Abstract
We address the problem of how to integrate health information systems in low-income African countries in which technical infrastructure and human resources vary wildly within countries. We describe a set of tools to meet the needs of different service areas including managing aggregate indicators, patient level record systems, and mobile tools for community outreach. We present the case of Sierra Leone and use this case to motivate and illustrate an architecture that allows us to provide services at each level of the health system (national, regional, facility and community) and provide different configurations of the tools as appropriate for the individual area. Finally, we present a, collaborative implementation of this approach in Sierra Leone.
Keywords: Africa, architecture, capacity building, electronic health information systems, mobile devices, Sierra Leone
Introduction
African health authorities and international agencies alike increasingly understand the need for good health information systems (HIS) at all levels of the health system. The launch of the Health Metrics Network (HMN) in 2005 provided global leadership as well as a consensus-based overall strategy for the development of national HIS. Countries should strive for in-teroperable sub-systems within a national framework where aggregated data from the subsystems are integrated and made available in a national data repository. Version 2 of the HMN Framework [1] provides an overview, context and tangible goals for national HIS development. In version 3, HMN plans to provide guidelines for how African countries could actually achieve these goals, particularly given the current status of their HIS, human resources and general technical infrastructure. For example, the fact that technical infrastructure is unevenly distributed between rural and urban areas poses a particular challenge when designing ICT solutions for uniform implementation in a country. Moreover, when the HMN Technical Framework advises countries to implement a central data repository receiving data electronically from sub-systems and the peripheral levels, it presupposes uniform access to a wide area network like the Internet. Furthermore, when many of the data sources are paper-based, as is the dominant tendency in Africa, new ICT solutions need to be established and interoperability created based on the available infrastructure, which ranges from a complete lack of power and connectivity through portable data systems, such as USB memory sticks all the way to mobile networks and the Internet.
In order to address this complex situation, this article argues for national HIS strategies in Africa to be based on scalable and comprehensive solutions. Scalable refers to the need for rolling out the solutions in a paced manner: 1) vertically “down” the health hierarchy, from national to region, district, facility, and finally to the patient and community levels, as well as 2) horizontally in “scope” of services and functional areas and finally 3) geographically. Comprehensive refers to the need for providing solutions that meet the needs of each service area and level of the health system; from medical records for patient management to aggregated data and indicator repositories supporting district management and national monitoring and evaluation (M&E).
The authors have been engaged in developing the HIS in Sierra Leone, and we use this case to motivate and illustrate the need for scalable strategies also applies to the comprehensiveness of the solutions. The pace of rolling out solutions along the vertical and horizontal axes will depend on the evolving maturity of the system in terms of human resources, institutional learning and infrastructure, as well as funding. For example, in Sierra Leone as in most countries in Africa, the HIV/AIDS area will typically take the lead on medical records, paving the way for other patient groups to be implemented later; national and district data repositories will start with essential indicators on some, but not all relevant areas; geographical and administrative regions may develop at different paces depending on infrastructure and maturity. The key issue, however, is that the various scaling processes develop within an interoperable and integrated framework, or architecture. This paper outlines a collaboration among several groups working together to build a scalable/comprehensive HIS using an enterprise architecture.
Materials and Methods
In order to expand the HMN Framework into practical implementable guidelines, example implementations as well as consistent conceptual models are needed. [2] In this article we use the HMN project in Sierra Leone as an example for describing a conceptual model together with practical solutions that may also be used in other countries. Sierra Leone has been a “first wave” country for implementing the HMN model since 2007, including initial HIS assessment, development of strategic plan and development of national HIS as according to the HMN Framework. National data sets and reporting tools have been harmonized and the District Health Information System (DHIS) v2 data repository software application has been implemented at district and national levels since early 2008. Recently, implementation of the Open Medical Record System (OpenMRS) including interoperability between OpenMRS and DHIS v2 has been established at Connaught Hospital with aggregated data needed for reporting automatically generated from the medical records and loaded into DHIS v2.
In this article, the case of the HIS development in Sierra Leone including the interoperability between OpenMRS and DHIS v2 is used to develop a general maturity model for scalable and comprehensive solutions and strategies for national HIS development in Africa.
