Abstract
There are many ways to repair distal biceps tendon ruptures with no outcome studies demonstrating superiority of a specific technique. There are few studies reporting on the repair of acute and chronic distal biceps tendon ruptures using the EndoButton via an anterior single-incision approach. We report on 27 patients who underwent distal biceps tendon repair with an EndoButton. The average age was 50.1 years (range, 36–78). There were 17 acute repairs (within 4 weeks of injury), nine chronic repairs (greater than 4 weeks), and one revision of a previous acute repair. All chronic repairs were repaired without the need for graft augmentation. Patients were assessed postoperatively using the ASES elbow outcome instrument and isokinetic flexion and supination strength and endurance testing. Eight control subjects were also tested for comparison. At an average follow-up of 30.9 months, 26 of 27 patients returned to their previous employment and activity level. The average ASES elbow score was 98.2 (range, 81–100). Compared with the contralateral extremity, there was no loss of motion. Average flexion strength recovery was 101% and mean supination strength recovery was 99%. There was no significant difference in function or strength with repair of acute versus chronic ruptures. Using the EndoButton technique, acute and chronic distal biceps tendon ruptures can be repaired safely with excellent clinical results.
Keywords: Distal biceps tendon ruptures, Acute, Chronic, Single incision
Introduction
Distal biceps tendon ruptures are relatively rare injuries, comprising only 3% of all biceps tendon ruptures [10]. Distal biceps tendon ruptures are usually seen in the dominant arm of middle-aged men who describe a single traumatic event in which an unexpected extension force is applied to an elbow in flexion. Anatomic repair of the ruptured distal biceps tendon to the radial tuberosity is recommended to prevent the loss of strength and endurance in forearm supination and elbow flexion [4, 7, 27, 31]. Single-incision techniques and two-incision approaches have been described using either bone tunnels, suture anchors, interference screws, or the EndoButton (Acufex; Smith & Nephew, Inc, Andover, MA) to re-attach the distal biceps tendon to the radial tuberosity [3, 5, 11, 12, 15, 24, 25, 29, 33].
Although initially developed for fixation of an ACL graft, repair of distal biceps tendon ruptures using the EndoButton provides strong fixation to allow for secure fixation and early motion. EndoButton repair of distal biceps tendon ruptures was first described by Bain and colleagues in 2000 [2] and subsequent clinical and biomechanical studies have demonstrated high patient satisfaction, a very low incidence of complications, and higher load to failure when compared to other techniques [2, 11, 13, 18, 26, 34]. The purpose of this study is to report the clinical results of a cohort of patients who underwent single-incision distal biceps tendon repair of acute and chronic injuries using the EndoButton.
Materials and Methods
Forty consecutive patients between November 2001 and September 2004 underwent single-incision distal biceps tendon repair using the EndoButton by the senior author and 27 patients (26 male, one female) agreed to participate in the study. Institutional review board approval was obtained. The patients’ average age was 50.1 years (range, 36–78). Fourteen (52%) injured their dominant extremity while 13 (48%) injured their non-dominant arm. Twelve patients reported lifting a heavy object, seven described a fall, three were catching a falling object, and five had miscellaneous injuries. All patients reported antecubital fossa pain and ecchymosis after the injury and demonstrated weakness with elbow flexion and forearm supination. There were 17 acute repairs (within 4 weeks of injury), nine chronic repairs (greater than 4 weeks), and one revision of a previous acute repair. All chronic repairs were able to be repaired via a single-incision technique without the need for graft augmentation. Eight patients received workers’ compensation.
