Abstract
We describe our early experience with use in emergency department settings of a standards-based medication history service integrated into a health information exchange (HIE). The service sends queries from one Exchange’s emergency department interface both to a local ambulatory care system and to the medication hub services provided by a second HIE. This second HIE in turn sends requests to SureScripts and returns histories for incorporation into the first Exchange’s clinical interface. The service caches all requests to avoid costly duplicate query charges and maintains an account of queries, registered users, charges, and results obtained. Usage may be increasing as additional retail pharmacy data become available. Early results suggest that research and development emphasis requirements will of necessity shift from obtaining prescription medication history to finding new means to ensuring effective use.
Introduction
The need for a comprehensive digital medication history has been recognized for over a decade.1 A 1999 telephone survey of 2, 590 individuals aged 18 or over showed that 81% used at least one medication in the preceding week; 50% took at least one prescription drug; and 7% took five or more prescription drugs.2 Patient history data from EMRs may not accurately represent a patient’s full prescription drug profile. An infrastructure to provide medication history services appears essential.3
Early efforts to provide comprehensive prescription medication histories were fraught with challenges.4 The earliest prescription medication histories on a national level were dependent on pharmacy benefits administrative claims available through RxHub or other third-party aggregators. Low-priced prescriptions and all prescriptions not covered by participating PBMs were not generally available through these services service. Over time, additional prescription data became available from SureScripts, a for-profit organization that fostered direct communication to almost every retail pharmacy for e-prescribing communications. With the merger of RxHub and SureScripts in 2009, prescription medication histories have become more comprehensive and more widely available through certified e-prescribing systems. But the availability of such histories in care settings without e-prescribing systems has been less comprehensive and traditionally has been associated with additional transaction costs.
The Memphis HIE
In 2004, Vanderbilt University was funded by the Agency for Health Research and Quality, Vanderbilt University, and the State of Tennessee to create a comprehensive health information exchange for the Memphis TN region.5 This Exchange became operational in May of 2006. Using an architecture developed for the Vanderbilt Medical Center, the Exchange is capable of delivering clinical information through a secure Web browser in emergency departments, ambulatory settings, and to hospitalists.6 The Exchange currently incorporates data from 15 hospitals and 15 ambulatory clinics in the greater Memphis Area. Currently, the Exchange makes available clinical data for over 5 million encounters by over 1.2 million individuals. The Exchange is governed by a non-profit board and is now supported by a commercial vendor. Operational costs to support the Exchange for over 1 million people are less than $2.5 million per year.
The most active area of Exchange use is in hospital emergency departments. Here registration events automatically trigger display on a “white board” of the patient, the number of past encounters in the institution in which they are seeking care as well as the number of encounters at other institutions. Clinicians can electively examine clinical data from the Exchange. Both anecdote and formal evaluation show statistically significant changes in workflow, test ordering, and other behaviors. (Publication in progress.) Unlike many other similar efforts, the Vanderbilt project in Memphis never incorporated savings associated from e-prescribing or medication history services into its business or sustainability plans because it was believed then that such services would arise independent of regional health information exchanges.
The Medication History Service
In the summer of 2007, AHRQ commissioned Vanderbilt to extend the Exchange’s functionality in order to explore the barriers to and benefits of incorporating a prescription medication history into clinical settings where clinicians did not have access to e-prescribing systems but did have access to the Exchange. The need for such work was the result of early national e-prescribing trials supported by CMS and the frustration experienced by a growing number of health information exchanges as they attempted to incorporate prescription drug information into their services.4,7 Recognizing the challenges and costs encountered in creating a de novo medication history service contract from SureScripts, Vanderbilt chose instead to create an interoperable system with a robust service already in use by the Regenstrief Institute and the Indiana Health Information Exchange (IHIE).8 Regenstrief was allowed contractually to expand its services to support Memphis on a trial basis.
To establish such a service, the Vanderbilt architecture in Memphis had to be extended to transmit necessary demographic information to Regenstrief. Because demographic information on a single individual at times differed because of data entry errors or name changes, choices had to be made on which demographic record to submit.
Because prescription medication history transactions incurred a charge from SureScripts, the Vanderbilt technologies in Memphis incorporated a query cache of queries requested and results obtained within the past 13 hours so that one request would not be made repeatedly and the service charged multiple times. Generally, requests to Regenstrief are based on the demographic information recorded by the institution in which the patient was currently seeking care. The HL7 messages are sent to Regenstrief are then sent to SureScripts. The SureScripts system in turn routes requests to record locator systems resident in member PBMs, pharmacies, and SureScripts core services (Figure 1).
Figure 1.
Data flows among Memphis clinical systems, the Memphis HIE, IHIE, and prescription history sources. With the exception of medication histories obtained from a local EHR system, all prescription medication history information was received through IHIE.
