This study suggests that minimally invasive, laparoscopic techniques be considered for drainage of liver abscess before open exploration is performed.
Keywords: Liver, Abscess, Laparoscopy, Interventional radiology
Abstract
Background and Objectives:
Pyogenic liver abscesses are mainly treated by percutaneous aspiration or drainage under antibiotic cover. If interventional radiology fails, surgical drainage becomes necessary. Recently, we performed laparoscopic liver abscess drainage successfully, and we aimed to focus on the topic in light of a systematic review of the literature.
Methods:
A 22-year-old man was admitted with a 4.5-cm multiloculated abscess in the left lobe of the liver. The abscess did not resolve with antibiotic-alone therapy. Percutaneous aspiration was unsuccessful due to viscous and multiloculated contents. Percutaneous catheter placement was not amenable. Laparoscopic abscess drainage was preferred over open abscess drainage. We used 3 trocars, operation time was 40 minutes, and blood loss was minimal. In the mean time, we searched PubMed using the key words [(liver OR hepatic) abscess*] AND [laparoscop* OR (minimal* AND invasiv*)].
Results:
Postoperative recovery of the patient was uneventful, and the patient was asymptomatic after 3 months of follow-up. In the literature search, we found 53 liver abscesses (51 pyogenic and 2 amebic) that were treated by laparoscopy. Mean success rate was 90.5% (range, 85% to 100%) and conversion rate was zero.
Conclusion:
Treatment of liver abscess is mainly percutaneous drainage. Laparoscopic drainage should be selected as an alternative before open drainage when other modalities have failed.
INTRODUCTION
If untreated, nearly all pyogenic abscesses prove fatal. Treatment includes (a) drainage of the abscess, (b) combined with appropriate antibiotics, and (c) if present, elimination of the underlying source of infection. At present, advances in interventional radiology have enabled percutaneous interventions instead of surgery. However, some cases still require surgical drainage when other treatments fail. Laparoscopic surgery can be a viable alternative before open abscess drainage. We present here a liver abscess that did not resolve with nonsurgical methods, and laparoscopic drainage was successfully applied. In light of this case, we reviewed indications of different treatment modalities for pyogenic liver abscess and results of laparoscopy in the literature.
CASE REPORT
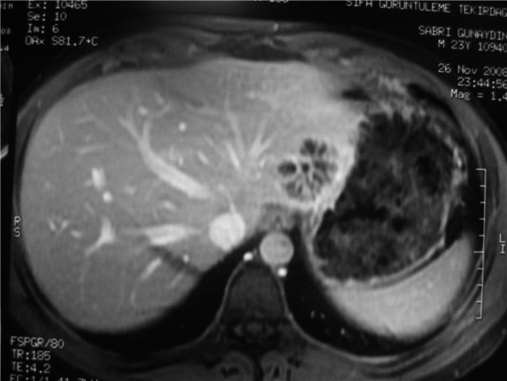
A 22-year-old man was admitted with a complaint of intermittent fever. He had received a diagnosis of liver abscess at another center 2 weeks earlier. The patient's clinician reported that the abscess was too small for drainage, and the patient was taking antibiotics (third-generation cephalosporins) only during this period. Antibiotic therapy had failed, and the patient was referred to our center for interventional radiology. He had no previously known disease, history of surgery, or coexisting intraabdominal pathology. Physical examination was normal except for mild epigastric tenderness. During his hospital stay, the patient's fever reached 38.2 °C at least 2 times each day. His white blood count was 10.500/mm3 with 76% neutrophils. Liver function tests were normal. Computed tomography and MRI revealed a 4.5-cm multiloculated abscess in the left lobe of the liver (Figure 1). During interventional radiology, a percutaneous aspiration was performed of 10mL of pus. The abscess was not amenable to catheter placement (too small for catheter placement), and antibiotic therapy was performed after aspiration (ceftriaxone 1g bid and clindamycin 300mg qid). Fever episodes did not resolve, and surgical drainage was planned. The patient was informed about open and laparoscopic drainage alternatives, and he decided on laparoscopy. While the patient was under general anesthesia, he was placed in a supine position, and pneumoperitoneum was established from an infraumbilical incision with a Veress needle. The abdomen was explored, and two 5-mm trocars were placed. One trocar was epigastric for liver retraction, and the other was left subcostal for drainage. The abscess was visualized under the left liver lobe adherent to the lesser curvature of the stomach. It was unroofed using electrocautery, and pus was aspirated. Debridement and irrigation of the abscess cavity were performed with an aspirator-irrigator apparatus. Laparoscopic ultrasonography was not used. A large-bored catheter was placed into the abscess cavity and taken out from the left subcostal trocar site. The operation time was 40 minutes, and operative blood loss was minimal. The postoperative course was uneventful. The patient was started on an oral diet on postoperative day one, and the catheter was removed on postoperative day 7 after a control computed tomography was performed (Figure 2). Microbiological tests revealed no species, probably due to prolonged antibiotic use. The patient was discharged on day 10, and antibiotics were continued for 2 weeks more. He was asymptomatic after 3 months of follow-up.
