For many years, the alternative to functional procedures in which the glottic or supraglottic level are preserved (cordectomy of varying extents, supraglottic horizontal laryngectomy) was total laryngectomy, as replacement sphincteric function was not believed to be possible.
The merit goes to Serafini 1, despite the initial failures of tracheohyoidoepiglottopexy, for having stimulated the research into techniques to replace total laryngectomy 2-4 making it possible to reconstruct the aerodigestive crossroads, whilst maintaining the three functions of the larynx, despite the absence of the “conventional” structures (epiglottis, false cords, vocal cords) assigned to sphincteric function.
All this was facilitated by the simultaneous development of speech therapy strategies, thanks primarily to the French schools, aimed at readapting swallowing first and subsequently speech to the neoglottis characterised by a dynamic opposition between the anterior structures (epiglottis or base of the tongue) and one or two arytenoids to the rear, which must maintain good movement for arytenoid health.
In the absence of the bases for adequate functional recovery (correct surgical technique with preservation of the function of the laryngeal nerves, correctly performed reconstruction, immediate post-operative rehabilitation) or in the presence of various types of complication that cause non-optimal anatomic and functional sequelae, recovery of the swallowing function can be problematic especially in patients whose neurological situation does not require efficacious neuronal plasticity.
In some cases, due to the persistence of swallowing difficulties, with progressive weight loss and the occurrence of repeated episodes of aspiration with bronchopneumonic complications, use of PEG can constitute a provisional measure for allowing an extension of the rehabilitation programme. If the functional situation does not improve to allow adequate, risk-free eating, patients are often offered total laryngectomy.
In order to avoid this kind of conclusion to the treatment programme, which undoubtedly represents a failure for functional surgery and is deeply frustrating for a patient who has gone through a difficult and exasperating postoperative phase in the hope of avoiding permanent tracheostomy, since the late 1980s, some Authors 5-7 have suggested surgical methods that aim to improve neoglottic competence and consequently, the functions (swallowing and voice) related to the sphincteric ability of the larynx. This functional rehabilitational surgery is gradually being adopted, after the early experiences based exclusively on injective laryngoplasty techniques in the light of more detailed evaluations of the various causes of deglutition failure.
Moreover, only with injective methods is it possible to find solutions to minimal pre- and post-deglutition disorders that, due to the presence of an efficacious expulsive cough, do not constitute a risk for the lower airways, rather a cause of inconvenience for the patient in social situations, which thus compromises quality of life.
In parallel with the attempts to solve the problems of neoglottic insufficiency, a voice surgery technique has been developed with the aim of improving glottic competence following cordectomy to improve voice quality and eliminate the phonoasthenia that often represents the greatest handicap for these patients 8-11.
Cordectomy
In cordectomies, the functional sequelae are exclusively voice-related. Difficulties swallowing liquids for the few days immediately after the procedure are temporary and resolve spontaneously in a few days. Dysphonia can be the direct consequence of glottic insufficiency, the effect of an anterior adherence (often inevitable when resection also affects the anterior commissure) or caused by supraglottic compensations (from false cords or arytenoepiglottic) favoured by certain situations, such as: oedematous arytenoids, pre-existent hypertrophy of the false cords, extensive glottic resections, retroverted epiglottis, spontaneous, unfavourable compensation due to the absence of postoperative speech therapy.
Speech therapy can resolve speech problems after limited resection (type I and II cordectomies) or after type III cordectomies with the formation of significant neocord scarring. It is also the first line of treatment since any late voice surgery, indicated in the event of unsatisfactory results after rehabilitation, is not recommended for at least 6 months.
Some Authors have suggested immediate surgical rehabilitation, during the same surgical session as the cordectomy, using autologous fat 12. On the basis of these experiences, we introduced into our clinical practice primary surgical rehabilitation using hyaluronic acid 13 with both augmentation aims and in order to improve the scarring processes with a stiffer neocord and that therefore can be applicable also to mucosectomy (type I cordectomy). This makes it possible to obtain a volume increase without additional morbidity around the harvesting site as occurs for fat and with a consequent reduction in the time needed to perform the procedure. We use a Medtronic Xomed Laryngeal Injector with a 27-gauge needle (Orotracheal injection set). Since hyaluronic acid is usually highly viscous and consequently offers a certain resistance when injected using a small gauge needle, we developed a metal plunger that makes it possible to exert adequate pressure that can be varied during the injection (Fig. 1).
