When carefully performed, laparoscopic antireflux surgery is an effective, durable procedure for the control of gastroesophageal reflux disease.
Keywords: GERD, Gastroesophageal reflux disease, LARS, Laparoscopic antireflux surgery, Randomized controlled trials, RCT, Nissen fundoplication
Abstract
Background:
For nearly 2 decades, the laparoscopic correction of gastroesophageal reflux disease (GERD) has demonstrated its utility. However, the surgical technique has evolved over time, with mixed long-term results. We briefly review the evolution of antireflux surgery for the treatment of GERD, provide an update specific to the long-term efficacy of laparoscopic antireflux surgery (LARS), and analyze the factors predictive of a desirable outcome.
Materials and Methods:
PubMed and Medline database searches were performed to identify articles regarding the laparoscopic treatment of GERD. Emphasis was placed on randomized control trials (RCTs) and reports with follow-up >1 year. Specific parameters addressed included operative technique, resolution of symptoms, complications, quality of life, division of short gastric vessels (SGVs), mesh repair, and approximation of the crura. Those studies specifically addressing follow-up of <1 year, the pediatric or elderly population, redo fundoplication, and repair of paraesophageal hernia and short esophagus were excluded.
Results:
LARS has varied in technical approach through the years. Not until recently have more long-term, objective studies become available to allow for evidenced-based appraisals. Our review of the literature found no long-term difference in the rates of heartburn, gas-bloat, antacid use, or patient satisfaction between laparoscopic Nissen and Toupet fundoplication. In addition, several studies have shown that more patients had an abnormal pH profile following laparoscopic partial as opposed to total fundoplication. Conversely, dysphagia was more common following laparoscopic total versus partial fundoplication in 50% of RCTs at 12-month follow-up, though this resolved over time, being present in only 20% with follow-up >24 months. We confirmed that preoperative factors, such as hiatal hernia, atypical symptoms, poor antacid response, body mass index (BMI), and postoperative vomiting, are potential predictors of an unsatisfactory long-term outcome. Last, no trial disfavored division of the short gastric vessels (SGVs), closure of the crura, or mesh repair for hiatal defects.
Conclusion:
LARS has significantly evolved over time. The laparoscopic total fundoplication appears to provide more durable long-term results than the partial approach, as long as the technical elements of the operation are respected. Division of the SGVs, closure of the crura, and the use of mesh for large hiatal defects positively impacts long-term outcome. Hiatal hernia, atypical symptoms, poor antacid response, body mass index (BMI), and postoperative vomiting are potential predictors of failure in LARS.
INTRODUCTION
Rudolph Nissen was the first to pioneer antireflux surgery in 1956.1 His initial 360° approach would subsequently come to be modified by André Toupet,2 Jacques Dor,3 Vicente Guarner,4 and Mario Rossetti.5 The premise for the modification of Nissen's original technique was to address various complications unique to antireflux surgery (such as dysphagia and gas-bloat syndrome) and disease processes of the esophagus (such as disorders of motility).
In 1991, the laparoscopic approach to antireflux surgery was moved forward by Bernard Dallemagne.6 By the time that Dallemagne and others were publishing their first reports of laparoscopic antireflux surgery (LARS) in the early 1990s, the utility in controlling gastroesophageal reflux disease (GERD) by open fundoplication had been established.7–9 However, even after 3 decades of antireflux surgery, much contention persisted as to which variation of fundoplication to use.10–12 Unfortunately, this contention has carried over to the laparoscopic era of antireflux surgery, and seems to persist to this day.13–15 Varin et al,16 in their recent metaanalysis of total versus partial fundoplication for GERD, concluded that many trials are of insufficient quality, are lacking in objectivity, and are too heterogeneous to reliably come to a serious consensus on the best operative technique and their predictors of success. Until larger, more objective studies come forth, Varin et al furthermore concluded that the laparoscopic antireflux approach be tailored to the surgeon's comfort level, based on evidence that still remains limited.
The goal of this review is to provide an additional avenue of clarity regarding paradigm shifts in LARS, long-term outcomes of laparoscopic fundoplication, and predictors of a successful surgical outcome.
MATERIALS AND METHODS
PubMed and Medline database searches were performed to obtain articles regarding both open and laparoscopic anti-reflux surgery for the treatment of GERD with follow-up >1 year. The searched articles appeared in print between January 1951 and December 2009. All articles appeared in peer-reviewed journals. The key words utilized in the search are as follows: “surgery/gastroesophageal reflux disease,” “laparoscopic surgery/gastroesophageal reflux disease,” “laparoscopic surgery/gastroesophageal reflux disease/long-term results,” “laparoscopic surgery/gastroesophageal reflux disease/failure,” and “laparoscopic surgery/gastroesophageal reflux disease/randomized trial.” Additional articles were obtained via a manual search of the references included in the essential articles. Articles related to the following were excluded: short esophagus, paraesophageal hernia, redo-fundoplication, those converted to open, trials with <1 year of follow-up, and those specific to either elderly or pediatric patients. The following were parameters that were analyzed: criteria for patient selection, partial versus total fundoplication, changes in the standard of practice, and long-term results or effectiveness with respect to the amelioration of symptoms, recurrence of symptoms, and anatomic failure.