Open Architectures, Software and Information Systems for Africa (OASIS)
The OASIS project, funded by the International Development Research Centre (IDRC), is a collaborative research project to support ICT for development through capacity building in open source software, including OpenMRS. The project was begun in 2006 in three countries: South Africa, Zimbabwe and Mozambique, but was renewed and expanded in 2009. OASIS II has added four new collaborating partners including: the Enterprise Architecture project, the Millennium Villages Project, the OpenROSA project and Partners in Health’s Rwanda Developer Training program. OASIS II has the explicit goal of fostering health information technology collaboration among different organizations through the use of an enterprise architecture approach. OASIS II is collaborating with the DHIS and other open software developers to demonstrate the full continuity of health information from community level to facilities, and up through the administrative levels to the Ministry of Health.
DHIS
The District Health Information Software (DHIS) is a generic tool for collecting, managing and presenting aggregated data and indicators. Unlike a pre-configured database application, DHIS with its open metadata model and a flexible user interface allows the user to design the contents of a specific information system without the need for programming. The first version of DHIS was based on MS Office and has been under continuous development in South Africa since 1997. After initial piloting and deployment, first in four districts, then in two provinces, DHIS v1 was established as a national HIS standard in South Africa since 2000 [3]. Since then, DHIS v1 has been deployed in a number of countries in Africa and Asia through the so-called HISP network, which is made up by universities, HISP-NGOs, as well as Masters and PhD programs [4]. Development of the fully open source and web-based DHIS v2 (www.DHIS2.org) began in 2004 under leadership of the University of Oslo, but aimed at distributing development activities to a number of the countries in the HISP-network in order to bring software development closer to the contexts of use. A stack of Java-based technologies was selected for v2, and in parallel a distributed development platform similar to those employed by many Free and Open Source (FOSS) projects was set up. After the first pilot in Kerala in the beginning of 2006, use of v2 spread rapidly in India and is now implemented in more than 20 states. Since 2008, in addition to India, Vietnam, Tajikistan, Tanzania and Sierra Leone have been the key implementation and development sites for DHIS v2 [5]. Currently WHO is adopting DHIS v2 as their new open-HealthMapper.
OpenMRS
OpenMRS (www.openmrs.org) is a community-developed free and open source medical record application [6]. The core data model captures information concerning the clinical encounter between a patient and healthcare provider and observations recorded during the encounter. OpenMRS is a general-purpose patient-based system and observations are mapped to a concept dictionary that can be easily configured to store any real world observable linked to the encounter. A modular design includes a robust core codebase and flexible modules conferring functionality that can be added to OpenMRS as part of the customization process.
OpenMRS has emerged as a key building block in a number of HIS due, in part, to the fact that it is flexible and standards-based making it highly interoperable. In addition, the development of OpenMRS has a strong community component [7], a key feature for its sustainability and capacity development.
OpenROSA and CommCare
Due to recent technological advancements, there is great excitement for using mobile phones to address current gaps in information. Phones and PDAs have proven to be dramatically faster and more complete than traditional methods of pen and paper, and can be more accurate and less expensive.
In 2007, IDRC funding helped establish OpenROSA, a consortium of organizations working on mobile data collection and decision support. OpenROSA fosters open source, standards-based tools for mobile devices. One outcome of Open-ROSA has been the JavaROSA codebase, which is j2me code that runs on a wide-range of relatively inexpensive phones and confirms to the OpenROSA standard. JavaROSA is a flexible codebase that many different organizations are using as the core component of their mobile applications. JavaROSA is designed to support interaction with generic survey systems, electronic medical record systems (EMRs), and can maintain longitudinal records over time.
MGV-Net and the Millennium Villages Project
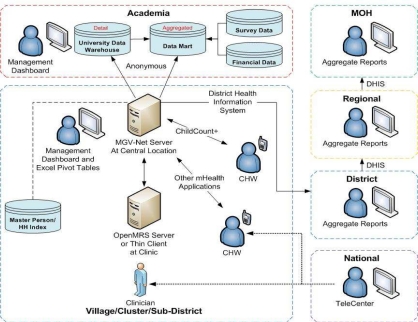
The Millennium Villages Project (MVP) operates in 10 countries and 14 agro-ecological zones and hopes to help villages achieve the Millennium Development Goals (MDGs) through the implementation of comprehensive, community-based, low-cost, integrated rural development strategies that includes primary health care. The Millennium Global Village-Network (MGV-Net) [8] is a health information and communication network designed for MVP communities that is built upon OpenMRS [6] and other information and communication technologies as shown in Figure 2. MGV-Net is designed to create centers of health knowledge based in the community, providing value to the care providers while also allowing data to be reused for Ministry of Health reporting and MVP evaluation and management across multiple countries and languages. MVP is a partner in the OASIS II project and MGV-Net will be used as a model for the Sierra Leone implementation.
