Abstract
Common ground refers to the knowledge shared by two communicating parties to enable communication to occur. We suggest that common ground could enhance collaborative care delivery by serving as the linkage between different healthcare team members. Despite research describing the importance of common ground to facilitate communication, little is known about how common ground forms, moments where it is necessary, and barriers to achieving it. To address this shortcoming we studied collaborative care delivery in two settings and then used Grounded Theory methodology to develop a model of common ground. The model contains four main concepts: moments of common ground, barriers to common ground, fabric of common ground, and consequences of weak common ground. Our findings show that common ground is multi-dimensional with both static and dynamic aspects. The results from this paper help us to better understand collaborative care delivery and how to design information and communication technologies to support it.
Keywords: common ground, collaboration, communication, healthcare teams
Introduction
Healthcare delivery is increasingly being provided via collaborative teams. However collaborative care delivery is difficult to implement owing to the different healthcare providers and work processes involved in collaboration. Collaborative care delivery encompasses the need for healthcare providers to understand their roles, responsibilities and competencies in relation to other professions, to manage uncertainty and ambiguity, and to work with other providers to assess, plan and provide care [1]. Ineffective coordination or communication across collaborative teams can result in inefficient use of healthcare resources, interruptions and other communication disruptions, and also cause serious adverse events and medical errors [2].
Common ground first emerged from the communication literature and refers to the shared knowledge, language and beliefs necessary for communication to occur [3]. Coiera first described the role of common ground in healthcare communication through an innovative perspective: when conversation is better than computation as a communication media. Coiera proposed different perspectives regarding the extent to which we can replace communication tasks with information seeking tasks [4]. A key message was that, in moments of low grounding, conversation is the preferred means of establishing common ground as people turn to each other for information.
Collaborative care delivery is very dependent on common ground as effective collaboration requires common ground between healthcare providers and across work processes. However forming common ground for complex team activities is different from forming common ground for conversation. Teamwork involves more than simply the exchange of information but rather it includes the coordination of actions and generation of solutions, all of which require common ground [5]. Although the proposal to use conversation to develop common ground is sound, it is not always practical. Collaborative care delivery is frequently provided asynchronously where the different healthcare providers have minimal face-to-face interaction. Consequently, person-to-person grounding is not always feasible and computer aided grounding becomes more important.
As important as common ground is for facilitating communication and collaboration, there is still much we do not know about it. We do not know when and how common ground is formed or the barriers and facilitators to its formation. Also, while person-to-person communication is sometimes available, research needs to investigate the role common ground plays to enable computer supported common ground in moments of asynchronous care delivery. Prjenstad et al. state that information and communication technologies (ICTs) can improve communication in collaborative healthcare settings but they caution that in complex healthcare delivery successful communication requires both interoperable systems and interoperable people [6]. Standards and semantic frameworks have improved system interoperability at the data level but interoperable people at the process level are still an issue. Common ground is the basis for interoperable people and by studying collaborative care delivery we can increase our understanding of common ground including 1) the role it plays in collaboration, 2) moments when it is needed, and 3) how it develops. This paper extends existing work by providing a model of the moments, barriers, and fabric of common ground, as well as the consequences of weak common ground. We suggest our model provides an improved understanding of the activities within the clinical communication space to enable us to design ICTs to support computer aided grounding for instances when face to face grounding is not possible.
Materials and Methods
Data Sources
We studied collaborative care delivery in two healthcare sites. Both sites were chosen because they provided care based on a collaborative care model that required the interaction of multiple healthcare providers. Site A was a nine bed inpatient hospice where we collected 90 hours of non-participant observations and 30 interviews with nurses, physicians, residents, volunteers, and personal support workers. In Site B, a 200 bed rural hospital, we collected data in five clinical units that featured team based care: complex continuing care, medical-surgery (acute care), day surgery, diabetic education and maternity. In site B, 114 hours of non-participant observations were conducted and 13 semi-structured interviews were held with physicians, nurses, ward clerks, physiotherapists, physiotherapy assistant, clinical managers and students from different disciplines. In both sites, observations were conducted at different times in the day in order to observe different collaboration processes such as morning rounds, shift change, and patient admission. Ethics approval was obtained prior to commencing the study.