RESULTS
Evolution of Antireflux Surgery and Paradigm Shifts in LARS
The initial surgical approach to the refluxing patient began with Philip Allison in 1951, and his attempt at hiatal hernia repair.17 His thoracic approach, posterior crural repair, and left phrenic nerve crush would fall into disfavor because of the poor patient outcome and high recurrence of hiatal hernia. The most proper beginnings, therefore, began with Nissen's report on fundoplication in 1956.1 This technique of fundoplication, involving a 360° wrap and gastropexy for the treatment of hiatal hernias, was adopted shortly thereafter as an acceptable anti-reflux procedure within the surgical community. Later, variations of the technique were described by others, such as Dor from Marseille, who posited a partial anterior fundoplication for the treatment of achalasia in 1962.3
Although Nissen's procedure improved reflux symptoms, it soon became evident that some patients who underwent a total fundoplication were troubled by dysphagia, bloating, and the inability to belch, the so-called “gas-bloat syndrome.” To avoid these side effects, in 1963 André Toupet advocated for the creation of a posterior partial (270°) fundoplication, termed a “semi-fundoplicative maneuver.”2 Baue and Belsey18 and Hill19 would follow in 1967, with their approaches aimed at restoring the normal physiology of the lower esophageal sphincter (LES). In 1975, Vicente Guarner from Mexico described a posterior fundoplasty in which the fundus of the stomach was passed behind the esophagus, thus forming between the esophagus and the right aspect of the fundus a 120° angle in the left upper quadrant on an imaginary circle. This procedure did not require division of the SGVs.4 Subsequently, Rossetti5 proposed in 1977 a revision that included a modified total fundoplication with minimal-dissection of the cardia and no division of the SGVs.
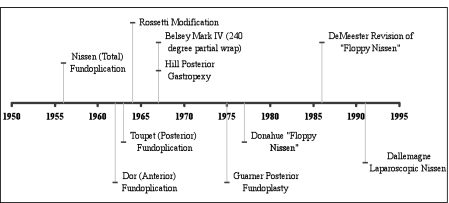
Unfortunately, these modifications still did not address recognized issues of postoperative dysphagia and the “gas-bloat” syndrome, for which Donahue and Bombeck pursued, with success, a “floppy Nissen.”20 DeMeester would soon recognize the benefits of this approach and publish his modifications and successful outcomes in 1986.12 In the 1990s, the advent of laparoscopic surgery revolutionized the surgical approach to the patient with GERD when the laparoscopic Nissen fundoplication was described by Dallemagne in 1991 (Figure 1).6 Soon thereafter, many modifications of the laparoscopic Nissen fundoplication were developed, by replicating laparoscopically the original modifications of the open techniques.
Figure 1.
Evolution of fundoplication.
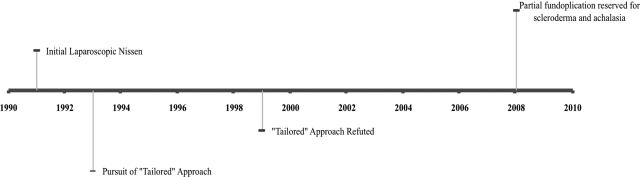
From 1991, then, the application of laparoscopic Nissen fundoplication for the treatment of GERD would undergo its own paradigm shifts. During the early stages of LARS, many agreed that those patients with esophageal dysmotility were at risk for dysphagia, and a “tailored approach” came into vogue.21 However, the report in 1999 by Horvath et al14 would dispel this myth, as they demonstrated reflux in 46% after partial fundoplication. The studies by Fibbe et al in 200122 and Patti et al in 200423 would confirm these findings, and the “tailored approach” would become disfavored. Finally, in an attempt to address an elevated prevalence of early dysphagia following total fundoplication, the “floppy” laparoscopic Nissen fundoplication seems to have become favored by many as the standard surgical procedure regardless of preoperative esophageal function, with a partial fundoplication reserved for those with achalasia and scleroderma without esophageal peristalsis (Figure 2).24
Figure 2.
Paradigm shifts in laparoscopic antireflux surgery.
Long-Term Results of LARS
From 1997 through 2009, 13 randomized control trials (RCTs) were identified that assessed the outcome of LARS (Table 1).25–37 Four26,28,32,36 of these 13 RCTs demonstrated follow-up of 60 months or more. The surgical approach varied considerably: Nissen versus anterior fundoplication, (3) Nissen-Rossetti versus anterior fundoplication, (3) Nissen versus Toupet, (6) Toupet versus anterior fundoplication, (2) and Nissen versus Nissen-Rossetti. (1) Two studies included were longer-term assessments of the same patient population that had been previously reported at least 12 months postoperatively. Initial sample size ranged from 39 to 200 patients.
Table 1.
