edema dello spazio di Reinke bilobato mono- o bilaterale; ciò avviene quando l’edema subepiteliale si organizza su due piani diversi in senso cranio-caudale con piano di separazione al margine libero della corda vocale. Il trattamento chirurgico con tecnica del microflap rappresenta attualmente il trattamento di eccellenza dell’edema dello spazio di Reinke. La tecnica prevede l’uso di strumentario “freddo” per l’incisione e l’exeresi della mucosa ridondante e sucking del contenuto in eccesso della lamina propria superficiale. L’incisione, l’exeresi della mucosa in eccesso e in alcuni casi la vaporizzazione dell’edema “organizzato” può essere eseguita in maniera ottimale anche con laser a CO2. Durante il trattamento dell’edema complesso si possono verificare specifici problemi tecnici ed in particolare la difficoltà nel mobilizzare abbastanza mucosa del microflap inferiore dopo l’exeresi completa della componente superiore; ne consegue la possibilità che il profilo della corda vocale non sia rettilineo per il persistere di un rigonfiamento centrale. Gli Autori presentano una modifica della tecnica originale con rimodellamento ad “M” del micro-flap per il trattamento dell’edema dello spazio di Reinke in condizioni di edema complesso bilobato, eseguibile con strumentario tradizionale o laser a CO2, applicabile anche al trattamento dell’edema semplice centrale. L’“M-shaped microflap” permette di ottenere la pressochè completa copertura del legamento vocale e nel contempo rettilineizzare il margine libero delle corde vocali al fine di ottenere un ottimale outcome funzionale.
Introduction
Vocal cords oedema was first described by Hajek 1 in 1891 and subsequently Reinke 2 reported the injection of fluid into a cadaveric vocal fold mimicking what was then called Reinke’s Space Oedema (RSO). Little is known of its true pathophysiology, but a correlation between heavy smoking and vocal cord abuse and subsequent chronic inflammation has been reported 3. The typical finding is of unilateral or more frequently bilateral and subepithelial oedema of the vocal cords within the lamina propria superficialis (LPS), also known as Reinke’s space. Histopathological examination of RSO tissue demonstrates decreased amounts of fibronectin, collage and elastin in the basement membrane and lamina propria 4. Classification of RSO is standardised by the system described by Yonekawa 5. Lesions were divided into 3 categories depending on severity: Grade I , contact of the anterior third of the vocal cords; Grade II , contact of the anterior two thirds of the vocal cords; and Grade III , contact of the entire vocal cords. Microsurgical removal of the redundant tissue can be performed with cold steel instruments or with Carbon Dioxide (CO2) laser 6.
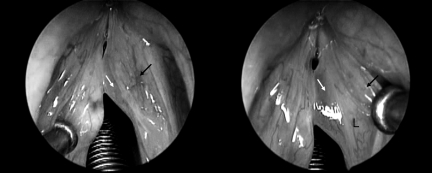
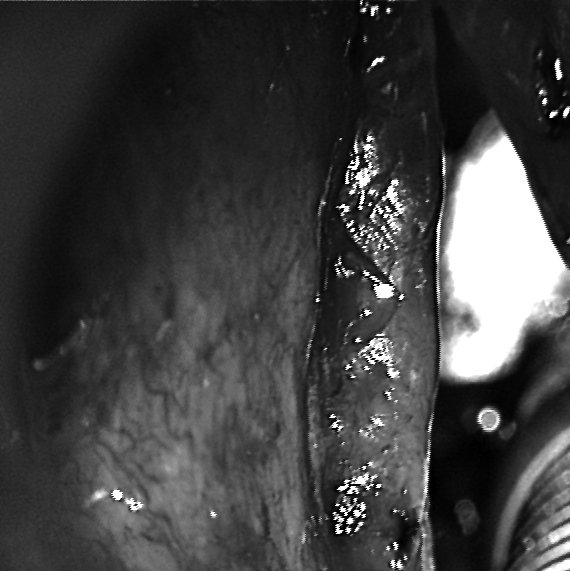
We have noted in a number of cases the phenomenon of bilobular RSO. This occurs when the subepithelial oedema is organised as a double bulge of the vocal cord in the supero-inferior plane (Fig. 1). This is caused by the coexistence of RSO and a sulcus or a vergeture at the level of the free margin, usually involving the middle third or the entire vocal cord. In these cases, it is impossible to manage the inferior RSO if the superior redundant component is not removed. Subsequent suction of the content of the inferior component is usually followed by persistence or early recurrence of the RSO. Excision of both lobes would lead to excess mucosal resection and thereby a large proportion of LPS and the vocal ligament exposed and has the consequence of an impaired mucosal wave as the result of unpredictable scar tissue or when re-epithelialisation is adherent to the vocal ligament.