Methods
Non-participant observation was used to collect data on the clinical wards. Semi-structured interviews were used to collect supplementary reflective and clarification data. Two trained qualitative researchers collected the data simultaneously at both sites. The data was analyzed using Grounded Theory (GT), which is a general methodology for developing theory that is grounded in data that has been systematically gathered and analyzed [7]. GT is suitable for developing introductory theory about a concept. The analysis was done by the two authors and two research assistants. The hallmark of GT is three coding cycles: open, axial and selective coding [7]. Our goal was to develop theory about common ground such as when and how it is formed, barriers to formation, and the role informatics plays in facilitating common ground. We did not code with any preconceived frameworks other than the common ground concept. Data was coded during open coding into concepts and categories. Common ground concepts and sub-concepts were identified and interconnected during our axial coding. The common ground concepts were refined and final concepts identified in selective coding.
Results
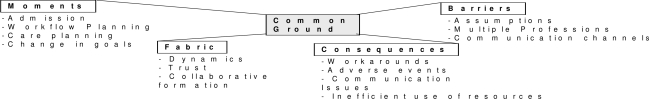
From our analysis we established a model of common ground (fig. 1) that has four concepts: moments of common ground, barriers to common ground, fabric of common ground and consequences of weak common ground. Each concept has a number of sub-concepts. By enumerating and studying these concepts and sub-concepts, we can better understand how to support collaborative care. Each concept and its sub-concepts are described below.
Figure 1.
Model of Common Ground (four main concepts are in boxes)
Moments of Common Ground
There are moments during care delivery where it is essential that common ground be established. In our observations, we noted that collaborative activities including discharge, care and workflow planning, clinical rounds, and patient goal setting were examples of such moments. We will now examine the importance of common ground in relation to moments of admission and workflow planning.
In interviews participants described that when a patient is admitted it is essential that a plan of care be agreed upon by all healthcare providers. This plan should detail the patient’s needs and how those needs are to be met within the care setting. Shared knowledge of this plan ensures that care goals are commonly known objectives. However we observed multiple instances when this shared knowledge, or common ground, was missing. To illustrate, during an interview a physician at Site A reflected about a patient who was admitted to the hospice with very complex care needs -- needs that exceeded what the unit could efficiently address. As a result the physician felt that the care the patient received was not ideal. If all the healthcare providers had had a common understanding of 1) the patient’s needs and 2) the team’s capacity to meet these needs, the site’s inability to address the patient’s needs may have been uncovered. In other words, if patient admission had required common ground involving all team members, this patient would probably not have been admitted. A second example was described where a patient was denied admission to Site A because he was undergoing a number of acute interventions, which violated the admission criteria of the hospice. The patient’s primary care physician was outraged that the patient was denied admission. Upon further inquiry, we learned that the patient was receiving the acute interventions in order to sustain his life for one more week so that he could attend his daughter’s wedding. That critical information was not available at the time of admission but it could have influenced the admission committee’s decision. As one of the hospice administrators commented, common ground is important in moments like these since ‘you don’t know what you don’t know’.
Moments of common ground are also essential for workflow planning at both the unit and organizational levels. For example, in Site A, a physician ordered a medication for a patient that was a high maintenance with multiple doses. Unbeknownst to this physician, the unit was already experiencing a heavy workload. The nursing staff were upset that their workload was further increased because of this new medication, especially since less workload heavy options were available. This physician’s medication decision was made without common ground about the unit level workflow. A second example occurred in Site B’s chronic care unit. The site’s emergency ward had a number of patients waiting for beds in the chronic care unit. Senior management at the hospital ordered two more beds opened on the chronic care unit without verifying the-current status of that unit. The unit was already struggling--with a heavy workload and was having difficulty scheduling nurses to meet the current workload. The nursing manager and staff on the unit were upset that the new beds were opened without checking with them. Again, a moment of common ground, this time at the organizational level, was missing.
