Abstract
As a way to promote consistency and completeness of pressure ulcer risk assessment, as well as to establish a framework for data and knowledge sharing in this domain, we constructed an ontology that represents how the characteristics of the high risk patients defined by the Braden scale are operationalized at two different settings. We observed great similarity between the two study hospitals. Forty scenarios that portrayed patients at each site were added to the ontology and algorithmically assessed for pressure ulcer risk using the ontology reasoner FACT++. When validated by manual assessment by the nurses from each site, high consistency in the assessed risk level was observed with the average consistency score of 0.82 (SD= 0.06) out of 1.0. The results suggest that explicitly defining the site specific methods for assessing pressure ulcer risk that comply with the standard methods defined in the Braden scale can improve assessment consistency.
Introduction
Pressure ulcer is a serious patient safety concern that causes significant discomfort to patients and high treatment cost to payers [1]. Identifying the patients at risk of developing a pressure ulcer is a crucial first step of prevention. However, assessing the risk for developing a pressure ulcer is a complex task that requires interpretation of various aspects of patient status. The Braden scale1, a widely adopted pressure ulcer risk assessment scale [2–3], determines the risk based on 6 risk factors. This scale provides detailed explanations on how to identify patients who have these risk factors, at various severity levels. Nonetheless, applying the described methods directly to assessment practice is not always straightforward and often requires additional steps of translation across specific practice settings.
The purpose of this study was to explore a consistent and systematic way to apply the standard methods of risk assessment defined in the Braden scale to different practice settings to promote consistency and accuracy of the risk assessment, which will facilitate data sharing across different healthcare settings. Specifically, we aimed to (1) identify site-specific methods of pressure ulcer risk assessment in terms of discrete patient data and data synthesis used for the assessment, (2) compare the methods from 2 different settings for similarities and differences, (3) construct a pressure ulcer risk assessment ontology that integrates site-specific methods into a common standard method, and finally to (4) demonstrate the consistent and systematic application of the assessment methods using patient scenarios.
Background and Significance
Challenges in assessing pressure ulcer risk with the Braden scale
Validity and inter-rater reliability are the key requirements of risk assessment scales. Validity of the Braden scale has been proved in many studies, but its reliability has been less often evaluated. A few studies raised concerns about the inter-rater reliability of this scale, especially at the individual parameter level [4–7]. The Braden scale’s six parameters represent six risk factors related to pressure ulcer formation (Sensory Perception, Activity Status, Mobility Status, Moisture Exposure, Nutritional Status, and Friction & Shear). Not all parameters are defined in a way that can be readily applicable to assessment practice due to the complex and sometimes chronic nature of the related risk factors [8].
Studies showed that understanding various aspects of patient status and correctly applying the patient characteristics defined in each parameter to assessment practice are the keys to accurate and reliable risk assessment with the Braden scale [4–5, 9–10]. The findings from these studies indicate that explicitly defining the patient data and the synthesis methods required to identify risk factors improves accuracy and inter-rater reliability of the assessment.
In a previous study we have developed a prototype decision support tool that would assemble patient data relevant to pressure ulcer risk assessment from an Electronic Medical Record (EMR) system. In that pilot study, we identified the ways in which the parameter definitions of the Braden scale were operationalized at a single study site. We converted the operational definitions directly into decision rules. The generalizability of this tool was limited, as it failed to explicitly represent the translation between the site-specific risk assessment methods and the standard methods defined in the Braden scale.
Using an ontology to represent and integrate various methods of pressure ulcer risk assessment
Studies have utilized ontologies to systematically map patient- or site-specific data into a common knowledge framework. Systematic abstraction of patient-specific data to high level standardized disease phenotypes was demonstrated in autism cases using an ontology and an added rule-based inference function [11]. Similarly, site-specific neurologic data were integrated into a standard cerebrovascular disease ontology using the description logic based inference engine embedded in that ontology [12]. Problem Solving Methods (PSM), a plug-in module of earlier version of Protégé, is another example of employing an ontology modeling approach to the representation of sharable knowledge on inference methods [13].