Long-term Outcome of Laparoscopic Antireflux Surgery for Gastroesophageal Reflux Disease Based on Randomized Control Trials
| Study Author (Year) | N | Follow-up (months) | Procedure Type | Major Morbidity | Re-operation | Dysphagia to Solids | Dysphagia to Liquids | Heartburn | Gas Bloat | Post-op pH Studies | Post-op H2-Blockers or Proton Pump Inhibitors | Satisfaction (Percent or Score) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baigrie, 200527 | 163 | 24 | Nissen | – | 4 | 0.6a,b | 0.1b | 0.2c | NS | – | – | 9.6 |
| Anterior | 6 | 0.1a,b | 0.0b | 0.2c | 9.7 | |||||||
| Ludemann, 200528 | 107 | 60 | Nissen | – | 3 | 2.6a,b | 1.0b | 1.8c | NS | – | 12% | 8.0 |
| Cai, 200832 | Anterior | 3 | 1.5a,b | 0.6b | 1.9c | 4% | 8.7 | |||||
| 107 | 120 | Nissen | – | 5 | 2.4b | 1.4b | 1.7c | NS | – | 19% | 8.2 | |
| Anterior | 5 | 1.7b | 1.0b | 2.3c | 27% | 8.3 | ||||||
| Spence, 200629 | 100 | 12 | Nissen-Rossetti | 7 | 3 | 49%a | 3 | 12% | NS | 0%a | – | NS |
| Anterior | ||||||||||||
| 2 | 2 | 13%a | 0 | 16% | 0.7%a | |||||||
| Laws, 199733 | 39 | 27 | Nissen | 0 | – | NSe | – | – | – | – | 4% | 91% |
| (Mean) | Toupet | 2 | 0% | 100% | ||||||||
| Guérin, 200734 | 140 | 36 | Nissen | 0 | – | 2 | 0 | 4 | NS | – | – | 91% |
| Toupet | 3 | 0 | 0 | 3 | 89% | |||||||
| Booth, 200830 | 127 | 12 | Nissen | 0 | 2%d | 27%a,e | – | 24% | NS | 0.1%a | – | – |
| Toupet | 1 | 9%a,e | – | 24% | 0.4%a | |||||||
| Strate, 200831 | 200 | 24 | Nissen | 3%d | 15a | 19a,e | – | – | 25% | 20g | – | 85% |
| Toupet | 4a | 8a,e | 13% | 15g | 85% | |||||||
| Mickevicius, 200835 | 153 | 12 | Nissen | 2 | 3%d | NSe | – | – | – | – | 7%g | – |
| Toupet | 5 | 9%g | ||||||||||
| Shaw, 200936 | 100 | 55–60 | Nissen | – | 4 | NSe | – | NS | NS | – | 2 | NS |
| (Mean) | Toupet | 3 | 1 | |||||||||
| Hagedorn, 200325 | 95 | 12 | Toupet | – | – | NSe | – | Favors | – | – | – | – |
| Toupeta | ||||||||||||
| Engström, 200726 | Anterior | 24%a | ||||||||||
| 95 | 60 | Toupet | – | 1 | NSe | – | 60%a | – | – | 7%a | 93%a | |
| Anterior | 5 | 23%a | 59%a | |||||||||
| Chrysos, 200137 | 78 | 12 | Nissen | 2 | – | 17% | 0% | 4% | 38% | – | – | NS |
| Nissen-Rossetti | 1 | 16% | 0% | 0% | 19% |
Indicates significance, P≤0.05.
Dysphagia based on visual analogue scale.
Heartburn based on visual analogue scale.
Not stratified by operative technique.
Distinction between dysphagia to solids or liquids not made.
Trend toward significance.
Significance not reported.
RCT=Randomized control trial; NS=No significance between groups; Dashes=no data recorded.
There was no long-term difference for relief of heartburn in any study that evaluated total versus partial fundoplication, suggesting that both techniques equally resolve typical symptoms of GERD. Hagedorn et al25 and Engström et al26 found a higher prevalence of postoperative heartburn in patients after the anterior fundoplication as opposed to the posterior fundoplication, both at 12 months (P<0.001) and 60 months (60% versus 24%, P<0.0001).
All trials reported on the long-term incidence of dysphagia following LARS. Assessment for dysphagia was performed in a varied fashion, though most often by visual analogue scale (VAS) or questionnaire. Not all studies reported dysphagia to solids and liquids independently. In 2 of 3 studies assessing Nissen versus anterior fundoplication and in the study assessing Nissen-Rossetti versus anterior fundoplication, patients at long-term follow-up displayed an increased prevalence of dysphagia to solids.27–29 This phenomenon was mirrored in some respects by those trials evaluating Nissen fundoplication versus Toupet, whereby 2 of 6 studies30,31 again demonstrated an increased prevalence of dysphagia in the Nissen group. No difference was demonstrated between anterior fundoplication and Toupet, or Nissen and Nissen-Rossetti. Of note, in only 1 of 5 trials of longer than 2-year follow-up comparing total versus partial fundoplication was there a significant difference in dysphagia.28
Nine of the 13 trials reported on gas-bloat, with none demonstrating a difference between groups. Postoperative pH testing was not commonly reported, as data were reported in only 3 of the 13 trials. In 2 of these, there appeared to be a protective effect against reflux for total rather than partial fundoplication.29,30 Both of these studies had only shorter follow-up, thus further long-term results are difficult to discern. None of these studies reporting on postoperative pH testing reported postoperative use of histamine blockers or proton pump inhibitors (PPIs), though 6 others did. Of these, only the study by Engström et al26 noted any difference in antisecretory use, which occurred at 60 months with a higher prevalence in anterior fundoplication versus Toupet, coinciding with a higher prevalence of heartburn. No difference was found for total versus partial fundoplication in the postoperative use of antacid therapy.
Last, 10 of the 13 randomized control trials reported on patient satisfaction, either by percentage satisfied or score. Again, Engström et al26 noted a difference in their study at 60 months, with more patients having undergone anterior fundoplication versus Toupet demonstrating their dissatisfaction. However, in all trials comparing total versus partial fundoplication, there was no difference in patient satisfaction, which remained high at long-term follow-up regardless of the approach.
