VCL-AB01, a cationic lipid-formulated plasmid DNA (pDNA)-based vaccine that contains genes encoding genetically detoxified B. anthracis protective antigen (PA) and lethal factor (LF), was assessed in a Phase 1, dose-escalating clinical trial in healthy adults for safety and immunogenicity, and in nonhuman primates for immunogenicity and efficacy against challenge with a lethal dose of B. anthracis spores. Healthy 18—45 year old subjects were randomly assigned to receive either the investigational vaccine containing 0.2 mg, 0.6 mg, or 2 mg of total pDNA per dose, or saline placebo, administered at 0, 1 and 2 months. The 0.2 mg and 0.6 mg dose levels were generally well tolerated; however, dose-limiting reactogenicity was observed among subjects given the first 2 mg dose and the remaining 2 injections in the 2 mg group were reduced to 0.6 mg. Dose-related increases in seroconversion frequencies were observed. Overall, 10%, 33.3% and 80% of subjects in the 0.2, 0.6 and 2 mg groups, respectively, developed antibodies to PA and/or LF as measured by ELISA; however, antibodies with toxin neutralizing activity (TNA) were detected in only 1 subject. In monkeys that received a 0.6 mg dose 3 times at 2 week intervals, low levels of antibodies were detected by ELISA but not by the TNA assay in all animals just prior to challenge. Despite the absence of TNA, 3/4 animals survived the lethal challenge. In summary, VCL-AB01 was generally well tolerated in humans at a dose that provided immunity in monkeys despite the lack of robust TNA titers in either species.
Introduction
Historically, Bacillus anthracis, the causative agent of anthrax, has been associated with herd animals and has not been commonly viewed as a significant human pathogen.1 However, with the realization that anthrax spores have been weaponized, anthrax has the potential to become a major human disease threat.2 Cases resulting from mailing of spores on the East Coast of the United States, as well as the outbreak in Sverdlovsk in the former Soviet Union, have demonstrated that B. anthracis spores can be produced inexpensively, are extremely stable when stored properly, and can be effectively distributed in populated areas.3 Mortality after infection with aerosolized anthrax spores (inhalational anthrax) has ranged from 40% to 90%.2,4 Consequently, B. anthracis spores are a likely organism for use as a bioterrorist weapon, and as such there is a real and present threat of an intentional and major outbreak of anthrax in humans.
Research on anthrax during the past several decades has provided information about the molecular basis of disease in humans, including the scientific basis for developing subunit vaccines.5 The virulence of B. anthracis is primarily the result of a multi-component toxin secreted by the organism. The protein toxins consist of three separate gene products, designated protective antigen (PA), lethal factor (LF) and edema factor (EF). LF and EF each bind to PA, resulting in the formation of lethal toxin (LT) and edema toxin (ET), respectively. The genes encoding these toxin components, along with the genes responsible for expression of the capsule, are required for full B. anthracis virulence. PA binds to the cell surface, where it undergoes cleavage resulting in the formation of a heptameric structure capable of delivering the toxins into the cell. LT is a zinc metalloprotease that cleaves several isoforms of mitogen-activated protein kinase and thereby disrupts signal transduction events within the cell eventually leading to cell death. ET is a calmodulin-dependent adenylate cyclase that causes deregulation of cellular metabolic events, leading to clinical manifestations that include edema. Protective antigen is an essential component of anthrax vaccines although other components may also contribute to immunity.5
The only anthrax vaccine licensed for use in the United States is Biothrax™ (also known as Anthrax Vaccine Adsorbed, or AVA), which is derived from vaccine candidates developed at Fort Detrick, Maryland in the 1950s. The licensed immunization regimen consists of 5 doses administered by the intramuscular route at 0 and 4 weeks and 6, 12 and 18 months, with annual boosters thereafter. The heightened public concern of deliberate, widespread anthrax exposure in the United States has resulted in a government call for an improved vaccine. Alternative vaccines that may offer improvements over Biothrax™ are under development, some of which are currently undergoing clinical testing, including recombinant PA (rPA)6,7 and plasmid DNA (pDNA)-based vaccine VCL-AB01 (Vical Incorporated, San Diego, CA) encoding genetically detoxified forms of PA and LF formulated with a cationic lipid-based DMRIE:DOPE adjuvant.8 Vaccination with anthrax PA protein-based vaccines or passive administration of anti-PA antibodies have conferred protection against lethal aerosol challenge with B. anthracis in mouse, rabbit, guinea pig and nonhuman primate models,9–14 providing evidence supporting a PA component for an anthrax vaccine. The plasmids used in VCL-AB01 have previously been shown to protect rabbits from aerosolized B. anthracis challenge.11
The objectives of these studies were three-fold: (1) to assess the safety of VCL-AB01 in a rabbit repeated dose toxicity study; (2) to assess the safety and immunogenicity of VCL-AB01 in a Phase 1, two-center, randomized, double-blind, placebo-controlled, dose-escalating clinical trial; and (3) to assess the immunogenicity and efficacy of VCL-AB01 in monkeys.
Results
Safety of VCL-AB01 in rabbits
A repeated dose toxicity study was conducted in rabbits to assess the safety of repeated IM injections of VCL-AB01 on Days 0, 14, 28 and 56. No deaths occurred and no safety issues were associated with either the 2 mg or the 0.2 mg dose as determined by daily Draize scoring of the injection sites, daily clinical observations, body weights, food consumption, clinical chemistry, coagulation or ophthalmoscopic examination 48 hours and 4 weeks after the last injections. In addition, there was no evidence of production of anti-nuclear antibodies or antibodies to double stranded DNA (ds DNA).
Some inflammation at the injection site was observed microscopically. The severity of inflammation was not dose-dependent, but was associated with administration of both the low and high doses of VCL-AB01 as well as the high dose pDNA in phosphate-buffered saline (PBS). In all groups, the inflammation was reduced markedly over the recovery period and was not associated with injection site edema or erythema.
Some increases in spleen and kidney weights of animals (predominantly males) treated with VCL-AB01 and pDNA or PBS were noted but were not associated with any histological changes. These changes in spleens and in kidneys resolved over the 28-day recovery period.
Safety of VCL-AB01 in humans
Forty subjects were enrolled and received at least one dose of vaccine. The vaccine doses tested in each group and the demographics of the vaccinated subjects are shown in Table 1. Most of the subjects in Group A (0.2 mg dose) and Group C (2.0 mg dose) were males, while most of the subjects in Group B (0.6 mg dose) were females. The numbers of males and females were similar in Group D (placebo). The racial composition of Group A was spread across all of the racial groups while most of the subjects in the other three groups were white.
Table 1.
