Abstract
While isolated limb injuries often lead to suspicion for and treatment of compartment syndrome, multi-limb compartment syndrome induced by a systemic disease is a rare entity, in which lack of immediate diagnosis can have catastrophic consequences to the patient. We present a patient with idiopathic systemic capillary leak syndrome (SCLS) resulting in compartment syndrome in all four extremities. Treatment required bilateral hand, forearm, calf, and thigh fasciotomies. Presenting symptoms included pain in all four extremities, malaise, and confusion. Laboratory data included polycythemia, hypoalbuminemia, leukocytosis, and elevated creatinine, but not a monoclonal spike on serum electrophoresis as is common in SCLS. Thus, when faced with clinical evidence of multiple extremity compartment syndrome, the surgeon should consider systemic disorders, such as SCLS, and aggressively treat the compartment syndrome as well as the underlying disease.
Keywords: Systemic capillary leak syndrome, Compartment syndrome
Introduction
Compartment syndrome is commonly caused by local insult to the limb or, rarely, systemic disease. In most cases, a clear mechanism can be identified during the initial evaluation. Common etiologies include crush or blast injuries, reperfusion or vascular injury, fracture, burn, or intravenous (IV) catheter infiltration. Some of the more obscure causes of compartment syndrome include systemic disorders such as nephrotic syndrome, hypothyroidism, acute rhabdomyolysis, viral or drug-induced myositis, and systemic capillary leak syndrome (SCLS). SCLS is a rare disorder of unknown etiology characterized by episodes of extreme capillary hyperpermeability leading to large fluid shifts from the intravascular to the interstitial space. Patients present with hypotension, hypoalbuminemia, hemoconcentration, acute renal failure, and edema. In the extremities, this profound capillary leak and edema can lead to compartment syndrome and vascular compromise. Here, we present a case of SCLS in a patient requiring fasciotomies in all four extremities. Although there has been one reported case of SCLS leading to fasciotomy of bilateral forearms and lower extremities, this is the first case to also require fasciotomies of bilateral hands and thighs.
Case Report
A previously healthy 32-year-old right-hand dominant Hispanic male presented to the emergency center with complaints of diffuse pain in all four extremities beginning within the past day while working as a day laborer. Furthermore, he complained of malaise, dizziness, and confusion. His only significant medical history included hypertension and cocaine use. He gave no history of recent trauma, and no physical evidence of such could be identified. Clinically, he was hypovolemic and tachycardic. Laboratory studies demonstrated an elevated hemoglobin and hematocrit, metabolic acidosis, hypoalbuminemia, and acute renal failure (Table 1). Initially diagnosed with possible polycythemia vera, he was admitted to the medical intensive care unit and a hematology consult was obtained. He received aggressive intravenous fluid therapy (10.5 L over 12 h) and a short course of vasopressors for hypotension. Phlebotomy was attempted but had to be abruptly stopped after 200 cc secondary to the patient’s sudden onset of chest pain. The consistency of the blood was noted to be highly viscous and dark in color.
Table 1.
Laboratory results at admission
| WBC | 36.5 |
| Hgb | 23.7 |
| Hct | 78.7 |
| Plt | 354 |
| Na | 134 |
| K | 4.3 |
| Cl | 97 |
| CO2 | 17.9 |
| BUN | 32 |
| Cr | 2.4 |
| Glucose | 185 |
| Protein | 3.6 |
| Albumin | 1.7 |
| T Bili | 0.5 |
| D Bili | 0.1 |
| AST | 27 |
| ALT | 63 |
| Alk phos | 55 |
| pH | 7.2 |
| pCO2 | 23.7 |
| pO2 | 121 |
| HCO3 | 9 |
| BE | −18 |
| Lactic acid | 8.9 |
The hematology team suggested an alternate diagnosis, given that polycythemia vera patients present in volume overload, not volume depletion. Following hydration with 10 L of crystalloid, the patient began to produce urine. However, he complained of more pain in his extremities and was noted to have tense forearms and calves. At this time, plastic hand surgery and orthopedic surgery consultations were obtained for possible compartment syndrome.
At the time of the evaluation, the patient’s fingers were found to be in a flexed position. The forearm, hand, and lower extremity compartments were tense and swollen bilaterally. He was hypertensive, tachycardic, tachypneic, anxious, and was subsequently intubated. Compartment pressures were measured in the volar and dorsal forearm as well as anterior and posterior calf compartments with both a Stryker needle and an arterial line setup which revealed pressures ranging from 50 to 85 mmHg.