Fig. 1. Syringe with a particular metal plunger that makes it possible to exert adequate pressure that can be varied during the injection.
Deferred rehabilitation surgical procedures secondary to cordectomy can be performed using injective laryngoplasty, using biological materials (autologous fat, bovine collagen, homologous collagen, hyaluronic acid) or synthetic materials (polydimethylsiloxane – PDM S) and with structural surgery 14-18. Whereas fat, collagen and hyaluronic acid can change in volume over time, due to partial reabsorption, PDMS is stable and non-reabsorbable. The main problem related to injective laryngoplasty is the impredictability of the size of volume increase in the neocord and the homogeneity of the distribution of the material, as these two factors depend on the distendibility of the scar tissue.
In the case of a neocord that is small and/or very close to the thyroid cartilage, and that cannot therefore be enlarged by injection, type I thyroplasty must be performed, using the Goretex technique that allows a gradual detachment of the perichondrium and simultaneous medialisation of the neocord. Goretex thyroplasty is preferable to techniques using implants because it is modulable and presents less risk of extrusion. In the case of procedures involving the commissural region or the juxta commissural one, the neocord can be inexistent with the newly formed perichondrium particularly close to the cartilage. This results in marked anterior glottic insufficiency that cannot be solved either with endoscopic enlargement or by external medialisation. In such situations, Zeitels et al. suggested a laryngoplasty of the anterior commissure that can be integrated with an injective method on the rear two-thirds of the neocord 14 16.
In the event of supraglottic false cord compensation, if this is adequate and the voice intense enough, particularly in male patients, voice surgery could take the form of helping the ventricular bands to meet (injective laryngoplasty). If glottic compensation is believed to be more favourable and feasible, it is achieved by laser resection of the false cords and surgical rehabilitation of the glottic level. When arytenoepiglottic compensation occurs, replacement, if deemed to be advantageous, will involve partial laser resection of the arytenoid hood or of the aryepiglottic fold and voice surgery treatment of the glottic level. In some cases, dysphonia occurs secondary to the formation of scar tissue in the anterior commissure. The surgical solution can either be a resection of the anterior scarring with application of mitomycin (Fig. 2) in an attempt to avoid relapses or reconstruction of the commissure using a flap of adequately deepithelised scar tissue and thinned and fixed with interrupted stitches on to the upper face of one of the two vocal cords, following removal by laser vaporisation of the mucosal coating (Fig. 3).
Fig. 2. Resection of the anterior scarring with application of mitomycin.

Fig. 3. Reconstruction of the commissure using a flap of adequately deepithelised scar tissue and thinned and fixed with interrupted stitches on to the upper face of one of the two vocal cords, following removal by laser vaporisation of the mucosal coating.

Supraglottic laryngectomies
Functional problems are almost exclusively related to cases of supraglottic laryngectomy extended to the arytenoid and the vocal cords, however “classic” procedures can present sequelae if the motility of one or both arytenoids is compromised, if mucosal flaps compromise respiratory tract patency, due to a reduced sensitivity that does not allow an efficacious adductory reflex of the vocal cords. The coexistence of these factors will worsen the dysphagia. In the case of breathing difficulties, the microlaryngoscopic approach using a laser technique will make it possible, either through the resection of the mucosal flap or performance of a rear cordotomy to restore respiratory tract patency and to remove of the tracheostomy tube. If one side of the larynx is immobile or one vocal cord absent, glottic insufficiency will be corrected by injective laryngoplasty using the same technique as for laryngeal monoplegia 19. Botulinum A toxin or cricopharyngeal myotomy may be considered in cases of sensitivity deficits and/or abnormal cricopharyngeal tone.