The senior author’s (JCK) technique for repair of distal biceps tendon ruptures using the EndoButton has been described in detail previously [20]. Briefly, a 3–4 cm longitudinal incision is made from the transverse cubital crease distally along the medial edge of the mobile wad. The lateral antebrachial cutaneous nerve is identified deep to the cephalic vein and protected. Blunt finger dissection in the proximal extent of the wound into the distal aspect of the brachium is performed to retrieve the distal ruptured end of the biceps. The tendon is delivered from the wound and the frayed tendon end debrided back to healthy appearing tissue. The tendon is then prepared for reattachment to the bone with a running suture arcade using two No. 2 braided, nonabsorbable sutures in the distal 2–4 cm of the tendon (Fig. 1). The first is placed in a modified Bunnell fashion, with the second suture arcade placed as a running Krackow, passing both of the sutures through the distal 1 cm of the tendon without grasping stitches. This allows the distal 1 cm of tendon to compress during the passing and flipping stage. The sutures are passed through the middle two holes of the EndoButton, back through the tendon, and tied 1 cm from the end of the tendon leaving a 2–3-mm gap between the tendon end and the button. Passing and flipping suture are placed in the outer holes of the EndoButton. The forearm is placed in a maximally supinated position to expose the bicep tuberosity and protect the posterior interosseous nerve. A unicortical trough is created in the tuberosity, using a 4.5-mm drill bit to make overlapping drill holes and create an oval socket measuring approximately 5 × 10 mm. The guide wire is then drilled across the far cortex of the radius in a distal and medial direction and then overdrilled with the EndoButton reamer. The passing and flipping sutures are fed through the eye of the Beath needle and the guide wire is passed through both holes and drawn out through the dorsal aspect of the forearm. Finally, the elbow is maximally flexed and the forearm supinated, and passing sutures were tensioned to turn the EndoButton 90° and pull the button across the far cortex of the radius. The “flipping” sutures are tensioned to reorient the button and anchor it outside the dorsal cortex of the radius [20] (Fig. 2).
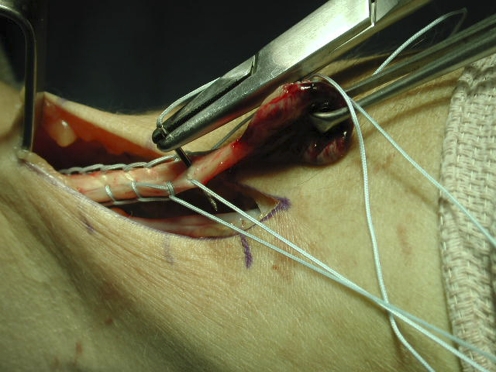
Figure 1.
With the tendon end delivered from the wound, a running suture arcade is placed that will be run through the EndoButton and then tied.
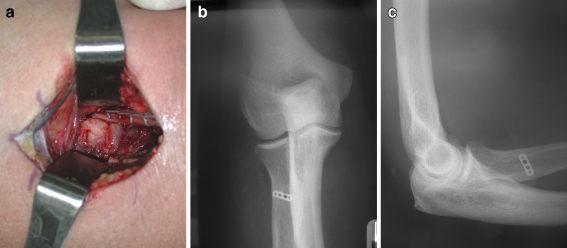
Figure 2.
Final construct with tendon fed through a unicortical radial trough (a). Anteroposterior (b) and lateral (c) radiographs demonstrating the EndoButton is anchored outside the far cortex of the radius.
A posterior mold splint in 90° of flexion is applied for 2 weeks. At 2 weeks, patients are allowed to start active elbow range of motion. At 4 weeks, they are allowed to begin using the arm for activities of daily living, but are not allowed to lift objects greater than 5 lbs. At 8 weeks, patients begin to work on strengthening exercises. Restoration of full forearm flexion and supination strength usually takes up to 6 months postoperatively.
At the latest follow-up, patient evaluation included the ASES Elbow Assessment form [21], physical examination, and strength and endurance testing of both extremities using the BTE work simulator (Baltimore Therapeutic Equipment, Hanover, Maryland). Strength testing was performed by examining the maximal isometric torque, in pounds, of both elbow flexion and supination. Endurance testing was performed by testing isotonic resistance set at 50% maximum, with an endpoint defined by less than 75% power of the initial 5-s interval for either two consecutive intervals or until patient fatigue. Endurance testing was measured in work (pounds degree), distance (degrees), and time (seconds). Elbow flexion, elbow extension, forearm pronation, and forearm supination was measured in the operative and non-operative arm using a standard handheld goniometer.
Other studies have not taken into account the difference between dominant and non-dominant extremities in calculating residual deficits. Therefore, a conversion factor was calculated to allow meaningful comparison between and across study data. This conversion factor was calculated by performing strength and endurance testing of the dominant and non-dominant arms of eight control subjects without biceps pathology. The strength and endurance testing was performed as described above. The conversion factor was then used to predict operative extremity strength or endurance given data from the non-operative side (predicted strength or endurance = measured non-operative value x conversion factor). With this data, a strength/endurance deficit was calculated (deficit = (predicted strength-actual strength)/predicted strength) and used to compare several subgroups of patients: acute versus chronic, workman’s compensation versus non-workman compensation, and non-dominant versus dominant extremity.
