Abstract
OBJECTIVE
To determine changes in gene expression in epicardial adipose tissue (EAT) associated with coronary atherosclerosis (CAD) and effects of pioglitazone therapy.
RESEARCH DESIGN AND METHODS
Genes were quantified by RT-PCR in EAT and thoracic subcutaneous adipose tissue (SAT) obtained during surgery in CAD patients with metabolic syndrome (MS) or type 2 diabetes and control subjects with minimal or no CAD and no MS or type 2 diabetes.
RESULTS
Increased expression of interleukin-1 receptor antagonist (IL-1Ra) and IL-10, a trend for higher IL-1β, and no change in peroxisome proliferator–activated receptor-γ (PPARγ) was found in EAT from MS or type 2 diabetes. Only PPARγ mRNA was reduced in SAT. Pioglitazone therapy in type 2 diabetes was associated with decreased expression of IL-1β, IL-1Ra, and IL-10 in EAT; decreased IL-10 in SAT; and increased PPARγ in SAT.
CONCLUSIONS
In MS and type 2 diabetes with CAD, proinflammatory and anti-inflammatory genes were differentially increased in EAT and selectively reduced in association with pioglitazone treatment.
In patients with multiple risk factors for coronary atherosclerosis (CAD), including type 2 diabetes, interleukin (IL)-1β and other proinflammatory genes and proteins are higher in epicardial adipose tissue (EAT) than subcutaneous adipose tissue (SAT) from the same patients (1) or EAT from patients without CAD (2), whereas anti-inflammatory IL-10 is increased (2) and anti-inflammatory adiponectin is reduced (3).The relative expression of pro- and anti-inflammatory mediators may determine whether EAT contributes in a harmful or protective paracrine manner to CAD (4), which might be therapeutically relevant (5).
IL-1β is secreted by classically activated M1 macrophages, whereas anti-inflammatory IL-1 receptor antagonist (IL-1Ra) and IL-10 are secreted by resident M2 or “alternatively activated” macrophages (6). IL-1Ra inhibits binding of IL-1β to and activation of its target cell receptor (7). IL-1Ra was identified in human visceral abdominal fat (VAT) and SAT by Juge-Aubry et al. (8). The balance between IL-1β and IL-1Ra (the IL-1Ra:IL-1β ratio) is considered to determine the severity of the chronic inflammatory disease (7), of which CAD is an example. Murine IL-1Ra gene knockout (9) and human IL-1Ra gene association studies (10) indicate an important role for IL-1Ra in atherosclerosis. To our knowledge, IL1-Ra has not been reported in EAT. The peroxisome proliferator–activated receptor-γ (PPARγ) mediates the anti-inflammatory action of thiazolidinediones in macrophages (6).
Our objectives were to determine inflammatory gene expression in EAT contiguous with CAD in patients with metabolic syndrome (MS) and type 2 diabetes and changes associated with pioglitazone therapy.
RESEARCH DESIGN AND METHODS
Control, MS, type 2 diabetic, and pioglitazone-treated type 2 diabetic patients’ age, sex, and anthropometric features; metabolic characteristics; drug therapy; study exclusion criteria; fat sample acquisition; mRNA isolation and quantification by RT-PCR; and statistical methods were previously described by us (11,12). In the current study, additional control subjects (12 vs. 6) were included; insulin resistance was estimated by homeostasis model assessment–insulin resistance (HOMA-IR) (13) in control subjects and MS patients. At the time of open heart surgery, seven type 2 diabetic patients had been treated with an average dose of 25 mg/day pioglitazone (range 15–45) for an average of 24 months (range 4–60), based on patient recalls of duration of therapy. Gensini scores of angiographic epicardial coronary atherosclerosis (14) were measured and were significantly lower in control subjects (mean 1.6, range 0–10) than in MS subjects (mean 29.7, range 6–62), type 2 diabetic patients (mean 38.0, range 10–100), and type 2 diabetic patients receiving pioglitazone (mean 30.9, range 17–80). The local institutional review board approved the study, and all patients involved gave their informed consent.