LARS appears to be associated with minimal morbidity, most often in less than 5% of cases. The group studied by Spence et al29experienced the highest rate of morbidity in any single category; however, the 7% morbidity in the Nissen-Rossetti group did not reach significance compared with the 2% experienced in the anterior fundoplication group. The necessity of reoperation was similarly infrequent throughout the studies, with the exception being the study of Strate et al.31 This group reported 19 reoperations for patient dissatisfaction (10% of study group, 15 who underwent Nissen and 4 who underwent Toupet, P<0.05). All patients were found to have a wrap herniation from disrupted hiatoplasty.
Factors Predictive of LARS Failure
Various pre- and postoperative features are commonly implicated in the failure of LARS (Table 2).14,31,38–50 In those studies identifying such potential predictors, the laparoscopic approach to antireflux intervention was varied. Preoperative disorders of peristalsis appeared to be the weaker predictor of LARS failure, reaching statistical significance in only 1 of 5 studies.38 On the contrary, the presence preoperatively of atypical symptoms, poor response to preoperative antacids, and postoperative vomiting, indicated a more pronounced predictive value, occurring in over 60% of included studies. Body mass index (BMI) >30 or 35 was correlated with poor operative outcome in 33% of studies. Finally, the presence of hiatal hernias >3cm was a predictor of failure in 38% of the studies.
Table 2.
Predictors of Laparoscopic Antireflux Surgery Failure
| Study Author (Year) | N | Procedure Type | Disorders of Peristalsis | Hiatal Hernia | Atypical Symptoms | Poor Response to Antacids | BMI | Postoperative Vomiting |
|---|---|---|---|---|---|---|---|---|
| Bell, 199938 | 143 | Toupet | p=0.003 | – | – | – | NS | – |
| Campos, 199939 | 199 | Nissen | 0% | 12%c | p=0.0001 | p<0.05 | NSd,e | – |
| Failure | Failure | |||||||
| Horvath, 199914 | 48 | Toupet | 7% | 64%b | – | – | – | – |
| Failure | Failure | |||||||
| Soper, 199940 | 290 | Nissen | – | p<0.005b | NS | – | – | p<0.0001 |
| Jackson, 200141 | 100 | Nissen (77) | NS | NSc | p<0.002 | p<0.0007 | – | – |
| Toupet (4) | ||||||||
| Perez, 200142 | 187 | Nissen | – | – | – | – | p=0.03 | – |
| Hahnloser, 2002f,43 | 126 | Nissen | – | NSb | NS | – | p<0.05 | 20%e |
| Failure | ||||||||
| Winslow, 200344 | 505 | Varied | – | – | – | – | NS | – |
| Power, 200445 | 131 | Nissen | – | p<0.001b | – | p<0.001 | – | – |
| D'Alessio, 200546 | 257 | Nissen | – | – | – | – | NS | – |
| Iqbal, 200647 | 41 Case | Nissen | – | 50%a,b | – | 42% | NS | 29%a |
| 50 Control | Failure | Failure | Failure | |||||
| Morgenthal, 200748 | 174 | Nissen | – | 25%b,c | 59%a | 44%a | 57%a | – |
| Failure | Failure | Failure | Failure | |||||
| Antoniou, 200849 | 32 | Nissen | – | – | – | 5% | – | – |
| Failure | ||||||||
| Strate, 200831 | 200 | Nissen (100) | 17% | – | – | – | – | – |
| Toupet (100) | Failure | |||||||
| Chisholm, 200950 | 481 | Varied | – | – | – | – | NS | – |
Significant difference at least P<0.05.
Hiatal hernia >3 cm.
Size of hiatal hernia not mentioned, or <2 cm.
100% of patients with BMI >38 had poor outcome.
Significance not reported.
Study based on postoperative complications.
Predictors are defined as demonstrating failure of physiologic improvement, patient dissatisfaction, or necessity of reoperation.
BMI=Body Mass Index; NS=Not significant; Dashes=no data recorded.
Over the years, specific details of the operative techniques that are independent of the skills of the surgeon and that may impact outcome have been identified (Table 3).37,38,40,51–61 The studies we reviewed had a large sample size, adequate follow-up, and addressed each technical variable specifically. Although some differences were noted as to the predictive value of each technical variable, no study disfavored division of the SGVs, closure of the crura, or mesh repair for hiatal defects.37,38,40,51–55
Table 3.
Operative Technique and Laparoscopic Antireflux Surgery
| Study Author (Year) | N | Procedure Type | Division of Short Gastrics | Closure of Crura | Mesh Repair |
|---|---|---|---|---|---|
| Bell, 199938 | 143 | Toupet | Favorsa | ND | – |
| Division | |||||
| Soper, 199940 | 290 | Variable Nissen (53), | Favors | Favorsa | – |
| Standard Nissen (237) | Division | Closure | |||
| Blomqvist, 200059 | 99 | Nissen | ND | – | – |
| Mardani, 200960 | 99 | Nissen | ND | – | – |
| Chrysos, 200137 | 78 | Nissen, Nissen-Rossetti | ND | – | – |
| Kamolz, 200251 | 200 | Nissen | – | – | Favors |
| Granderath, 200552 | 100 | Nissen | – | – | Mesh |
| Favors | |||||
| Mesh | |||||
| Turkcaper, 200754 | 551 | Toupet | – | – | Favors |
| Mesh | |||||
| Farah, 200756 | 90 | Nissen | ND | – | – |
| O'Boyle, 200257 | 102 | Nissen | ND | – | – |
| Yang, 200858 | 102 | Nissen | ND | – | – |
| Kösek, 200961 | 41 | Nissen | ND | – | – |
| Soricelli, 200955 | 297 | Varied | – | – | Favors |
| Mesh |
Statistically significant.
N=Number of patients, ND=No difference.