The patient was taken to the operating room emergently where he underwent bilateral fasciotomies of the hands and forearms by the plastic surgery service and the calves and thighs by orthopedic surgery. At the time of surgery, all of the forearm compartments and the entire hand were clinically very tight. The superficial and deep flexor compartments were released via a Rowland’s incision including a carpal tunnel release. The extensor compartment and the mobile wad were released through a dorsal longitudinal incision. Two longitudinal incisions were made on the dorsum of the hand over the second and fourth metacarpals to release the interosseous compartments, and incisions were made over the thenar and hypothenar compartments for their release. Upon release, the muscle immediately bulged from within the fascia (Fig. 1). No frank necrotic muscle was seen; however, both forearms contained areas of dusky muscle in the deep flexor muscles with poor contracture upon stimulation with electrocautery. After release of all compartments, the skin was approximated loosely covering vital structures (Fig. 2), splints were placed, and the patient was returned to the intensive care unit.
Fig. 1.
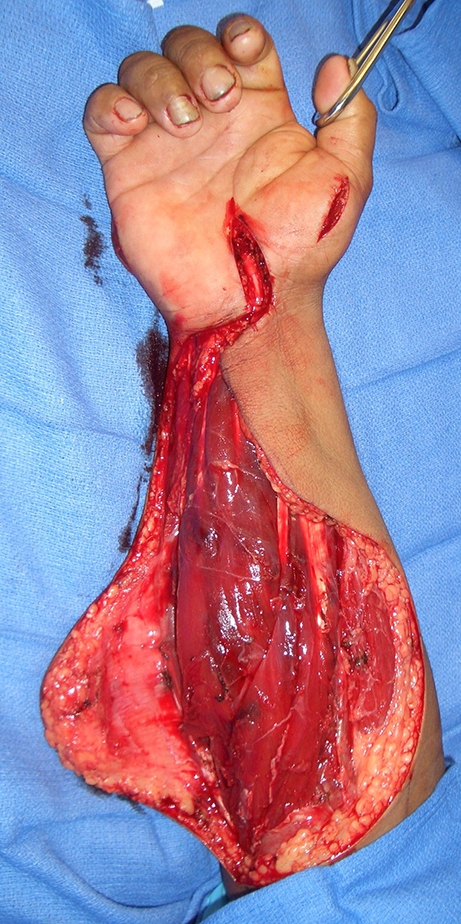
Intraoperative photograph after right forearm fasciotomy and carpal tunnel release
Fig. 2.

Intraoperative photograph after partial closure of right forearm fasciotomy wound to cover vital structures
The patient remained intubated for several days secondary to pulmonary edema. He developed fevers but repeated blood, urine, and sputum cultures were all negative. Computed tomography of the abdomen and pelvis revealed no cause of fever. His wounds remained clean without evidence of infection.
Hematology and infectious disease consults coordinated in order to determine the patient’s primary diagnosis. Serologies for Hantavirus, dengue fever, and Brucella were negative. A hepatitis panel was negative. HIV 1 and 2 tests were negative. Urine drug screen was negative. A JAK2 mutation, seen in the vast majority of patients with polycythemia vera, was not present. Serum protein electrophoresis was consistent with acute phase reaction, and a monoclonal spike was not seen. Following complete workup, the patient’s presentation was thought to be consistent with idiopathic systemic capillary leak syndrome.
One week after fasciotomy, the patient was taken back to the operating room for irrigation and debridement of the wounds and partial closure. No necrotic muscle was detected in the upper extremities; however, small foci of necrotic muscle in the calves were debrided by the orthopedic surgery service. Closure and skin grafting of the remainder of his wounds was completed 10 days later. Physical and occupational therapy was begun for range of motion and strength once his wounds were healed.
The patient was discharged home on hospital day 33. Six weeks after discharge, he is recovering well, ambulating without assistance, and has regained hand function sufficient for performing his activities of daily living. He is still in physical therapy and shows continued improvement in his strength and range of motion.
Discussion
While localized tissue trauma is often the cause of isolated compartment syndrome, systemic fluid shifts can cause increased compartment volumes and result in compartment syndrome in multiple limbs. These fluid shifts can occur due to increased capillary permeability and diffusion of solutes across different compartments. Increased capillary permeability can result from release of endogenous inflammatory mediators, such as histamine and prostaglandin or by exogenous endotoxins as in gram-negative bacterial sepsis. In contrast, several non-physiologic situations can promote fluid diffusion across a normal capillary membrane such as the sodium imbalance encountered with nephrotic syndrome.