Demographic characteristics of vaccinated subjects
| Group | Dose (mg) |
Schedule (months) |
Number enrolled |
Male/ Female |
Mean age in years (range) |
Race (W/B/A/M)* |
|---|---|---|---|---|---|---|
| A | 0.2 | 0, 1, 2 | 10 | 7/3 | 28 (21,41) | 4/3/2/1 |
| B | 0.6 | 0, 1, 2 | 10 | 3/7 | 30 (21, 44) | 8/1/1/0 |
| C | 2/0.6/0.6 | 0, 1, 2 | 11 | 8/3 | 32 (20, 45) | 10/0/1/0 |
| D | 0 | 0, 1, 2 | 9 | 5/4 | 32 (23, 41) | 9/0/0/0 |
| (Placebo) |
W, white; B, black; A, Asian; M, multiracial.
Three subjects discontinued the study early due to reasons unrelated to vaccination: two subjects in the 0.6 mg group (one withdrew; one was discontinued for noncompliance), and one subject in the 2 mg dose group (lost to follow-up). No deaths were reported during the study. Toxicity gradings of 3 and 4 were predetermined as serious adverse events (SAEs). Eight subjects experienced an SAE during the trial, three of which were considered vaccine-related grade 3 events: injection site pain, injection site reaction and headache. All vaccine-related grade 3 adverse events (AEs) occurred in subjects that received the 2 mg dose of vaccine. The occurrence of two grade 3 reactions (injection site pain) and systemic symptoms within 24 hours after the first injection among the 10 subjects given the first 2 mg dose of vaccine resulted in review of the safety data and a decision to dose de-escalate the 2 mg dose to 0.6 mg for subsequent doses for all subjects randomized to the 2 mg dose level. One subject given the first 0.6 mg dose in the 0.6 mg group developed grade 3 systolic hypertension 30 minutes after immunization, but the blood pressure was normal at the subsequent visit, and no further vaccinations were given. The remaining SAEs (social hospitalization, defined as having no place to go but in need of care; peritonsillar abscess; asymptomatic bradycardia; and a febrile syndrome) were not considered vaccine-related. There were no clinically important safety findings related to vaccination for any vaccine group with regard to clinical laboratory assessments, vital signs or physical examination findings.
The frequencies of injection site and systemic symptoms and signs recorded during the week following the first immunization are shown in Table 2. Most subjects given vaccine at any dose level experienced injection site discomfort, and dose-related increases in the frequencies of subjects who reported moderate to severe discomfort were observed (Table 2). Only one subject given placebo reported mild injection site discomfort after dose 2. Similar trends were observed after the second and third dose; although the overall frequencies were generally lower (Table 2). Two subjects discontinued the study early due to an AE in each of the groups given VCL-AB01; one subject in the placebo group also was discontinued from the study due to an AE. Most of the subjects who discontinued early from the study due to an AE had a vaccine-related AE that prompted the discontinuation.
Table 2.
Injection site and systemic symptoms during the week following immunization
| Dose (mg) | Dose # | N= | Fever | Injection site discomfort |
Fatigue | Chills/Feverish sensations |
Loss of appetite |
||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Any | Mod-Severe | Any | Mod-Severe | Any | Mod-Severe | Any | Mod-Severea | ||||
| 0.2 | 1 | 10 | 10 | 2 | 3 | 1 | 1 | 0 | 1 | 0 | |
| 2 | 10 | 1 | 8 | 1 | 2 | 0 | 1 | 0 | 0 | - | |
| 3 | 8 | 6 | 0 | 0 | - | 0 | - | 0 | - | ||
| 0.6 | 1 | 10 | 1 | 9 | 5 | 8 | 3 | 5 | 2 | 3 | 1 |
| 2 | 8 | 1 | 6 | 3 | 4 | 1 | 3 | 0 | 3 | 0 | |
| 3 | 7 | 7 | 0 | 1 | 0 | 1 | 0 | 0 | - | ||
| 2/0.6/0.6 | 1 | 11 | 2b | 11 | 10c | 9 | 4 | 7 | 5 | 3 | 2 |
| 2 | 9 | 8 | 2 | 1 | 0 | 1 | 1 | 1 | 0 | ||
| 3 | 9 | 8 | 4 | 3 | 0 | 3 | 1 | 2 | 0 | ||
| Placebo | 1 | 9 | 1 | 0 | - | 5 | 3d | 2 | 1 | 1 | 1 |
| 2 | 8 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | - | ||
| 3 | 8 | 1 | 0 | - | 1 | 0 | 1 | 0 | 0 | - | |
Numbers represent case counts against the number (N) in each group.
Moderate =Grade 2, sufficient to interfere with usual activities; severe = Grade 3 or 4, incapacitating or unable to perform usual activities. See text for details.
One additional subject had mild fever recorded on examination in clinic.
Injection site discomfort in 2 of the 10 subjects was graded as severe.
Fatigue in 1 of 3 subjects was graded as severe.
In general, the frequencies and severities of systemic symptoms increased with increasing dose levels after the first dose of vaccine. The majority of subjects given the 2 mg dose level experienced fatigue and feverish sensations or chills, and many of these symptoms were characterized as moderate to severe. Systemic symptoms were somewhat less frequent and less severe after the second and third doses of 0.6 mg. Following the first injection, three subjects given the 2 mg dose reported fever, compared with zero and one in each of the other vaccine-recipient groups.
The frequencies of other injection site and/or systemic AE considered to be related to immunization increased in a dose-related fashion after the first dose of vaccine: 2, 1, 4 and 11 AEs were reported among 2, 1, 4 and 7 subjects in the placebo, 0.2 mg, 0.6 mg and 2 mg groups, respectively. Headache, the most common AE after the first dose, was reported by 0, 0, 1 and 5 subjects in the placebo, 0.2 mg, 0.6 mg and 2 mg groups, respectively. Myalgia and injection site swelling were reported in two subjects each after a 2 mg dose. From zero to two subjects in each group reported associated AEs after the second or third dose of vaccine.
Serologic responses following immunization of humans with VCL-AB01
Serologic responses were assessed before and after each immunization for anti-PA and anti-LF antibodies and for toxin neutralizing antibodies. The antibody concentrations of anti-PA IgG and anti-LF IgG were measured from serum samples collected at Day 0 and Weeks 6, 10, 28, 39 and 52. Table 3 shows the seroconversion frequencies, defined as the number of responders/total vaccinees at one or more time points after receiving at least one dose of VCL-AB01 or placebo. Overall comparisons among the three VCL-AB01 groups were significant for the number of subjects achieving anti-LF or anti-PA responses (p < 0.01); among pairwise comparisons, the 0.2 mg and 2/0.6/0.6 mg groups were significantly different (p = 0.0055) and the 0.6 mg and 2/0.6/0.6 mg groups trended toward significance (p = 0.0689).
Table 3.
