Intestinal perforation by a migrating intrauterine device is a serious complication and may be corrected by using a laparoscopic approach.
Keywords: Intrauterine device, Colon, Perforation, Laparoscopy
Abstract
Background:
Intrauterine device (IUD) migration and colon perforation is a rare but serious complication occurring sometimes years after insertion. Laparoscopic removal of a colon-perforating device is a seldom-used approach.
Case:
A 35-year-old presented with right upper quadrant (RUQ) abdominal pain one year following intrauterine device (IUD) insertion. Upon vaginal examination, no IUD string was detected. An abdominal X-ray depicted the IUD in a position below the hepatic flexure. Abdominal computerized tomography (CT) scan suggested an IUD-like foreign object posterior and medial to the hepatic flexure. Colon perforation by an intrauterine device was diagnosed, the device was identified and removed, and the intestinal damage was repaired with a laparoscopic approach.
Conclusion:
Clinical diagnosis and surgical removal of a perforating intrauterine device reduces the possible risks of abdominal complications this condition presents. In select cases, the laparoscopic approach for intrauterine device removal may be a simple and safe approach, thus minimizing possible postoperative complications.
INTRODUCTION
Since the introduction of the intrauterine device (IUD) by Richter in 1909, it has undergone many design modifications to increase its effectiveness and safety. Complications accompanying IUD insertion are uncommon, but may include expulsion, retraction into the cervix or uterus, bleeding, infection, ectopic pregnancy, and perforation through the uterine wall and into the abdominal cavity or neighboring organs.1
IUD migration and colon perforation is a rare but serious complication that can occur years after insertion. Laparoscopic removal of a colon-perforating device is a seldom-used approach.
CASE REPORT
A 35-year-old gravida 3 para 3 woman underwent, for the first time in her life, intrauterine device (IUD) insertion in 2002. The device used was a copper T (375). The insertion was uneventful and was the first time an IUD had been inserted.
A year later, she began complaining of right upper quadrant (RUQ) abdominal pain. Upon vaginal examination, no IUD string was detected. An abdominal X-ray depicted the IUD in a position below the hepatic flexure.
A month later, the patient was admitted to our medical center for evaluation and treatment.
Upon admission, she underwent a physical examination that detected no abnormalities, apart from light tenderness upon abdominal palpation of the RUQ. Vital signs were in the normal range. Her blood workup was normal with a white blood cell count=5180 (cells/μL) and neutrophils= 3040(cells/μL). An abdominal roentgenogram was performed that demonstrated a metallic foreign body in the abdominal cavity. An abdominal computerized tomography (CT) scan revealed an IUD located posterior and medial to the hepatic flexure, with light fat blurring of the surrounding tissues (Figure 1). Colonoscopy revealed normal colonic mucosa.
Figure 1.
CT scan reveals the location of the IUD. A coronal section of the patient's abdominal CT scan. Note the hyper-intense IUD-shaped object lodged within the colon just below the hepatic flexure (arrow).
Following these findings, the patient underwent abdominal laparoscopic surgery. Three access openings were created: a 10-mm diameter opening at the umbilicus, a 5-mm opening in the right lateral abdomen, and a 10-mm opening in the right middle abdomen area. During the operation, an IUD thread was noted in the mesocolon region of the hepatic flexure. Laparoscopic exploration revealed the IUD lodged in the colon serosa under the hepatic flexure (Figure 2). The IUD was excised, and the colonic defect was repaired using an EndoGIA. The operation was uneventful, and the patient made a full recovery. She was released 3 days after surgery.
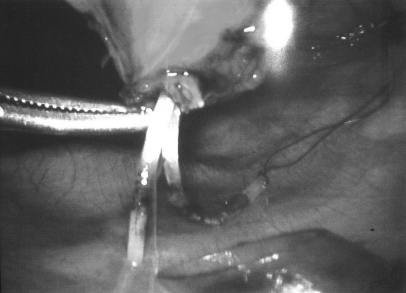
Figure 2.
Laparoscopic removal of the IUD. The IUD was extracted from the colon through an incision made in the colon wall. Note that the IUD was removed intact including the attached strings.