Dashes=no data recorded.
DISCUSSION
Antireflux surgery has been an evolving process for over half a century. Changes in technique were aimed at improving patient outcome and satisfaction. Starting with the laparoscopic age of antireflux surgery in 1991, paradigms in technique and patient approach shifted along the lines of technological advance. Oftentimes, information gleaned from postoperative follow-up was for <1 year, limiting the surgeon's perspective as to the true outcome of a particular modification in technique. Unfortunately, this methodology carried over from the previous 30 or so years of antireflux surgery, whereby objectivity in the form of RCTs was few and far between. Presently, we are on the cusp of 2 full decades of experience with LARS. Though the “tailored approach” has fallen into disfavor, there is still no true international consensus on the basic technique of total versus partial fundoplication; however, some evidence suggests that a partial fundoplication ought to be reserved for those with achalasia and GERD secondary to scleroderma.24 Indeed, LARS has come full circle to using the same concept of a “floppy” Nissen proposed by Donahue8 and DeMeester12 before laparoscopy was even introduced.
Our review of RCTs for long-term outcome in LARS was hampered by an impoverished standardization in reporting morbidity and reoperation, as well as in standardization of outcome assessment. Studies relied heavily on subjective determinations of postoperative dysphagia, gas-bloat, heartburn, and overall patient satisfaction, leaving comparison of these parameters between trials arduous. The most consistent objectivity that we found was in the analysis of postoperative pH testing, manometry, and use of H2-blockers or PPIs, though the intertrial consistency of these objective parameters is questionable. Nonetheless, particular patterns are apparent and consistent.14,24,62 First, either laparoscopic total or partial fundoplication result in equivalently low rates of heartburn at long-term follow-up. Only one group undertook long-term randomized comparison of 2 partial approaches to fundoplication. In anterior versus posterior fundoplication, Engström et al26 demonstrated more heartburn after the anterior approach, which persisted to 60 months. Not surprisingly, those patients in the anterior fundoplication group were more likely to require medical management of their recurrent disease and to be significantly dissatisfied with their results. Second, most RCTs demonstrated a higher incidence of postoperative dysphagia with total fundoplication as opposed to partial fundoplication, yet this persisted in only 1 of 5 trials with greater than 24 months of follow-up.28 Third, those few studies that reported on postoperative esophageal pH testing data showed that partial fundoplication resulted in a higher prevalence of acid reflux than total fundoplication did at long-term follow-up.29,30 This is in line with the current understanding that dysphagia with total fundoplication is more common, yet that it diminishes overtime, affording the patient a greater likelihood of freedom from acid reflux with no difference in heartburn or gas-bloat.
We also sought to identify the factors predictive of LARS failure (Tables 2 and 3). Many of the studies suggested that large hiatal hernias, atypical symptoms, poor response to medical reflux management, an elevated BMI, and postoperative vomiting are potential predictors for long-term failure. Interestingly, only the group in the Bell et al study,38 that used a posterior fundoplication, noted any increased rate of failure for those with disorders of peristalsis, in line with the notion that a tailored approach is unnecessary. In addition, the DeMeester score, the presence of Barrett's esophagus and esophagitis, and a defective LES have all been additionally implicated as independent predictors in some series, though this is not uniform throughout the studies.14,37,41,48 Similarly, variations in technique, including division of the SGVs, closure of the crura, and prosthetic repair of the hiatus may influence long-term outcomes. Indeed, no study identified a benefit to leaving the SGVs intact, and Bell et al38 and Soper et al40 found statistical differences to favor their division. Shorter-term studies and the metaanalysis by Catarci et al uphold this conclusion.63,64 Last, some reports have focused on the utility of prosthetic closure of the hiatus, with a consensus in favor of using mesh for this purpose.51–55 However, a recent case series by Stadlhuber et al65 places a caveat on the use of mesh, and given their findings they propose multicenter prospective studies to further validate its use.
Finally, it is the authors' position that tailoring of technique to weak peristalsis should not be routinely practiced except in the face of achalasia or GERD secondary to scleroderma. In addition, we favor complete mobilization of the gastric fundus and meticulously approximated crural pillars. Our approach is that supported by the best attempts to interpret the limited body of consistent and objective literature regarding long-term outcomes in LARS.
CONCLUSION
Since its beginnings, LARS has been slow to assume an evidence-based understanding of fundoplication technique, and the approach has meandered from variation to variation. Although we are now afforded more objectivity by way of esophageal testing and a handful of long-term RCTs, a clear discrepancy remains in the laparoscopic approach, pre- and postoperative analysis, and report of study findings regarding the patient with GERD. Nevertheless, it appears that laparoscopic total fundoplication affords more durable long-term results than the partial fundoplication, provided that potential predictors of failure are identified early and that the technical elements of the operation are respected.