The underlying idea in these studies is to model the common domain knowledge or concepts as high level entities and specific applications of the knowledge or concepts as specializations of the high level entities. This is a viable approach to representing site-specific methods for pressure ulcer risk assessment in relation to the standard assessment methods defined by the Braden scale.
Methods
This study was done in collaboration with 2 tertiary academic medical centers. One is a rehabilitation hospital where a commercial EMR system has been used for several years and the other is an acute care hospital that mostly uses paper-based records, except in intensive care units, where an in-house built EMR system is used. Both sites assess pressure ulcer risk using the Braden scale.
Identifying site-specific data and data synthesis methods for pressure ulcer risk assessment
We had extracted 38 detailed patient characteristics (e.g., “patient has no problem with communication”, “patient sometimes has a communication problem”) that are grouped into 15 patient characteristics categories (e.g., “ability to communicate”) from the Braden scale parameter definitions. The 38 patient characteristic descriptions were presented to a nurse from each study site, who was experienced in assessing pressure ulcer risk using the Braden scale. These nurses identified the specific data items that they use to evaluate patients against the 38 characteristics. When multiple data items were related to a single patient characteristic in the Braden scale, the nurses also explained how those discrete data items were synthesized for the evaluation.
We presented the data items collected at one site to a nurse at the other site to identify those that were potentially misleading due to the unfamiliar local expressions. These items were clarified either by being replaced with a standardized term matched in the Systematized Nomenclature of Medicine, Clinical Terms (SNOMED-CT) or by providing definitions.
Discovering the commonalities in assessing the risk
We converted the parameter definitions of the Braden scale to IF-THEN statements, i.e., high level data abstraction rules. We produced their site-specific versions by replacing the general patient characteristic descriptions with the corresponding site-specific data items. We then examined the site-specific data abstraction rules of the two sites to find the commonalities that could be promoted to a high level common rule. For example, the ability to effectively communicate pressure-related discomfort or pain is described as one of the patient characteristics that are important on evaluating the risk factor related to the Sensory Perception function. Both sites assessed communication capability by synthesizing orientation status, emotional status and limitations in verbalization. These three items can potential be promoted to a common rule in the category of “ability to communicate”.
Building a pressure ulcer risk assessment ontology
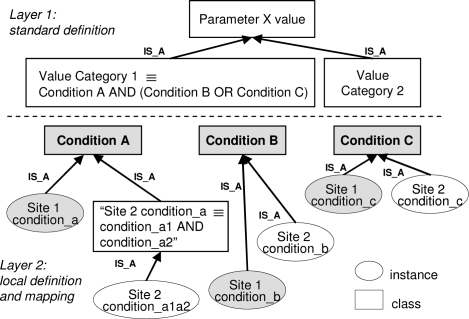
We constructed a 2-layer ontology using Protégé-OWL 2 to map the pressure ulcer risk assessment methods defined at the two study sites to the standard assessment methods defined in the Braden scale. In Figure 1, Layer 2 represents the former and Layer 1 represents the latter.
Figure 1.
A schematic view of the 2-layer ontology
Relating the site specific data to the general patient characteristics defined by the Braden scale was straightforward in many cases: one site-specific data item represented one general description (Condition B and Condition C of Figure 1). When a general description was mapped to a synthesis of multiple site specific data items that could not be promoted to the common rule, we created a subclass of the related general description and annotated the class with the site-specific data synthesis rule as in Condition A of Figure 1. We then created a synthesized version of the site-specific data as an instance of this subclass.
Table 1 depicts the way that the Braden scale is modeled in the ontology. One of the Sensory Perception parameter values no impairment was presented as an example.
Table 1.