Figure 2:
The Millennium Global Village-Network (based on OpenMRS) linked with the District Health Information System.
Results – The Case of Sierra Leone
As mentioned above, Sierra Leone was selected as one of Health Metrics Network’s (HMN) pilot countries for health information systems strengthening in 2007 and in early 2008, a project to use DHIS v2 as a data warehouse to integrate the various data reporting structures at district level was initiated. At that time, collection and reporting of health data was characterised by extreme fragmentation and there were no agreed upon data standards across the various health programs. Each facility had to report data on 17 separate but overlapping forms which resulted in very poor quality data.
A pilot to convince the various stakeholders to standardize and share their health information and that they would all benefit by collaborating used the following approach: 1) acknowledging the existence of the various overlapping data collection tools by providing a data entry form for each one of them in DHIS v2, while at the same time 2) harmonizing all the data elements (variables) being collected “inside” the database. In this way all stakeholders got their own data, as well as the other health data, integrated in one database. The pilot was regarded as a success, and DHIS v2 was scaled up to cover all 13 districts as well as the reporting from the districts to the national level towards the end of 2008. The result was that, for the first time, the Ministry of Health in Sierra Leone could make a comprehensive analysis of all public health data being collected within the country. With success of the pilot and scale-up, all stakeholders agreed in January 2009 to combine and integrate their plethora of data collection formats. Later the data sets have been further revised to reduce redundancy.
The availability of a comprehensive and increasingly high-quality data set from the entire country has led various donors to also start using the data from the shared repository. A training workshop for donors and other stakeholders on the use and analysis of data from the repository was conducted in February 2010, thus adding to the positive momentum.
Sierra Leone’s HIV/AIDS program, traditionally a separate and financially independent organization, was not part of the initial DHIS v2 implementation. During a January 2010 revision of the data collection tools and database, the program agreed to use DHIS for their data collection as well. Forms on voluntary testing (VCCT), prevention of mother to child transmission (PMTCT), and paediatrics were included in the new version of the DHIS v2 database. Further enhancing the integrated system included adding OpenMRS for the management of antiretroviral (ART) patients in the main hospital in the capital, Freetown, which covers 4000 out of 6000 patients nationwide. The export of aggregated ART, HIV testing, and PMTCT data from this electronic medical record system to DHIS v2 was the first implementation of the SDMX-HD standard for health data transmission, as described below.
The Use of SDMX-HD for Aggregate Data Interchange
The benefits of using open XML-based standards for interoperability between disparate systems is well understood and particularly so in the context of developing countries [9]. We decided early on that we would make use of the emerging standard, SDMX-HD, to communicate between OpenMRS and DHIS v2. SDMX-HD is an implementation of the ISO SDMX standard (ISO/TS, 2005). SDMX (Statistical Data and Meta-data Exchange) is a mature XML based standard which has found use in a number of domains for international reporting of statistical data. SDMX-HD (SDMX-HD, 2010) is an emerging effort driven by the World Health Organisation to create a health domain specific dialect of SDMX.
We developed SDMX-HD profiles to represent the ART Summary paper form as an SDMX-HD dataset which is an input into DHIS2. We successfully exported the metadata describing this form in SDMX-HD from DHIS2. The OpenMRS program running in the pilot facility was able to import this metadata and use it to produce a monthly summary report. DHIS2 is able to read in the resulting report and update its database. This is a process which would otherwise consist of staff at the facility completing a paper form which would be entered manually at the district level.
Creating a Comprehensive and Scalable HIS
Our goal is to combine the strengths of the systems outlined in the section on materials and methods and the experience of their development communities to create a scalable and comprehensive system applicable in Sierra Leone as well as in similar country contexts. Our approach assumes that infrastructure, skills, and uptake will be uneven through most countries. In Sierra Leone Internet connectivity and other infrastructures are poor. Nevertheless, the DHIS v2 is implemented nationwide and OpenMRS is implemented in the main hospital in the capital. Since the interoperability between the two systems is based on a shared and open standard, the SDMX-HD, this approach is scalable as expansion of patient records to new patient groups and areas can be “plugged in” to the backbone systems using the SDMX-HD standard. More generally in African countries, some facilities may use electronic medical records at the point of care with access to sophisticated decision support while others are still working off paper registers. One common rollout strategy is to quickly overcome all foreseen obstacles, e.g., by planning to install solar power, increase connectivity, perform additional trainings etc. In contrast, we are building a flexible system that can exist under many different configurations. For example, there may be situations where OpenMRS is implemented without any mobile data collection, or alternatively there may be patient-level data being collected on mobiles without OpenMRS. When OpenMRS is present, it will automatically aggregate data and report it to DHIS. Facilities using paper registers may use mobile devices to assist with monthly reporting or they may continue to use paper reports that will be typed into DHIS at a central facility. To achieve this flexibility in design several additional factors need to be kept in mind.