Systemic capillary leak syndrome results in fluid shifts in an unknown manner. The syndrome was first described in 1960 by Clarkson [3], and while there are approximately 100 reported cases documented, the condition remains of unknown etiology.
SCLS Presentation
The disorder occurs in primarily healthy patients between the ages of 3 and 68 years with a slight male predominance [4]. It is a phenomenon characterized by recurring episodes of increased capillary permeability where up to 70% of the plasma volume and proteins up to 200,000 Da can be spilled into the extracellular space [4]. This hyperpermeable condition leads to the typical presenting findings of hypovolemia, hypotension, polycythemia, hypoalbuminemia, edema, and renal failure.
All patients who present with SCLS demonstrate signs and symptoms of shock and up to 80% have recurrent episodes of shock [4]. Flu-like prodromal symptoms including myalgias have been reported in about 50% of patients and other prodromal symptoms such as abdominal pain, nausea/vomiting, polydipsia, and dizziness have also been reported [4]. These patients develop significant edema which when involving the muscular compartments can lead to compartment syndrome in up to 24% of the cases [4].
It is not uncommon for patients to present with hemoglobin levels approaching 30 and hematocrit approaching 80. In fact, patients are not infrequently diagnosed and treated as if they have polycythemia vera [5]. Another contributor to the limb pain, swelling, and the renal failure is the high viscosity of the blood leading to low oxygen perfusion and possible microthrombi [9].
Most patients (82%) are found to have a monoclonal gammopathy on serum protein electrophoresis, usually IgG kappa [9]. It is unclear how this feature is linked to the pathophysiology of the condition as it has not been shown to be directly linked to the capillary pathology. The monoclonal spike is supportive, but not required for the diagnosis.
Pathophysiology of SCLS
Many have attempted to isolate a plasma protein responsible for the pathophysiology of the disease since Clarkson was able to cause hypotension in rats after he injected the plasma from a SCLS patient into the bloodstream. Of note, this study was not reproducible [2, 10]. Culprits have included leukotreines and CD8 cell receptors. In several studies, looking at the histology of the capillaries, muscle, and skin after autopsies, the only significant finding remains a single report of a thickened capillary basement membrane [8].
The increase in capillary permeability causes leakage of fluid into the interstitial spaces including the muscular compartments, leading to an elevation in intracompartmental pressure. This effect is thought to be exacerbated by the aggressive fluid resuscitation that the patients require. Perry et al. conjecture that the need for high-volume intravenous hydration alone cannot explain the development of compartment syndrome since the patients do not demonstrate any signs and symptoms of pulmonary edema at the time of the diagnosis [9]. Interestingly, the pulmonary capillaries seem to be relatively unaffected by the hyperpermeability which may explain why patients seem to develop pulmonary edema only after copious intravenous fluid administration [7]. Intravenous fluids are likely to exponentiate the development of the high compartment pressures. Under normal physiologic parameters, one can assume that approximately one third the volume of isotonic crystalloids remains within the intravascular space. In patients with capillary leak, the portion of fluids that remains intravascular can be expected to be even less.
Treatment
First, treating physicians must appropriately monitor the patients during resuscitation for signs and symptoms of developing compartment syndrome. At the minimum, the muscular compartments must be followed by serial examination. Continuous pressure monitoring has been used during the acute resuscitation period to track compartmental pressures and determine the need for fasciotomy. Since SCLS is a systemic disease, compartment syndrome may be seen in multiple limbs simultaneously, as was seen in our case. If the patient is non-responsive or intubated, measured compartment pressures exceeding 30 mmHg or within 30 mmHg of the diastolic pressure support the diagnosis and help make the decision for operative release of the compartments. There has only been one other report in the literature of simultaneous compartment syndrome in all four limbs, which was also in a patient with SCLS, although only bilateral forearm and calf fasciotomies were needed in that patient [6].
Once the patient has stabilized and begins to recruit the fluid back from the interstitial space, the patient becomes hypervolemic and the treatment becomes one of treating fluid overload by diuresis or dialysis if renal function has not recovered. Steroids and plasmapheresis have been used by some for treatment of the acute phase with limited success [1].
Long-term treatment to prevent future episodes consists of theophylline and terbutaline [1]. Though some medication regimens have been shown to decrease the frequency and severity of the attacks, the long-term survival from this condition as reported in the literature is quite poor, with an estimated 5-year mortality rate ranging from 30% to 76% [7]. It is imperative that patients with this condition be informed of the likelihood of recurrent episodes and how to recognize them early in order to be appropriately treated.
Patients in whom a monoclonal gammopathy is identified must also be aware that they are at increased risk for development of leukemia or multiple myeloma in the future and accordingly should be followed by a hematologist. These patients have up to a 30% risk of developing multiple myeloma over the next 25 years [1].