Serum antibody responses after immunization
| Dose in mg (group) |
Number evaluable |
Number (%) with indicated antibody response |
|||
|---|---|---|---|---|---|
| Anti-LF | Anti-PA | Anti-LF or Anti-PA |
TNA | ||
| 0.2 (A) | 10 | 1 (10) | 1 (10) | 1 (10) | 0 |
| 0.6 (B) | 9 | 3(33) | 1 (11) | 3 (33) | 1 (11) |
| 2/0.6/0.6 (C) | 10 | 5 (50) | 4 (40) | 8 (80) | 0 |
| Placebo (D) | 9 | 1 (11) | 0 | 1 (11) | 0 |
| *p-value | 0.17 | 0.12 | <0.01 | 0.47 | |
Statistical comparisons of antibody responses after receipt of 2 or 3 does of VCL-AB01.
Overall comparison among three groups receiving VCL-AB01. Fisher's exact test, pairwise p values for anti-LF or anti-PA; A vs. B, p = 0.3034; A vs. C, p = 0.0055; B vs. C, p = 0.0698.
Table 4 shows the number of subjects who seroconverted after 2 or 3 injections. Overall, 12/28 subjects (43%) who received ≥2 doses seroconverted following vaccination with VCL-AB01. A significant difference in overall seroconversion frequencies between the high and low dose groups (Fisher’s exact test p = 0.0027) and a trend between high and middle dose groups (p = 0.154) were seen. A total of 8/10 subjects in the high dose group seroconverted to PA, LF, or both. No positive responses were observed among the 54 samples tested in each assay from the 9 placebo subjects except for one LF positive sample at week 28 (anti-LF antibody = 3.8 µg/mL).
Table 4.
Number of subjects responding after 2 or 3 injections
| Does level (mg) |
Anti-PA antibody No./Total responding after indicated number of doses |
Anti-LF antibody No./Total responding after indicated number of doses |
||||
|---|---|---|---|---|---|---|
| Dose 2 | Dose 3 | Any | Dose 2 | Dose 3 | Any | |
| 0.2a | 1/10 | 1/8 | 1/10 | 1/10 | 1/8 | 1/10 |
| 0.6b | 0/8 | 1/7 | 1/9 | 1/8 | 3/7 | 3/9 |
| 2/0.6/0.6c | 3/9 | 3/9 | 4/10 | 4/9 | 4/9 | 5/10 |
| placeboc | 0/8 | 0/8 | 0/8 | 1/8 | 0/8 | 0/8 |
Two subjects received only 2 doses.
Two subjects received only 1 dose; one received 2 doses.
One subjects received only 1 dose.
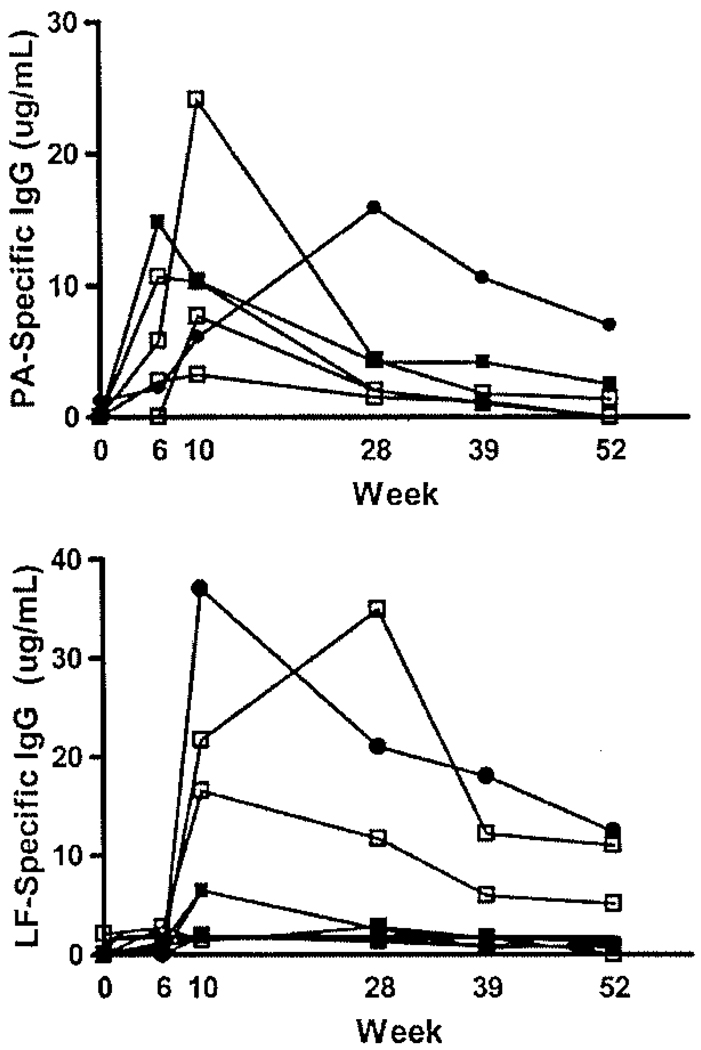
Serum concentrations of anti-PA IgG and anti-LF IgG among responding subjects are shown in Figure 1. This figure illustrates the kinetics, magnitude and longevity of the anti-PA and anti-LF responses. The concentration ranges of anti-PA IgG and anti-LF IgG were 3.2–24.1 µg/ml and 1.9–37 µg/ml, respectively. The antibody responses for the majority of subjects peaked at Week 10, with a minority peaking at either Week 6 or Week 28. The duration of positive anti-PA and anti-LF antibody levels ranged from 10 weeks to 52 weeks with a median of 28 weeks. Because of the low frequency of seroconversion in the 0.2 mg and 0.6 mg dose level groups, it was not possible to define a relationship between vaccine dose level and magnitude of antibody concentration. All serum samples were also tested for TNA. TNA was positive in only 1 subject, who also was positive for anti-PA IgG (Fig. 2). At Week 28, the TNA ED50 titer was 32 and the corresponding anti-PA IgG was 15.9 µg/ml.
Figure 1.
Anti-PA IgG responses (upper) and anti-LF IgG responses (lower) following vaccination with VCL-AB01 at Weeks 0, 4 and 8. Each line represents the longitudinal antibody levels from individual responders from all 3 dosing groups (0.2 mg, solid squares; 0.6 mg, solid circles; and 2 mg, open squares) for 6 time points up to 1 year after the first vaccination.
