Abstract
Many hospitals have experienced challenges with accomplishing the Joint Commission’s National Patient Safety Goal for medication reconciliation. Our institution implemented a fully electronic process for performing and documenting medication reconciliation at hospital admission. The process used a commercial EHR and relied on a longitudinal medication list called the “Outpatient Medication Profile” (OMP). Clinician compliance with documenting medication reconciliation was difficult to achieve, but approached 100% after a “hard-stop” reminder was implemented. We evaluated the impact of the process at a large urban academic medical center. Before the new process was adopted, the average number of medications contained in the OMP for a patient upon admission was <2. One year after adoption, the average number had increased to 4.7, and there were regular updates made to the list. Updating the OMP was predominantly done by physicians, NPs, and PAs (94%), followed by nurses (5%) and pharmacists (1%).
Introduction
Medication reconciliation is the process of comparing a patient’s medication orders to all of the medications the patient has been taking. The purpose of medication reconciliation is to avoid medication errors. In 2005, the Joint Commission created a National Patient Safety Goal (NPSG) requiring that medication reconciliation be performed at every care transition (e.g., a change in setting, service, practitioner, or level of care) where medication orders are changed or rewritten.1 The current version of the NPSG specifies that when patients are admitted to the hospital, a complete list of the medications they are taking at home (including dose, route, and frequency) should be created and documented. Medications ordered for patients should be compared to those on the list, and any discrepancies (e.g., omissions, duplications, adjustments, deletions, additions) should be reconciled and documented.2
In March 2010, the Joint Commission issued a statement explaining that “many organizations have struggled to develop and implement effective and efficient processes to meet the intent of the Goal” for medication reconciliation.3 As a result, the Joint Commission temporarily suspended the requirement, noting that “failure to comply will not be factored into an organization’s accreditation decision.” Notwithstanding the suspension, medication reconciliation continues to be an important patient safety issue4, and a revised NPSG is expected from the Joint Commission in January 2011.3
Our hospital instituted an interdisciplinary, electronic process for reconciling patients’ medications upon hospital admission. Before the adoption of the medication reconciliation process, pre-admission medications were generally documented on paper or as free-text in notes in the electronic health record (EHR). After the adoption, an electronic structured medication list was shared across the institution’s ambulatory EHR and inpatient EHR. The goal of this study was to assess the impact of adopting the electronic medication reconciliation process at a large academic medical center.
Background
As patients transfer among community-based and hospital providers, there are numerous opportunities for medication errors, including omissions, duplications, dosing errors, and drug interactions. Evidence suggests that poor communication at care transition points is responsible for 50% of medication errors and 20% of adverse drug events in hospitals.5, 6 In the emergency department, Caglar et al. found that 87% of medication lists had at least one error (incorrect dosage, frequency, or missing medication).7 Shepherd and Schwartz found that the history obtained at triage failed to identify at least one medication in 48% of patients.8
Examining admission orders compared to a comprehensive medication history obtained through interview, Cornish et al. found that 54% of patients had at least 1 unintended discrepancy, 39% of which had the potential to cause moderate to severe discomfort or clinical deterioration.9 In a prospective observational study examining admission and discharge orders in 180 patients, Pippins et al. identified 186 unintended medication discrepancies that had potential for harm due to errors taking the preadmission medication history.10 Electronic medication reconciliation tools can improve the accuracy and completeness of medication information and potentially reduce errors.11, 12
Methods
The setting for this investigation was Columbia University Medical Center (CUMC), an urban hospital delivering care to a medically underserved population in New York City. CUMC was one of two academic medical centers that were part of NewYork-Presbyterian Hospital. CUMC used a commercial EHR (Eclipsys Sunrise, Eclipsys Corp., Atlanta, GA). The EHR had been deployed since 2004 and was used for computerized provider order entry (CPOE), recording medication administration events, and clinical documentation.
In April 2007, clinical and information technology leadership at the hospital began developing a strategy to improve the existing medication reconciliation process. At that time, medication reconciliation at hospital admission used paper forms and was unreliable. The decision of the group was to use the EHR to maintain a coded, longitudinal medication list known as the “Outpatient Medication Profile” (OMP).
In July 2007, the OMP was made available in the EHR for use by physicians, physician assistants, and nurse practitioners. As the OMP was refined over the course of several months, pharmacists and nurses were given the ability to enter historical outpatient medications. Medications were entered as coded data elements, and optionally included fields such as form, dose, route, frequency, and start and end times. Entering a medication was accomplished by selecting the drug name from a formulary database, from a personal “favorites” list, or entering it as free-text.