Results
The average follow-up was 30.9 months (range, 13–53 months). Results are reported in Table 1. Twenty six of 27 patients returned to their previous employment and activity level. The average score was 9.31 on a ten-point satisfaction visual analog score (VAS). Compared with the contralateral extremity, there was no loss of motion. Strength testing demonstrated near complete return of flexion strength, supination strength, and supination endurance. The strength and endurance ratios of injured side compared to the uninjured side are reported in Table 1. Average flexion strength recovery was 101% (range, 43–118%) and mean supination strength recovery was 99% (range, 47–162%). The average ASES elbow score was 98.2 (range, 81–100).
Table 1.
Patient results: range of motion, strength, and outcome scores.
| Case no. | Age (years) | Acute (<4 weeks); chronic (>4 weeks) | Follow-up (months) | ROM (deg)a; injured side/uninjured side | Flexion strength ratio; injured side/uninjured side (%) | Flexion endurance ratio; injured side/uninjured side (%) | Supination strength ratio; injured side/uninjured side (%) | Supination endurance Ratio; injured side/uninjured side (%) | ASES Elbow Score | |
|---|---|---|---|---|---|---|---|---|---|---|
| Extension/flexion | Pronation/supination | |||||||||
| 1 | 44 | Chronic | 41 | 0–130/−5–135 | 70–60/80–75 | 100% | 103 | 106% | >200% | 98 |
| 2 | 52 | Acute | 43 | 2–132/4–134 | 66–69/60–78 | 113% | 113% | 88.7% | 58.8% | 99 |
| 3 | 78 | Chronic | 32 | 23–125/19–127 | 47–70/48–85 | 109% | 132% | 142% | 73% | 100 |
| 4 | 69 | Chronic | 15 | −1–135/0–135 | 65–72/75–70 | 110% | 26% | 102% | 100% | 100 |
| 5 | 38 | Chronic | 22 | 0–135/0–135 | 70–70/70–75 | 97% | 69% | 145% | >200% | 97 |
| 6 | 49 | Acute | 18 | −5–144/−5–145 | 75–75/75–80 | 91% | 73% | 47% | >200% | 100 |
| 7 | 48 | Acute | 38 | 0–144/1–135 | 70–75/70–65 | 101% | 162% | 100% | 46% | 100 |
| 8 | 48 | Acute | 40 | −2–118/1–128 | 42–73/44–68 | 90% | 132% | 87% | 85% | 95 |
| 9 | 51 | Chronic | 31 | −2–137/−2–135 | 81–74/78–76 | 111% | 103% | 86% | 30% | 98 |
| 10 | 46 | Chronic | 24 | 3–132/1–133 | 53–80/50–74 | 91% | 113% | 98% | 105% | 100 |
| 11 | 53 | Acute | 16 | 0–135/0–135 | 75–90/75–85 | 109% | 67% | 92% | 47% | 100 |
| 12 | 55 | Chronic | 26 | −17–150/−15–150 | 80–85/75–80 | 113% | 81% | 50% | 24% | 100 |
| 13 | 60 | Chronic | 53 | 5–137/−1–137 | 75–67/75–75 | 117% | 109% | 99% | 109% | 100 |
| 14 | 36 | Revision | 53 | 15–125/5–130 | 65–60/65–65 | 43% | 41% | 56% | 39% | 81 |
| 15 | 48 | Acute | 30 | 2–134/8–138 | 54–81/60–79 | 117% | 100% | 73% | 18% | 98 |
| 16 | 49 | Acute | 42 | −4–137/−3–141 | 64–77/74–84 | 105% | 99% | 69% | 118% | 100 |
| 17 | 55 | Acute | 33 | 15–135/20–135 | 75–50/75–60 | 98% | 73% | 69% | 10% | 97 |
| 18 | 41 | Acute | 32 | 0–130/0–135 | 70–70/70–80 | 84% | 91% | 95% | 82% | 100 |
| 19 | 50 | Acute | 15 | 0–150/0–140 | 75–55/75–75 | 118% | 138% | 162% | 123% | 100 |
| 20 | 54 | Acute | 28 | −5–137/−5–130 | 50–70/60–70 | 78% | 137% | 55% | 15% | 97 |
| 21 | 53 | Acute | 15 | −15–140/−5–140 | 70–65/65–75 | 110% | 99% | 89% | 56% | 100 |
| 22 | 52 | Acute | 29 | −5–135/14–137 | 75–90/65–80 | 114% | 81% | 158% | 70% | 98 |
| 23 | 55 | Acute | 37 | 2–136/2–137 | 52–74/55–86 | 110% | 124% | 96% | 67% | 98 |
| 24 | 46 | Acute | 50 | 3–133/−2–134 | 90–75/90–83 | 101% | 75% | 118% | 85% | 97 |
| 25 | 62 | Acute | 28 | −3–129/−1–121 | 63–68/56–72 | 97% | 82% | 113% | 106% | 100 |
| 26 | 58 | Acute | 32 | −6–131/−7–126 | 70–76/71–75 | 106% | 73% | 87% | 86% | 99 |
| 27 | 47 | Chronic | 13 | −3–131/−6–132 | 70–74/70–80 | 100% | 87% | 98% | >200% | 100 |
aNegative values denote hyperextension
Using the conversion factors generated from the control group, strength and endurance deficits, range of motion, and subjective outcomes comparing three subgroups are reported in Table 2. Compared with uninjured contralateral extremities, operative extremities had −2% flexion strength deficit and a −1% supination strength deficit. Supination endurance was also restored when comparing the operative extremity to the other side (endurance deficits of −1% for work, −49% for distance, and −21% for time). There was a slight loss of flexion endurance when comparing sides (endurance deficits of 5% for work, 5% for distance, and 12% for time).