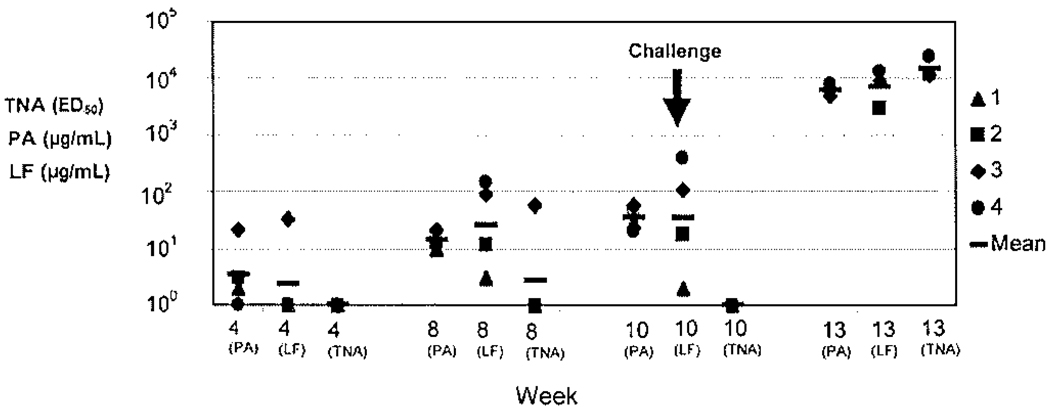
Figure 2.
Anti-PA and anti-LF IgG responses following vaccination of monkeys with VCL-AB01 at Weeks 4, 8 and 10 (prior to challenge), and at Week 13. Individual results for each animal are shown. Animal #1 (designated with the triangle) had low anti-LF concentration at week 10 and did not survive challenge.
Immunogenicity and efficacy in nonhuman primates
VCL-AB01 was well tolerated in monkeys. No deaths and no adverse clinical signs attributable to the vaccine were noted after 3 biweekly doses of the 0.6 mg dose level of VCL-AB01. In VCL-AB01 vaccinated monkeys, anti-PA and anti-LF antibodies increased over time (Fig. 2). By 8 weeks, anti-PA (10–22 µg/mL) and anti-LF (3–149 µg/mL) antibodies were present in all animals. At Week 10, immediately prior to challenge, values ranged from 21–58 µg/mL for anti-PA antibodies and 2–390 µg/mL for anti-LF antibodies. Similar to what was seen in the Phase 1 trial, TNA was not detectable in monkeys at 10 weeks, although one animal did show a positive TNA titer of 58 ED50 at Week 8 that became undetectable by Week 10.
At Week 10, animals received an average of 585 LD50 of Ames strain anthrax spores. Bacteremia was detected at Days 2, 4 and/or 6 in all animals in the PBS group and all but one animal in the VCL-AB01 group. Elevated body temperatures for 1–3 days (≥2°F above baseline) were observed in 3 of the 4 VCL-AB01 group while decreased body temperatures for 1–2 days (≤2°F below baseline) were observed in 2 of the 4 PBS group. No sign of illness including adverse clinical signs, bacteremia and temperature change appeared to correlate with mortality in individual animals (data not shown).
Despite the lack of TNA at Week 10, 3 of 4 (75%) animals survived challenge, with one VCL-AB01 vaccinated animal succumbing to challenge on Day 5, in contrast to 4 of 4 PBS-injected controls that died within 3–8 days. Anti-PA and anti-LF antibodies as well as TNA rose by several orders of magnitude by Week 13 (with, anti-PA antibodies ranging from 4,748–8,231 µg/mL, anti-LF antibodies ranging from 3,045–12,948 µg/mL, and TNA ranging from 11,296–23,676 ED50) indicating that a substantial, antigen-specific boost in antibody production occurred following spore challenge in each of those individuals. In addition to a lack of antibodies with detectable TNA prior to challenge, the animal that died had an anti-PA antibody concentration comparable to those of survivors, but had the lowest concentration (2 µg/mL) of anti-LF antibodies of the 4 vaccinated animals. Control animals (n = 4) demonstrated no antigen-specific antibodies or TNA prior to challenge and all died within 3–8 days after challenge.
Discussion
During the past few years there has been substantial interest in developing pDNA-based vaccines for a number of infectious diseases. Potential advantages of pDNA-based vaccines include the speed, uniformity and cost of manufacture and the ability to elicit both humoral and cellular immune responses. These features, combined with the proven safety of administering nonadjuvanted pDNA doses as high as 8 mg, make this technology very attractive for an anthrax vaccine.
This was the first clinical trial to assess a DMRIE:DOPE formulation as an adjuvant for a prophylactic pDNA-based vaccine. Prior to evaluating VCL-AB01 in the clinic, the vaccine was tested in a repeated-dose toxicology study that included the 2 mg dose intended for use in the clinic, administered 4 times at 3 week intervals (an “n + 1” dosing regimen compared to that used in the Phase 1 clinical trial). Each dose administered in the rabbit study was approximately 28 times the single human dose on a mg/kg basis, assuming a 2.5 kg rabbit and a 70 kg human, thereby providing an adequate safety margin for translational assessment of the vaccine. The results from this study demonstrate the safety of the vaccine in rabbits, with no evidence of an adverse systemic response or injection-site reactogenicity. In monkeys, although no formal toxicity profile was determined, 3 vaccinations with the 0.6 mg dose of VCL-AB01 induced no local or systemic signs of adverse reactions to the vaccine.
The results from the rabbit toxicology study, in addition to studies demonstrating immunogenicity and efficacy, adequate clearance of the pDNA over time (data not shown), and the lack of potential for integration of the pDNA into the host genome,15 were used to support clinical testing of the vaccine. The primary endpoints of the Phase 1 trial were the clinical and laboratory safety and tolerability profiles. The rabbit toxicology data were, in general, predictive for the majority of the same parameters investigated, with no observed changes in biochemistry or hematology parameters noted after injections. The exception appears to be injection site pain, which is difficult to measure in rabbits and requires a severity that results in favoring of the injected limb. In contrast to the results seen in rabbits with the 2 mg dose, dose-related reactogenicity and some systemic responses to VCL-AB01 were observed in humans at that dose, although the changes in clinical signs observed (fever, headache and injection-site pain) are not atypical for vaccines and were transient, resolving within days for all subjects. Injection site pain in humans appeared to be dose-dependent. All subjects who received the first injection of the 2 mg dose reported grade 3 injection site pain and two out of ten subjects reported systemic symptoms. Based on the local and systemic reactions to the 2 mg dose, the high dose group did not receive the full dose vaccine series and instead was boosted with the next lower tolerated dose, 0.6 mg, at 6 weeks after the first injection, with one more dose administered approximately 5–6 weeks after the second dose. Reduction of the dose to 0.6 mg resulted in fewer AEs for that group after both the second and third injections. The 0.2 and 0.6 mg doses of the vaccine were well tolerated in human subjects. In monkeys, the 0.6 mg dose also appeared to be well tolerated.