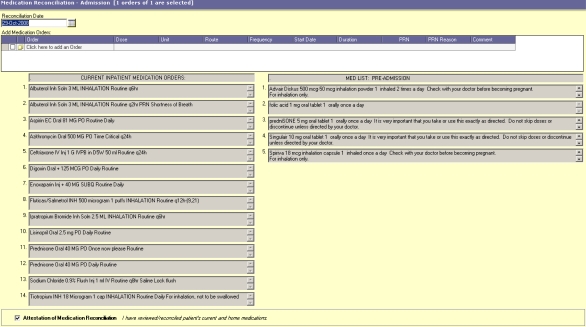
In addition to its use in the medical center, the OMP was used in several community-based clinics to enter prescriptions and historical medications. The OMP was longitudinal in scope, meaning that medications were visible to providers during subsequent inpatient encounters and clinic visits. When a patient was admitted to the hospital, a member of the care team was expected to update the OMP by verifying existing entries and adding new medications that the patient was taking. A medication reconciliation view was created within the EHR that displayed two columns: 1) the list of the current inpatient medication orders and 2) the list of outpatient medications from the OMP (see Figure 1). From this screen, a provider could identify discrepancies between the two lists and update the inpatient orders accordingly. Once finished, the provider attested that medication reconciliation was complete by clicking a checkbox and entering his or her password.
Figure 1.
Custom medication reconciliation screen in the commercial EHR. Current inpatient orders are shown on the left side of the screen, and on the right are home medications from the outpatient medication profile (OMP).
By February 2008, the OMP was integrated into all admission notes, and the medication reconciliation view was linked to admission order sets. The electronic process became the approved method for reconciling medications throughout the institution. Adoption of the process was slow. To improve adoption, clinical leadership of the hospital consulted with the house staff and IT personnel to create a medication reconciliation reminder in the inpatient EHR. Six hours after admission to the hospital (as recorded by the institution’s electronic admission/discharge/transfer system), a reminder dialog was displayed when placing orders in the CPOE system if attestation of medication reconciliation had not been completed. If the attestation had not been completed by eighteen hours after admission to the hospital, a “hard-stop” dialog was displayed and no orders could be placed until attestation was documented. Attestation of admission medication reconciliation required the OMP to be non-empty (i.e., one or more outpatient medications were listed, or the absence of home medications was documented).
The “hard-stop” reminder for medication reconciliation was implemented in October 2008. To evaluate how the new process affected the ways by which clinicians collected and reconciled medications, we answered the following questions:
When a patient was admitted to the hospital, how many active medications already existed in the Outpatient Medication Profile? How many were added or modified at the time of admission? What types of medications were added?
What was the delay between hospital admission and the attestation of medication reconciliation? Did the delay decrease in the weeks following the implementation of the “hard-stop” reminder?
How often did various types of care providers (e.g., physician/provider, nurse, and pharmacist) enter medications into the Outpatient Medication Profile?
Data to answer these questions was obtained by querying the institutional clinical data warehouse. The Institutional Review Board at CUMC approved the study.
Results
All inpatient encounters from November 2007 through October 2009 were reviewed. There were a total of 114,614 encounters during this period. We identified 9,038 hospitalizations with length of stay less than 24 hours. Because hospital policy required medication reconciliation to be performed within 24 hours of admission, these encounters were excluded from further analyses.
Of the remaining 105,576 encounters, 52.0% were repeat visits (i.e., these patients were already known to the institution). 57.8% of the hospitalizations came from female patients, and the average patient age was 49.7 years. The most common admission service for patients was Medicine (44%), followed by Maternal/Fetal Medicine (14%), Surgery (11%), Pediatric Medicine (8%), Psychiatry (4%), Neurology (4%), and Orthopedic Surgery (3%).
