Abstract
Melorheostosis of the hand is rare. We report a 28-year-old woman with persistent pain associated with a slowly growing mass on the dorsum of the right thumb. The radiographs, computed tomography, and magnetic resonance imaging were used to examine characteristic of melorheostosis involving the trapezium bone, first metacarpal, and proximal phalange. The lesions underwent a surgical debulking of the hyperostotic cortex and a cortical fenestration.
Keywords: Melorheostosis, Hand
Introduction
The melorheostosis was first described by the two French neurologists Leri and Joanny in 1922 [13]. It is a rare, benign, non-familial condition of hyperostosis of the cortical bone [11]. Its name comes from the Greek “melos”, meaning limb, and “rhein”, meaning to flow. It usually involves the periosteum and endosteum of diaphyseal cortical bone and can be associated with various soft tissue changes. Based on the extension of the lesion bone, involvement may be monostotic, polyostotic, or monomelic. Patients with melorheostosis may have associated cutaneous and soft tissue lesions such as vascular malformation, neurofibromatosis, arterial aneurysms, linear scleroderma, tuberous sclerosis, hemangiomas, and focal subcutaneous fibrosis [2]. The age of presentation ranges from the neonatal period to the elderly. The peak age of presentation is between the ages 5 and 20, and approximately half of the cases are detected by the age of 20 [9]. There are no gender differences in the reported cases or any difference with respect to ethnicity, suggesting increase risk in certain populations [9]. Although the etiology of this disease is unknown, two main theories have been proposed. The “classic theory” claims the presence of an early embryonic infection of a sensory nerve inducing changes in the respective sclerotome. The second is the concept of “Mosaicism”, which better explains the sporadic occurrence, the asymmetric “segmental” pattern with variable extent of involvement and equal gender ratio of the disease [9].
Case Report
E.P.A. is a 28-year-old woman, married, a saleswoman, and a Brazilian, who presented to the office with a 3-year history of persistent pain in the right thumb. The pain was relieved by use of non-steroidal anti-inflammatory agents, but had become severe during the last 4 months. She referred a slowly growing mass on the dorsum of the right thumb too.
The examination of the musculoskeletal system showed a limitation of the last degrees of the supination of the right forearm. There was a full range of motion in wrist, all joints of the fingers, and thumb, and there weren’t contractures or rotational deformity. Continuous on examination, a hard mass approximately 1 × 2 cm was identified over the proximal phalange of the right thumb. This region was firm and very painful to palpation. Superficially, there was no evidence of discoloration, skin thickening, or a local increase in temperature.
There wasn’t atrophy of the muscles, and sensibility in the fingers was normal.
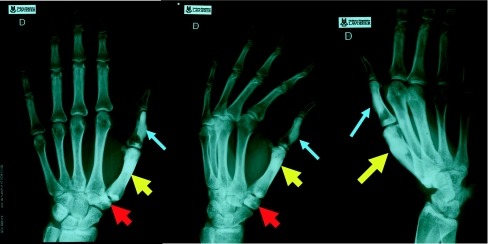
Conventional radiographs of the right hand (Fig. 1) showed cortical hyperostosis of the first metacarpal, extending over a length of 4 cm, and the dorsal side of the proximal phalange of the right thumb, extending for approximately 3.5 cm, and a sclerosis of the trapezium bone. The dense hyperostosis encroached into the medulla of the involved bones and showed a segmental distribution corresponding to the sixth cervical sclerotomes.
Fig. 1.
Radiograph of the right hand reveals sclerosis in the trapezium bone (red arrow), the first metacarpal (yellow arrow), and the proximal phalange (blue arrow) of the right thumb
Laboratory tests, including complete blood count, erythrocyte sedimentation rate, C-reactive protein, serum phosphorus, alkaline phosphatase, and calcium level were normal.
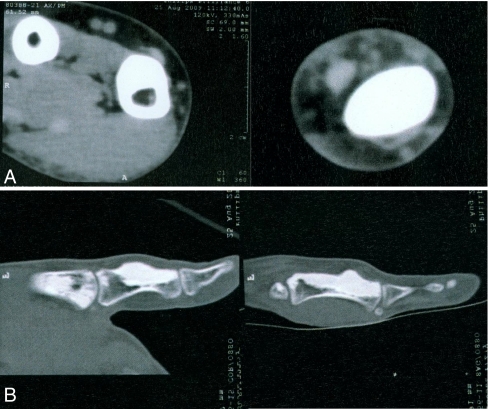
Computed tomography (CT) scans showed a high-attenuation undulating cortical hyperostosis involving the ulnar side of the first metacarpal and dorsal aspects of the proximal phalange of the thumb (Fig. 2)
Fig. 2.