RESULTS
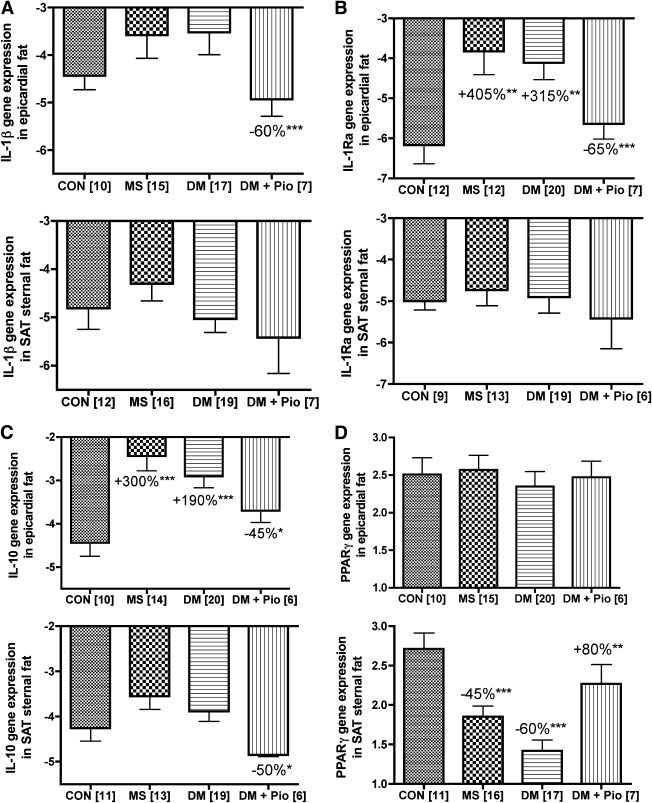
Figure 1B and C show that IL-1Ra and IL-10 mRNAs, respectively, were significantly higher in EAT from MS and type 2 diabetic than control patients, whereas PPARγ was similar (Fig. 1D). In anterior thoracic (sternal) SAT, only PPARγ mRNA was lower in MS and type 2 diabetes. There was a trend for higher IL1-β in EAT that was not statistically significant (Fig. 1A). However, IL-1β mRNA was significantly greater in EAT than in SAT when measured within patient groups. Thus, for control subjects, mean IL-1β ΔCp was −3.14 for EAT versus −4.73 for SAT (P = 0.003); for MS patients, mean IL-1β ΔCp was −3.44 for EAT versus −4.96 for SAT (P = 0.007), and, for type 2 diabetic patients, mean IL-1β ΔCp was −3.93 for EAT versus −5.90 for SAT (P = 0.02). Pioglitazone therapy in type 2 diabetic patients was associated with decreased expression of IL-1β, IL-1Ra, and IL-10 mRNA in EAT (Fig. 1A–C) as well as less IL-10 mRNA (Fig. 1C) and greater PPARγ (Fig. 1D) in SAT.
Figure 1.
IL-1β (A), IL-1Ra (B), IL-10 (C), and PPARγ (D) gene expression in epicardial and sternal subcutaneous fat (SAT) from controls (CON), MS, type 2 diabetic (DM), and type 2 diabetic patients treated with pioglitazone (DM + Pio). The data were normalized by the use of cyclophilin as the recovery standard in each run and shown as the means ± SEM of the ΔCp from cyclophilin, with the sign of the ΔCp values reversed so that the greater the number, the more mRNA. The mean ΔCp values for IL1-β, IL-1Ra, and IL-10 mRNAs assayed in EAT were corrected for the lower recovery of cyclophilin in the MS (0.87 units) and type 2 diabetic (0.81 units) groups. No correction was necessary for SAT, since cyclophilin Cp values in this depot were the same in all groups. Likewise, the cyclophilin Cp values in type 2 diabetic patients without and treated with pioglitazone were not significantly different, being 27.20 ± 0.39 and 27.45 ± 0.40 in SAT and 25.81 ± 0.28 and 25.96 ± 0.34 in EAT, respectively; therefore, no correction factor was necessary. Numbers of patients are shown in brackets. The % changes shown in the figures were derived from the ratios and significant differences in the MS or type 2 diabetic patients compared with control subjects as well as type 2 diabetic patients compared with type 2 diabetic patients treated with pioglitazone and are indicated as follows: *P < 0.05; **P < 0.01; ***P < 0.005. There were no significant differences in expression of the four genes in EAT and SAT between MS and type 2 diabetic patients.