Fig. 1. Microlaryngoscopic view of Reinke’s Space Oedema (left) showing superior bulge (black arrow) and when reflected laterally (right) the inferior bulge (white arrow) becomes more apparent, as well as the vocal ligament (L).
It is recognised that continuity of the cover at the level of the free margin of the vocal cord 7 as well as maintenance of content in the LPS 8 is of paramount importance in obtaining an optimal voice outcome by allowing restoration of the mucosal wave.
We present a simple yet easily reproducible technique of an “M” shaped microflap for the treatment of bilobular and also centrally lobulated RSO using a CO2 laser and/ or cold micro instruments allowing for the maintenance of a layer of LPS and easy coverage of the potentiallly exposed part of the vocal cord.
Methods
Between March 2006 and January 2009, 11 adult patients underwent microlaryngoscopy and combined cold/CO2 laser treatment for complex RSO at the ENT Department of the Queen Alexandra Hospital, Portsmouth, UK. A modified M shaped microflap technique was constantly carried out in all patients as the technique of choice for the treatment of bilobed RSO.
The patient is prepared for a standard microlaryngoscopy under general anaesthetic. A Mallinckrodt metallic reinforced tube (I.D. 5.0-7.0 mm; Athlone, Ireland) is used if the CO2 laser is employed. Using the European Laryngological Society Classification 9 our procedure is determined as primary vocal fold surgery (VFS) with a direct endolaryngeal approach. The complete exposure of the glottis is achieved by the Kleinsasser laser laryngoscopes modified by Rudert with the Riecker-Kleinsasser suspension system (Storz, Tuttlingen, Germany). A Sharplan 1050 CO2 laser with an Accuspot 712 micro-manipulator (Sharplan®, Tel Aviv, Israel) set on the superpulse mode (2 watts, 270 micron spot size) was used until July 2009, subsequently substituted by an AcuPulse 40ST CO2 laser with Digital AcuBlade (Lumenis® Ltd, Tel Aviv, Israel). The parameters used were: operating mode: superpulsed; power: 10 Watts; beam scan shape: linear incision from 2 to 4 mm; incision width: 0.27 mm; penetration depth: 0.2 mm.
Once the bilobed RSO is identified on microlaryngoscopy (Fig. 2), the superior component is completely excised using CO2 laser, leaving the inferior lobe (Fig. 3) and an adequate amount of the LPS in situ, covering the superior aspect of the ligament. The subepithelial space of the inferior component is mobilised and as routinely performed, the amorphous material from RSO is reduced with suction tubing. If organised the RSO is reduced by gentle vaporisation or partially resected with cupped forceps. It is mandatory to leave a pliable layer of LPS in order to maintain the mucosal wave.
Fig. 2. Microlaryngoscopic view of larynx confirming RSO. LVC: left vocal cord with RSO; RVC: right vocal cord with RSO; MLT: microlaryngoscopy tube; LFC: left false cord.
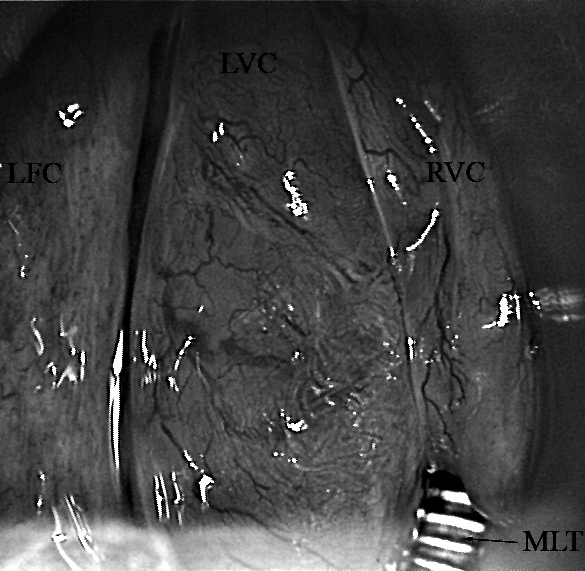
Fig. 3. Microlaryngoscopic view with upper lobe resected. LL: lower lobe of RSO; * exposed superior aspect of the vocal cord.