Subtotal laryngectomies
In the case of subtotal laryngectomies, the most frequent complication from a functional point of view is the persistence of swallowing problems of varying importance, characterised by a risk of bronchopulmonary infection or cause discomfort while eating (need for accentuated facilitating postures during swallowing, sudden coughing, stagnation of foods causing numerous rasps or need to perform liberating manoeuvres of various types) with consequent difficulties eating certain foods and a tendency to avoid social events 20. Dysphagia is often directly related to poor compensation voice sonority, as both swallowing and voice are conditioned by the sphincteric capacity of the cricoarytenoid unit. However, functional failure is sometimes of the respiratory type, making it impossible to decannulise patients.
The main causes of neoglottic insufficiency are: ankylosis or arytenoid paralysis, backward displacement of the cricoid in relation to the hyoid bone, morpho-functional deficiency of the base of the tongue, however deglutition can also be compromised by other situations, such as: sensitivity deficit of the pharyngeal mucosa and/or neoglottis, preventing the triggering of the pharyngeal phase and the adductory laryngeal reflex; increase in crico-pharyngeal tone or narrowing due to scarring of the mouth of the oesophagus, which by slowing down the pharyngeal phase of swallowing prolong contact between the bolus and the neoglottic aditus, thus increasing the risk of post-deglutition aspiration; presence of atonic piriform fossae or scarring roughness that cause bolus stagnation, leading to a prolonged feeling of presence of a foreign body and constituting a cause of postdeglutition aspiration; separation of the reconstruction, a factor that is particularly important in the absence of the epiglottis since moving the neoglottis away from the hyoid bone vanquishes the protective mechanism of the base of the tongue and compromises the efficiency of arytenolingual compensation, due to the formation of a recess between the hyoid bone and cricoid cartilage at the point in which the arytenoid usually comes into contact with the base of the tongue. It must not be forgotten that, particularly in elderly patients, it is possible that a bone spur (DI SH syndrome), may compress the oesophagus, constituting an obstacle to the progression of the bolus, which thus becomes an important concomitant cause of postoperative dysphagia, an eventuality that should be explored with a preoperative l-l projection x-ray of the cervical spine.
The main causes of respiratory impairment are: persistence of oedema or arytenoid mucosal flap, stenosis of the neoglottis due to membranous or structural causes due to the collapse of the cricoid cartilage (fracture caused by reconstruction traction or chondritis sequelae), forward displacement of the cricoid due to incorrect reconstruction alignment.
Video fibroendoscopy is the fundamental technique for the diagnostic approach to these problems, as it is able to document the anatomic and functional situation, in addition to a sensitivity test and, using boli of varying textures, provides an assessment of deglutition (FEES) that, in the presence of a tracheotomy can also be completed with a hypoglottoscopic examination 21.
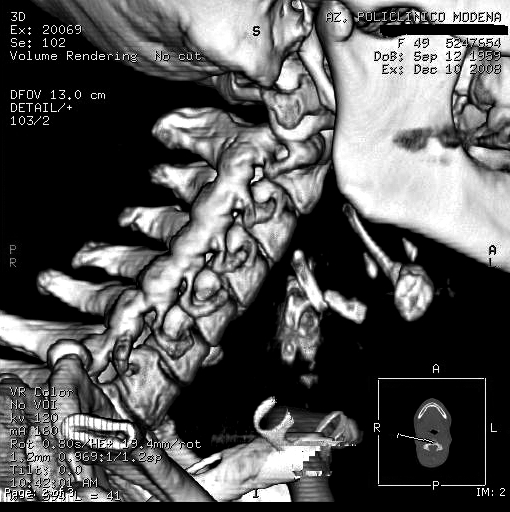
The fibroendoscopic examination of swallowing is irreplaceable also for preoperative planning of a surgical correction by injective laryngoplasty in direct microlaryngoscopy, as during the procedure it is not possible to predict the injection points that will make it possible to correct the disorder. During fibroscopy, an expert eye is able to guess the presence of a reconstruction separation (Fig. 4) requiring confirmation using a X-ray study: a laterolateral projection X-ray of the cervical spine (Fig. 5) and CT of the larynx with 3D reconstructions (Fig. 6), which is also useful for identifying any cervical bone spurs.