Table 2.
Statistical analysis of subjective and objective measures between subgroups.
| Variable | Dominant | Non-dominant | P value | Acute | Chronic | P value | Work comp | Non-work comp | P value |
|---|---|---|---|---|---|---|---|---|---|
| Number | 14 | 13 | 17 | 10 | 19 | 8 | |||
| Age (years) | 48.4 years | 51.9 years | 50.0 years | 50.1 years | 51.7 years | 46.3 years | |||
| Dom/nondom | n/a | n/a | 9/8 | 5/5 | 9/10 | 4/4 | |||
| Acute/chronic | 9/5 | 8/5 | n/a | n/a | 13/6 | 4/4 | |||
| Interval | 1.8 months | 1.4 months | 15.5 days | 3 months | 1.4 months | 1.5 months | |||
| Follow-up | 28.9 months | 28.6 months | 28.9 months | 28.4 months | 27.6 months | 30.6 months | |||
| Workman’s comp | 4 | 4 | 4 | 4 | n/a | n/a | |||
| Strength | |||||||||
| Flexion deficit | 0.08 ± 0.19 | −0.12 ± 0.09 | 0.0003 | −0.03 ± 0.15 | 0.01 ± 0.22 | 0.7955 | −0.04 ± 0.15 | 0.04 ± 0.23 | 0.4254 |
| Supination deficit | −0.22 ± 0.44 | 0.22 ± 0.16 | 0.0063 | −0.01 ± 0.39 | 0 ± 0.44 | 0.9903 | −0.05 ± 0.43 | 0.11 ± 0.30 | 0.3398 |
| Endurance | |||||||||
| Flexion deficit | |||||||||
| Work | 0.05 ± 0.30 | 0.05 ± 0.36 | 0.9145 | 0.13 ± 0.26 | −0.09 ± 0.38 | 0.0953 | 0.06 ± 0.33 | 0.03 ± 0.32 | 0.7060 |
| Distance | 0.005 ± 0.30 | 0.10 ± 0.39 | 0.4365 | 0.13 ± 0.32 | −0.09 ± 0.35 | 0.1909 | 0.08 ± 0.37 | −0.02 ± 0.26 | 0.3135 |
| Time | 0.02 ± 0.40 | 0.23 ± 0.39 | 0.1506 | 0.20 ± 0.42 | −0.02 ± 0.34 | 0.0719 | 0.15 ± 0.43 | 0.04 ± 0.33 | 0.3006 |
| Supination deficit | |||||||||
| Work | −0.93 ± 2.88 | −0.01 ± 0.72 | 0.9430 | −0.76 ± 2.52 | −0.02 ± 1.26 | 0.1406 | −0.83 ± 2.48 | 0.32 ± 0.46 | 0.1323 |
| Distance | −0.26 ± 1.85 | −0.16 ± 0.64 | 0.0969 | −0.53 ± 1.65 | 0.32 ± 0.37 | 0.1179 | −0.38 ± 1.58 | 0.18 ± 0.60 | 0.2539 |
| Time | −1.22 ± 3.31 | −0.02 ± 0.70 | 0.7832 | −0.99 ± 2.97 | −0.06 ± 1.09 | 0.3659 | −0.99 ± 2.87 | 0.18 ± 0.55 | 0.2880 |
| Range of motion | |||||||||
| Flexion-extension | −0.71 ± 8.79 | 2.62 ± 5.82 | 0.1498 | 3.06 ± 6.79 | −2.80 ± 7.70 | 0.0563 | 1.37 ± 6.46 | −0.25 ± 10.15 | 0.5221 |
| Pronation–supination | −5.86 ± 11.18 | −0.38 ± 8.25 | 0.1066 | −5.35 ± 9.33 | 0.40 ± 10.77 | 0.0498 | −3.84 ± 9.17 | −1.75 ± 12.57 | 0.9065 |
| Pain | |||||||||
| Worst | 2.46 ± 2.91 | 0.15 ± 0.43 | 0.0227 | 1.71 ± 2.40 | 0.75 ± 2.37 | 0.1091 | 1.18 ± 2.21 | 1.75 ± 2.90 | 0.7163 |
| Resting | 0.25 ± 0.58 | 0.04 ± 0.14 | 0.4037 | 0.21 ± 0.53 | 0.05 ± 0.16 | 0.6319 | 0.16 ± 0.50 | 0.12 ± 0.23 | 0.5583 |
| Lifting | 1.89 ± 3.13 | 0.77 ± 1.18 | 0.7319 | 1.32 ± 2.11 | 1.40 ± 3.00 | 0.6927 | 0.74 ± 1.73 | 2.81 ± 3.26 | 0.0342 |
| Repeated activity | 1.61 ± 2.59 | 0.42 ± 0.84 | 0.3252 | 0.94 ± 1.81 | 1.20 ± 2.41 | 0.8361 | 0.82 ± 1.74 | 1.56 ± 2.60 | 0.3598 |
| Night | 0.18 ± 0.46 | 0.04 ± 0.14 | 0.6059 | 0.09 ± 0.26 | 0.15 ± 0.47 | 1.0000 | 0.05 ± 0.23 | 0.25 ± 0.54 | 0.1404 |
| Satisfaction | 9.36 ± 1.06 | 9.27 ± 1.96 | 0.5658 | 9.53 ± 0.74 | 8.95 ± 2.36 | 0.6802 | 9.79 ± 0.54 | 8.19 ± 2.43 | 0.0083 |
NS not significant *significant p values
