Both laparoscopic occlusion and superselective embolization of the uterine artery for symptomatic uterine leiomyomata improved clinical symptoms in the majority of patients.
Keywords: Uterine myoma, Uterine artery occlusion, Laparoscopy
Abstract
Objective:
To compare the effectiveness and safety of uterine artery occlusion by laparoscopy versus embolization as a treatment modality for symptomatic uterine fibroids.
Methods:
Ninety-six premenopausal women with symptomatic uterine leiomyomata were studied. None of them desired further pregnancy. They were randomized to treatment either by laparoscopic occlusion (group 1) or by radiologic embolization of uterine arteries (group 2). The primary outcome measure was patient satisfaction as regards menstrual blood loss compared with pretreatment loss. Secondary outcome measures included postoperative pain, complications, secondary interventions, and failures.
Results:
Ninety women were followed for 1, 3, 6, and 12 months after both procedures. The primary outcome was comparable between the 2 groups (86.7% after laparoscopic occlusion versus 88.8% after embolization, with no statistically significant difference). After 12 months of follow-up, more patients resumed heavy periods in the uterine artery occlusion group [4/45 patients, 8.8% in occlusion group compared with 3/45 (6.6%) in embolization group, P=0.044].
Conclusion:
Both laparoscopic occlusion and superselective embolization of uterine arteries improved clinical symptoms in the majority of patients. At 12-month follow-up, embolization might be more effective.
INTRODUCTION
Uterine leiomyomata, which occurs in one of every 4 to 5 women during reproductive life, is the most common solid pelvic tumor in women.1 Menstrual abnormalities, especially menorrhagia, which often leads to iron deficiency anemia, are the most common complications of uterine leiomyoma.1
Hysterectomy is the most common treatment for symptomatic leiomyomata. Medical treatment combining progestogen and hormonal therapy gonadotropin releasing hormone agonists often meets with encouraging but transient results in uterine leiomyomas.2 Surgical procedures including myomectomy and hysterectomy often are needed later during the course of events.3,4 But in addition to the risks associated with surgical procedures, hysterectomy may be a cause of emotional trauma.5,6
For these reasons, the demand for alternative treatments has increased during the last decade, both by patients and by physicians looking for less invasive procedures. Uterine leiomyoma embolization has become one such alternative procedure, and laparoscopic occlusion of uterine vessels is suggested as another.
In a preliminary nonrandomized study,7 the authors reported a reduction in menstrual bleeding and reduction of leiomyoma volume after both uterine leiomyoma embolization and laparoscopic occlusion of uterine vessels. In the present randomized study, the clinical outcome of these 2 methods is compared. The reduction in bleeding after 6 months and 12 months, as measured by the patients' own assessment, was the primary outcome variable. Secondary outcome measures were the patients' own assessment of pressure symptom reduction, postoperative pain, and nausea registration on visual analogue scales, recovery time, complications, secondary interventions, and failures.
MATERIALS AND METHODS
The study was performed in the Department of Obstetrics and Gynecology and the Department of Radiology, Mansoura University Hospital. Ninety-six premenopausal women referred to the university clinic for uterine leiomyomas and menorrhagia or pressure symptoms between August 2006 and December 2008 were included in this randomized, nonblinded trial. Inclusion criteria were the women's own interpretation of increased amounts of bleeding, pressure symptoms, and an expressed desire not to have a hysterectomy. Exclusion criteria were suspicion of malignancy, subserous leiomyomata that could easily be removed by laparoscopic surgery, known adenomyosis, and uterus size exceeding the umbilical level. Submucous leiomyomata with a diameter of <3.5cm situated completely intracavitarily or with an intramural extension of >50% were considered more suitable for hysteroscopic resection and were therefore excluded. In addition, women wishing to have children were excluded, as were those with contraindications for surgery. All eligible patients attended a consultation by a gynecologist, which included a gynecological examination, ultrasonography (the preoperative uterine evaluations were carried out using ultrasound, which is the standard method for evaluating myomas at our hospital). The patients were informed about the possible risks and benefits of both treatments. After agreeing to participate, patients signed a written informed consent form before randomization took place. Randomization of 1:1 was undertaken in a total of 10 blocks of 10 patients each, using sealed envelopes. Five envelopes in each block of 10 were assigned to laparoscopic treatment and 5 to uterine leiomyoma embolization. The envelopes in each block were closed, mixed, and then numbered. Treatment was decided by drawing the next available envelope in ascending numerical order.