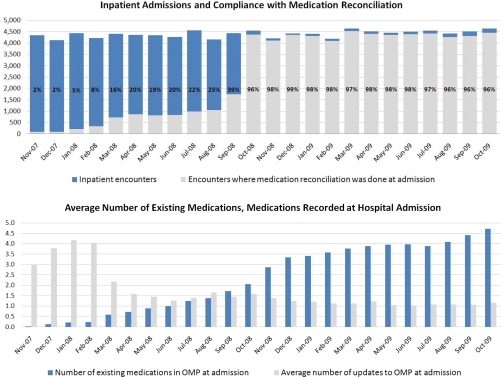
Figure 2 shows the monthly trend of medication reconciliation attestation compliance, the number of medications listed in patients’ outpatient medication profiles at hospital admission, and number of updates during medication reconciliation process. Before the implementation of the reminder, usage of the electronic medication reconciliation process was low (<40% usage). The “hard-stop” intervention improved the rate of medication reconciliation documentation to above 96% within one month. Before the intervention, the average number of medications contained in the OMP for a patient upon admission was less than 2. One year later, the average number had increased to 4.7 medications. The average number of modifications made to the list during the medication reconciliation process decreased over time, from more than 3 modifications in October 2007 to approximately 1 in October 2009. The decline in the number of modifications on admission demonstrates the benefit of a longitudinal medication list that spans encounters.
Figure 2.
Compliance with medication reconciliation, number of medications in patients’ Outpatient Medication Profile (OMP) at hospital admission, and number of updates during medication reconciliation process.
Before the reminder intervention, the mean duration between hospital admission and attestation of medication reconciliation was 84.5 hours (median= 9.1 hours). After the reminder intervention, the mean duration between hospital admission and attestation of medication reconciliation was 9.2 hours (median= 5.3 hours).
Table 1 shows the frequency of additions to the OMP. The most common medications added to the list were central nervous system agents (including pain medications) (17%), cardiovascular agents (16%), and gastrointestinal agents (9%). The medications in the “Other” class included immunologic agents, antineoplastics, genitourinary tract agents, and items entered as free-text that were not classifiable.
Table 1.
Medications added to OMP by drug class.
| Drug Class | # | % |
|---|---|---|
| Central nervous system agents | 47,386 | 17 |
| Cardiovascular agents | 45,221 | 16 |
| Gastrointestinal agents | 24,572 | 9 |
| Nutritional products | 21,100 | 8 |
| Metabolic agents | 20,906 | 8 |
| Coagulation modifiers | 20,395 | 7 |
| Anti-infectives | 14,068 | 5 |
| Respiratory agents | 8,751 | 3 |
| Hormones/hormone modifiers | 8,327 | 3 |
| Psychotherapeutic agents | 8,270 | 3 |
| Topical agents | 5,499 | 2 |
| Other | 51,687 | 18 |
| TOTAL | 276,182 | 100 |
Table 2 shows the number of additions to the OMP by clinician role. The medications in the OMP were most commonly updated by resident physicians (39%) and nurse practitioners/physician assistants (36%), followed by attending physicians (19%). Nurses occasionally edited information in the OMP (5%); pharmacists performed this task rarely (1%).
Table 2.
Additions to OMP by clinician role.
| Role | # | % |
|---|---|---|
| Resident Physician | 108,423 | 39 |
| Nurse Practitioner/Physician Assistant | 99,751 | 36 |
| Attending Physician | 51,475 | 19 |
| Nurse | 14,339 | 5 |
| Pharmacist | 2,194 | 1 |
| TOTAL | 276,182 | 100 |
Discussion
The medication reconciliation process at our institution had a substantial impact on clinician workflow. Compliance with the process was poor prior to the introduction of the hard-stop reminder. Clinicians complained about the amount of time required for adding medications to the OMP (estimated to require from 30–60 seconds per medication). Another issue was a technical limitation of the EHR software which prevented medications entered into the OMP from being converted to inpatient orders. This limitation caused clinicians to perform medication lookups in the EHR twice, in addition to documenting the home medications in the electronic admission note. Some of these issues have been addressed in newer versions of the EHR software and by local customization, but there is still room for improvement. EHR vendors can facilitate better medication reconciliation processes by improving user interfaces and by synchronizing data with external pharmacies and personal health records (PHRs) to enhance the accuracy and completeness of home medication lists.
To alleviate the time burden on physicians, physicians assistants and nurse practitioners for data entry, nurses and pharmacists were given access to update the OMP. However, nurses and pharmacists seldom updated medications in practice. This is in contrast to processes described at other institutions 12, 13, where admission medication reconciliation involved pharmacy or nursing staff to a much greater degree. We did not examine whether nurse usage of the OMP decreased after physicians became more familiar with the process.
Though clinician input was used in the design of the hard-stop reminder, like many EHR alerts, the reminder was initially unpopular. The reminder was perceived more as an attempt to address a compliance issue than an effort to improve patient safety. While we are encouraged by the high rate of compliance with the process, we are more encouraged by the growing use of the OMP across encounters and care settings. The fact that the OMP is regularly updated suggests that effective medication reconciliation is occurring. In this retrospective study, there was no “gold standard” home medication list. Likewise, in clinical practice, there is often uncertainty about the medications a patient is taking. While the use of the OMP has been perceived to improve medication management for patients at our institution, additional analyses are necessary to assess the validity and quality of the data entered.