References:
- 1. Nissen R. Eine einfache Operation zur Beeinflussung der Refluxoesophagitis. Schweiz Med Wochenschr. 1956;86:590–592 [PubMed] [Google Scholar]
- 2. Toupet A. Technic of esophago-gastroplasty with phrenogastropexy used in radical treatment of hiatal hernias as a supplement to Heller's operation in cardiospasms. Mem Acad Chir (Paris). 1963;89:384–389 [PubMed] [Google Scholar]
- 3. Dor J, Humbert P, Dor V, Figarella J. L'interet de la technique de Nissen modifiee dans la prevention du reflux apres cardiomyotomie extramuqueuse de Heller. Mem Acad Chir (Paris). 1962;3:877–883 [Google Scholar]
- 4. Guarner V, Degollade JR, Tore NM. A new antireflux procedure at the esophagogastric junction: experimental and clinical evaluation. Arch Surg. 1975;110(1):101–106 [DOI] [PubMed] [Google Scholar]
- 5. Rossetti M, Hell K. Fundoplication for the treatment of gastroesophageal reflux in hiatal hernia. World J Surg. 1977;1(4):439–443 [DOI] [PubMed] [Google Scholar]
- 6. Dallemagne B, Weerts JM, Jehaes C, Markiewicz S, Lombard R. Laparoscopic Nissen fundoplication: preliminary report. Surg Laparosc Endosc. 1991;1(3):138–143 [PubMed] [Google Scholar]
- 7. Spechler SJ. Comparison of medical and surgical therapy for complicated gastroesophageal reflux disease in veterans. The Department of Veterans Affairs Gastroesophageal Reflux Disease Study Group. N Engl J Med. 1992;326(12):786–792 [DOI] [PubMed] [Google Scholar]
- 8. Donahue PE, Samelson S, Nyhus LM, Bombeck CT. The floppy Nissen fundoplication. Effective long-term control of pathologic reflux. Arch Surg. 1985;120(6):663–668 [DOI] [PubMed] [Google Scholar]
- 9. Henderson RD, Marryatt G. Total fundoplication gastroplasty. Long-term follow-up in 500 patients. Thorac Cardiovasc Surg. 1983;85(1):81–87 [PubMed] [Google Scholar]
- 10. Shirazi SS, Schulze K, Soper RT. Long-term follow-up for treatment of complicated chronic reflux esophagitis. Arch Surg. 1987;122(5):548–552 [DOI] [PubMed] [Google Scholar]
- 11. Thor KB, Silander T. A long-term randomized prospective trial of the Nissen procedure versus a modified Toupet technique. Ann Surg. 1989;210(6):719–724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. DeMeester TR, Bonavina L, Albertucci M. Nissen fundoplication for gastroesophageal reflux disease. Evaluation of primary repair in 100 consecutive patients. Ann Surg. 1986;204(1):9–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Watson DI, Jamieson GG, Pike GK, Davies N, Richardson M, Devitt PG. Prospective randomized double-blind trial between laparoscopic Nissen fundoplication and anterior partial fundoplication. Br J Surg. 1999;86(1):123–130 [DOI] [PubMed] [Google Scholar]
- 14. Horvath KD, Jobe BA, Herron DM, Swanstrom LL. Laparoscopic Toupet fundoplication is an inadequate procedure for patients with severe reflux disease. J Gastrointest Surg. 1999;3(6):583–591 [DOI] [PubMed] [Google Scholar]
- 15. Shaw JM, Bornman PC, Callanan MD, Beckingham IJ, Metz DC. Long-term outcome of laparoscopic Nissen and laparoscopic Toupet fundoplication for gastroesophageal reflux disease: a prospective, randomized trial. Surg Endosc. 2009. September 30 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 16. Varin O, Velstra B, De Sutter S, Ceelen W. Total vs partial fundoplication in the treatment of gastroesophageal reflux disease: a meta-analysis. Arch Surg. 2009;144(3):273–278 [DOI] [PubMed] [Google Scholar]
- 17. Allison PR. Reflux esophagitis, sliding hiatal hernia, and the anatomy of repair. Surg Gynecol Obstet. 1951;92(4):419–431 [PubMed] [Google Scholar]
- 18. Baue J, Belsey RHR. The treatment of sliding hiatus hernia and reflux esophagitis by the Mark IV technique. Surgery. 1967;62:396–406 [Google Scholar]
- 19. Hill LD. An effective operation for hiatal hernia: an eight year appraisal. Ann Surg. 1967;166:681–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Donahue PE, Bombeck PT. The modified Nissen fundoplication – reflux prevention without gas bloat. Rev Surg. 1977;11:15–27 [Google Scholar]
- 21. Kauer WK, Peters JH, DeMeester TR, Heimbucher J, Ireland AP, Bremner CG. A tailored approach to antireflux surgery. J Thorac Cardiovasc Surg. 1995;110(1):141–147 [DOI] [PubMed] [Google Scholar]
- 22. Fibbe C, Layer P, Keller J, Strate U, Emmermann A, Zornig C. Esophageal motility in reflux disease before and after fundoplication: a prospective, randomized, clinical, and manometric study. Gastroenterology. 2001;121(1):5–14 [DOI] [PubMed] [Google Scholar]
- 23. Patti MG, Robinson T, Galvani C, Gorodner MV, Fisichella PM, Way LW. Total fundoplication is superior to partial fundoplication even when esophageal peristalsis is weak. J Am Coll Surg. 2004;198(6):863–870 [DOI] [PubMed] [Google Scholar]
- 24. Patti MG, Gasper WJ, Fisichella PM, Nipomnick I, Palazzo F. Gastroesophageal reflux disease and connective tissue disorders: pathophysiology and implications for treatment. J Gastrointest Surg. 2008;12(11):1900–1906 [DOI] [PubMed] [Google Scholar]