Seventeen patients were repaired acutely (less than 4 weeks) and nine patients were fixed after 4 weeks. The average time from injury to surgery was 15.5 days in the acute group (range 5–27 days) and 3 months in the chronic group (range 6 weeks to 6 months). All chronic repairs were done through a single incision without the need for graft augmentation. There was no significant difference in flexion strength, flexion endurance, supination strength or supination endurance between the two groups. Acute repairs lost 5° of forearm rotation compared to a gain of 0.40° in the chronic group, although this was not clinically significant. There was no significant difference between the two groups in flexion or extension range of motion.
Fourteen patients injured their dominant extremity (average age 48.4 years) compared to 13 patients who injured their non-dominant extremity (average age 51.9 years). Operative dominant extremities demonstrated significantly greater deficits in maximal elbow flexion strength compared with operative non-dominant extremities (p = 0.0003). Patients with repaired dominant extremities also reported significantly more pain (p = 0.0227). There were no significant differences observed when comparing endurance between the two sides.
There were eight patients who had filed a workers’ compensation claim compared to 19 patients who had not. The average age of those involved in worker’s compensation was 46.3 years compared to 51.7 years without worker’s compensation. Patients receiving worker’s compensation reported more pain with heavy lifting and were less satisfied with their outcome (8.19 VAS versus 9.79 VAS in non worker’s comp, p = 0.0083). However, there was no significant difference in the two groups in regard to objective strength or range of motion measurements.
There was one re-rupture requiring revision distal biceps tendon repair. Six patients (22%) reported decreased sensation in the distribution of the lateral antebrachial cutaneous nerve, of which two resolved at the time of final evaluation. Four of the six occurred in repairs of chronic injuries. One patient reported occasional cramping of the operative extremity and one patient reported cold intolerance.
Discussion
There have been many described techniques for distal biceps tendon repair. Historically, authors have favored a two-incision approach popularized by Boyd and Anderson [5]. This technique relies on fixation of the distal biceps tendon into a trough at the radial tuberosity with sutures tied over a bony bridge. This technique can be associated with nerve injury [17], heterotopic ossification [9, 17, 22, 27], and radioulnar synostosis [22, 27, 29]. A single-incision anterior approach with the use of suture anchors or interference screw fixation has become popular in recent years [3, 15, 24, 25, 33]. However, there are technical challenges associated with knot-tying and tendon tensioning in a muscular forearm or with chronic repairs.