DISCUSSION
Since the introduction of the IUD by Richter in 1909, it has undergone many design modifications to increase its effectiveness and safety. As such, complications accompanying IUD insertion are uncommon, but may include expulsion, retraction into the cervix or uterus, bleeding, infection, ectopic pregnancy, and perforation through the uterine wall and into the abdominal cavity or neighboring organs.2 Among these, perforation is one of the most serious and may lead to abdominal cavity infection and organ failure. The incidence of uterine perforation is estimated to be between 1 in 350 to 2500 insertions.1 Perforation tends to occur in the immediate postinsertion period, especially during the first 6 months following insertion,3 but cases of uterine perforation have also been noted several years after insertion.4 The risk of IUD perforation is affected by several factors including the type of IUD, uterine size and position, timing of the insertion in relation to the last delivery or abortion, and the experience of the operator.2 Following perforation, IUDs may be found throughout the abdominal cavity. However, few cases exist in the literature describing perforation of adjacent organs.5–8
Symptoms of perforation are generally nonspecific. The suspicion of a perforating IUD should arise when patients present with abdominal pain, diarrhea, and fever accompanied by missing IUD strings and no detection of the IUD in the uterine cavity by a transvaginal ultrasound scan.1 Upon perforation into an adjacent organ, symptoms may present as acute inflammation of the perforated organ.4
Diagnosis of IUD perforation is usually made with the use of imaging modalities that depict the ectopic location of the device. Once suspicion of an immigrating IUD is proposed, a plain radiograph of the abdomen should be performed, followed by other, more precise modalities (ultra sound, CT), which assist in its localization.
Treatment for IUD removal is surgical, either by laparotomy or laparoscopy.9,10 In most cases, the repair of IUD withdrawal and perforation results in complete resolution of symptoms.3
CONCLUSION
We present a case of intestinal perforation by an IUD one year after its insertion. The device was located by using a colonoscopy and abdominal CT scan that showed it to be lodged within the large intestine, below the intestinal mucosa, under the hepatic flexure. The device was successfully removed by a laparoscopic approach.
The great advances made in recent years in minimally invasive laparoscopic surgery have resulted in a significant reduction in operative complications, and in the risk of postsurgical morbidity. Few reports in the past have shown that laparoscopic removal of an IUD is not only possible but a long-term established minimally invasive operative technique, that should be available to both general surgeons and gynecologists.9,10 Therefore, in patients suspected of having an IUD perforating the colon, laparoscopy for identifying, localizing, and assessing the intestinal trauma should be regarded as a first-line approach. Laparoscopic removal of the IUD and primary repair of the intestinal perforation should be considered according to the abdominal and pelvic findings, and the surgeon's skills.
Contributor Information
Arie Bitterman, Department of Surgery A, Carmel Medical Center, Haifa, Israel..
Oleg Lefel, Department of Surgery A, Carmel Medical Center, Haifa, Israel..
Yakir Segev, Department of Obstetrics and Gynecology, Carmel Medical Center, Haifa, Israel..
Ofer Lavie, Department of Obstetrics and Gynecology, Carmel Medical Center, Haifa, Israel..
References:
- 1. Heartwell SF, Schlesselman S. Risk of uterine perforation among users of intrauterine devices. Obstet Gynecol. 1983;61:31–36 [PubMed] [Google Scholar]
- 2. Key TC, Kreutner AK. Gastrointestinal complications of modern intrauterine devices. Obstet Gynecol. 1980;55:239–244 [PubMed] [Google Scholar]
- 3. Heartwell SF, Schlesselman S. Risk of uterine perforation among users of intrauterine devices. Obstet Gynecol. 1983;61:31–36 [PubMed] [Google Scholar]
- 4. Stuckey A, Dutreil P, Aspuru E, Nolan TE. Symptomatic cecal perforation by an intrauterine device with appendectomy removal. Obstet Gynecol. 2005;105:1239–1241 [DOI] [PubMed] [Google Scholar]
- 5. Chang HM, Chen TW, Hsieh CB, et al. Intrauterine contraceptive device appendicitis: a case report. World J Gastroenterol. 2005;11:5414–5415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ozgur A, Sismanoglu A, Yazici C, Cos ar E, Tezen D, Ilker Y. Intravesical stone formation on intrauterine contraceptive device. Int Urol Nephrol. 2004;36:345–348 [DOI] [PubMed] [Google Scholar]
- 6. Timonen H, Kurppa K. IUD perforation leading to obstructive nephropathy necessitating nephrectomy: a rare complication. Adv Contracept. 1987;3:71–75 [DOI] [PubMed] [Google Scholar]
- 7. Carson SA, Gatlin A, Mazur M. Appendiceal perforation by Copper-7 intrauterine contraceptive device. Am J Obstet Gynecol. 1981;141(5):586–587 [DOI] [PubMed] [Google Scholar]
- 8. Mederos R, Humaran L, Minervini D. Surgical removal of an intrauterine device perforating the sigmoid colon: a case report. Int J Surg. 2008;6(6):e60–e62 [DOI] [PubMed] [Google Scholar]
- 9. Heinberg EM, McCoy TW, Pasic R. The perforated intrauterine device: endoscopic retrieval. JSLS. 2008;12(1):97–100 [PMC free article] [PubMed] [Google Scholar]
- 10. Silva PD, Larson KM. Laparoscopic removal of a perforated intrauterine device from the perirectal fat. JSLS. 2000;4(2):159–162 [PMC free article] [PubMed] [Google Scholar]