Suction evacuation using a double valve IPAS syringe with Carmen plastic cannula No. 6 was done for all patients to exclude malignancy and small intracavitary lesions.
Interventional radiologists performed the embolization procedure. The right femoral artery was punctured, and the uterine arteries intubated with a 4F Cobra catheter or a microcatheter. In all cases, both arteries were embolized with 355- to 500-micron polyvinyl alcohol particles.
The laparoscopic bilateral occlusion of the uterine arteries was carried out according to the standard technique established by Semme.8 The uterine arteries and the anastomotic sites between uterine and ovarian arteries were occluded using clips or bipolar coagulation. The anterior leaf of the broad ligament was opened with scissors, then a Maryland clamp was used to dissect the broad ligament towards its base. The roof of the ureteric canal was dissected, and skeletonization of the uterine artery from the ureter was carried out. The main stem of the uterine artery was occluded using 2 clips (Figure 1) or using bipolar coagulation. Cauterization of the anastomotic sites between uterine and ovarian arteries was then carried out and the procedure repeated on the other side.
Figure 1.
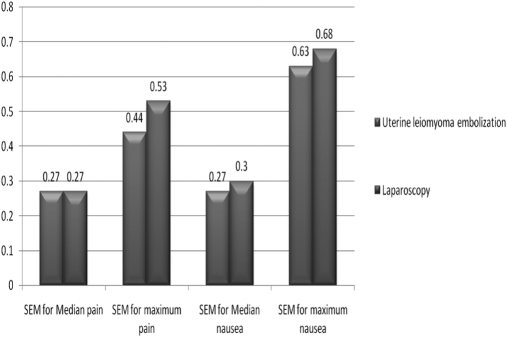
Pain and nausea recorded in the first 48 hours after treatment. SEM=standard error of the mean.
The participants were encouraged to use the same type of sanitary pads during the study period. The study participants were surveyed in relation to their present leiomyoma-related symptoms before treatment and after 1, 3, 6, and 12 months, respectively.
A standardized questionnaire was used at all appointments. The amount of bleeding was rated as “little,” “moderate,” “heavy,” or “very heavy.” Pressure symptoms, including voiding problems, were recorded as “yes” or “no.” Participants were asked to grade changes in amount of bleeding and pressure symptoms as better, worse, or unchanged. Total relief of symptoms at the 12-month follow-up was defined as little or moderate bleeding and no pressure symptoms. Clinical failure was defined as persisting symptoms requiring secondary treatment or no improvement at the 6-month follow-up. Postoperative pain and nausea during the hospital stay were recorded on postoperative charts. The resident doctors were asked to fill in the level of pain and nausea patients experienced every 4 hours during the first 24 hours in the hospital and every 6 hours during the next 24 hours or until the patient left the hospital. The analgesic regimen consisted of nonsteroidal anti-inflammatory drugs and paracetamol-codeine combination in fixed doses.
Adverse events were also recorded for each patient during the hospital stay and during outpatient visits after 1, 3, 6, and 12 months. All subsequent surgical and medical interventions, as well as readmission to the hospital or prolonged hospitalization, were recorded as adverse events. Doppler study of uterine arteries was done 48 hours after the procedure for all participants.
Statistical analysis was performed with SPSS 12.0 (Chicago, IL), and the data are presented as mean values for normal distributed data and as median values for skewed data. A 2-sided t test was used for comparisons of a continuous variable in 2 patient groups if the variable in question did not have a markedly skewed distribution. If the distribution was markedly skewed, a 2-sided Wilcoxon-Mann-Whitney test was used. A significance level of 0.05 was used for all tests. Power of the study and sample size was acheived using PASS 2008 (Power analysis and sample size, NCSS, Kaysville, UT, USA), we needed a sample size of 90 patients, 45 in each group, achieving 98% power to detect a difference of -1.0, between the null hypothesis that both group means were 0.0 and the alternative hypothesis that the mean of group 2 was 1.0, with estimated group standard deviations of 1.0 and 1.0 and with a significance level (alpha) of 0.05000 using a 2-sided 2-sample t test.9,10
RESULTS
Of the 96 patients randomized and included in the study, 90 patients received treatment, 45 with bilateral laparoscopic occlusion of uterine arteries (group 1) and 45 with uterine artery embolization (group 2). All participants in each group completed the 12-month trial. The 2 groups were similar with respect to age, body mass index, parity, and baseline symptoms.