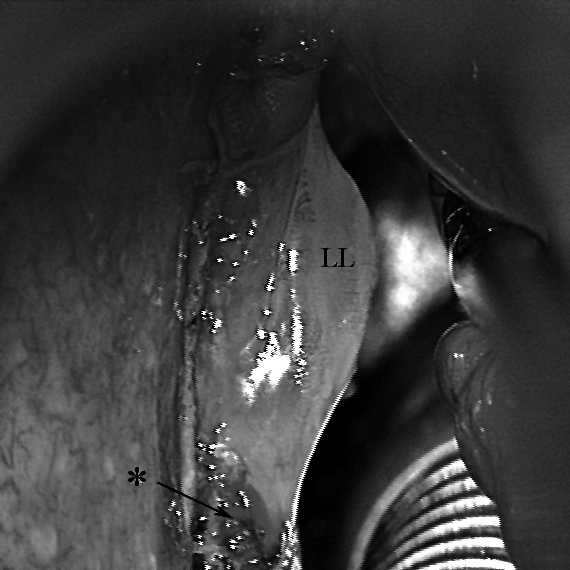
After reduction of the content of the Reinke’s space, in the lower lobe, and mobilisation of the microflap, it is recognized that the mucosa cannot be completely brought up to cover the exposed cord. At this stage, a horizontal incision is made in the superior aspect of the bulging microflap from the free margin of the vocal cord to the external margin of the mucosa. This is performed with cold steel instruments or CO2 laser avoiding excess loss of mucosa. By making this medial horizontal incision to split the lower lobe (Fig. 4), the two halves of the mucosal microflap can be immediately brought laterally to cover the vocal ligament. Any excess mucosa is completely trimmed so that coverage of the ligament is from the free margin to the ventricle. A minimal V shaped segment of the ligament is left exposed in the supero-lateral aspect of the vocal cord (Fig. 5). Further haemostasis can be obtained with neurosurgical patties soaked in 1:80,000 adrenaline. Fibrin glue (Tissucol® Immuno A.G., Vienna, Austria) can be used to stabilise the flap. Specific post-operative instructions are given to start speaking immediately.
Fig. 4. Incision marker in lower lobe of RSO and direction of microflap movement.
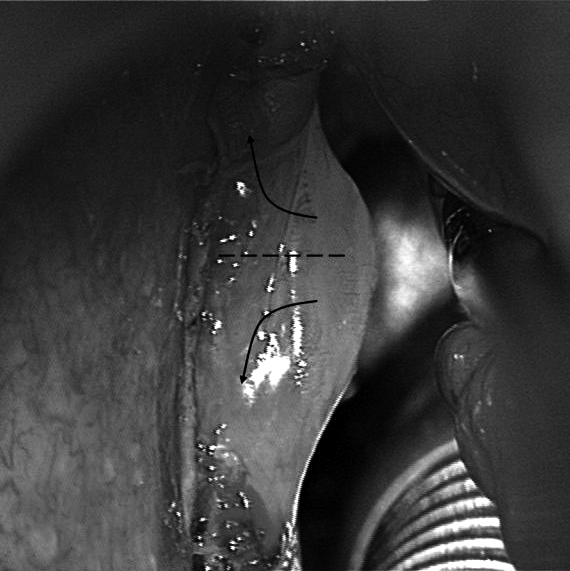
Fig. 5. Final resting position of “M” shaped microflap, noting the small triangular portion of the exposed lamina propria superficialis.
Discussion
The treatment of Reinke’s Oedema has evolved from the “stripping” technique, as described by Lore, in 1934 10 11, to vaporization with CO2 laser and debridement of excess oedematous tissue 12 13. More precise procedures have been described including the microflap technique with elevation of a mucosal microflap and microsuction of the amorphous material within Reinke’s Space.