System Maturity Model
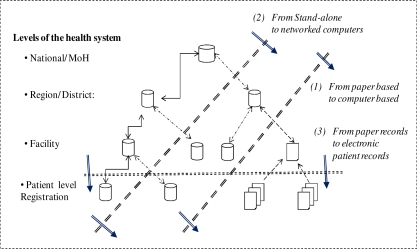
One such factor is that systems must have a maturity model. The maturity model implies that solutions need to be able to grow with time; from one to more places, from one level of the health system to the level below (from district to facility) and generally to become more granular and comprehensive. Figure 1 depicts three general processes that are ongoing at the same time, but at different paces within the same country: 1) from paper to computer, 2) from stand-alone computers to networked computers, and 3) from paper-based patient records to electronic medical record systems. The latter process of introducing medical records systems will in itself typically represent uneven development within patient groups, as we have seen in Sierra Leone, starting with HIV patients enrolled in ART programs.
Figure 1:
A Scalability-Maturity Model for eHealth Systems
The maturity model represents a practical way in which to implement the HMN framework in a country. The national data repository represents an integrated framework within which medical record systems can scale, as they are “plugged in” (transferring aggregated data) at the pace they are being implemented. Where Internet is not available the national data repository will have instances in each district, which will report to the national level using whatever means are available.
Re-Use of Information
Another factor required for successful implementation is reuse of information. One of the main efficiencies created by using electronic systems is the savings in time and money by reusing information collected for another purpose or in another context. Rolling up information from community, to facility and higher, requires clear definitions for variables and terms. Without a concept-based dictionary, it is difficult to clearly define the data fields for use by different systems. This applies to both the design of electronic systems like OpenMRS and DHIS, and the paper forms used to populate the electronic systems.
Ontologies and Rolling-up Data from Disparate Sources
In the hybrid model proposed by this paper, it is necessary to be able to combine data collected at different levels and with different technologies, and some instruments may collect more granular data than others. For example, a paper form may request the number of patients with “Diseases of the Blood and Blood-forming Organs”, while a medical record may record separate entries for “anemia”, “leukemia” and “sickle cell anemia”. If these were to be simply aggregated, the smaller, more granular entries would likely be reported as separate entries and be lost in the list. To prevent this from happening, it is necessary to have an ontology that relates the data elements with one another. For example, the OASIS II project is mapping all of its concepts to reference terminologies such as SNOMED®CT. SNOMED is an ontology with hierarchical IS-A relationships that allows us to automatically subsume more granular concepts within higher-order concepts [10]. For example, “anemia” IS-A “red blood cell disorder” which IS-A “finding of cellular component of blood (Blood disease). MVP, through Columbia University, has a SNOMED name-space identifier and will be adding to and clarifying these ontologies to facilitate data aggregation.
MGV-Net as a Model
In Figure 2, identified person-level data is captured from each clinical encounter in an OpenMRS database. All persons from the village, cluster or sub-district are captured in the OpenMRS database and given a unique identifier. Additional information is collected by community health workers (CHWs) using CommCare or ChildCount+ (RapidSMS) on their mobile phones. Alerts and other data from the medical record can be sent to the CHWs using SMS. The OpenMRS database then provides aggregated data via a link to DHIS v2, which then is aggregated as it moves up the hierarchy from district, to province, to Ministry. In addition to this aggregated reporting, specific MVP indicators are aggregated at Columbia University where they are combined with data from surveys and financial reports. Another planned secondary use of data is an anonymized person-level data warehouse for research purposes. Finally, in some MVP sites, plans are underway to introduce teleconsultation and telemedicine services to assist providers and CHWs in their care.
Conclusions and Next Steps
The OASIS and DHIS collaboration is working with the Ministry of Health in Sierra Leone, HMN and other stakeholders to implement an integrated eHealth information system using the architecture and principles described in this paper. The first two years of work in Sierra Leone have revealed that there is a desperate need for developing human capacity and local support structures as part of the process. In order to address this challenge in a sustainable way and to establish an institutional base for capacity building and international collaboration at the educational and academic level, the local Njala University is part of the collaborative setup.