Previous studies have measured anti-PA antibody levels in volunteers receiving licensed AVA or investigational rPA vaccines, 6,7,16 as well as in individuals infected by anthrax spores through cutaneous or inhalational routes.17 TNA has been shown to correlate with the level of anti-PA antibodies produced in response to protein-based vaccines,17 and has been shown to correlate with antigen-specific antibodies in monkeys that survive lethal B. anthracis challenge. Therefore, for protein-based vaccines, TNA or anti-PA antibodies have been selected as an appropriate correlate of protection expected to be raised against an anthrax vaccine in humans. The anti-PA antibody seroconversion frequency (40%) and the amount of PA-specific antibodies in subjects receiving the highest dose of VCL-AB01 (3.2–24.1 µg/ml) were lower than in subjects receiving AVA in a previous study (100% seroconversion frequency and a range of 15–147 µg/ml). More importantly, TNA was not detected in the majority of subjects who seroconverted, irrespective of dose level or numbers of doses administered, but LF-specific antibodies were detected in 50% of subjects (1.9 µg/ mL–34.9 µg/mL). Unfortunately, it is unknown whether higher PA- and/or LF-specific antibody concentrations, and even TNA, could have been elicited in the Phase 1 trial had the intended 2 mg boosting doses been administered to the 2 mg group instead of the 0.6 mg doses.
Since a correlation has been established between anti-PA IgG and TNA (r2 = 0.83),17 and only a minority of subjects had measurable anti-PA IgG levels, the finding that TNA was not detectable in most subjects is not surprising. However, it is important to note that there was a significant increase in the number of seroconverters to either PA or LF when comparing the high and the low dose groups (Table 3), and more importantly the monkeys that received 3 × 0.6 mg doses of the VCL-AB01 vaccine survived the challenge despite the lack of detectable TNA prior to challenge and low anti-PA and anti-LF antibody concentrations measured using the same assay methods used for evaluation of the human sera. Low to undetectable levels of antibodies determined by ELISA and TNA assays, respectively, did not predict protection in monkeys. Despite the absence of detectible TNA and in the presence of low concentrations of anti-PA and anti-LF antibodies, 75% of VCL-AB01-vaccinated monkeys survived a B. anthracis lethal challenge that killed all PBS injected controls within 3–8 days. These results suggest that for this pDNA-based vaccine, anti-PA IgG levels and/or TNA levels alone did not sufficiently predict protection against inhalational anthrax in primates. Therefore, based on results from these assays, it is not known if humans vaccinated with VCL-AB01 would have likewise been protected with this pDNA-based vaccine against exposure to anthrax spores. Interestingly, the high serological responses in monkeys following spore challenge is suggestive of an anamnestic response that may represent adequate priming of the immune response to sufficiently protect vaccinees despite the lack of obvious serological indicators. Bacteremia was detected in 3 of 4 VCL-AB01-vaccinated animals at 2 and 4 days after challenge that may have provided antigen for boosting the low level immune responses, although one survivor in this group had no detectable bacteremia (data not shown). Further studies are necessary to understand the breadth of immunological responses to this and perhaps other pDNA-based vaccines.
Collectively, these results suggest that VCL-AB01 vaccine is safe and well tolerated at the 0.6 mg dose, both in humans and monkeys. They also suggest that TNA titer, an adequate predictor of protection of protein-based anthrax vaccines, may not be the optimal predictor of protection for this pDNA-based anthrax vaccine. In addition, high concentrations of anti-PA antibodies may not be required for protection following immunization with this pDNA-based vaccine. These results imply that vaccination with this pDNA-based anthrax vaccine may elicit a potent memory response that can be boosted extremely rapidly following exposure to anthrax spores and indicates that an alternative correlate of protection besides serum antibody levels should be explored for this and perhaps other pDNA vaccines. Recent evidence with a pDNA vaccine intended to prevent cytomegalo-virus reactivation in hematopoietic stem cell transplant recipients suggests that a cultured interferon-γ enzyme-linked immunosorbent spot (ELISPOT) assay detected priming of antigen-specific memory T cells in subjects who failed to demonstrate responses by an ex vivo ELISPOT assay. These data suggest that assays such as the ex vivo ELISPOT assay that measure only effector responses may not suffice for detecting immunological priming by pDNA-based vaccines. Further studies of VCL-AB01 in monkeys are warranted to determine if a similar cultured antigen-specific B cell ELISPOT assay will provide evidence of memory that is predictive of protection.
Methods
VCL-AB01 vaccine
The VCL-AB01 vaccine is composed of two covalently closed circular plasmids, VCL-6292 and VCL-62952 combined in equal mass amounts and formulated with a cationic lipid delivery system described below. These plasmids have been described previously.11 VCL-6292 contains a human codon-optimized gene encoding a detoxified B. anthracis PA. To prevent the expressed PA protein from processing into a mature, biologically active protein, the furin cleavage site (RKKR) was deleted from the PA coding sequence. Therefore, the expressed PA antigen, (PAΔfurin) is not active even in the presence of wild type LF.11
VCL-62952 contains a human codon-optimized gene encoding a detoxified B. anthracis LF that is truncated at amino acid 583 to remove the entire domain IV containing the metalloprotease enzymatic activity. The expressed antigen, referred to as LF [I–III], has been shown to be nontoxic even in the presence of wild type PA,11
VCL-AB01 plasmids are formulated with the cationic lipid delivery system, DMRIE/DOPE. DMRIE, synthesized as DMRIE-Br (CAS name: (+)-N-(2-hydroxyethyl)-N, N-dimethyl-2,3-bis(tetradecyloxy)-l-propanaminium bromide) is a cationic lipid with a molecular weight of 636.89 (Fig. 1). DOPE (CAS name; l,2-dioleoyl-sn-glycero-3-phosphoethanolamine) is a zwitterionic phospholipid with a molecular weight of 744.04. These two lipids are formulated at a 1:1 molar ratio and complexed with plasmid at a 4:1 molar ratio of DNA:cationic lipid.
Rabbit repeated dose toxicity study
The purpose of this study was to evaluate the safety of VCL-AB01 following repeated intramuscular (IM) administration in New Zealand White rabbits on Days 0,14,28 and 56. This study was performed in accordance with Institutional Animal Care and Use Committee (IACUC)-approved protocols, with the Guide for the Care and Use of Laboratory Animals (National Academy Press, 1996), and in compliance with the Good Laboratory Practices as set forth in 21 CFR 58.