Barriers to Common Ground
Barriers prevent the formation of common ground. The most significant barrier we observed was professional socialization differences that were reflected in conflicting communication practices and expectations. To illustrate, one site B physician described an incident where he was waiting to discharge a patient pending the patient regaining sufficient physical mobility. This physician generally conducted his rounds early in the morning and so did not usually meet the other care team members. The patient chart was how the physician communicated with other care providers. After several days of treatment the patient had made significant progress and nursing staff contacted the physician to ask why the patient had not yet been discharged. The physician explained he did not think the patient had sufficient mobility for safe discharge. The nurses informed the physician that the patient had acquired sufficient mobility a few days ago. We learned that the physiotherapist was charting using profession-specific terms that were not known to the physician. The physiotherapist and physician’s clinical vocabularies were not interoperable with each other. As the physician explained: ‘OT, Dietary. I need to know different information than they’re giving me, and again I think it’s more an issue of practicality. From a physiotherapist, I need to know are they [patients] ready to go home? Can they walk up the stairs? Can they get to the bathroom..those sort of basic things. I’m no physiotherapist so I don’t really need to know if they have 27 degrees of range of motion or 54 as long as they can walk’. As that example illustrates, each healthcare profession has unique socialization patterns which informs professional practices such as charting practices. These profession-specific practices can become barriers to common ground.
Assumptions are another barrier to the formation of common ground. We may believe we have common ground based on an assumption but that can in fact be very wrong. The management of palliative care patients is difficult and general practitioners (GPs) sometimes prefer to leave the difficult decisions about treatment or transfers to the site A staff. The medical advisor at site A said that was done in the GPs best interest to protect them from having to make those difficult decisions. The assumption was that most GPs were not comfortable making such decisions as GPs generally have limited palliative care knowledge. However while some GPs appreciated having decision making done for them some believed it was impacting the long standing relationship between the GP and patient. Assumptions led some GPs to be frustrated that decisions were made without their knowledge. It was not that the GPs believed the decisions were necessarily wrong; they just wanted to know about them before the fact so they could be involved in the decision.
The different communication channels used in collaborative care delivery can also be barriers to common ground. Both site A and B used numerous communication channels including paper, electronic, and oral. Oral communication was a very common channel, particularly among nursing staff. However, reliance on oral communication is problematic because, while patient case information may be discussed orally, that information may not be recorded in the chart. In asynchronous care delivery, the patient chart is the communication tool that links the team. The chart is a vital communication tool that must provide common ground for all healthcare providers. However charts do not always contain the requisite detail to act as the team’s communication link. Although patient data has to be recorded in the chart for legal reasons, the data included therein is often only a summary of what is discussed on the unit. As the nursing director at Site A explained, in the transformation from oral to written communication, some details are lost: ‘It [patient information detail] may all be there, in their head, but it’s a challenge to actually communicate it to enough people given that there are different team members coming in and interacting at different times of the day. The person who makes the observations may not be around to have their input heard, so they have to somehow make sure that their input gets heard in a way that people will see it’. Further it was common for multiple paper and electronic documents to exist on a patient and a challenge was how to reconcile all the documents to provide the complete picture about a patient. In asynchronous team settings the plethora of communication channels that support effective team collaboration can be barriers to the formation of common ground.
Fabric of Common Ground
The fabric of common ground refers to interconnected aspects that form common ground. A key insight from our data was that common ground is a dynamic process that forms over time with trust being the single biggest factor in its ongoing formation. Most notably, physicians and nurses regularly described how the establishment of trust must take place when a provider is unfamiliar with the staff. A physician described how part of--forming common ground is developing trust of what people can do, and also understanding what they cannot do. This physician stated ‘I know what [nurse’s name] personality is like so I know that I can rely on her to do x, y, and z but not necessarily a, b, and c, and that’s not necessarily a bad thing. It’s just that’s their skill set, that’s their personality, that’s their whatever, and that does make a big, big difference.’
As trust develops, and different healthcare providers have common ground about what people can and cannot do they are more likely to defer decisions or tasks to other providers. For instance, in Site A, a patient’s palliative status can change rapidly. We observed that physicians who trusted the nurses they were working with would give the nurses a lot of independence with respect to dosing and provision of medications since they trusted the nurses to make the necessary assessments for safe treatment provision. However, if trust was not established, we observed that a nurse would have to phone the physician to give a patient update and to develop a treatment option. Once that trust and common ground were established, these conversations were much less frequent.
Our data also revealed that the pace of formation of common ground fabric was different for intra-disciplinary teams than for inter-disciplinary teams. Although trust was essential between all healthcare providers, interviewees suggested that intra-disciplinary common ground (i.e. nurse-nurse) formed faster than inter-disciplinary common ground (i.e. nurse-physician).
