Abstract
Circadian rhythm sleep disorder, free-running type (CRSD, FRT) is a disorder in which the intrinsic circadian rhythm is no longer entrained to the 24-hour schedule. A unique case of CRSD, FRT in a 67-year-old sighted male is presented. The patient had a progressively delayed time in bed (TIB) each night, so that he would cycle around the 24-h clock approximately every 30 days. This was meticulously documented each night by the patient over the course of 22 years. The patient's CRSD, FRT was associated with severe depression, anxiety, and agoraphobia. The agoraphobia may have exacerbated the CRSD, FRT. Entrainment and stabilization of his circadian rhythm was accomplished after treatment that included melatonin, light therapy, and increased sleep structure.
Citation:
Brown MA; Quan SF; Eichling PS. Circadian rhythm sleep disorder, free-running type in a sighted male with severe depression, anxiety, and agoraphobia. J Clin Sleep Med 2011;7(1):93-94.
Keywords: Circadian rhythm disorders, depression, anxiety
Circadian rhythm sleep disorder, free-running type (CRSD, FRT)1 is a disorder in which the intrinsic circadian rhythm is no longer entrained to the 24-h schedule. Normal individuals who are exposed to an environment devoid of zeitgebers develop free-running rhythms with a period longer than 24 h.2 CRSD, FRT is rare in sighted people but common in blind persons whose entrainment to the light/dark cycle is limited or absent.
CRSD, FRT may result in symptoms such as insomnia, excessive sleepiness, and/or impairment in daytime function with brief asymptomatic periods when their internal circadian rhythms are in line with their desired schedule. Sighted subjects with CRSD, FRT are typically male, younger than age 30 years, have environments with low light levels and atypical schedules, and may have an increased incidence of psychiatric disorders (28%).3,4 We present a unique case of CRSD, FRT in a sighted male associated with severe depression, anxiety, and agoraphobia.
REPORT OF CASE
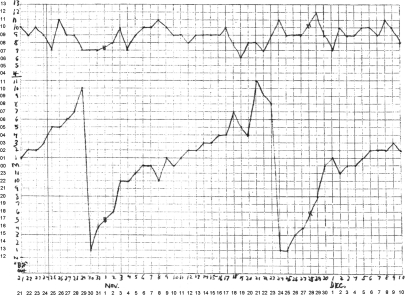
The patient was a 67-year-old sighted, divorced, Caucasian male with major depressive disorder (MDD), obsessive-compulsive disorder (OCD), panic disorder with agoraphobia, chronic obstructive pulmonary disease, and hypertension. He presented with a chief complaint of 22 years of “sleep cycling.” His time in bed (TIB) delayed approximately 30 minutes later each night. Given his severe anxiety and agoraphobia, he was disabled, unemployed, and reclusive, rarely leaving the home. He received minimal natural light but did have environmental cues in the form of clocks, periodicals, and television. He kept meticulous records of his sleep each night for the past 22 years, recording estimated TIB and total sleep time (TST). A sample of the sleep graphs provided by the patient is depicted in Figure 1. He was anxious regarding his sleep; however, sleep onset latency was normal. He experienced 2–3 awakenings per night each lasting 5–30 minutes. He awoke feeling refreshed with an Epworth Sleepiness Scale score of 2/24. Estimated TST was 8–10 hours.
Figure 1.
Example of patient generated sleep log graph from 1986
These were documented daily for over 20 years. The top graph represents total sleep time in hours on the y-axis with calendar day on the x-axis. The bottom graph represents time in bed on the y-axis with calendar day on the x-axis. Number annotations were added to the axes including military time on lower graph y-axis for clarity.
There was no history consistent with other sleep disorders, such as sleep disordered breathing or restless legs syndrome. Medications included doxepin, alprazolam, lisinopril-hydrochlorothiazide, aspirin, kava kava, and valerian root. He smoked tobacco and stopped drinking alcohol in 1977, 5 years prior to symptom onset. There was no history of illicit drug use. Laboratory studies including a normal thyroid-stimulating hormone were unremarkable.
He was prescribed melatonin 3 mg one hour prior to TIB with the intent of phase advancement by taking it one half hour earlier each week. He began taking the melatonin at 02:00 when his current TIB was 03:00 and stopped advancement of the melatonin at 01:00 after 2 weeks. Our subject was also prescribed bright light therapy by stepping outside into direct Arizona sunlight for one half hour each morning upon awakening at 11:00 by alarm clock, slowly advancing to a final time of 10:00. His TIB stopped delaying and advanced to the goal TIB of 02:00 and wake time of 10:00 after approximately one month of melatonin and bright light therapy. His sleep continued to be stable over 4 years of follow-up on this regimen.
DISCUSSION
A presumptive diagnosis of CRSD, FRT was made, given the patient's history and documentation of progressively delayed TIB out of phase with the established 24-h clock. The patient's CRSD, FRT may have been related to his agoraphobia and subsequent lack of exposure to natural light and other social zeitgebers. Isolated subjects in environments devoid of zeitgebers, despite being able to control their own light/dark cycles with artificial light, have changes in the length of the circadian period.2 Psychiatric disorders, and notably anxiety disorders, are also associated with CRSDs. One study examining the incidence of psychiatric disorders in 90 subjects with CRSDs found the most common disorders to be social phobia, OCD, and MDD,5 which were observed in our subject as well.
Although the patient was treated successfully, there are several caveats that deserve consideration. Unfortunately, the patient would not consent to a polysomnogram to exclude other sleep disorders or serial melatonin measurements to estimate his circadian phase. Morning bright light therapy has been described to entrain and advance a sighted individual with CRSD, FRT.6 However, the role of melatonin in our case is uncertain. Notably, maximum circadian advancement with melatonin occurs in the afternoon, approximately 5 hours before the dim light melatonin onset, with relatively little effect when taken close to bedtime.7 In addition, other treatment interventions such as a more structured sleep schedule including an alarm clock may have contributed to his improvement.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.American Academy of Sleep Medicine. The international classification of sleep disorders: Diagnostic & coding manual. 2nd ed. Westchester, IL: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 2.Wever RA. The circadian system of man: Results of experiments under temporal isolation. New York: Springer-Verlag; 1979. [Google Scholar]
- 3.Hayakawa T, Uchiyama M, Kamei Y, et al. Clinical analyses of sighted patients with non-24-hour sleep-wake syndrome: A study of 57 consecutively diagnosed cases. Sleep. 2005;28:945–52. doi: 10.1093/sleep/28.8.945. [DOI] [PubMed] [Google Scholar]
- 4.Sack RL, Auckley D, Auger RR, et al. Circadian rhythm sleep disorders: Part II, advanced sleep phase disorder, delayed sleep phase disorder, free-running disorder, and irregular sleep-wake rhythm. An American Academy of Sleep Medicine Review. Sleep. 2007;30:1484–501. doi: 10.1093/sleep/30.11.1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yamadera W, Sasaki M, Itoh H, Ozone M, Ushijima S. Clinical features of circadian rhythm sleep disorders in outpatients. Psychiatry Clin Neurosci. 1998;52:311–6. doi: 10.1046/j.1440-1819.1998.00395.x. [DOI] [PubMed] [Google Scholar]
- 6.Eastman C, Anagnopoulos C, Cartwright R. Can bright light entrain a free-runner? Sleep Res. 1988;17:372. [Google Scholar]
- 7.Burgess HJ, Revell VL, Eastman CI. A three pulse phase response curve to three milligrams of melatonin in humans. J Physiol. 2008;586:639–47. doi: 10.1113/jphysiol.2007.143180. [DOI] [PMC free article] [PubMed] [Google Scholar]