Figure 1.
Multiseptated abscess in the left lobe of the liver.
Figure 2.
Postoperative image of the abscess.
DISCUSSION
Several methods are available to treat pyogenic liver abscess. Patients presenting with multiple and small abscesses are the best candidates for antibiotic-alone therapy, but this therapy usually fails for a solitary liver abscess.1 In our case, antibiotic-alone therapy had been preferred at first but failed after 2 weeks of treatment. Percutaneous aspiration plus antibiotic therapy can be useful for small, solitary, unilocular abscesses, particularly in young healthy patients. Elderly, debilitated patients, multiloculated, with multiple or large abscesses have a higher failure rate with percutaneous aspiration.2,3 Our patient was thought to be a candidate for aspiration, but it failed probably due to multilocular and viscous content. Percutaneous catheter drainage recently appeared as the first-line treatment instead of surgical drainage, and it is successful in 70% to 90% of solitary and unilocular abscess.2,3 Coexisting abdominal pathology, coagulopathy, inaccessibility, massive ascites, small, multiloculated or multiple abscess are unsuitable for percutaneous drainage. Failure after catheter placement can result from catheter obstruction with pus, inappropriate catheter placement, premature catheter removal, untreated abscess, multiloculated abscess, or immunocompromised patients.4 We did not try catheter placement, because of small, multiloculated abscess with content that was too viscus. Surgery is indicated for failed percutaneous drainage and for patients who require hepatic resection.5,6 All surgically accessible liver abscesses are candidates for laparoscopic drainage.6 If a coexisting abdominal pathology is present that cannot be resolved by laparoscopy, then open surgery should be preferred.
We searched PubMed using the key words [(liver OR hepatic) abscess*] AND [laparoscop* OR (minimal* AND invasiv*)] and found 53 laparoscopically treated liver abscess (51 pyogenic and 2 amebic) reported in the literature.4–12 The mean success rate was 90.5% (range, 85% to 100%). The reported conversion rate of those 53 cases was zero. Laparoscopic surgery has the advantages of both open surgery and the minimal invasiveness of percutaneous drainage. In our case, surgery was indicated after treatment failure with antibiotic-alone therapy, percutaneous aspiration, and unsuitability for catheter placement, respectively. Indications for laparoscopic surgery were present, and the outcome was successful in this patient.