Repair of distal biceps tendon ruptures with an EndoButton was first described by Bain for use in a single-incision anterior approach [2]. Advantages include less technical difficulty in securing fixation through a single anterior incision, a bone socket to maximize healing, and strong fixation allowing early motion. The higher load to failure of the EndoButton technique has been shown in several studies [18, 26, 34] and is associated with cortical bone based fixation through the dorsal aspect of the radius. The EndoButton has been shown to have higher load to failure than interference screws, suture anchors, and transosseus tunnels [6, 19, 34]. Strong initial fixation of the biceps tendon to the radial tuberosity bone socket allows for aggressive early range of motion. In our study, all patients regained fully functional range of motion.
Clinical results of EndoButton repair are also encouraging [2, 11, 28, 30]. Bain et al. [2] reported satisfactory outcomes with early active mobilization in all 12 patients with no complications. All patients regained grade 5 strength and returned to full activities. Peeters and colleagues [28] recently reported on 26 patients who underwent EndoButton repair of distal biceps tendon ruptures. Average flexion strength recovery was 80% and supination strength recovery was 91%. Greenberg et al. [11] reported on 14 patients at an average follow-up of 20 months. Strength testing demonstrated return of 97% flexion and 82% supination strength when compared to the non-operative arm. Ranelle [30] reported on 11 men and one woman who underwent repair with an EndoButton. All patients returned to their prior activity level with no complications. Our study demonstrated similar results with 26 of 27 patients returning to their previous employment and activity level. Using conversion factors generated from eight control subjects, there was only a 1% supination strength deficit and a 2% flexion strength deficit when comparing the operative extremity to the uninjured arm.
There have been few reports of outcomes after chronic distal biceps tendon repairs. Most techniques advocate the use of a tissue graft including semitendinosis tendon [13, 14, 35], achilles tendon [8, 32], flexor carpi radialis tendon [23], and fascia lata [16]. Our study reports nine patients with a chronic rupture of the distal biceps tendon (mean of 3 months from injury). Our data show that repair can be performed without the use of allograft or autograft tendon augmentation in chronic ruptures up to 6 months old. We found complete restoration of motion, strength and endurance when compared to the non-operative extremity. We also suggest that patients will regain full motion even if the repair is completed with the elbow in a significant amount of flexion because of the biceps muscle elasticity. Although further studies are in progress to examine the outcomes of chronic repairs performed without graft augmentation, there are obvious advantages of avoiding the use of allograft or autograft, which include the lack of autograft donor site morbidity and no risk of allograft disease transmission.
The effect of hand dominance on the outcome following repair of distal biceps ruptures has rarely been addressed. Agins and colleagues used a two-incision technique to demonstrate that repaired non-dominant extremities were 46% weaker in flexion following repair when compared to the uninjured dominant extremity [1]. Leighton et al. [22] reviewed nine patients and examined the role of hand dominance on outcome. Three dominant extremities demonstrated complete return of strength and endurance in both flexion and supination. However, repair in six non-dominant extremities demonstrated deficits in flexion strength, flexion endurance, and spination strength. D’Alessandro et al. noted weakness with flexion endurance in the dominant extremity and loss of supination endurance in non-dominant extremities [7]. The role of hand dominance in strength and endurance recovery and postoperative pain may alter the pre-operative discussion regarding expected outcomes.
Lateral antebrachial cutaneous (LABC) sensory deficit may be due to the increased dissection that is required to mobilize the tendon in chronic injuries or secondary to increased tension on the repaired tendon stretching the LABC nerve. Patients should be warned about this potential complication when repair of a chronic rupture is performed.
The weaknesses of this study include that it is retrospective. Additionally, only 27 patients were available for follow-up examination and strength testing, although this is still the largest study of this technique to date. Pre-operative DASH scores, along with pre-operative strength and endurance testing, could have provided additional information of interest. While providing little additional insight into those patients with an acute rupture, such data could prove beneficial when examining those with chronic injuries.
EndoButton fixation of distal biceps tendon ruptures is a safe and effective method of treatment with excellent clinical results. Patients demonstrate full recovery of range of motion and near complete return of strength and endurance with a low complication rate. This technique is ideal for repairing chronic ruptures without the need for allograft or autograft augmenation.
Acknowledgment
The authors would like to thank Joshua A. Johnston, MD for assistance with data collection.
Conflict of Interest The authors declare that they have no conflict of interest.