Eighty New Zealand White rabbits (40 males and 40 females) approximately 13–17 weeks old with body weights between 2.2 and 2.9 kg at the onset of the study were used. Four groups of ten animals per sex were used in each test group. Each animal was injected IM in the vastus lateralis (the same muscle for each administration) with 1 mL of either PBS, a. low (0.2 mg/mL) or high dose (2 mg/mL) concentration of VCL-AB01 [1 mg each of VCL-6292 and VCL-62952 plasmids formulated with DMRIE/DOPE (964 µg DMRIE/1,128 µg DOPE) in PBS]. The 2 mg/mL dose was the highest dose of VCL-AB01 used in the Phase 1 clinical trial. A high dose (2 mg/mL) VCL-AB01 pDNA in PBS was used as a control to evaluate any possible safety issues associated with the DMRIE/DOPE delivery system. All test and control articles in this study were produced and packaged in Vical’s manufacturing facility according to current Good Manufacturing Practices.
Animals were evaluated daily throughout the study for adverse clinical signs (ill health and behavioral changes). Injection sites were scored for signs of edema and erythema once during the pretreatment period, and daily throughout the study, and were graded on a scale of 0–4 for severity (Draize scoring), Fundoscopic (indirect ophthalmoscopy) and biomicroscopic (slit lamp) examinations were performed by a board-certified veterinary ophthalmologist on all animals once during the pretreatment period and once within 48 hours prior to sacrifice. Food consumption and change in body weights were monitored throughout the study. Laboratory investigations (hematology, coagulation and clinical chemistry) were performed on sera taken from all study animals once during the last week of the pretreatment period, and once each during Weeks 2, 4, 6, 8, 10 and 12. Sera taken from each animal were also evaluated for anti-nuclear antibodies and antibodies to ds DNA.
Five animals/sex/group were sacrificed 48 hours following the last injection. The remaining animals (5 animals/sex/group) were sacrificed four weeks following the last injection. Full necropsy was performed on all animals at both time points for gross and histological evaluation to determine if there were any pathological changes associated with 4 repeated injections of VCL-AB01 at either the high or the low dose compared to controls.
Numerical data were subjected to calculation of group means and standard deviations. Data were analyzed using the analysis of variance (ANOVA) and the significance of inter-group differences was analyzed using Dunnett’s t test. Statistical analysis was performed using SPSS for Windows, Version 11.0.1 (SPSS, Inc., Chicago, IL).
Phase 1 clinical trial
A Phase 1, randomized, double-blind, placebo-controlled, dose-escalating trial of VCL-AB01 was conducted at two sites, Baylor College of Medicine (Houston, TX) and the University of Rochester (Rochester, NY) from the summer of 2004 to the fall of 2005. The trial was performed to evaluate safety and immunogenicity according to a protocol approved by each center’s respective Institutional Review Board and Institutional Biosafety Committee, and was conducted in accordance with Good Clinical Practice (GCP) and the National Institutes of Health Guidelines for Research Involving Recombinant DNA Molecules Section III regarding human gene transfer experiments.
Healthy nonpregnant adults between the ages of 18 and 45 years were recruited to participate. Eligible subjects did not have acute or chronic illnesses by history or laboratory screening, and reported no history of allergy to vaccine components or history of severe reactions to vaccines. Receipt of anthrax vaccine in the past was an exclusion criterion. After giving informed consent, eligible subjects were randomized through a web-based data acquisition system (EMMES Corporation, Rockville, MD) to one of 4 study groups to receive investigational vaccine at a dose of 0.2 mg, 0.6 mg or 2 mg of total pDNA or PBS placebo administered at 0, 1 and 2 months (Table 1). Groups were enrolled sequentially at higher doses with a 14 day pause between groups for safety evaluation. Vaccine or placebo was administered as a 1 mL IM injection into the deltoid muscle of alternating arms for each injection. Subjects kept a daily diary of injection site and systemic symptoms and oral temperature during the week following each vaccination. Solicited local and systemic symptoms including discomfort, temperature, fatigue, chills/feverishness, rash and loss of appetite were evaluated. Concomitant medications taken during the trial were documented. Subjects were monitored after each immunization and examined on Days 2, 7 and 14 after each immunization for potential clinical AEs. A final phone call was made approximately 12 months after enrollment to identify and document the occurrence of any intercurrent SAE. A Safety Monitoring Committee consisting of one independent safety monitor at each site and at least one other independent safety monitor evaluated the safety results prior to dose escalation. Due to injection site reactogenicity observed at the 2 mg dose level after the first immunization, the second and third immunizations in that Group were de-escalated to 0.6 mg. The schedule for the 0.6 mg group was delayed up to 2 weeks to complete the evaluation of the dose-related toxicity.
Blood samples for safety assessments were taken at Day 7 after each immunization. Biochemical and hematological evaluations performed included the following: human chorionic gonadotropin (when appropriate), blood urea nitrogen, creatinine, aspartate aminotransferase, alanine aminotransferase, total bilirubin, alkaline phosphatase, anti-double stranded DNA antibodies, ANA, hematocrit, hemoglobin, white blood cell count, platelet count, neurrophil count, lymphocyte count, eosinophil count. Antibody assays were performed using sera collected on Days 0, 14 and 28 and Weeks 6, 10, 28, 39 and 52. Sera were analyzed for anti-PA and anti-LF antibodies by enzyme-linked immunosorbent assay (ELISA) and for antibodies with toxin neutralizing activity (TNA) by an in vitro cell-based assay developed at the U.S. Centers for Disease Control and Prevention (CDC),18
Clinical endpoints and statistical analysis
The primary reactogenicity endpoints were the frequency and severity of solicited local and systemic AEs. Symptoms were graded as absent, mild (grade 1; noticeable but with no activity impairment), moderate (grade 2; sufficient to interfere with usual activities), severe (grade 3; incapacitating or unable to perform usual activities), or life-threatening (grade 4). Grade 3 and 4 reactions were considered to be SAEs. Injection site redness and swelling were graded based on size (0 = <5 mm; 1 = 5–49 mm; 2 = 50–99 mm; 3 = ≥100 mm). Fever was defined as an oral temperature ≥100°F.
The immunogenicity endpoints were the seroconversion frequency and levels of serum antibodies against PA and LF after receipt of all 3 doses. Clinical and serologic responses (PA- and LF-specific antibodies measured using ELISA and TNA) were assessed before and after each immunization, as described.
Differences in dichotomous variables were compared by chi-square or Fisher’s exact tests and continuous variables were compared using paired t tests and ANOVA. Linear least squares regression analyses of titers after immunization were used to evaluate dose response relationships, controlling for preimmunization antibody titers and gender. Statistical analyses were performed using SPSS version 14.0.2 (SPSS, Inc., Chicago, IL). The sample size determination was based on empirical evidence gathered from prior Phase 1 trials, in which the number of subjects per dose was adequate to rule out common AEs. If 10 subjects per dose group are enrolled, there is a 95% confidence of observing at least one occurrence of a specific AE given that the true proportion that would develop this AE in the population is 30%.