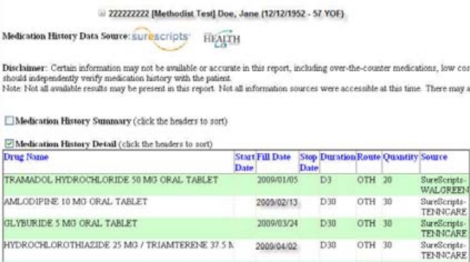
Response messages were of three message types: “no patient identified”; “patient identified but no prescription history available”; “prescription history available.” When a history was available it was returned to Regenstrief and returned to the Exchange. Although the Regenstrief medication hub had the capability to link medication histories to RxNorm and to resolve some duplicates, the Vanderbilt architecture did not take advantage of these services. Data were incorporated into displays similar to those used at the Vanderbilt Medical center (Figure 2). Some data sorting and associating features were available but comprehensive integration based on RxNorm and other lexicons was not attempted during the trial period.
Figure 2.
Display of the prescription drug history
Later, data recorded in medication histories obtained by clinicians using the NextGen EHR were also incorporated into the service.
Use of the Prescription History Service
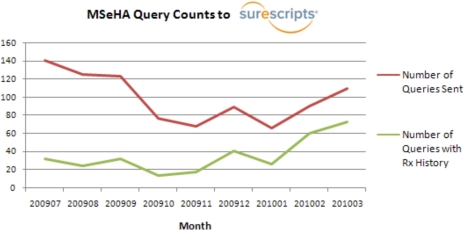
Usage is low probably because the project has not yet been formally introduced to clinicians and the charge associated with the service provided some disincentive. In the initial weeks users did not consistently use the service because few records were returned. During this period, only 27% of queries returned positive results. Since then, usage has stabilized and may be increasing with the addition first Tennessee Medicaid data later as data were available from a major retail chain pharmacy (Figure 3).
Figure 3.
Usage over time. Usage decreased by 50% in the early months as users recognized the relative low yield. Use is trending upward as the positive query response rate has grown from 27% to almost 70%. (Data for March are extrapolated from the first 12 days of the month.)
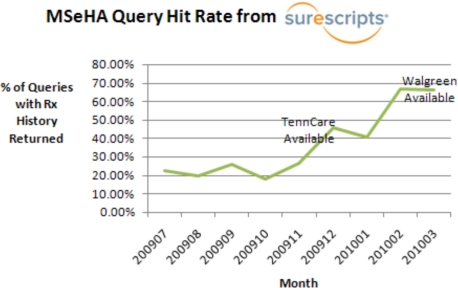
Most striking is the relationship between response rate and participation of health plans and participating pharmacies active in the region. Few patients were covered by the original RxHub PBMs and initial queries returned a history in only 27% of cases. The positive prescription history response rate predictably increased to almost 50% when Tennessee Medicaid (TennCare) data became available (Figure 4). The positive response rate increased to 70% as data from just one dominant chain pharmacy was made available through SureScripts (Figure 5).
Figure 4.
The relationship between positive prescription history response and the availability of additional relevant prescription data sources.
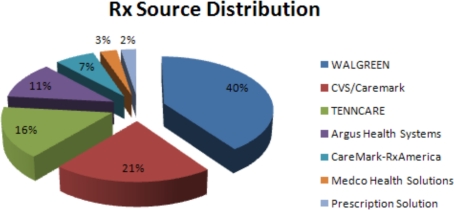
Figure 5.
Sources of prescription drug histories to the Memphis HIE. (February, 2010).
A compelling argument can be made that retail pharmacy data is the most crucial contributor to a comprehensive prescription drug history. Administrative claims prescription drug history data may be incomplete because claims for inexpensive drugs are not always submitted. Furthermore, many individuals do not have PBM or health plan coverage and pay for their own medications. But retail pharmacies can make prescription medication history available through SureScripts and through these means address this deficiency. Some independent pharmacies may not have the resources available to contribute data to these services.
Implications
Regulatory and market considerations make a “liquid” prescription medication history service an inevitability. The HITECH act cannot be implemented without this service.9.10 The rapid growth in e-prescribing and the interest of both pharmacy benefits managers and retail pharmacies will drive standards and lower the marginal cost to provide prescription medication history services. The networking effect seen in e-prescribing adoption is perhaps a harbinger for a corresponding increase in prescription history services. History suggests such a network effect. In August of 2007, Regenstrief Institute reported only a 5% positive response rate from RxHub.8 Our early results now return a 70% positive response rate. This response rate should exceed 90% as additional retail pharmacies make their history available through real-time aggregator services. This interest will undoubtedly create ancillary products to support real-time monitoring of controlled substances and novel approaches to supporting medication adherence. Because of meaningful use provisions, all vendors will integrate these services but may take different approaches to presentation and workflow integration.