- 25. Hagedorn C, Jönson C, Lönroth H, Ruth M, Thune A, Lundell L. Efficacy of an anterior as compared with a posterior laparoscopic partial fundoplication: results of a randomized, controlled clinical trial. Ann Surg. 2003;238(2):189–196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Engström C, Lönroth H, Mardani J, Lundell L. An anterior or posterior approach to partial fundoplication? Long-term results of a randomized trial. World J Surg. 2007;31(6):1221–1227 [DOI] [PubMed] [Google Scholar]
- 27. Baigrie RJ, Cullis SN, Ndhluni AJ, Cariem A. Randomized double-blind trial of laparoscopic Nissen fundoplication versus anterior partial fundoplication. Br J Surg. 2005;92(7):819–823 [DOI] [PubMed] [Google Scholar]
- 28. Ludemann R, Watson DI, Jamieson GG, Game PA, Devitt PG. Five-year follow-up of a randomized clinical trial of laparoscopic total versus anterior 180 degrees fundoplication. Br J Surg. 2005;92(2):240–243 [DOI] [PubMed] [Google Scholar]
- 29. Spence GM, Watson DI, Jamiesion GG, Lally CJ, Devitt PG. Single center prospective randomized trial of laparoscopic Nissen versus anterior 90 degrees fundoplication. J Gastrointest Surg. 2006;10(5):698–705 [DOI] [PubMed] [Google Scholar]
- 30. Booth MI, Stratford J, Jones L, Dehn TC. Randomized clinical trial of laparoscopic total (Nissen) versus posterior partial (Toupet) fundoplication for gastro-oesophageal reflux disease based on preoperative oesophageal manometry. Br J Surg. 2008;95(1):57–63 [DOI] [PubMed] [Google Scholar]
- 31. Strate U, Emmermann A, Fibbe C, Layer P, Zornig C. Laparoscopic fundoplication: Nissen versus Toupet two-year outcome of a prospective randomized study of 200 patients regarding preoperative esophageal motility. Surg Endosc. 2008;22(1):21–30 [DOI] [PubMed] [Google Scholar]
- 32. Cai W, Watson DI, Lally CJ, Devitt PG, Game PA, Jamieson GG. Ten-year clinical outcome of a prospective randomized clinical trial of laparoscopic Nissen versus anterior 180 (degrees) partial fundoplication. Br J Surg. 2008;95(12):1501–1505 [DOI] [PubMed] [Google Scholar]
- 33. Laws HL, Clements RH, Swillie CM. A randomized, prospective comparison of the Nissen fundoplication versus the Toupet fundoplication for gastroesophageal reflux disease. Ann Surg. 1997;225(6):647–654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Guérin E, Bétroune K, Closset J, et al. Nissen versus Toupet fundoplication: results of a randomized and multicenter trial. Surg Endosc. 2007;21(11):1985–19890 [DOI] [PubMed] [Google Scholar]
- 35. Mickevicius A, Endzinas Z, Kiudelis M, et al. Influence of wrap length on the effectiveness of Nissen and Toupet fundoplication: a prospective randomized study. Surg Endosc. 2008;22(10):2269–2276 [DOI] [PubMed] [Google Scholar]
- 36. Shaw JM, Bornman PC, Callanan MD, Beckingham IJ, Metz DC. Long-term outcome of laparoscopic Nissen and laparoscopic Toupet fundoplication for gastroesophageal reflux disease: a prospective, randomized trial. Surg Endosc. 2009. September 30 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 37. Chrysos E, Tzortzinis A, Tsiaoussis J, Athanasakis H, Vasssilakis J, Xynos E. Prospective randomized trial comparing Nissen to Nissen-Rossetti technique for laparoscopic fundoplication. Am J Surg. 2001;182(3):215–221 [DOI] [PubMed] [Google Scholar]
- 38. Bell RC, Hanna P, Mills MR, Bowrey D. Patterns of success and failure with laparoscopic Toupet fundoplication. Surg Endosc. 1999;13(12):1189–1194 [DOI] [PubMed] [Google Scholar]
- 39. Campos GM, Peters JH, DeMeester TR, et al. Multivariate analysis of factors predicting outcome after laparoscopic Nissen fundoplication. J Gastrointest Surg. 1999;3(3):292–300 [DOI] [PubMed] [Google Scholar]
- 40. Soper NJ, Dunnegan D. Anatomic fundoplication failure after laparoscopic antireflux surgery. Ann Surg. 1999;229(5):669–677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Jackson PG, Gleiber MA, Askari R, Evans SR. Predictors of outcome in 100 consecutive laparoscopic antireflux procedures. Am J Surg. 2001;181(3):231–235 [DOI] [PubMed] [Google Scholar]
- 42. Perez AR, Moncure AC, Rattner DW. Obesity adversely affects the outcome of antireflux operations. Surg Endosc. 2001;15(9):986–989 [DOI] [PubMed] [Google Scholar]
- 43. Hahnloser D, Schumacher M, Cavin R, Cosendey B, Petropoulos P. Risk factors for complications of laparoscopic Nissen fundoplication. Surg Endosc. 2002;16(1):43–47 [DOI] [PubMed] [Google Scholar]
- 44. Winslow ER, Frisella MM, Soper NJ, Klingensmith ME. Obesity does not adversely affect the outcome of laparoscopic antireflux surgery (LARS). Surg Endosc. 2003;17(12):2003–2011 [DOI] [PubMed] [Google Scholar]
- 45. Power C, Maguire D, McAnena O. Factors contributing to failure of laparoscopic Nissen fundoplication and the predictive value of preoperative assessment. Am J Surg. 2004;187(4):457–463 [DOI] [PubMed] [Google Scholar]