Enzyme-linked immunosorbent assay (ELISA) for anti-PA and anti-LF IgG antibodies
The ELISA to quantify anti-PA IgG in human and monkey sera was performed at Vical Incorporated according to the method of Quinn et al.18 with recombinant PA (List Biological Laboratories; Campbell, CA) as a solid phase immobilized antigen and horseradish peroxidase (HRP)-conjugated mouse anti-human gamma chain-specific (PAN) monoclonal antibody (clone HP6043, Hybridoma Reagent Laboratory, Baltimore, MD) with 2,2'-azino-bis-(3-ethylbenzylthiazoline-6-sulphonic acid, ABTS) substrate (Kirkegaard & Perry Laboratories, KPL, Gaithersburg, MD) as the reporter or signal system. For monkey sera, HRP-conjugated mouse anti-monkey IgG was used instead of mouse anti-human IgG. Each plate was required to pass acceptance criteria using CDC reference serum. Subjects were considered to be responders to PA if one or more of their serum samples collected after vaccination: (a) exceeded the reactivity threshold of ≥3 µg/mL18 for a subject with nonreactive or 0 values before vaccination, or (b) increased by ≥4 fold relative to baseline values for subjects with ≥3 µg/mL of PA antibody before vaccination.
The ELISA to quantify anti-LF IgG in human and monkey sera was performed at Vical Incorporated according to the method of Selinsky et al.19 This method is similar to that of the PA ELISA with the following modifications: (1) wells of Immulon 2-HB 96-well plates were coated with recombinant LF protein (List Biological Laboratories; Campbell, CA) in PBS; (2) the positive control, VCT530, was serially diluted two-fold in ELISA diluent [PBS containing 5% skim milk and 0.1% polyoxyethylene sorbitol monolaurate (Tween 20)] starting at 1/100 and, (3) each dilution was assayed in duplicate. For monkey sera, HRP-conjugated mouse anti-monkey IgG was used instead of mouse anti-human IgG. Each plate was required to pass acceptance criteria based on the performance of standard reference and quality control sera assayed in parallel with the test sera. Subjects were considered to be responders to LF if one or more of their serum samples collected after vaccination: (a) exceeded the reactivity threshold of ≥1.75 µg/mL19 for a subject with nonreactive or 0 values before vaccination, or (b) increased by ≥4 fold relative to baseline values for subjects with ≥1.75 µg/mL of LF antibody before vaccination.
Lethal toxin neutralizing activity (TNA) assay
The ability of human and monkey serum samples to neutralize the cytotoxic effects of anthrax lethal toxin was measured using the J774A.1 mouse macrophage cytotoxicity assay as previously described.17 TNA assays were performed at Vical Incorporated using a protocol and serum standards provided by Conrad Quinn, CDC. The reciprocal dilution of serum antibody that resulted in 50% neutralization of lethal toxin-mediated cell death (the ED50) was determined using a 4-PL curve fitting algorithm performed by SAS software (version 8.0) running an end-point calculation algorithm developed by the CDC.l8 Data were reported as the ED50 titers. To be considered a positive result, at least 2 points were required to be present on the curve above the threshold titer (TT) and the TT had to be at least 2x the starting dilution.
Monkey anthrax spore challenge study
VCL-AB01 was evaluated in a B. anthracis lethal spore challenge model at the Battelle Memorial Institute (Columbus OH). This study was performed in accordance with Batelle’s Institutional Animal Care and Use Committee approved protocols, and with the Guide for the Care and Use of Laboratory Animals (National Academy Press, 1996).
Only healthy animals prescreened to confirm seronegative status for anti-PA and anti-LF antibodies were included. VCL-AB01 from the same lot used in the clinical trial was administered as 0.6 mg/1 mL IM injections to cynomolgus macaques (2/sex) on Days 0, 14 and 28. A second group of controls received 1 mL IM injections of PBS according to the same schedule. All animals were aerosol challenged using a head-only exposure system 6 weeks after the last vaccination with an average dose of approximately 585 LD-50 Ames strain spores (range 311–1341). Spores were produced in a New Brunswick BioFlo 4500 Fermentor/Bioreactor (Edison, New Jersey) from a well characterized parent stock. A scale-up inoculum was produced and used to initiate fermentation, which continued until approximately 95 percent sporulation was reached. The culture was heat shocked for 45 min at 60°C, harvested, washed with sterile water and suspended in sterile water with 1% phenol for storage at 2–8°C. This spore lot was characterized for consistency with parent stock and purified by density gradient centrifugation. After challenge, animals were monitored closely for signs of disease. Temperature and bacteremia were also monitored (daily for 2 weeks and on Days 2, 4 and 6, respectively). Moribund animals were euthanized. Antibody assays to detect anti-PA and anti-LF antibodies and TNA were performed from sera collected prior to vaccination and at Weeks 4, 8, 10 and 13 (3 weeks after challenge).
Acknowledgements
The authors would like to thank Lisreina Toro, Robert Atmar, Shital Patel, Janer Wells and the staff at Baylor College of Medicine; Carrie Nolan, Diane O’Brien and the staff at the University of Rochester, School of Medicine and Dentistry; Holli Hamilton, Steve Heyse, Rosemary McCown, Ed Nuzum, Janet Shimko and Lanling Zou at the NIH/NIAID/DMID for their assistance with the clinical trial; Mark Perry, Jim Long and the staff at The Battelle Memorial Institute, Alice Chu for statistical analyses; and Dr. Holly Horton, Gail Fieser and Jackie Stupack for their expertise. We gratefully acknowledge the Safety Monitoring Committee members (Robert Edelman, Ann Falsey, Richard Sutton) for their participation in the clinical trial.
The nonclinical studies were supported by SBIR grant # 2R44AI053060-03. The clinical trial was supported by contracts N01-AI-25465, N01-AI-25460 and M01 RR00044 (NCRR).
Abbreviations
- AE
adverse event
- ALT
alanine aminotransferase
- ANOVA
analyses of variance
- ANA
antinuclear antibody
- AST
aspartate aminotransferase
- AVA
anthrax vaccine adsorbed
- B
bacillus
- BUN
blood urea nitrogen
- CDC
centers for disease control and prevention
- cGMP
current good manufacturing practices
- DMRIE
(±)-N-(2-hydroxyethyl)-N,N-dimethyl-2,3-bis(tetradecyloxy)-1-propanaminium Br
- DOPE
dioleoylphosphatidylethanolamine
- EF
edema factor
- ET
edema toxin
- ELISA
enzyme-linked immunosorbent assay
- ELISPOT
enzyme-linked immunosorbent spot
- GCP
good clinical practice
- hCG
human chorionic gonadotropin
- HRP
horseradish peroxidase
- IgG
immunoglobulin G
- IM
intramuscular
- IACUC
institutional animal care and use committee
- LF
lethal factor
- LT
lethal toxin
- PA
protective antigen
- PBS
phosphate-buffered saline
- pDNA
plasmid DNA
- rPA
recombinant protective antigen
- SAE
serious adverse event
- TNA
toxin neutralizing activity
- TT
threshold titer
- USAMRIID
united states army medical research institute of infectious diseases
- WBC
white blood cell
Footnotes
Presented in part at the 2005 Annual Meeting of the Infectious Diseases Society of America, San Francisco, CA.