Although adoption will impact safety significantly, the inclusion of accurate data on herbals, supplements, and over-the-counter medications remains problematic and significant. At least thirteen percent of elderly individuals purchase herbal drugs.11 Use of other over-the-counter medicines that could impact adverse drug events is higher. An effective system, therefore, must acquire accurate data on all drug classes, present these data in ways that enable effective decision-making, and integrate such services into clinical workflow.12
Many research and technical tasks lie ahead. The national effort to map NDC codes to RxNorm terms and to identify therapeutic classes and other semantic relationships will be essential to guide therapy and to promote medication adherence. Matching diverse data sources to the right individual must be consistently realized. Developing means of delivering additional information to support decision-making in clinical settings will become essential as therapies become more influenced by genetics and genomic science, proteomics, and the discovery of new biomarkers.
Our experience with a prescription medication history service suggests that the availability of a standardized prescription medication history will be of great clinical value. The research and application focus will necessarily shift from acquisition to effective use and informed clinical action.
Acknowledgments
Portions of this work were funded through AHRQ Contract 290-04-0006, the State of Tennessee, and Vanderbilt University. This presentation has not been approved by the Agency for Healthcare Research and Quality. The authors acknowledge the contribution, partnership, and collegiality of the Regenstrief Institute and the many Vanderbilt faculty and staff participants.
References
- 1.Kohn LT, Corrigan J, Donaldson MS, Institute of Medicine (U.S.) To err is human: building a safer health system. Washington, D.C: National Academy Press; 2000. Committee on Quality of Health Care in America. [PubMed] [Google Scholar]
- 2.Kaufman DW, Kelly JP, Rosenberg L, Anderson TE, Mitchell AA. Recent patterns of medication use in the ambulatory adult population of the United States: the Slone survey. JAMA. 2002 Jan 16;287(3):337–44. doi: 10.1001/jama.287.3.337. [DOI] [PubMed] [Google Scholar]
- 3.National Library of Medicine (U.S.) Commission on Systemic Interop-erability. Bethesda, MD: U.S. National Library of Medicine, NIH; 2005. [Google Scholar]
- 4.Gottlieb LK, Stone EM, Stone D, Dunbrack LA, Calladine J. Regulatory and policy barriers to effective clinical data exchange: lessons learned from MedsInfo-ED. Health Affairs (Millwood) 2005 Sep–Oct;24(5):1197–204. doi: 10.1377/hlthaff.24.5.1197. [DOI] [PubMed] [Google Scholar]
- 5.Frisse ME. State and community-based efforts to foster interoperability. Health Affairs (Millwood) 2005 Sep–Oct;24(5):1190–6. doi: 10.1377/hlthaff.24.5.1190. [DOI] [PubMed] [Google Scholar]
- 6.Frisse ME, King JK, Rice WB, Tang L, Porter JP, Coffman TA, et al. A regional health information exchange: architecture and implementation. AMIA Annu Symp Proc. 2008:212–6. [PMC free article] [PubMed] [Google Scholar]
- 7.Leavitt M. Pilot Testing of Initial Electronic Prescribing Standards – Cooperative Agreements Required Under Section 1860D-(4) (e) of the Social Security Act as Amended by the Medicare Prescription Drug, Improvement, and Modernization Action (MMA) of 2003. Washington: Department of Health and Human Services; 2007. [Google Scholar]
- 8.Simonaitis L, Belsito A, Overhage JM. Enhancing an ePrescribing system by adding medication histories and formularies: the Regenstrief Medication Hub. AMIA Annu Symp Proc. 2008:677–81. [PMC free article] [PubMed] [Google Scholar]
- 9.Blumenthal D. Nov 12, 2009. The HITECH Foundation for Information Exchange: A Message from Dr David Blumenthal, National Coordinator for Health Information Technology: Department of Health and Human Services.
- 10.2010. Federal Register. 45 CFR Part 170 Health Information Technology: Initial Set of Standards, Implementation Specifications, and Certification Criteria for Electronic Health Record Technology; Interim Final Rule. Washington.
- 11.Bruno JJ, Ellis JJ. Herbal use among US elderly: 2002 National Health Interview Survey. Ann Pharmacother. 2005 Apr;39(4):643–8. doi: 10.1345/aph.1E460. [DOI] [PubMed] [Google Scholar]
- 12.Stead WW, Lin H, National Research Council (U.S.) Computational technology for effective health care: immediate steps and strategic directions. Washington, D.C: National Academies Press; 2009. Committee on Engaging the Computer Science Research Community in Health Care Informatics. [PubMed] [Google Scholar]