Defining the Sensory Perception parameter and the value no impairment
| Sensory Perception: No Impairment– the patient responds to voice AND has no sensory loss AND has no communication problem |
| Sensory Perception_No Impairment ≡ ∃ has Response Level. Respond To Voice ∧ ∃ has Sensory Loss. No Sensory Loss ∧ ∃ has Communication Status. Communication Intact |
| “Communication Intact”is further specified as below |
| Communication Intact ≡ ∃ Orientation. Intact ∧ ∃ Emotion. Calm ∧ ∃ Verbalization. Intact |
| Specific patient status valuesindicating the conditions specified above are as below |
| Respond To Voice. x ∈ {alert, respond To Voice, obey Commands, open Eyes To Pain} No Sensory Loss. x ∈ {no Sensory Loss Finding, sensory Intact On Dermatome Assess} Calm. x ∈ {behavior Calm, RASS_alert Calm} Orientation Intact. x ∈ {oriented x3, oriented Verbal Response} Verbalization Intact. x ∈ {no Aphasia, verbal Response Present} |
Testing the effects of the explicitly defined assessment methods on assessment consistency
We created two sets of 20 patient scenarios reflecting various levels of pressure ulcer risk. The set of scenarios was created using data identified from one site. These 40 scenarios were added to the ontology as 40 classes defined with the site-specific data instantiated in the second layer. We then classified the 40 scenarios under the parameter value classes in layer 1 using FACT++, a description logic reasoner provided with Protégé-OWL [14].
The two nurses who identified the site-specific assessment methods reviewed the 20 scenarios in paper forms and scored the Braden scale. We offered an option of “need more data,” so that nurses could select it when they felt the presented data were not enough to make the risk assessment with the Braden scale. This was done to test the completeness and the relevancy of the site specific assessment methods identified at the 38 patient characteristics levels by placing them back into the entirety of pressure ulcer risk assessment context. Another nurse from each site also assessed the 20 scenarios following the assessment methods defined by the expert nurses from the same site.
We compared the parameter values determined by the ontology and by the nurses, and assigned consistency scores. We didn’t calculate Kappa statistics because there were unused value categories in certain parameters. When the same values are assigned to a presented scenario by two different assigners at a given site, we gave a score of 2. When the values differed by 1 point (e.g., very limited vs. completely limited), a score of 1 was given. When the values differed by more than 1 point, a score of 0 was given. We then generated summary consistency scores for each parameter separately by sites, for easy interpretation. We divided the total scores that each parameter had earned with the 20 scenarios by the maximum possible score of 40. That is, if two different assigners assigned the same value on the parameter for every scenario, the summary score becomes 1. If they assigned values differed by 1 point to all, the summary score becomes 0.5, if differed by more than 1 point, the summary score becomes 0.
Results
Data items used at the two sites
We identified 19 data items from site 1, which are assembled into 62 patient status descriptions corresponding to the 15 patient characteristic categories of the Braden scale. From site 2, 14 data items that are assembled into 58 patient descriptions were identified. Eighteen of the 19 data items identified from site 1 were the regularly documented structure data items. On the other hand, half of the data items identified from site 2 were documented in nursing narrative notes.
The cross review of data items showed that the site-specific expressions of patient data are not a huge obstacle to sharing assessment methods, but the ordinal descriptors of the data, defined for the site specific usage are. Seven items from site 1 and 1 item from site 2 were deemed unclear to the other site’s nurse. Two of them required definitions (e.g., close guard) and five of them required better quantifiable descriptors (e.g., maximum assistance vs. total assistance). These items were clarified by adding textual definitions or numeric qualifiers. “Bowels: continent/incontinent” was the only item that required an alternative name. Although its meaning was conveyed, it required a more suitable expression. This item was replaced with “Bowel: occasional accident”, a term mapped from SNOMED-CT.
We observed that the two sites used almost identical data items in evaluating 8 of the 15 patient characteristic categories (Table 2). We also observed many discrepancies in the data items used to evaluate the other patient characteristic categories, which include “response level”, “sensory loss”, “activity level”, “protein intake amount”, “transfer mobility”, “non-oral nutritional intake amount”, and “fluid intake status”.
Table 2.