- 46. D'Alessio MJ, Arnaoutakis D, Giarelli N, Villadolid DV, Rosemurgy AS. Obesity is not a contraindication to laparoscopic Nissen fundoplication. J Gastrointest Surg. 2005;9(7):949–954 [DOI] [PubMed] [Google Scholar]
- 47. Iqbal A, Kakarlapudi GV, Awad ZT, et al. Assessment of diaphragmatic stressors as risk factors for symptomatic failure of laparoscopic Nissen fundoplication. J Gastrointest Surg. 2006;10(1):12–21 [DOI] [PubMed] [Google Scholar]
- 48. Morgenthal CB, Lin E, Shane MD, Hunter JG, Smith CD. Who will fail laparoscopic Nissen fundoplication? Preoperative prediction of long-term outcomes. Surg Endosc. 2007;21(11):1978–1984 [DOI] [PubMed] [Google Scholar]
- 49. Antoniou SA, Delivorias P, Antoniou GA, et al. Symptom-focused results after laparoscopic fundoplication for refractory gastroesophageal reflux disease–a prospective study. Langenbecks Arch Surg. 2008;393(6):979–984 [DOI] [PubMed] [Google Scholar]
- 50. Chisholm JA, Jamieson GG, Lally CJ, Devitt PG, Game PA, Watson DI. The effect of obesity on the outcome of laparoscopic antireflux surgery. J Gastrointest Surg. 2009;13(6):1064–1070 [DOI] [PubMed] [Google Scholar]
- 51. Kamolz T, Granderath FA, Bammer T, Pasiut M, Pointner R. Dysphagia and quality of life after laparoscopic Nissen fundoplication in patients with and without prosthetic reinforcement of the hiatal crura. Surg Endosc. 2002;16(4):572–577 [DOI] [PubMed] [Google Scholar]
- 52. Granderath FA, Schweiger UM, Kamolz T, Asche KU, Pointner R. Laparoscopic Nissen fundoplication with prosthetic hiatal closure reduces postoperative intrathoracic wrap herniation: preliminary results of a prospective randomized functional and clinical study. Arch Surg. 2005;140(1):40–48 [DOI] [PubMed] [Google Scholar]
- 53. Granderath FA, Carlson MA, Champion JK, et al. Prosthetic closure of the esophageal hiatus in large hiatal hernia repair and laparoscopic antireflux surgery. Surg Endosc. 2006;20(3):367–379 [DOI] [PubMed] [Google Scholar]
- 54. Turkcapar A, Kepenekci I, Mahmoud H, Tuzuner A. Laparoscopic fundoplication with prosthetic hiatal closure. World J Surg. 2007;31(11):2169–2176 [DOI] [PubMed] [Google Scholar]
- 55. Soricelli E, Basso N, Genco A, Cipriano M. Long-term results of hiatal hernia mesh repair and antireflux laparoscopic surgery. Surg Endosc. 2009. April 3 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 56. Farah JF, Grande JC, Goldenberg A, Martinez JC, Lupinacci RA, Matone J. Randomized trial of total fundoplication and fundal mobilization with or without division of short gastric vessels: a short-term clinical evaluation. Acta Cir Bras. 2007;22(6):422–429 [DOI] [PubMed] [Google Scholar]
- 57. O'Boyle CJ, Watson DI, Jamieson GG, Myers JC, Game PA, Devitt PG. Division of short gastric vessels at laparoscopic Nissen fundoplication: a prospective double-blind randomized trial with 5-year follow-up. Ann Surg. 2002;235(2):165–170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Yang H, Watson DI, Lally CJ, Devitt PG, Game PA, Jamieson GG. Randomized trial of division versus nondivision of the short gastric vessels during laparoscopic Nissen fundoplication: 10-year outcomes. Ann Surg. 2008;247(1):38–42 [DOI] [PubMed] [Google Scholar]
- 59. Blomqvist A, Dalenbäck J, Hagedorn C, Lönroth H, Hyltander A, Lundell L. Impact of complete gastric fundus mobilization on outcome after laparoscopic total fundoplication. J Gastrointest Surg. 2000;4(5):493–500 [DOI] [PubMed] [Google Scholar]
- 60. Mardani J, Lundell L, Lönroth H, Dalenbäck J, Engström C. Ten-year results of a randomized clinical trial of laparoscopic total fundoplication with or without division of the short gastric vessels. Br J Surg. 2009;96(1):61–65 [DOI] [PubMed] [Google Scholar]
- 61. Kösek V, Wykypiel H, Weiss H, et al. Division of the short gastric vessels during laparoscopic Nissen fundoplication: clinical and functional outcome during long-term follow-up in a prospectively randomized trial. Surg Endosc. 2009;23(10):2208–2213 [DOI] [PubMed] [Google Scholar]
- 62. Oleynikov D, Eubanks TR, Oelschlager BK, Pellegrini CA. Total fundoplication is the operation of choice for patients with gastroesophageal reflux and defective peristalsis. Surg Endosc. 2002;16(6):909–13 [DOI] [PubMed] [Google Scholar]
- 63. Hunter JG, Swanstrom L, Waring JP. Dysphagia after laparoscopic antireflux surgery. The impact of operative technique. Ann Surg. 1996;224(1):51–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Catarci M, Gentileschi P, Papi C, et al. Evidence-based appraisal of antireflux fundoplication. Ann Surg. 2004;239(3):325–337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Stadlhuber RJ, Sherif AE, Mittal SK, et al. Mesh complications after prosthetic reinforcement of hiatal closure: a 28-case series. Surg Endosc. 2009;23(6):1219–1226 [DOI] [PubMed] [Google Scholar]