IL-1Ra and IL-10 mRNAs in EAT from MS and type 2 diabetes that were significantly different from control subjects (Fig. 1) were tested in multiple factor covariate analyses for effects of age, weight, BMI, waist, fasting blood glucose, A1C, HOMA-IR, ACE inhibitors, angiotensin receptor blockers, statins, aspirin, and metformin. None of these variables had a significant impact on the effects arising from MS and type 2 diabetic patients versus control subjects, since these differences also persisted after multiple covariate analysis.
CONCLUSIONS
In patients with MS and type 2 diabetes with severe CAD, increased IL-1Ra and IL-10 mRNAs and an upward IL-1β trend were observed in EAT, whereas the three mRNA levels were similar in SAT, highlighting depot-specific gene expression differences and confirming higher IL-10 (2) in EAT contiguous with CAD.
Macrophages are densely concentrated in EAT around lipid-filled coronary atherosclerotic plaques (5). Although M1 and M2 macrophages have not been studied in EAT, our data suggested that increases in IL-1Ra and IL-10 expression in EAT might represent a protective mechanism mediated by M2 macrophages in response to activated M1 macrophages recruited possibly by “inside-to-outside” coronary signaling (1). The expression of IL-1β was not significantly enhanced in EAT, although there was an upward trend. However, IL-1β expression was greater in EAT compared with SAT within MS, type 2 diabetic, and control patient groups, suggesting the possibility that the lack of difference in IL-1β expression in EAT between MS patients, type 2 diabetic patients, and control subjects may have been due to masking by its higher expression in control subjects.
Treatment with pioglitazone in type 2 diabetic patients was associated with reductions in expression of IL-1β, IL-1Ra, and IL-10 in EAT and with only IL-10 in SAT. In this context, rosiglitazone has been shown to directly inhibit phorbol myristate acetate–activated but not basal IL-1Ra release from human SAT explants in vitro (8). Because pioglitazone suppresses macrophage-mediated adipose tissue inflammation and IL-1β (6), it can be hypothesized that during pioglitazone therapy, reduced IL1-Ra expression in EAT might have been an indirect consequence of reduced expression of IL-1β in EAT. Pioglitazone was also associated with a selective increase in PPAR-γ mRNA in SAT but not EAT. In as much as EAT is visceral fat originating embryologically from VAT (4), this finding was consistent with the report of greater pioglitazone-mediated upregulation of PPARγ transcripts in cultured human abdominal SAT preadipocytes than omental preadipocytes in vitro (15).
In conclusion, augmentation of anti-inflammatory IL-1Ra and IL-10 gene expression in EAT suggested a potentially beneficial role for these adipokines in a proinflammatory milieu contiguous with CAD. Treatment with pioglitazone in type 2 diabetic patients with CAD was associated with a reduction of proinflammatory and anti-inflammatory genes in EAT and a selective increase in PPARγ in SAT.
Acknowledgments
This study was supported by The Van Vleet Chair of Excellence, University of Tennessee; The Baptist Heart Institute and Foundation, Memphis, TN; and The Cardiometabolic Disease Research Foundation, Memphis, TN.
This study was also supported by Takeda Pharmaceuticals, Deerfield, IL. No other potential conflicts of interest relevant to this article were reported.
H.S.S. wrote the manuscript and researched data. J.N.F. and P.C. researched data and reviewed and edited manuscript. S.W.B. reviewed and edited the manuscript. E.G. and R.Y.W. provided adipose tissue and reviewed and edited the manuscript. D.W. and J.S. performed coronary angiogram analyses and reviewed and edited the manuscript.