The number of patients reporting reduced menstrual bleeding, reduction of pressure symptoms, or total relief of all symptoms after treatment did not differ significantly between the 2 treatment groups (Table 1).
Table 1.
Clinical Outcome at 1-Year Follow-up
| LOUA (n=45) | UAE (n=45) | P | |
|---|---|---|---|
| Bleeding Reduction | 39 | 40 | 0.69 |
| Reduction of Pressure Symptoms | 35 | 36 | 0.88 |
| Total Relief of Pressure | 33 | 35 | 0.15 |
| All Symptoms Completely Resolved | 35 | 37 | 0.18 |
| Satisfaction | 36 | 39 | 0.23 |
| Clinical Failure | 6 | 5 | 0.13 |
LOUA = laparoscopic occlusions of the uterine arteries; UAE = uterine artery embolization.
Clinical failure was seen in 5 (11.2%) subjects after uterine leiomyoma embolization and in 6 (13.3%) subjects after laparoscopic occlusion. There was no statistical difference between the 2 groups (P=0.13). However, there were 11/90 (12.2%) women still reporting heavy or very heavy bleeding 6 months after treatment: 5/45 (11.1%) after uterine leiomyoma embolization, and 6/45 (13.3%) after laparoscopic treatment (Table 1). The difference in the intention-to-treat analysis with regard to the number of patients who reported heavy bleeding was statistically insignificant (P=0.044). Four of these patients, 2 in the uterine leiomyoma embolization group and 2 in the laparoscopy group, did not meet the definition of clinical failure. All 4 participants reported improvement of symptoms, together with reductions in their bleeding and received no additional treatment during the study period. If these 4 participants had been added to the group of patients deemed clinical failures, there would have been 5 (11.2%) patients after uterine leiomyoma embolization and 6 (13.3%) after laparoscopy with unfavorable results 12 months after treatment (P=0.094).
Significantly more pain and nausea were observed after uterine leiomyoma embolization than after laparoscopy. The median amount of analgesic used after the embolization procedure was 4 times higher than after laparoscopic surgery: 46mg compared with 12mg (P<0.001). No significant difference occurred in bleeding reduction between the treatment groups 1 month after treatment (P=0.96). At 1-month follow-up, the subjects treated by uterine artery embolization had a mean bleeding assessment reduction of 88.8%, as opposed to 86.7% for those treated with laparoscopy. Also, at the 3-month follow-up, the subjects treated with uterine artery embolization had a mean bleeding assessment reduction of 88.9%, as opposed to 84.4% for those treated by laparoscopy (Table 2), while 6 months after uterine leiomyoma embolization, the reduction was still 88.9%, and the corresponding reduction for laparoscopic treatment was 86.7% (Table 2). At 12-month follow-up, the results were 91.9% versus 93.3% in group 1 and group 2, respectively (Table 2).
Table 2.
Adverse Events After Treatment at 3-, 6-, and 12-Month Follow-up
| LUAO |
UAE |
P | |||||
|---|---|---|---|---|---|---|---|
| 3m | 6m | 12m | 3m | 6m | 12m | ||
| Menorrhagia | 4 | 3 | 2 | 3 | 2 | 1 | 1.00 |
| Metrorrhagia | 3 | 3 | 2 | 2 | 3 | 2 | 1.00 |
| Recurrent pressure symptoms | 0 | 1 | 2 | 1 | 2 | 2 | 0.19 |
| Total | 7 | 7 | 6 | 6 | 7 | 5 | 0.12 |
LOUA = laparoscopic occlusions of the uterine arteries; UAE = uterine artery embolization.
Only minor in-hospital adverse events were observed. The patients were scheduled to stay for up to 48 hours in the department after treatment.
Twenty-two patients noticed increased vaginal discharge during the postoperative period, perhaps due to missed submucosal or intrauterine tumors in those patients. No significant differences were observed in the proportion of women with vaginal discharge extending to 7 days. The most serious adverse event, unilateral deep vein thrombosis, occurred in one patient who was readmitted to the hospital 1 week after laparoscopic bilateral occlusion.