Fig. 4. Fibroendoscopy showing a reconstruction separation.
Fig. 5. Laterolateral projection X-ray of the cervical spine.

Fig. 6. CT of the larynx with 3D reconstructions.
Video fluoroscopy can be used as a complement to FEES to document the extent of inhalation with the various barium textures, to identify crico-pharyngeal hypertone or scarring stenosis.
Rehabilitation surgery is performed via the cervicotomy route (reconstruction review and cervical spinal surgery for Forestier’s syndrome), direct suspended microlaryngoscopic procedures (laser resection of the arytenoid mucosal flap or membranous stenosis, laser myotomy of the crico-pharyngeal muscle and injective laryngoplasty), fibroendoscopic arytenoid augmentation.
Reconstruction review can correct situations of separation and anterior or posterior cricohyoid misalignment and membranous and cartilaginous stenosis, cervical spine surgery with prevascular access makes it possible to eliminate compression on the oesophagus by filing the bone spurs. In direct microlaryngoscopy, as well as recanalisation of the respiratory tract, augmentation techniques can be used to reduce or eliminate neoglottic insufficiency and to exclude or minimise any scarring furrows responsible for food stagnation.
The materials that can be used, depending on the infiltration site, are shown in Figure 7. Our experience is based on the use of Vox-Implants (Uroplasty, Inc.), whose injection site stability and absence of reabsorption allow a stable result. This product is constituted by a suspension of PDMS grains with a diameter of between 100 and 200 mm in a polyvinylpyrrolidone (PVP) that acts as a thinner and carrier. The PVP is subsequently reabsorbed by the lymphoreticular system, whilst the particle of PDMS, thanks to their size and superficial texture, which leads to the formation of a connective lattice, do not migrate. The injection system is constituted by a gun whose plunger progresses in steps, each time the lever is pressed. It adapts perfectly to the syringe containing the material and the Luer Lock type connection constitutes a solid graft with the needle in the pack. It is malleable enough to be shaped so as to allow the surgeon optimum surgical field visibility and correct needle tip direction, which is essential for positioning the implant correctly.
Fig. 7. Materials that can be used depending on the infiltration site.
The injection sites are indicated in Figure 8. In general, 2 or 3 cc of PDMS only are used.
Fig. 8. Injection sites.

One of the sites that most often requires intervention is the front part of the neoglottis in correspondence to the cricoid ring and/or adjacent base of the tongue. Also in the case of a cricohyoidoepiglottopexy, an injection at the base of the tongue can be useful for positioning the suprahyoid epiglottis further back. The aim of the injection here is to reduce the anteroposterior gap caused by incomplete contact between the arytenoid(s) and the base of the tongue or the laryngeal face of the epiglottis. Another important injection site is the lateral side of the neoglottis to overcome the lateral gap that is sometimes present either on the side of the removed arytenoid or because the preserved arytenoid tilts without performing any forward sliding movement. The lateral part of the neoglottis can constitute an inhalation site when the piriform fossa is absent, atonic or scarred. This situation, and even scarring furrows that may form in other sites adjacent to the neoglottic aditus constitute the ideal condition for post-deglutition inhalations.