CT. a Coronal images of the first metacarpal. Hyperostotic bone almost totally occupies the medullary cavity of the proximal phalange. b Longitudinal images of the first metacarpal and proximal phalange
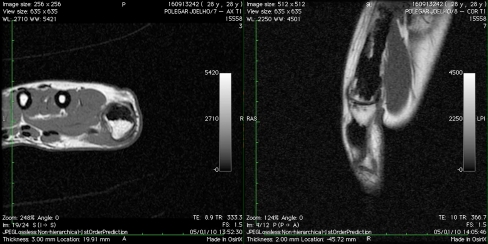
With regard to surgical intervention a magnetic resonance imaging (MRI) of the right thumb and wrist was performed for further evaluation of osseous and possible tissue abnormalities (Fig. 3). The classical cortical hyperostosis characteristic of melorheostosis demonstrated a signal void on all pulse sequences. No soft reactive soft tissue inflammation, tissue masses, or tumors were demonstrated.
Fig. 3.
MRI. Hyperostosis characteristic of melorheostosis, demonstrated on all pulse sequences
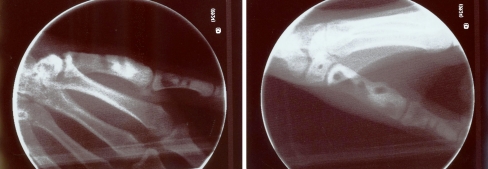
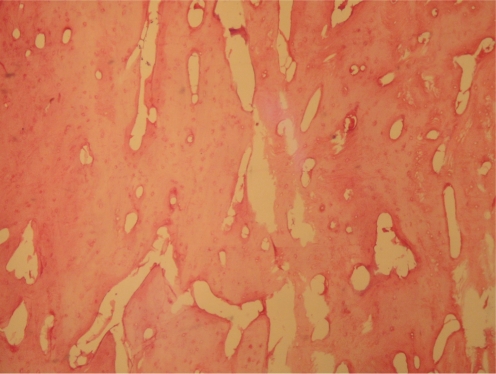
During the operation, the periosteum was found to be thickened and the underlying bone to be very hard and sclerotic, then exostectomy and perforations were performed (Fig. 4). Histologic examination of the resected bone revealed a dense and mature lamellar bone with enlargement of the haversian spaces consistent with melorheostosis (Fig. 5).
Fig. 4.
Exostectomy and cortical fenestration in the first metacarpal, proximal phalange, and trapezium
Fig. 5.
Histologic analysis confirmed the clinical and imaging diagnosis and revealed extremely dense sclerotic bone of cortical pattern
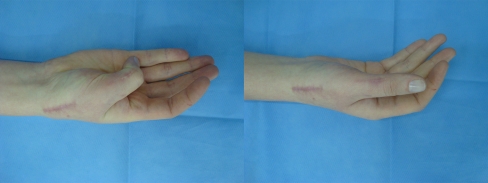
The postoperative recovery was uneventful with normal wound healing. The cosmetic appearance was better, with no swelling and a linear scar. The function of the thumb was normal (Fig. 6). The patient was relieved of her pain and returned to work in 4 weeks.
Fig. 6.
The cosmetic appearance and the function of the thumb
Discussion
The presenting signs and symptoms of this condition are variable depending on age of presentation. Adults typically present with pain, joint stiffness, or a progressive deformity, while presentation in a child would more likely be as limb length discrepancy, deformity, or joint contractures which may also be seen before radiographic evidence of any bony changes [10]. Symptoms of pain and tenderness have been common complaints in the majority of cases resulting from melorheostosis of the hand, and although there are many theories regarding the etiology of pain, the cause of pain associated with is not known [3]. Fibrosis of skin and soft tissues and joint contractures described in others patients [9] were not present in this patient.
The diagnosis of melorheostosis is usually made by the classical plain radiographic findings. The pattern of bony changes are variable, and there have been five pattern identified radiographically which include osteoma-like pattern (30%), classic candle wax appearance (22%), myositis ossificans-like pattern (4%), osteopathia striata-like (26%), and mixed pattern (18%). The location of lesions is also variable. The anatomic distribution is as follows: upper limb (22%), lower limb (70%), upper and lower extremities (4%), and axial skeleton (4%) [9].
CT and MRI, however, better delineate the soft tissue finding. CT and MRI reveal cortical hyperostosis as high attenuation and low signal intensity on all MR pulse sequences, respectively with encroachment on the marrow space. Judkiewicz et al. concluded that osseous abnormalities in melorheostosis are identical on advanced imaging and radiographs [12].
The differential diagnosis includes osteomyelitis, osteopetrosis, osteopoikilosis, pycnodysostosis, and osteopathia striata, all of which can have similar radiographic findings [7, 12], but the most important differential diagnosis of melorheostosis is bone tumors producing dense bone, primarily the various types of osteosarcoma. This is especially true for the osteoma-like form and some classic forms of melorheostosis.