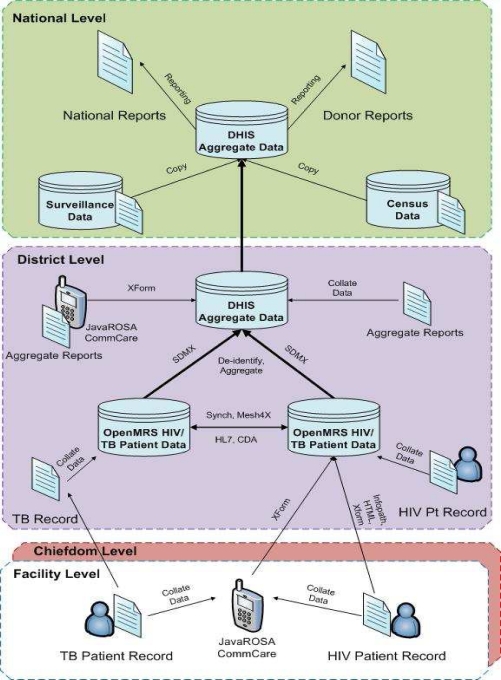
The full planned implementation is shown in Error! Reference source not found.. Health information is captured at multiple levels of the system, either by paper entered into a computer or via mobile phones. Data can be entered directly into phones or computers in either patient-level or aggregated form. OpenMRS represents the core patient-level repository and DHIS v2 handles the aggregated data and the roll-up through the hierarchy.
We have presented an approach that emphasizes flexibility, architecture, and collaboration. Several existing networks, each with a deep experience in one area of expertise have committed to integrating scalable and comprehensive information systems into Sierra Leone’s health system. Our next steps are to build off of the existing deployment of OpenMRS and DHIS v2, deploying OpenMRS and mobile solutions where appropriate, and helping to build capacity where necessary. In many places we will start with a simple system and gradually introduce and spread more of these tools over time. However, since our system is designed for an uneven spread of technology we will be able to take advantage of whatever data we collect, rather than waiting for a single technology to be in use everywhere before providing actionable data.
Figure 3:
Proposed OASIS-DHIS eHealth enterprise architecture for Sierra Leone.
References
- [1].Health Metrics Network . Framework and Standards for Country Health Information Systems. Second Edition. World Health Organization; Jan, 2008. [Google Scholar]
- [2].Stansfield S, Orobaton N, Lubinski D, Uggowitzer S, Mwanyika H. The Case for a National Health Information System Architecture; a Missing Link to Guiding National Development and Implementation. Making the eHealth Connection; Bellagio: 2008. [Google Scholar]
- [3].Braa J, Hedberg C. The struggle for developing District health information systems in South Africa. Information Society. 2002;2002;18(3) [Google Scholar]
- [4].Braa J, Monteiro E, Sahay S. Networks of action: sustainable health information systems across developing countries. MIS Quarterly. 2004;28(3):337–362. [Google Scholar]
- [5].Titlestad OH, Staring K, Braa J. Distributing Development to Enable User Participation: Multilevel Design in the HISP Network. Scandinavian Journal of Information Systems. 2009;21(1):27–50. [Google Scholar]
- [6].Mamlin B, et al. Cooking Up An Open Source EMR For Developing Countries: OpenMRS – A Recipe For Successful Collaboration. AMIA Annu Symp Proc. 2006 [PMC free article] [PubMed] [Google Scholar]
- [7].Seebregts CJ, Mamlin BW, Biondich PG, Fraser HSF, Wolfe BA, et al. The OpenMRS Implementers Network. Int J Med Info. 2009;78:711–720. doi: 10.1016/j.ijmedinf.2008.09.005. [DOI] [PubMed] [Google Scholar]
- [8].Kanter AS, Negin J, Olayo B, Bukachi F, Johnson E, Sachs SE. Millennium Global Village-Net: Bringing together Millennium Villages throughout sub-Saharan Africa. Int J Med Inform. 2009 Sep 17; doi: 10.1016/j.ijmedinf.2009.08.002. [DOI] [PubMed] [Google Scholar]
- [9].deNardis L. A Development Agenda for Open Standards; Technology, Globalization, and Development Conference; St. Louis, MO. April 5, 2007. [Google Scholar]
- [10].Lieberman MI, Ricciardi TN, Masarie FE, Spackman KA. The use of SNOMED CT simplifies querying of a clinical data warehouse. AMIA Annu Symp Proc. 2003;910 [PMC free article] [PubMed] [Google Scholar]