Aside from trust, the fabric of common ground is also woven together by the push-and-pull dynamics of collaboration. Collaboration is not just putting multiple providers together but rather it requires them to exchange information, sometimes by actively requesting or pulling information from others, and at other times sharing or pushing information towards others. For example, when a patient was admitted to Site A, the patient’s GP was generally considered to be the best source of information about the patient since this provider usually had a long term relationship with the patient. GPs possessed relevant clinical knowledge and contextual knowledge that was not always included in the patient’s chart. Despite this general consensus, some GPs explained that Site A admissions staff did not consistently or comprehensively pull information from them. As a result, some GPs described feeling underappreciated. As one physician explained: ‘it’s how all the team members feel about being heard, about having their wishes addressed, or their expertise listened, you know, noted, their input valued’. That example illustrates the importance of the collaborative push-and-pull needed to weave the fabric of common ground. While the GPs need to push, common ground is only developed when the information receiver also pulls. Different healthcare providers must respect each other’s knowledge so the fabric of common ground can be formed through a meaningful exchange.
Consequences of Weak Common Ground
Weak common ground can have a range of consequences including inefficient use of resources, adverse events, workarounds, and communication disruptions between healthcare providers. Inefficient use of resources was a common consequence of weak common ground between healthcare providers. This paper has already provided two examples of the inefficiencies that result from weak common ground. First was the example of the patient whose discharge was delayed because the physician and physiotherapist did not have common ground with respect to clinical vocabulary. Second was the example of the patient who was admitted to Site A with care needs that exceeded the site’s resources. When weak common ground exists between team members, such inefficiencies often result.
Weak common ground can also lead to adverse events. During observations at Site B, a patient’s medical status became terminal and the patients’ care plan changed to include a do not resuscitate (DNR) order at the request of the patient. However this change in care plan was not effectively communicated to all healthcare providers and, after coding, the patient was resuscitated. Both the patient and his family experienced significant distress because their orders had not been followed. It is essential that all healthcare providers have common ground about a patient’s status and care plan, particularly when there are significant changes in care goals, to prevent adverse events from occurring due to missing common ground.
Workarounds were another unintended consequence of weak common ground. At Site A, physicians often commented that the chart did not provide sufficient historic details about the patient’s care before being admitted to the hospice. Patients at Site A were often transferred there from a local hospital and Site A physicians knew that the patient’s hospital record (not accessible at Site A) would have more data. One Site A medical resident worked around this problem by going to the hospital, where he had privileges, to read the patient’s hospital chart and take notes back to Site A. Although that workaround gave the resident the data he needed, the workaround was an example of second order problem solving since it did not permanently resolve the problem. Physicians at Site A continue to encounter this problem. But not all workarounds were problematic. We also observed workarounds that were examples of first order problem solving. One example was generated by the physician who was unable to understand the physiotherapist’s assessment of his patient. By creating a note in the chart that specifically asked ‘Is [patient name] mobile enough to go home?’, the physician directly addressed the problem and created common ground between him and the physiotherapist.
Other unintended consequences of weak common ground were communication issues such as interruptions. During clinical observations we observed if healthcare providers did not have common ground about, for example, a patient’s care objectives, they commonly interrupted another healthcare provider to develop common ground. While interruptions often led to the formation of common ground, they also generated an interruption heavy work environment, particularly for the nursing staff. It was not uncommon that a nurse would be doing a task such as counting a prescription or charting data and be interrupted and have to return to the task later. Sometimes there were multiple interruptions before the initial task was completed.
Discussion
Common ground is an important part of collaborative care delivery since it ensures that different healthcare providers are interoperable with one another. Building off a statement from one of our participant’s statements, we propose that common ground is important because: While ‘you don’t know what you don’t know’, what you don’t know makes a difference. Weak or missing common ground can have a range of consequences – from wasted healthcare resources (e.g. beds, provider time) to workarounds and adverse events and medical errors.