There are some limitations to this study. First, it was performed retrospectively and relied only on quantitative methods. A survey of user experience with the medication reconciliation process will provide much additional insight. Another limitation is that the study was performed at a single site. Comparable data from other hospitals adopting electronic medication management processes are needed to assess the generalizability of our findings.
Conclusions
A fully electronic medication reconciliation process with a hard-stop reminder achieved widespread compliance at our academic medical center. Use of a structured, longitudinal medication list can be beneficial for medication reconciliation. EHR vendors should improve the efficiency and usability of home medication lists in their products to enhance accuracy and minimize the need for local development and customization.
Acknowledgments
This project was supported by a grant from the Agency for Healthcare Research and Quality (AHRQ) (1 R03 HS018250-01).
References
- 1.Hospitals’ National Patient Safety Goals. 2005. (Accessed March 10, 2010, at http://www.jointcommission.org/NR/rdonlyres/CA814047-805D-4143-AD3C-0C1944C49E75/0/05_hap_npsg.pdf.)
- 2.Hospitals’ National Patient Safety Goals. 2010. (Accessed March 10, 2010, at http://www.jointcommission.org/NR/rdonlyres/868C9E07-037F-433D-88580D5FAA4322F2/0/RevisedChapter_HAP_NPSG_20090924.pdf.)
- 3.Medication reconciliation National Patient Safety Goal to be reviewed, refined. 2010. (Accessed March 10, 2010, at http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/npsg8_review.htm.)
- 4.Gleason KM, McDaniel MR, Feinglass J, et al. Results of the Medications At Transitions and Clinical Handoffs (MATCH) Study: an analysis of medication reconciliation errors and risk factors at hospital admission. J Gen Intern Med. 2010. epub ahead of print. [DOI] [PMC free article] [PubMed]
- 5.Barnsteiner JH. Medication reconciliation: transfer of medication information across settings-keeping it free from error. Am J Nurs. 2005;105:31–6. doi: 10.1097/00000446-200503001-00007. quiz 48–51. [DOI] [PubMed] [Google Scholar]
- 6.Rozich JD. Medication safety: one organization’s approach to the challenge. J Clin Outcomes Manage. 2001;8:27–34. [Google Scholar]
- 7.Caglar S, Henneman PL, Blank FS, et al. Emergency department medication lists are not accurate. J Emerg Med. 2008 doi: 10.1016/j.jemermed.2008.02.060. [DOI] [PubMed] [Google Scholar]
- 8.Shepherd G, Schwartz RB. Frequency of incomplete medication histories obtained at triage. Am J Health Syst Pharm. 2009;66:65–9. doi: 10.2146/ajhp080171. [DOI] [PubMed] [Google Scholar]
- 9.Cornish PL, Knowles SR, Marchesano R, et al. Unintended medication discrepancies at the time of hospital admission. Arch Intern Med. 2005;165:424–9. doi: 10.1001/archinte.165.4.424. [DOI] [PubMed] [Google Scholar]
- 10.Pippins JR, Gandhi TK, Hamann C, et al. Classifying and predicting errors of inpatient medication reconciliation. J Gen Intern Med. 2008;23:1414–22. doi: 10.1007/s11606-008-0687-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bails D, Clayton K, Roy K, Cantor MN. Implementing online medication reconciliation at a large academic medical center. Jt Comm J Qual Patient Saf. 2008;34:499–508. doi: 10.1016/s1553-7250(08)34063-x. [DOI] [PubMed] [Google Scholar]
- 12.Schnipper JL, Hamann C, Ndumele CD, et al. Effect of an electronic medication reconciliation application and process redesign on potential adverse drug events: a cluster-randomized trial. Arch Intern Med. 2009;169:771–80. doi: 10.1001/archinternmed.2009.51. [DOI] [PubMed] [Google Scholar]
- 13.Murphy EM, Oxencis CJ, Klauck JA, Meyer DA, Zimmerman JM. Medication reconciliation at an academic medical center: implementation of a comprehensive program from admission to discharge. Am J Health Syst Pharm. 2009;66:2126–31. doi: 10.2146/ajhp080552. [DOI] [PubMed] [Google Scholar]