Financial disclosure
A.R. and L.R.S. are employees of Vical Incorporated and declare financial holdings in the company.
References
- 1.Mock M, Fouer A. Anthrax. Annu Rev Microbiol. 2001;55:647–671. doi: 10.1146/annurev.micro.55.1.647. [DOI] [PubMed] [Google Scholar]
- 2.Inglesby TV, O'Toole T, Henderson DA, Bardett JG, Ascher MS, Eitzen E, et al. Anthrax as a biological weapon, 2002: updated recommendations for management. JAMA. 2002;287:2236–2252. doi: 10.1001/jama.287.17.2236. [DOI] [PubMed] [Google Scholar]
- 3.Meselson M, Guillemin J, Hugh-Jones M, Langmuir A, Popova I, Shelokov A, Yampolskaya O. The Sverdlovsk anthrax outbreak of 1979. Science. 1994;266:1202–1208. doi: 10.1126/science.7973702. [DOI] [PubMed] [Google Scholar]
- 4.Brookmeyer R, Blades N. Prevention of inhalational anthrax in the U.S. outbreak. Science. 2002;295:1861. doi: 10.1126/science.1068474. [DOI] [PubMed] [Google Scholar]
- 5.Bhatnagar R, Batra S. Anthrax toxin. Crit Rev Microbiol. 2001;27:167–200. doi: 10.1080/20014091096738. [DOI] [PubMed] [Google Scholar]
- 6.Campbell JD, Clement KH, Wasserman SS, Donegan S, Chrisley L, Kotloff KL. Safety, reactogenicity and immunogenicity of a recombinant protective antigen anthrax vaccine given to healthy adults. Hum Vaccin. 2007;3:205–211. doi: 10.4161/hv.3.5.4459. [DOI] [PubMed] [Google Scholar]
- 7.Gorse GJ, Keitel W, Keyserling H, Taylor DN, Lock M, Alves K, et al. Immunogenicity and tolerance of ascending doses of a recombinant protective antigen (rPA102) anthrax vaccine: randomized, double-blinded, controlled, multicenter trial. Vaccine. 2006;24:5950–5959. doi: 10.1016/j.vaccine.2006.05.044. [DOI] [PubMed] [Google Scholar]
- 8.Ferrari ME, Hermanson G, Rolland A. Development of anthrax DNA vaccines. Curr Opin Mol Ther. 2004;6:506–512. [PubMed] [Google Scholar]
- 9.Fellows PF, Linscott MK, Ivins BE, Pitt ML, Rossi CA, Gibbs PH, Friedlander AM. Efficacy of a human anthrax vaccine in guinea pigs, rabbits and rhesus macaques against challenge by Bacillus anthracis isolates of diverse geographical origin. Vaccine. 2001;19:3241–3247. doi: 10.1016/s0264-410x(01)00021-4. [DOI] [PubMed] [Google Scholar]
- 10.GU ML, Leppla SH, Kliuman DM. Protection against anthrax toxin by vaccination with a DNA plasmid encoding anthrax protective antigen. Vaccine. 1999;17:340–344. doi: 10.1016/s0264-410x(98)00210-2. [DOI] [PubMed] [Google Scholar]
- 11.Hermanson G, Whitlow V, Parker S, Tonsky K, Rusalov D, Ferrari M, et al. A cationic lipid-formulated plasmid DNA vaccine confers sustained antibody-mediated protection against aerosolized anthrax spores. Proc Natl Acad Sci USA. 2004;101:13601–13606. doi: 10.1073/pnas.0405557101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Little SF, Ivins BE, Fellows PE, Friedlander AM. Passive protection by polyclonal antibodies against Bacillus anthracis infection in guinea pigs. Infect Immun. 1997;65:5171–5175. doi: 10.1128/iai.65.12.5171-5175.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McBride BW, Mogg A, Telfer JL, Lever MS, Miller J, Turnbull PC, Baillie L. Protective efficacy of a recombinant protective antigen against Bacillus anthracis challenge and assessment of immunological markers. Vaccine. 1998;16:810–817. doi: 10.1016/s0264-410x(97)00268-5. [DOI] [PubMed] [Google Scholar]
- 14.Pitt ML, Little SF, Ivins BE, Fellows P, Barth J, Hewetson J, et al. In vitro correlate of immunity in a rabbit model of inhalational anthrax. Vaccine. 2001;19:4768–4773. doi: 10.1016/s0264-410x(01)00234-1. [DOI] [PubMed] [Google Scholar]
- 15.Vilalta A, Mahajan RK, Hartikka J, Leamy V, Martin T, Rusalov D, et al. Cationic lipid-formulated plasmid DNA-based Bacillus anthracis vaccine: evaluation of plasmid DNA persistence and integration potential. Hum Gene Ther. 2005;16:1151–1156. doi: 10.1089/hum.2005.16.1151. [DOI] [PubMed] [Google Scholar]
- 16.Pittman PR, Norris SL, Barrera Oro JG, Bedwell D, Cannon TL, McKee KT., Jr Patterns of antibody response in humans to the anthrax vaccine adsorbed (AVA) primary (six-dose) series. Vaccine. 2006;24:3654–3660. doi: 10.1016/j.vaccine.2006.01.054. [DOI] [PubMed] [Google Scholar]
- 17.Quinn CP, Dull PM, Semenova V, Li H, Crotty S, Taylor TH, et al. Immune responses to Bacillus anthracis protective antigen in patients with bioterrorism-related cutaneous or inhalation anthrax. J Infect Dis. 2004;190:1228–1236. doi: 10.1086/423937. [DOI] [PubMed] [Google Scholar]
- 18.Quinn CP, Semenova VA, Elie CM, Romero-Steiner S, Greene C, Li H, et al. Specific, sensitive and quantitative enzyme-linked immunosorbent assay for human immunoglobulin G antibodies to anthrax toxin protective antigen. Emerg Infect Dis. 2002;8:1103–1110. doi: 10.3201/eid0810.020380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Selinsky CL, Whitlow VD, Smith LR, Kaslow DC, Horton HM. Qualification and performance characteristics of a quantitative enzyme-linked immunosorbent assay for human IgG antibodies to anthrax lethal factor antigen. Biologicals. 2007;35:123–129. doi: 10.1016/j.biologicals.2006.07.003. [DOI] [PubMed] [Google Scholar]