References
- 1.Agins HJ, Chess JL, Hoekstra DV, et al. Rupture of the distal insertion of the biceps brachii tendon. Clin Orthop. 1988;234:34–38. [PubMed] [Google Scholar]
- 2.Bain GI, Prem H, Heptinstall RJ, et al. Repair of distal biceps tendon rupture: a new technique using the EndoButton. J Shoulder Elbow Surg. 2000;9:120–126. doi: 10.1016/S1058-2746(00)90040-5. [DOI] [PubMed] [Google Scholar]
- 3.Bain GI. Repair of distal biceps tendon avulsion with the EndoButton technique. Tech Shoulder Elbow Surg. 2002;3:96–101. doi: 10.1097/00132589-200206000-00005. [DOI] [Google Scholar]
- 4.Baker BE, Bierwagen D. Rupture of the distal tendon of the biceps brachii: operative versus non-operative treatment. J Bone Jt Surg. 1985;67-A:414–417. [PubMed] [Google Scholar]
- 5.Boyd HB, Anderson LD. A method for reinsertion of the distal biceps brachii tendon. J Bone Jt Surg. 1961;43-A:1041–1043. [Google Scholar]
- 6.Chavan PR, Duquin TR, Bisson LJ. Repair of the ruptured distal biceps tendon: a systematic review. Am J Sports Med. 2008;36:1618–1624. doi: 10.1177/0363546508321482. [DOI] [PubMed] [Google Scholar]
- 7.D’Alessandro DF, Shields CL, Jr, Tibone JE, et al. Repair of distal biceps tendon ruptures in athletes. Am J Sports Med. 1993;21:114–119. doi: 10.1177/036354659302100119. [DOI] [PubMed] [Google Scholar]
- 8.Darlis NA, Sotereanos DG. Distal biceps tendon reconstruction in chronic ruptures. J Shoulder Elbow Surg. 2006;15:614–619. doi: 10.1016/j.jse.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 9.Failla JM, Amadio PC, Morrey BF, et al. Proximal radioulnar synostosis after repair of distal biceps brachii rupture by the two-incision technique: a report of four cases. Clin Orthop. 1990;253:133–136. [PubMed] [Google Scholar]
- 10.Gilchreest EL. The common syndrome of rupture, dislocation and elongation of the long head of the biceps brachii: an analysis of one hundred cases. Surg Gynecol Obstet. 1934;58:322–340. [Google Scholar]
- 11.Greenberg JA, Fernandez JJ, Wang T, et al. EndoButton-assisted repair of distal biceps tendon ruptures. J Shoulder Elbow Surg. 2003;12:484–490. doi: 10.1016/S1058-2746(03)00173-3. [DOI] [PubMed] [Google Scholar]
- 12.Gregory T, Roure P, Fontes D. Repair of distal biceps tendon rupture using a suture anchor. Am J Sports Med. 2009;37(3):506–511. doi: 10.1177/0363546508326985. [DOI] [PubMed] [Google Scholar]
- 13.Hallam P, Bain GI. Repair of chronic distal biceps tendon ruptures using autologous hamstring graft and the EndoButton. J Shoulder Elbow Surg. 2004;13:648–651. doi: 10.1016/j.jse.2004.01.032. [DOI] [PubMed] [Google Scholar]
- 14.Hang DW, Bach BR, Jr, Bojchuk J. Repair of chronic distal biceps brachii tendon rupture using free autogenous semitendinosus tendon. Clin Orthop. 1996;323:188–191. doi: 10.1097/00003086-199602000-00025. [DOI] [PubMed] [Google Scholar]
- 15.Idler CS, Montgomery WH, Lindsey DP, et al. Distal biceps tendon repair: a biomechanical comparison of intact tendon and 2 repair techniques. Am J Sports Med. 2006;34:968–974. doi: 10.1177/0363546505284185. [DOI] [PubMed] [Google Scholar]
- 16.Kaplan FT, Rokito AS, Birdzell MG, et al. Reconstruction of chronic distal biceps tendon rupture with use of fascia lata combined with a ligament augmentation device: a report of 3 cases. J Shoulder Elbow Surg. 2002;11:633–636. doi: 10.1067/mse.2002.126102. [DOI] [PubMed] [Google Scholar]
- 17.Kelly EW, Morrey BF, O’Driscoll SW. Complications of repair of the distal biceps tendon with the modified two-incision technique. J Bone Jt Surg. 2000;82-A:1575–1581. doi: 10.2106/00004623-200011000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Kettler M, Lunger J, Kuhn V, et al. Failure strengths in distal biceps tendon repair. Am J Sports Med. 2007;35:1544–1548. doi: 10.1177/0363546507300690. [DOI] [PubMed] [Google Scholar]