Data items commonly used by the sites
| Patient characteristics | Data items used |
|---|---|
| Communication status | Orientation, emotion, Verbalization ability |
| Walking amount | Activity observation |
| Ability of change body position independently | Limb strength, position change schedule |
| Maintaining body position | Position change schedule |
| Skin moisture pattern | Skin observation, urinary or bowel pattern |
| Nutritional intake mode | Diet order |
| Oral intake amount | Intake & output assess |
| NPO duration | Diet order |
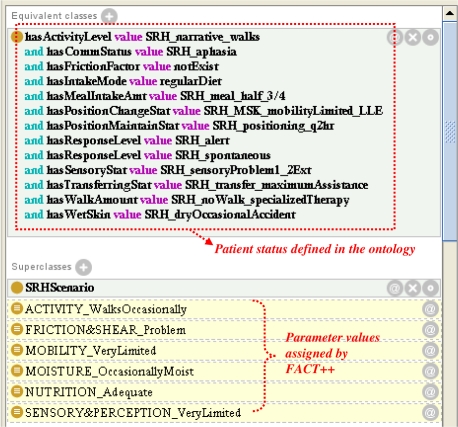
Pressure ulcer risk levels assessed for the scenarios
The 40 patient scenarios were classified into the value categories of the 6 Braden scale parameters using FACT++. Figure 2 is a part of the interface for the Protégé-OWL ontology that shows how a scenario case is defined in the ontology and how it is classified under the Braden scale parameter values based on the data abstraction rules embedded in this ontology.
Figure 2.
Parameter values assigned to a patient scenario by FACT++
Consistency in parameter value assignment
We hypothesized that the consistency scores between the ontology and the nurses would be higher than those between the nurses because variability in interpreting the data can still exist among nurses at a given site, even with the implementation of detailed guidelines. Overall, we observed high consistency scores in most of the parameters. In general, we observed higher levels of consistency between the ontology and the expert nurses than between other pairs (see Table 3). This was expected because the ontology represents the assessment methods identified by the expert nurses. The opposite results like in the Moisture Exposure parameter at site 1, where the consistency between the nurses was higher than the consistency between the ontology and nurses, suggest that the assessment methods identified by the expert nurse was either incorrectly or incompletely represented in the ontology.
Table 3.
Consistency scores of parameter assessment
| Site 1 | Site 2 | |||||
|---|---|---|---|---|---|---|
| Parameter | O-E | E-A | O-A | O-E | E-A | O-A |
| SensPerc | 0.80 | 0.65 | 0.70 | 0.83 | 0.83 | 0.85 |
| Moisture | 0.53 | 0.80 | 0.53 | 0.90 | 0.83 | 0.93 |
| Activity | 0.80 | 0.75 | 0.85 | 1.00 | 0.95 | 0.95 |
| Mobility | 0.83 | 0.85 | 0.78 | 0.83 | 0.85 | 0.88 |
| Nutrition | 0.99 | 0.75 | 0.83 | 1.00 | 0.95 | 1.00 |
| FricShear | 0.73 | 0.83 | 0.80 | 0.73 | 0.73 | 0.80 |
O: Ontology, E: Expert nurse, A: Another nurse
Discussion
In this study, we demonstrated that site-specific methods for pressure ulcer risk assessment can be explicitly defined and integrated into the standard assessment methods that the Braden scale provides. In addition, the scenario testing seems to show that a high level of consistency can be achieved in assigning parameter values when nurses use the same data items based on the explicitly-stated decision guidelines.
However, lack of directly comparable counter examples and use of the patient scenarios, which might be simpler than real patient cases, constitute limitations of this study. Among others, the high level of consistency shown in Nutritional Status assessment in both sites is noticeable. Nutritional Status has been identified as the least consistently assessed parameter because it requires long-term nutritional intake information for a patient [4]. The high level of consistency could be explained as a true positive effect of following the explicitly defined assessment methods, but could also indicate that the testing scenarios and/or the site-specific assessment methods were over-simplified. Further studies are necessary to elucidate this question.
The scenario testing results also showed that certain site-specific data items and data synthesis methods were not completely captured in the ontology. We are following up with the expert nurses on this result to better understand the causes of this discrepancy. However, this may imply that the pressure ulcer risk assessment as a whole is bigger than the sum of its parts – the collection of discrete patient data. When the discrete data are assembled together in the risk assessment context, additional features about the patient status may arise, as explained by the studies on humanistic- or context-dependent views on the nature of nursing inference [16].
Further investigation on the noted limitations needs to follow this study. First, the site-specific assessment methods obtained from one nurse need to be validated in a larger group of nurses at that site. Second, the risk assessment methods compiled in this study need to be tested with real patient data to identify any practical issues in applying this approach to real world practice. Missing data and difficulties with temporal abstraction of long-term observations are a few examples of such issues. In addition, we need to include more diverse settings in future studies, to better capture practical pressure ulcer risk assessment methods that can be shared across various practice settings.