The authors are indebted to James Karas, MS, Baptist Healthcare Corporation, for providing statistical analysis; to Dr. Bill Taylor and the staff of the Molecular Resource Center of University of Tennessee for access to and assistance with the Roche LightCycler 480 real-time PCR system; and to the Clinical Research Center staff of Baptist Hospital.
References
- 1.Mazurek T, Zhang L, Zalewski A, et al. Human epicardial adipose tissue is a source of inflammatory mediators. Circulation 2003;108:2460–2466 [DOI] [PubMed] [Google Scholar]
- 2.Eiras S, Teijeira-Fernández E, Salgado-Somoza A, et al. Relationship between epicardial adipose tissue adipocyte size and MCP-1 expression. Cytokine 2010;51:207–212 [DOI] [PubMed] [Google Scholar]
- 3.Lacobellis G, Pistilli D, Gucciardo M, et al. Adiponectin expression in human epicardial adipose tissue in vivo is lower in patients with coronary artery disease. Cytokine 2005;29:251–255 [DOI] [PubMed] [Google Scholar]
- 4.Sacks HS, Fain JN. Human epicardial adipose tissue: a review. Am Heart J 2007;153:907–917 [DOI] [PubMed] [Google Scholar]
- 5.Vela D, Buja M, Madjid M, et al. The role of peri-adventitial fat in atherosclerosis: an adipose subset with potential diagnostic and therapeutic implications. Arch Pathol Lab Med 2006;130:108–115 [Google Scholar]
- 6.Olefsky JM, Glass CK. Macrophages, inflammation, and insulin resistance. Annu Rev Physiol 2010;72:219–246 [DOI] [PubMed] [Google Scholar]
- 7.Goldbach-Mansky R. Blocking interleukin-1 in rheumatic diseases: its initial disappointments and recent successes in the treatment of autoinflammatory diseases: cytokine therapies. Ann N Y Acad Sci 2009;1182:111–123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Juge-Aubry CE, Somm E, Giusti V, et al. Adipose tissue is a major source of interleukin-1 receptor antagonist: upregulation in obesity and inflammation. Diabetes 2003;52:1104–1110 [DOI] [PubMed] [Google Scholar]
- 9.Nicklin MJH, Hughes DE, Barton JL, Ure JM, Duff GW. Arterial inflammation in mice lacking the interleukin 1 receptor antagonist gene. J Exp Med 2000;191:303–311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Francis SE, Camp NJ, Dewberry RM, et al. Interleukin-1 receptor antagonist gene polymorphism and coronary artery disease. Circulation 1999;99:861–866 [DOI] [PubMed] [Google Scholar]
- 11.Sacks HS, Fain JN, Holman B, et al. Uncoupling protein-1 and related messenger ribonucleic acids in human epicardial and other adipose tissues: epicardial fat functioning as brown fat. J Clin Endocrinol Metab 2009;94:3611–3615 [DOI] [PubMed] [Google Scholar]
- 12.Fain JN, Sacks HS, Bahouth SW, Tichansky DS, Madan AM, Cheema PS. Human epicardial adipokine mRNAs: comparisons with their expression in substernal, subcutaneous and omental fat. Metabolism 2010;59:1379–1386 [DOI] [PubMed] [Google Scholar]
- 13.Bonora E, Formentini G, Calcaterra F, et al. HOMA-estimated insulin resistance is an independent predictor of cardiovascular disease in type 2 diabetic subjects. Prospective data from the Verona Diabetes Complications study. Diabetes Care 2002;25:1135–1141 [DOI] [PubMed] [Google Scholar]
- 14.Gensini GG. A more meaningful scoring system for determining the severity of coronary heart disease. Am J Cardiol 1983;51:606. [DOI] [PubMed] [Google Scholar]
- 15.Sewter CP, Blows F, Vidal-Puig A, O’Rahilly S. Regional differences in the response of human pre-adipocytes to PPARgamma and RXRalpha agonists. Diabetes 2002;51:718–723 [DOI] [PubMed] [Google Scholar]