The absence of tactile sensation that makes the breakdown of septations and perihepatic adhesions difficult is one of the difficulties of laparoscopic abscess drainage. Laparoscopic drainage provides faster recovery, shorter hospital stay, less surgical-site infection, and better cosmesis than open surgical drainage does.4,6 Furthermore, severely ill patients who need surgical drainage can tolerate laparoscopy better than they can tolerate open drainage. Wang and associates6 reported that port-site positions for abscess drainage were similar to those for laparoscopic cholecystectomy. Others, like us, reported the use of only 3 trocars.5 Some authors used routine laparoscopic ultrasound.6,7 We believe that laparoscopic ultrasound is not mandatory for every case, particularly if the abscess wall is visible during laparoscopy. Some authors6,7 also report that the Harmonic scalpel is useful for unroofing of liver abscesses. We used electrocautery for opening the abscess wall, and there was no bleeding. A large-bore drain is essential for both laparoscopic and open surgical drainage. Although no randomized study compares surgical and percutaneous drainage, the failure rate can be expected to be higher in the percutaneous group because of smaller caliber drainage catheters. Large-bore tube drains prevent failure, provide quicker resolution of the abscess cavity, and laparoscopy permits placement of large-bore drains.13
CONCLUSION
Although treatment of liver abscess is mainly percutaneous drainage, indications for other treatment modalities should be keep in mind, and laparoscopic drainage should be selected as an alternative before open drainage.
References:
- 1. Pearce N, Knight R, Irving H, et al. Non-operative management of pyogenic liver abscess. HPB. 2003;5:91–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zerem E, Hadzic A. Sonographically guided percutaneous catheter drainage versus needle aspiration in the management of pyogenic liver abscess. AJR Am J Roentgenol. 2007;189:138–142 [DOI] [PubMed] [Google Scholar]
- 3. Rajak CL, Gupta S, Jain S, Chawla Y, Gulati M, Suri S. Percutaneous treatment of liver abscesses: needle aspiration versus catheter drainage. AJR Am J Roentgenol. 1998;170:1035–1039 [DOI] [PubMed] [Google Scholar]
- 4. Baca B, Hamzaoğlu I, Karahasanoğlu T, Hamzaoğlu HO. Laparoscopic treatment of pyogenic liver abscess complicating Crohn's disease: A case report. Turk J Gastroenterol. 2007;18:58–61 [PubMed] [Google Scholar]
- 5. Tay KH, Ravintharan T, Hoe MN, See AC, Chang HC. Laparoscopic drainage of liver abscesses. Br J Surg. 1998;85:330–332 [DOI] [PubMed] [Google Scholar]
- 6. Wang W, Lee WJ, Wei PL, Chen TC, Huang MT. Laparoscopic drainage of pyogenic liver abscesses. Surg Today. 2004;34:323–325 [DOI] [PubMed] [Google Scholar]
- 7. Yeh TS, Ho YP, Jan YY, Chen MF. Efficacy of color sonography and harmonic scalpel in laparoscopic management of multiple/lobulated liver cysts and abscesses. Hepatogastroenterology. 2007;54:485–488 [PubMed] [Google Scholar]
- 8. Iwamura K. Therapeutic utilization of laparoscopy in liver abscess cases. Tokai J Exp Clin Med. 1981;6:275–284 [PubMed] [Google Scholar]
- 9. Cappuccino H, Campanile F, Knecht J. Laparoscopy-guided drainage of hepatic abscess. Surg Laparosc Endosc. 1994;4:234–237 [PubMed] [Google Scholar]
- 10. Siu WT, Chan WC, Hou SM, Li MK. Laparoscopic management of ruptured pyogenic liver abscess. Surg Laparosc Endosc. 1997;7:426–428 [PubMed] [Google Scholar]
- 11. Short M, Desai AP. Laparoscopy and transdiaphragmatic thoracoscopy in management of ruptured amebic liver abscess. J Laparoendosc Adv Surg Tech A. 2008;18:473–476 [DOI] [PubMed] [Google Scholar]
- 12. Robles PJ, Lara JG, Lancaster B. Drainage of hepatic amebic abscess successfully treated by laparoscopy. J Laparoendosc Surg. 1994;4:451–454 [DOI] [PubMed] [Google Scholar]
- 13. Kayaalp C, Yol S, Nessar G. Drainage of liver abscess via laparoscopic trocar with local anesthesia. Surg Laparosc Endosc Percutan Tech. 2003;13:121–124 [DOI] [PubMed] [Google Scholar]