DISCUSSION
The primary goal of the present study was to compare the improvement in bleeding patterns between uterine artery embolization and laparoscopic occlusion. No significant difference in symptom reduction was found between the 2 treatment options 12 months after treatment.
In the literature, one additional study11 reports using Pictorial Bleeding Assessment Chart reduction in 76 patients treated by embolization and reported improvement in 55.6% after 3 months and 58.1% after 6 months, which is significantly less than in our study.
The patients' own assessment of symptom relief is more commonly used as an outcome parameter than the Pictorial Bleeding Assessment Chart, even though there is a lack of uniformity in defining the degree of improvement. Notwithstanding these limitations, the present findings, based on the patients' own assessment 6 months after uterine leiomyoma artery embolization, are similar to those of other studies.2,3,5,6,11 The reduction of menstrual bleeding symptoms in 93.3% and 91.9% of the patients, after uterine leiomyoma embolization and laparoscopic occlusion, respectively, in this study is in accordance with the short-term results of the 2 largest prospective single-center studies evaluating uterine leiomyoma embolization to date, which reported improvements in menorrhagia in 89% of patients after 6 months and in 84% after 16 months, respectively.6,11 Furthermore, the reduction in the amount of bleeding in 91.9% of the patients after bilateral laparoscopic occlusion in this study is similar to that of other studies that report improvement in these symptoms in about 90% of the participants.
In contrast to the lack of difference between the 2 treatment groups with regard to the percentage reduction in patients' own assessment of bleeding, significantly more participants reported heavy or very heavy bleeding 6 months after laparoscopic treatment. One possible explanation for this discrepancy might be differences in the assessment of bleeding.
There are several possible explanations for the slightly less favorable results after laparoscopic treatment. In the literature, angiographic and surgical studies have shown numerous anatomical variations of the uterine arteries.12,13 It is thus possible to occlude the wrong artery in laparoscopy or to overlook one artery in cases where there are 2 instead of 1 single artery on one side. The reason for the failure was found to be insufficient occlusion of the uterine artery on one side.
The collateral arterial supply to the uterus in general could explain smaller amounts of pain after surgical uterine artery occlusion, in spite of ischemia and infarction of leiomyomata. Because embolization is a more distal occlusion reducing collateral flow, increased uterine ischemia can be expected, resulting in increased pain and potentially increased efficacy compared with proximal surgical occlusion. Concerns have been expressed among interventional radiologists that leiomyomata that are not completely infarcted will have the potential to regrow.13 In 2 prospective studies, 16%14 and 20%15 recurrence was found 5 years to 7 years after embolization. If smaller amounts of pain after laparoscopy were caused by less ischemia and thus incomplete infarction of leiomyomata, one would expect even more recurrences with time after laparoscopic occlusion.
The proportion of patients requiring secondary surgery was 5 (11.2%) in the UAE group and 6 (13.3%) in the LOUA group in our study. This proportion is in accordance with other reported outcomes after uterine leiomyoma embolization or laparoscopic occlusion. In 2 larger studies, subsequent interventions or readmission occurred in 10.5% after 21 months6 and in 7.5% after 17 months,11 respectively. In both of these studies, the main indications for secondary surgery were similar to those in this study: continuous menorrhagia or symptoms related to leiomyoma expulsion. Patient selection is probably most significant for beneficial results, and more careful selection might reduce the number of cases of secondary surgery caused by persistent menorrhagia or expulsion of leiomyomata.
Based on this study, both laparoscopic occlusion of the uterine vessel and embolization appear to improve symptoms associated with uterine leiomyomata in the majority of patients. The laparoscopic procedure resulted in less postoperative pain and nausea and shorter hospital stays, although significantly more participants experienced heavy menstrual bleeding 6 months after laparoscopic occlusion, indicating a more favorable effect after uterine leiomyoma embolization. In light of these results and bearing in mind the significant risk of surgical complications and lack of long-term results, considering the fact that the laparoscopic techniques are in the field of gynecologic surgery, laparoscopic uterine artery occlusion is likely to attract considerable interest as an effective alternative to hysterectomy treatment of symptomatic uterine leiomyomata.
CONCLUSION
To perform successful laparoscopic uterine artery occlusion, the surgeon has to be equipped with the necessary laparoscopic skills and should be able to precisely locate the uterine artery to correctly ligate the vessels. If these prerequisites are not met, massive bleeding may ensure necessitating laparotomy; therefore, the laparoscopic procedure for leiomyoma treatment should be confined to centers with appropriate expertise in laparoscopic surgery.