- 19.Kettler M, Tingart MJ, Lunger J, et al. Reattachment of the distal tendon of biceps: factors affecting the failure strength of the repair. J Bone Joint Surg Br. 2008;90:103–106. doi: 10.1302/0301-620X.90B1.19285. [DOI] [PubMed] [Google Scholar]
- 20.King J, Bollier M. Repair of distal biceps tendon ruptures using the EndoButton. J Am Acad Orthop Surg. 2008;16:490–494. doi: 10.5435/00124635-200808000-00008. [DOI] [PubMed] [Google Scholar]
- 21.King GJW, Richards RR, Zuckerman JD, et al. A standardized method for assessment of elbow function. J Shoulder Elbow Surg. 1999;8:351–354. doi: 10.1016/S1058-2746(99)90159-3. [DOI] [PubMed] [Google Scholar]
- 22.Leighton MM, Bush-Jopseph CA, Bach BR., Jr Distal biceps brachii repair: results in dominant and nondominant extremities. Clin Orthop. 1995;317:114–121. [PubMed] [Google Scholar]
- 23.Levy HJ, Mashoof AA, Morgan D. Repair of chronic ruptures of the distal biceps tendon using flexor carpi radialis tendon graft. Am J Sports Med. 2000;28:538–540. doi: 10.1177/03635465000280041501. [DOI] [PubMed] [Google Scholar]
- 24.Limpisvasti O, Singer DI. Single-inicision suture anchor repair of distal biceps tendon rupture. Tech Hand Up Extrem Surg. 2003;7:82–86. doi: 10.1097/00130911-200309000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Linter S, Fischer T. Repair of distal biceps tendon using suture anchors and an anterior approach. Clin Orthop. 1996;322:116–119. [PubMed] [Google Scholar]
- 26.Mazzocca AD, Burton KJ, Romero AA, et al. Biomechanical evaluation of 4 techniques of distal biceps brachii tendon repair. Am J Sports Med. 2007;35:252–258. doi: 10.1177/0363546506294854. [DOI] [PubMed] [Google Scholar]
- 27.Morrey BF, Askew LJ, An KN, et al. Rupture of the distal tendon of the biceps brachii: a biomechanical study. J Bone Jt Surg. 1985;67-A:418–421. [PubMed] [Google Scholar]
- 28.Peeters T, Ching-Soon NG, Jansen N, et al. Functional outcome after repair of distal biceps tendon ruptures using the EndoButton technique. J Shoulder Elbow Surg. 2009;18:283–287. doi: 10.1016/j.jse.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 29.Ramsey ML. Distal biceps tendon injures: diagnosis and management. J Am Acad Orthop Surg. 1999;7:199–207. doi: 10.5435/00124635-199905000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Ranelle RG. Use of the EndoButton in repair of the distal biceps brachii tendon. Proc (Baylor Univ Med Cent) 2007;20:235–236. doi: 10.1080/08998280.2007.11928294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rantanen J, Orava S. Rupture of the distal biceps tendon: a report of 19 patients treated with anatomic reinsertion, and a meta-analysis of 147 cases found in the literature. Am J Sports Med. 1999;27:128–132. doi: 10.1177/03635465990270020201. [DOI] [PubMed] [Google Scholar]
- 32.Sanchez-Sotelo J, Morrey BF, Adams RA, et al. Reconstruction of chronic ruptures of the distal biceps tendon with use of an Achilles tendon allograft. J Bone Jt Surg. 2002;84-A:999–1005. doi: 10.2106/00004623-200206000-00015. [DOI] [PubMed] [Google Scholar]
- 33.Sotereanos DG, Pierce TD, Varitimidis SE. A simplified method for repair of distal biceps tendon ruptures. J Shoulder Elbow Surg. 2000;9:227–233. doi: 10.1016/S1058-2746(00)90060-0. [DOI] [PubMed] [Google Scholar]
- 34.Sprang JT, Weinhold PS, Karas SG. A biomechanical comparison of EndoButton versus suture anchor repair of distal biceps tendon injuries. J Shoulder Elbow Surg. 2006;15:509–514. doi: 10.1016/j.jse.2005.09.020. [DOI] [PubMed] [Google Scholar]
- 35.Wiley WB, Noble JS, Dulaney TD, et al. Late reconstruction of chronic distal biceps tendon ruptures with a seitendinosis autograft technique. J Shoulder Elbow Surg. 2006;15:440–444. doi: 10.1016/j.jse.2005.08.018. [DOI] [PubMed] [Google Scholar]