Our patient presented with all classic findings for systemic capillary leak syndrome including hypovolemia, hypotension, polycythemia, hypoalbuminemia, interstitial edema, and renal failure. The combination of severe capillary leak along with large volume intravenous fluid resuscitation led to the development of compartment syndrome in all four extremities. Although his serum electrophoresis did not show a monoclonal spike, this is not required to make the diagnosis and other possible causes were ruled out, making SCLS the most likely etiology. Timely diagnosis of compartment syndrome led to fasciotomies in all four extremities leading to preservation of limb function and prevention of the systemic consequences of muscle necrosis.
Conclusion
Evaluation of patients with possible compartment syndrome must include determination of the etiology. While the cause of compartment syndrome is usually easily ascertained, when faced with a patient with multiple extremity compartment syndrome and/or no identifiable cause for compartment syndrome, systemic capillary leak syndrome should be considered. These patients commonly present with hypovolemic shock, polycythemia, hypoalbuminemia, edema, and renal failure. A serum electrophoresis should be obtained to determine presence of monoclonal gammopathy as this may help confirm the diagnosis. All patients with SCLS should be followed for possible development of hematologic malignancies in the future. Although systemic capillary leak syndrome is rare, it is essential that hand surgeons be aware of it as a potential cause of compartment syndrome.
Acknowledgments
Conflicts of interest None of the authors has any financial interest to declare related to the content of this article.
References
- 1.Amoura Z, Papo T, Ninet J, et al. Systemic capillary leak syndrome: report on 13 patients with special focus on course and treatment. Am J Med. 1997;103:514–519. doi: 10.1016/S0002-9343(97)00272-6. [DOI] [PubMed] [Google Scholar]
- 2.Atkinson JP, Waldmann TA, Stein SF, Gelfand JA, Macdonald WJ, Heck LW, et al. Systemic capillary leak syndrome and monoclonal IgG gammopathy; studies in a sixth patient and a review of the literature. Medicine (Baltimore) 1977;56(3):225–239. doi: 10.1097/00005792-197705000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Clarkson B, Thompson D, Horwith M, Luckey EH. Cyclical edema and shock due to increased permeability. Am J Med. 1960;29:193–216. doi: 10.1016/0002-9343(60)90018-8. [DOI] [PubMed] [Google Scholar]
- 4.Dhir V, Arya V, Malav IC, Suryanarayanan BS, Gupta R, Dey AB. Idiopathic systemic capillary leak syndrome (SCLS): case report and systematic review of cases reported in the last 16 years. Intern Med. 2007;46:899–904. doi: 10.2169/internalmedicine.46.6129. [DOI] [PubMed] [Google Scholar]
- 5.Doubek M, Brychtova Y, Tomiska M, Mayer J. Idiopathic systemic capillary leak syndrome misdiagnosed and treated as polycythemia vera. Acta Haematol. 2005;113:150–151. doi: 10.1159/000083455. [DOI] [PubMed] [Google Scholar]
- 6.Dowden AM, Rullo OJ, Aziz N, Fazano MB, Chatila T, Ballas ZK. Idiopathic systemic capillary leak syndrome: novel therapy for acute attacks. J Allergy Clin Immunol. 2009;124(5):1111–1113. doi: 10.1016/j.jaci.2009.06.043. [DOI] [PubMed] [Google Scholar]
- 7.Kawabe S, Saeki T, Yamazaki H, Nagai M, Aoyagi R, Miyamura S. Systemic capillary leak syndrome. Intern Med. 2002;32:364–366. doi: 10.2169/internalmedicine.41.211. [DOI] [PubMed] [Google Scholar]
- 8.Navarro C, Garcia-Bragado F, Lima J, Fernandez JM. Muscle biopsy findings in systemic capillary leak syndrome. Hum Pathol. 1990;21:297–301. doi: 10.1016/0046-8177(90)90230-3. [DOI] [PubMed] [Google Scholar]
- 9.Perry J, Balasubramanian S, Imray C. Systemic capillary leak syndrome resulting in compartment syndrome and the requirement for a surgical airway. Anesthesia. 2009;64(6):679–682. doi: 10.1111/j.1365-2044.2009.05891.x. [DOI] [PubMed] [Google Scholar]
- 10.Zhang W, Evan PW, Lachman PJ. The paraproteins in systemic capillary leak syndrome. Clin Exp Immunol. 1993;93(3):424–429. doi: 10.1111/j.1365-2249.1993.tb08195.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