It is important not to overcorrect as the material cannot be reabsorbed and the increase in volume obtained is stable. The quantity to be injected must be carefully evaluated to avoid an excessive reduction in lumen taking into consideration also a possible mild post-operative oedema that can be avoided by administering cortisone therapy on the day of the procedure. The presence of the anaesthetic tube preserves the calibre, which avoids the risk of an excessive reduction in respiratory tract patency. During infiltration, it is appropriate to make sure that adequate filling occurs. An absence of filling suggests that the material has been introduced too deep or that the material is sliding towards sites of lesser tissue resistance with a consequent inefficacy of the procedure. Lastly, it should be remembered that excessively superficial infiltration, particularly under pressure, can cause later extrusion, thus vanquishing the results obtained. It can be necessary to intervene in steps, particularly when scar tissues do not allow the first injection to infiltrate an adequate quantity of material and obtain the volume increase needed to correct the functional disorder. Some Authors 22 use the fibroendoscopic approach using instruments that bend with the operational channel, allowing the introduction of a 25-gauge needle. This technique makes it possible to intervene almost exclusively on the arytenoid hood and the material currently used is collagen, which requires a thin needle for injection. Although as a material, fat is suitable for this area, it requires a larger infiltration needle, to dispense the pressurised substance easily. In patients with hypertonic oesophageal mouths or with a pharyngeal phase slowdown, botulinic toxin can be injected into the cricopharyngeal muscle or a myotomy performed. Both procedures can be performed either endoscopically or via the external route 23-26.
References
- 1.Serafini I. Laringectomia totale con mantenimento della respirazione per vie naturali. Minerva O.R.L. 1970;20:73–84. [PubMed] [Google Scholar]
- 2.Mayer EH, Reider W. Technique de laringectomie permettant de conserver la permeabilité respiratoire (la crico-hyoido- pexie) Ann Otolaryngol. 1959;76:677–681. [Google Scholar]
- 3.Piquet JJ, Desaulty A, Delacroix G. La crico-hyoido-pexie. Technique operatoire et resultat fonctionels. Ann Otolaryngol Chir Cervicofac. 1974;91:681–686. [PubMed] [Google Scholar]
- 4.Labayle J, Bismuth R. La laryngectomie totale avec reconstruction. Ann Otolaryngol Chir Cervicofac. 1971;88:219–228. [PubMed] [Google Scholar]
- 5.Bessede SP, Sauvage JP, Morin R, et al. Correction des troubles de deglutition aprés chirurgie partielle du pharyngolarynx par injection de collagene. Etude de 9 cas. Ann Otolaryng. 1988;105:343–348. [PubMed] [Google Scholar]
- 6.Remacle M, Hamoir M, Marbaix E. Gax-collagen injection to correct aspiration. Problems after subtotal laryngectomy. Laryngoscope. 1990;100:663–669. doi: 10.1288/00005537-199006000-00023. [DOI] [PubMed] [Google Scholar]
- 7.Galetti G, Botti M, Croatto L, et al. La riabilitazione delle insufficienze glottiche e neoglottiche. Acta Otorhinol. 1990;10:217–261. [PubMed] [Google Scholar]
- 8.Galetti G, Bergamini G, Ghidini A, et al. Surgical rehabilitation of glottal insufficiency after a cordectomy. Medicine Biologic Environnement. 1990;18:489–496. [Google Scholar]
- 9.Galetti G, Bergamini G, Ghidini A, et al. Insufficienza glottica e neoglottica: inquadramento clinico, diagnosi e terapia chirurgica con gax collagene. Chirurgia funzionale della laringe: stato attuale dell’arte. In: Vincentiis M, editor. Rel. Uff. LXXX Cong. Naz. S.I.O. e Ch. C.-F. Pisa: Pacini Editore; 1993. pp. 123–142. [Google Scholar]
- 10.Rotemberg M. L’utilisation du collagèn en rehabilitation glottique et vocale. Cah ORL. 1990;26:46–47. [Google Scholar]