Early “stripping” and resection techniques fell out of favour due to post-operative exposure of the vocal ligament. Nielsen 11 noted that in 120 cases of Reinke’s Oedema treated with mucosal stripping, only 19% had a normal voice post-operatively with a 58% recurrence rate. Stripping of vocal cord mucosa has the catastrophic consequence of ligament exposure and, in many instances, the lack of an adequate amount of lamina propria superficialis with the absence of the mucosal wave and a resulting asthenic, strain or breathy voice. A significantly prolonged period of vocal rehabilitation was required in patients undergoing vocal cord stripping compared to those who underwent other forms of treatment 14. Use of the CO2 laser for the treatment of vocal cord lesions was first described in 1976 15. The microflap technique was described by Hirano 12, who recommended incision of the epithelium lateral to the polypoid area, reduction of the gelatinous material with trimming of redundant mucosa and redraping the microflap over the cord, thus preserving the mucosal waveform. The microflap technique is actually considered the procedure of choice, in the treatment of the RSO 13 and we prefer the use of the CO2 laser as we feel it allows for more accurate dissection of the flap.
In the presence of complex lesions, like concomitant RSO and sulcus or vergeture, it is possible to find a bilobular lesion that can be difficult to treat without leaving a significant part of the cord and vocal ligament exposed. In bilobular RSO organised in the supero-inferior plane, resection of the upper lobe can leave the vocal ligament exposed and the mucosa of the inferior lobe is too tight to be pulled upwards in order to give sufficient coverage. In some cases of centralised RSO, it is also difficult to bring enough mucosa upwards to cover the ligament adequately or to avoid leaving a central bulging of the mucosa in excess, potentially allowing early recurrence or persistence. One suggested technique is to release the anterior and posterior margins of the inferior lobe. This allows for coverage of the middle part of the ligament but increases the chance of web and scar formation by exposing the ligament close to the anterior commissure. There have been no other reports on the management of complex RSO and how to treat the double bulge of oedema in the superoinferior plane.
Fibrin glue can be used to stabilise the flap, however it is not always necessary and is a human derivate, therefore informed consent should be obtained from the patient prior to the use of human products. Use of fibrin glue can improve final positioning of the flap, however further investigations are necessary.
Although it has been hypothesised that the CO2 laser can cause thermal injury to the vocal ligament 16, we feel that use of meticulous microsurgical techniques combining both CO2 laser and cold steel instruments, where appropriate, as well as updated laser equipment 13 17 and low wattage settings (2-5 W, continuous, superpulse) offers the possibility of safe treatment of RSO, as routinely performed in our unit.
Some phonosurgeons will not operate on RSO unless the patient has given up smoking for at least 2 to 4 months before the procedure. We believe that in addition to airway obstruction, moderate and severe dysphonia, especially in women, represents a good indication for elective surgery, even in patients who have not stopped smoking so as to improve their quality of life.
We follow the policy of allowing the patient to speak immediately. Specific post-operative instructions are given to start speaking immediately. Although this is the empirical procedure followed, there is little real evidence regarding voice rest versus immediate phonation.
We believe that phonation will maintain the flap in the original position, especially in the first 24 hours postoperatively. After this time, the flap will become adherent to the vocal ligament in a definitive position. We do not believe that total voice rest is, in truth, feasible since frequent episodes of coughing or “clearing of the throat” by the patient, in the immediate post-operative period, produces a significant stress on the vocal cords as phonation. Immediate phonation prevents the micro-flap from slipping back and medialising during breathing, due to the negative pressure at the level of the glottis during the inspiratory acts.
Our modified micro-flap technique allows excellent easy coverage of the majority of the ligament with the exception of a small V shaped segment in the mid-cord. The free edge of the vocal cord becomes immediately covered by the microflap and more important the profile of the cord is straight with a complete cord-to-cord approximation during phonation, in the post-operative period, thus causing minimal asymmetry of the mucosal waves. It reduces the possibility of persistence or recurrence of the RSO and decreases the chance of unpredictable scar tissue in the surgical area. We have carried out this procedure in 11 patients with excellent results. It offers very good results in terms of fast recovery and predictable long-term outcome in voice quality, allowing the procedure to be carried with the same anaesthetic if bilateral disease is encountered.
Conclusions
The “M” shaped microflap is a simple, yet reproducible, surgical technique in the management of complex bi-lobular or centrally located RSO, offering predictable voice outcome.
Acknowledgements
Authors thank Mrs Emma Narramore for assistance with the figures.