Coiera stated that before we can design ICTs to support the clinical communications space we need to characterize it [4]. This study has generated a model of four concepts of common ground and helps characterize the clinical communication space by describing how common ground is the basis for human interoperability. For example common ground is not always randomly required; instead, there are specific moments when it is needed such as during admission or changing a patient’s care plan. This study has also highlighted the importance of examining common ground in the context of the constraints and fabric involved in its formation. Team members’ mutual trust, the generation of workarounds, and the number of communication channels used all impact on common ground. Further, we cannot assume common ground exists but rather a collaborative effort must be made to build its fabric across different agents. Many common ground misunderstandings in our study occurred because a decision was made without asking whether the task could be actually be done (capability), asking whether there is sufficient resources to do the task (workflow), or asking who else needs to know about and contribute to the task (collaboration)? Asking those three questions provides a starting point to forming common ground.
Our common ground model provides insight for the design and evaluation of ICTs to support computer aided grounding when in person grounding is not an option. Alerts and reminders could be built into charting and order entry systems to ensure all providers have common ground at key moments (e.g. admission, care planning, order entry) and also to ensure that information is appropriately ‘pushed’ to and ‘pulled’ from all requisite parties. Asynchronous care delivery is a key barrier to achieving common ground but technologies such as Web 2.0 provide the means for collaborative decision making to take place asynchronously at the key common ground moments. The barriers to common ground provide specific obstacles to overcome in ICT design and evaluation. For example, as electronic health record systems are designed we need to ensure that the clinical vocabulary used in these systems are designed and evaluated by all providers given they will have different professional vocabularies. We also need to reconcile the different communication channels (i.e. oral, paper, electronic) that are used. Informal and oral communication was frequently used to support common ground. We need to consider those informal communication channels when we design standardized ICTs. There is little benefit in designing interoperable information systems if the people using them are not interoperable. We also need to consider the fabric of common ground in ICT design. Providers may have varying roles and responsibilities depending on the degree of social fabric. ICTs therefore need to be designed with flexible functionality to support dynamic team settings and the clinical tasks within those settings. Weak common ground was also a key source of interruptions. Many of the interruptions we observed were about care planning for a patient or staff issues like workflow planning. Incorporation and communication of the common ground concepts from this study may help reduce the occurrence of interruptions by ensuring that common ground is pro-actively achieved when it is needed (i.e. care planning).
Developing common ground amongst healthcare team members requires the expense of time, but we argue that the consequences of weak common includes patient safety, workflow, social, and financial issues, which makes grounding a cost worth incurring. Limitations to this paper are it was an exploratory study and we only studied collaborative care delivery in two settings. Given the influence that context has on common ground, it is likely that additional concepts and sub-concepts could be seen in other settings. The results from this paper also provide the basis for further work on common ground and how it can inform ICT design to support collaboration. Unanswered questions include: 1) to what extent does common ground form more quickly intra-disciplinarily as opposed to inter-disciplinarily, and 2) how can we assess if teams share sufficient common ground?
Common ground will become increasingly important as more healthcare delivery is provided via asynchronous collaborative teams. The model from this research provides a starting point for understanding the clinical communication space and how we can design ICTs to support collaboration.
References
- [1].Freeth D, Reeves S. Learning to work together: using the presage, process, product (3P) model to highlight decisions and possibilities. Journal of Interprofessional Care. 18(1):2004, 43–55. doi: 10.1080/13561820310001608221. [DOI] [PubMed] [Google Scholar]
- [2].Alvarez G, Coiera E. Interdisciplinary communication: an uncharted source of medical error? Journal of Critical Care. 2006;21:236–242. doi: 10.1016/j.jcrc.2006.02.004. [DOI] [PubMed] [Google Scholar]
- [3].Clarke H, Brennan S. Grounding in communication. In: Resnick LB, Levine J, Behreno SD, editors. Perspectives on Socially Shared Cognition. Washington, DC: American Psychological Association; 1991. [Google Scholar]
- [4].Coiera E. When conversation is better than computation. J Am Med Inform Assoc. 2000;7(3):277–86. doi: 10.1136/jamia.2000.0070277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Convertino G, Mentis HM, Rosson HB, et al. pp. 2339–2348. Supporting Content and Process Common Ground in Computer-Supported Teamwork. CHI 2009.
- [6].Pirnejad H, Niazkhani Z, Berg M, Bal R. Intra-organizational Communication in Healthcare. Methods Inf Med. 2008:47. [PubMed] [Google Scholar]
- [7].Strauss A, Corbin J. Basics of qualitative research: grounded theory procedures and techniques. Newbury Park, CA: Sage Publications; 1990. [Google Scholar]