- 11.Remacle M, Marbaix E, Hamoir M, et al. Correction of glottic insufficiency by collagen injection. Ann. Otol Rhinol Laryngol. 1990;99:438–444. doi: 10.1177/000348949009900605. [DOI] [PubMed] [Google Scholar]
- 12.Bolzoni Villaret A, Piazza C, Redaelli De Zinis LO, et al. Phonosurgery after endoscopic cordectomies. I. Primary intracordal autologous fat injection after transmuscular resection: preliminary results. Eur Arch Otorhinolaryngol. 2007;264:1179–1184. doi: 10.1007/s00405-007-0331-z. [DOI] [PubMed] [Google Scholar]
- 13.Molteni G, Bergamini G, Ricci Maccarini A, et al. Autocrosslinked hyaluronan gel injections in Phonosurgery. Otolaryngol Head Neck Surg. 2010;142:547–553. doi: 10.1016/j.otohns.2009.12.035. [DOI] [PubMed] [Google Scholar]
- 14.Zeitels MS, Jarboe J, Franco RA. Phonosurgical reconstruction of early glottic cancer. Laryngoscope. 2001;11:1862–1885. doi: 10.1097/00005537-200110000-00036. [DOI] [PubMed] [Google Scholar]
- 15.Sittel C, Friedrich G, Zorowka P, et al. Surgical voice rehabilitation after laser surgery for glottic carcinoma. Ann Otol Rhinol Laryngol. 2002;111:433–439. doi: 10.1177/000348940211100604. [DOI] [PubMed] [Google Scholar]
- 16.Zeitels MS. Optimizing voice after endoscopic partial laryngectomy. Otolaryngol Clin North Am. 2004;37:627–636. doi: 10.1016/j.otc.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 17.Remacle M, Lawson G, Morsomme D, et al. Reconstruction of glottic defects after endoscopic cordectomy. Voice outcome. Otolaryngol Clin North Am. 2006;39:191–204. doi: 10.1016/j.otc.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 18.Piazza C, Villaret AB, Radaelli De Zinis LO, et al. Phonosurgery after endoscopic cordectomies. II. Delayed medialization techniques for major glottic incompetence after total and extended resections. Eur Arch Otorhinolaryngol. 2007;264:1185–1190. doi: 10.1007/s00405-007-0330-0. [DOI] [PubMed] [Google Scholar]
- 19.Bergamini G, Alicandri-Ciufelli M, Molteni G, et al. Therapy of unilateral vocal fold paralysis with polydimethylsiloxane injection laryngoplasty: our experience. J Voice. 2010;24:119–122. doi: 10.1016/j.jvoice.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 20.Bergamini G, Alicandri-Ciufelli M, Molteni G, et al. Rehabilitation of swallowing with polydimethylsiloxane injections in patients who underwent partial laryngectomy. Head Neck. 2009;31:1022–1030. doi: 10.1002/hed.21064. [DOI] [PubMed] [Google Scholar]
- 21.Ricci Maccarini A, Stacchini M, Salsi D, et al. Trans-tracheostomic endoscopy of the larynx in the evaluation of dysphagi. Acta Otorhinolaryngol Ital. 2007;27:290–293. [PMC free article] [PubMed] [Google Scholar]
- 22.Ricci Maccarini A, Stacchini M, Salsi D, et al. Surgical rehabilitation of dysphagia after partila laryngectomy. Acta Otorhinolaryngol Ital. 2007;27:294–298. [PMC free article] [PubMed] [Google Scholar]
- 23.Schneider I, Thumfart WF, Pototschnig C, et al. Treatment of dysfunction of the cricopharyngeal muscle with botulinum A toxin: introduction of a new, non-invasive method. Ann Otol Rhinol Laryngol. 1994;103:31–35. doi: 10.1177/000348949410300105. [DOI] [PubMed] [Google Scholar]
- 24.Moerman MBJ. Cricopharyngeal Botox injection: indications and techniques. Curr Opin Otolaryngol Head Neck. 2006;14:431–436. doi: 10.1097/MOO.0b013e328010b85b. [DOI] [PubMed] [Google Scholar]
- 25.Kaplan S. Paralysis of deglutition, a post-poliomyelitis complication treated by section of the cricopharyngeus muscle. Ann Surg. 1951;133:572–573. doi: 10.1097/00000658-195104000-00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lawson G, Remacle M. Endoscopic cricopharyngeal myotomy: indications and technique. Curr Op Otolaryngol Head Neck Surg. 2006;14:437–441. doi: 10.1097/MOO.0b013e3280106314. [DOI] [PubMed] [Google Scholar]