There is no specific treatment for melorheostosis. Generally, emphasis is placed on conservative measures such as pain control with non-steroidal anti-inflammatory drugs and physiotherapy. Unfortunately, neither conservative nor surgical methods of treatment appear to be very effective. Some authors suggest early training to use the unaffected extremity. There seemed to be a connection between severity of pain and extent of hyperostosis especially in the bone marrow compartment, perhaps due to an elevated intra-osseous pressure resulting from hindered blood circulation.
The pain can be caused by carpal tunnel syndrome, and surgical intervention relieved the symptoms and signals in more than 90% of the patients [8].
Preservation of motion is an important aim. Like the present patient, with intra-osseous osteoma-like lesion, most of the reported patients that underwent three surgical debulking of the hyperostotic cortex and cortical fenestration are well in terms of symptoms [1, 4–6, 14–17].
Acknowledgments
Conflict of Interest The authors declare that they have no conflict of interest.
References
- 1.Barfred T, Ipsen T. Congenital carpal tunnel syndrome. J Hand Surg [Am] 1985;10:246–248. doi: 10.1016/s0363-5023(85)80114-3. [DOI] [PubMed] [Google Scholar]
- 2.Birtane M, Eryavuz M, Unualan H, Tuzun F. Melorheostosis: Report of a new case with linear scleroderma. Clin Rheumatol. 1998;17:543–545. doi: 10.1007/BF01451298. [DOI] [PubMed] [Google Scholar]
- 3.Böstman OM, Bakalim GE. Carpal tunnel syndrome in melorheostotic limb. J Hand Surg [Br] 1985;10:101–102. doi: 10.1016/s0266-7681(85)80031-0. [DOI] [PubMed] [Google Scholar]
- 4.Brenner P, Wannske M. Die monomelische Melorheostose der Hand. Handchir Mikrochir Plast Chir. 1985;17:56–59. [PubMed] [Google Scholar]
- 5.Campell CS. Melorheososis of the upper limb. Report of a case. J Bone Joint Surg [Br] 1955;37:471–473. doi: 10.1302/0301-620X.37B3.471. [DOI] [PubMed] [Google Scholar]
- 6.Caudle RJ, Stern PJ. Melorheostosis of the hand. A case report with long-term follow-up. J bone joint Surg. 1987;69:1229–1231. [PubMed] [Google Scholar]
- 7.Fernandes CH, Matheus RP, Faloppa F, Albertoni WM. Alterações esqueléticas da mão na picnodisostose. Rev Bras Ortop. 1996;31:441–442. [Google Scholar]
- 8.Fernandes CH, Meirelles LM, Carneiro RS, Faloppa F, Albertoni WM. Tratamento cirúrgico da síndrome do canal do carpo por incisäo palmar e utilização do instrumento de Paine. Rev Bras Ortop. 1999;34:260–270. [Google Scholar]
- 9.Freyschmdt J. Melorheostosis: A review of 23 cases. Eur Radiol. 2001;11:474–479. doi: 10.1007/s003300000562. [DOI] [PubMed] [Google Scholar]
- 10.Gossler C, Kall C, Christopoulos G, Prommerberger KJ. Melorheostosis of the hand. A case report. Hand Chir Mikro Chir Plast Chir. 2001;33:328–331. doi: 10.1055/s-2001-17767. [DOI] [PubMed] [Google Scholar]
- 11.Greespan A, Azouz EM. Bone dysplasia series. Melerheostosis: review and update. Can Assoc Radiol J. 1999;50:324–330. [PubMed] [Google Scholar]
- 12.Judkiewicz AM, Murphey MD, Resnik CS, Newberg AH, Temple HT, Smith WS. Advanced imaging of melorheostosis with emphasis on MRI. Skeletal Radiol. 2001;30:447–453. doi: 10.1007/s002560100366. [DOI] [PubMed] [Google Scholar]
- 13.Leri A, Joanny J. Une affectione non décrite des os Hyperostose ‘en couléé’ sur toute la longeur d’un membre our ‘mélorheostose’. Bull mém soc med Hôp Paris. 1922;46:1141. [Google Scholar]
- 14.Murray RO, McCredie J. Melorheostosis and the sclerotomes. A radiological correlation. Skel Radiol. 1979;4:57–71. doi: 10.1007/BF00349329. [DOI] [PubMed] [Google Scholar]
- 15.Rozencwaig R, Wilson MR, McFarland GB. Melorheostosis of the skeletally immature hand: a case report and long term follow-up evaluation. J Hand Surg [Am] 1996;21:703–706. doi: 10.1016/S0363-5023(96)80033-5. [DOI] [PubMed] [Google Scholar]
- 16.Sharma R, Burke FD. Melorheostosis of the hand. J Hand Surg [Br] 1996;21:413–415. doi: 10.1016/s0266-7681(05)80220-7. [DOI] [PubMed] [Google Scholar]
- 17.Waiter JM, King JC, Louis DS, Smith J. Melorheostosis of the hand: a comprehensive review. Hand Surg. 1998;3:123–123. doi: 10.1142/S0218810498000167. [DOI] [Google Scholar]