References
- 1.Hajek M. Anatomische Untersuchungen über das Larynxödem. Langenbecks Arch Chir. 1891;42:46–93. [Google Scholar]
- 2.Reinke F. Untersuchungen über das menschliche Stimmband. Fortschr Med. 1895;12:469–478. [Google Scholar]
- 3.Marcotullio D, Magliulo G, Pezone T. Reinke’s edema and risk factors: clinical and histopathologic aspects. Am J Otolaryngol. 2002;23:81–84. doi: 10.1053/ajot.2002.30961. [DOI] [PubMed] [Google Scholar]
- 4.Zeitels SM, Casiano RR, Gardner GM, et al. Management of common voice problems: Committee report. Otolaryngol Head Neck Surg. 2002;126:333–348. doi: 10.1067/mhn.2002.123546. [DOI] [PubMed] [Google Scholar]
- 5.Yonekawa H. A clinical study of Reinke’s edema. Auris Nasus Larynx. 1988;15:57–78. doi: 10.1016/s0385-8146(88)80010-5. [DOI] [PubMed] [Google Scholar]
- 6.Dursun G, Ozgursoy OB, Kemal O, et al. One-year follow-up results of combined use of CO2 laser and cold instrumentation for Reinke’s edema surgery in professional voice users. Eur Arch Otorhinolaryngol. 2007;264:1027–1032. doi: 10.1007/s00405-007-0309-x. [DOI] [PubMed] [Google Scholar]
- 7.Lim JY, Choi JN, Kim KM, et al. Voice analysis of patients with diverse types of Reinke’s edema and clinical use of electroglottographic measurements. Acta Otolaryngol. 2006;126:62–69. doi: 10.1080/00016480510043927. [DOI] [PubMed] [Google Scholar]
- 8.Zeitels SM, Hillman RE, Desloge R, et al. Phonomicrosurgery in singers and performing artists: treatment outcomes, management theories, and future directions. Ann Otol Rhinol Laryngol. 2002;190(Suppl):21–40. doi: 10.1177/0003489402111s1203. [DOI] [PubMed] [Google Scholar]
- 9.Friedrich G, Remacle M, Birchall M, et al. Defining phonosurgery: a proposal for classification and nomenclature by the Phonosurgery Committee of the European Laryngological Society (ELS) Eur Arch Otorhinolaryngol. 2007;264:1191–1200. doi: 10.1007/s00405-007-0333-x. [DOI] [PubMed] [Google Scholar]
- 10.Lore JM. Stripping of the vocal cords. Laryngoscope. 1934;44:803–816. [Google Scholar]
- 11.Nielsen VM, Højslet PE, Karlsmose M. Surgical treatment of Reinke’s oedema (long-term results) J Laryngol Otol. 1986;100:187–190. doi: 10.1017/s0022215100098959. [DOI] [PubMed] [Google Scholar]
- 12.Hirano M. Endolaryngeal microsurgery. In: English GM, editor. Otolaryngology. Vol 3. Philadelphia, PA: Lippincott; 1988. pp. 1–11. [Google Scholar]
- 13.Remacle M, Lawson G, Watelet JB. Carbon dioxide laser microsurgery of benign vocal fold lesions: indications, techniques, and results in 251 patients. Ann Otol Rhinol Laryngol. 1999;108:156–164. doi: 10.1177/000348949910800210. [DOI] [PubMed] [Google Scholar]
- 14.Lumpkin SM, Bishop SG, Bennett S. Comparison of surgical techniques in the treatment of laryngeal polypoid degeneration. Ann Otol Rhinol Laryngol. 1987;96:254–257. doi: 10.1177/000348948709600303. [DOI] [PubMed] [Google Scholar]
- 15.Lyons GD, Lousteau RJ, Mouney DF. CO2 laser laryngoscopy in a variety of lesions. Laryngoscope. 1976;86:1658–1662. doi: 10.1288/00005537-197611000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Vaughn CW, Blaugrund SM, Gould WJ, et al. Discussion: surgical management of voice disorders. J Voice. 1988;2:176–181. [Google Scholar]
- 17.Remacle M, Friedrich G, Dikkers FG, et al. Phonosurgery of the vocal folds: a classification proposal. Eur Arch Otorhinolaryngol. 2003;260:1–6. doi: 10.1007/s00405-002-0507-5. [DOI] [PubMed] [Google Scholar]