Conclusion
Consistent and accurate assessment of risk for developing pressure ulcers is a critical first step for effective prevention. This study demonstrated modeling the site-specific methods for pressure ulcer risk assessment within a framework of standard methods of the Braden scale. The model built for this study has limitations that need to be addressed in a future studies. If these limitations are successfully addressed, the resulting model may serve as the basis to build a generalizable decision support tool for pressure ulcer risk assessment that can assist nurses with consistent and accurate pressure ulcer risk assessment, and allow comparison of adjusted outcomes across different healthcare settings.
Footnotes
References
- 1.Hill-Rom 2007. Hospitals could improve outcomes for patients and save millions according to Hill-Rom 10th Annual Pressure Ulcer Survey.
- 2.Bergstrom N, et al. The Braden Scale for Predicting Pressure Sore Risk. Nurs Res. 1987;36(4):205–10. [PubMed] [Google Scholar]
- 3.Pancorbo-Hidalgo PL, et al. Risk assessment scales for pressure ulcer prevention: a systematic review. J Adv Nurs. 2006;54(1):94–110. doi: 10.1111/j.1365-2648.2006.03794.x. [DOI] [PubMed] [Google Scholar]
- 4.Kottner J, Dassen T. An interrater reliability study of the Braden scale in two nursing homes. Int J Nurs Stud. 2008;45(10):1501–11. doi: 10.1016/j.ijnurstu.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 5.Kottner J, Dassen T. Pressure ulcer risk assessment in critical care: Interrater reliability and validity studies of the Braden and Waterlow scales and subjective ratings in two intensive care units. Int J Nurs Stud. 2009 doi: 10.1016/j.ijnurstu.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Bergstrom N, et al. Predicting pressure ulcer risk: a multisite study of the predictive validity of the Braden Scale. Nurs Res. 1998;47(5):261–9. doi: 10.1097/00006199-199809000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Anthony D, et al. Do risk assessment scales for pressure ulcers work? J Tissue Viability. 2009 doi: 10.1016/j.jtv.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 8.Papanikolaou P, Lyne P, Anthony D. Risk assessment scales for pressure ulcers: a methodological review. Int J Nurs Stud. 2007;44(2):285–96. doi: 10.1016/j.ijnurstu.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 9.Magnan MA, Maklebust J. The effect of Web-based Braden Scale training on the reliability and precision of Braden Scale pressure ulcer risk assessments. J Wound Ostomy Continence Nurs. 2008;35(2):199–208. 209–12. doi: 10.1097/01.WON.0000313643.60117.b2. discussion. [DOI] [PubMed] [Google Scholar]
- 10.Maklebust J, Magnan MA. A quasi-experimental study to assess the effect of technology-assisted training on correct endorsement of pressure ulcer preventive interventions. Ostomy Wound Manage. 2009;55(2):32–42. [PubMed] [Google Scholar]
- 11.Tu SW, et al. Using an integrated ontology and information model for querying and reasoning about phenotypes: The case of autism. AMIA Annu Symp Proc. 2008:727–31. [PMC free article] [PubMed] [Google Scholar]
- 12.Colombo G, et al. An ontological modeling approach to cerebrovascular disease studies: The NEUROWEB case. J Biomed Inform. 2010 doi: 10.1016/j.jbi.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 13.Tu SW, et al. Ontology-based configuration of problem-solving methods and generation of knowledge-acquisition tools: application of PROTEGE-II to protocol-based decision support. Artif Intell Med. 1995;7(3):257–89. doi: 10.1016/0933-3657(95)00006-r. [DOI] [PubMed] [Google Scholar]
- 14.FACT++. [cited 2010 February 5]; Available from: http://owl.man.ac.uk/factplusplus/.
- 15.Banning M. A review of clinical decision making: models and current research. J Clin Nurs. 2008;17(2):187–95. doi: 10.1111/j.1365-2702.2006.01791.x. [DOI] [PubMed] [Google Scholar]