Contributor Information
Adel Helal, Department of Obstetrics and Gynecology, Mansoura University Hospitals, Faculty of Medicine, Mansoura University, Egypt..
Abd El-Mageed Mashaly, Department of Obstetrics and Gynecology, Mansoura University Hospitals, Faculty of Medicine, Mansoura University, Egypt..
Talal Amer, Department of Radiology, Mansoura University Hospitals, Faculty of Medicine, Mansoura University, Egypt..
References:
- 1. Vollenhoven BJ, Lawrence AS, Healy D. Uterine fibroids: a clinical review. Br J Obstet Gynecol. 1990;97:285–298 [DOI] [PubMed] [Google Scholar]
- 2. Worthington-Kirsch RL, Popky GL, Hutchins FL. Uterine arterial embolization for the management of leiomyomas: quality-of-life assessment and clinical response. Radiology. 1998;208:225–229 [DOI] [PubMed] [Google Scholar]
- 3. Goodwin SC, McLucas B, Lee M, et al. Uterine artery embolization for the treatment of uterine leiomyomata midterm results. J Vasc Interv Radiol. 1999;10:1159–1165 [DOI] [PubMed] [Google Scholar]
- 4. Healy D, Vollenhoven BJ. The role of GnRH agonists in the treatment of uterine fibroids. Br J Obstet Gynecol. 1992;99:23–26 [DOI] [PubMed] [Google Scholar]
- 5. Pelage JP, Le Dref O, Soyer P, et al. Fibroid-related menorrhagia: treatment with superselective embolization of the uterine arteries and midterm follow-up. Radiology. 2000;215:228–231 [DOI] [PubMed] [Google Scholar]
- 6. Spies JB, Ascher SA, Roth AR, Kim J, Levy EB, Gomez-Jorge J. Uterine artery embolization for leiomyomata. Obstet Gynecol. 2001;98:29–34 [DOI] [PubMed] [Google Scholar]
- 7. Hald K, Langebrekke A, Klow NE, Noreng HJ, Berge AB, Istre O. Laparoscopic occlusion of uterine vessels for the treatment of symptomatic fibroids: initial experience and comparison to uterine artery embolization. Am J Obstet Gynecol. 2004;190:37–43 [DOI] [PubMed] [Google Scholar]
- 8. Semm K, Mettler L. Technical progress in pelvic surgery via operative laparoscopy. Am J Obstet Gynecol. 1980;138:121. [DOI] [PubMed] [Google Scholar]
- 9. Machin D, Campbell M, Fayers P, Pinol A. Sample Size Tables for Clinical Studies. 2nd ed Malden, MA: Blackwell Science; 1997 [Google Scholar]
- 10. Zar Jerrold H. Biostatistical Analysis. 2nd ed Englewood Cliffs, New Jersey; Prentice-Hall; 1984 [Google Scholar]
- 11. Spis JB, Cooper JM, Worthington-Kirsch R, Lipman JC, Mills BB, Benenati JF. Outcome of uterine embolization and hysterectomy for leiomyomas: results of a multicenter study. Am J Obstet Gynecol. 2004;191:22–31 [DOI] [PubMed] [Google Scholar]
- 12. Walker WJ, Pelage JP. Uterine artery embolisation for symptomatic fibroids: clinical results in 400 women with imaging follow up. BJOG. 2002;109:1262–1272 [DOI] [PubMed] [Google Scholar]
- 13. Holub Z, Lukac J, Kliment L, Urbanek S. Variability of the origin of the uterine artery: laparoscopic surgical observation. J Obstet Gynaecol Res. 2005;31:158–163 [DOI] [PubMed] [Google Scholar]
- 14. Gomez-Jorge J, Keyoung A, Levy EB, Spies JB. Uterine artery anatomy relevant to uterine leiomyomata embolization. Cardiovasc Intervent Radiol. 2003;26:522–527 [DOI] [PubMed] [Google Scholar]
- 15. Iverson RE, Chelmow D, Strohbehn K, Waldman L, Evantash EG. Relative morbidity and mortality of abdominal hysterectomy and myomectomy for management of uterine leiomyomas. Obstet Gynecol. 1996;88:415–419 [DOI] [PubMed] [Google Scholar]