Abstract
Aim
To report photographically the evolution of an astrocytic hamartoma of the left optic nerve head over a 2-year follow-up in a patient with retinitis pigmentosa.
Methods
A 14-year-old boy was seen in the medical retina clinic with a 3-year history of night blindness. Best corrected visual acuity was 6/18 in both eyes. Colour vision was normal in both eyes and confrontation fields showed peripheral constriction. Fundus examination revealed bone spicule pigmentary changes at the retinal mid periphery typical of retinitis pigmentosa and superficial globules at the margins of both optic nerve heads. Electrodiagnostic tests confirmed moderately severe rod cone dystrophy with macular involvement bilaterally.
Results
Two years later, the ocular examination was unchanged except for the appearance of the optic nerve head lesion in the left eye. There was an increase in the size of the lesion which was diagnosed as an astrocytic hamartoma. Further investigations were recommended to exclude neurofibromatosis and tuberous sclerosis.
Conclusion
Astrocytic hamartomas of the optic nerve head and optic nerve head drusen have both been described in patients with retinitis pigmentosa. They can be a diagnostic dilemma although drusen are more common (10%). To differentiate these two entities it is very important to document any growth during the follow-up period which is suggestive of astrocytic hamartoma rather than optic disc drusen.
Key Words: Astrocytic hamartoma, Optic disc drusen, Retinitis pigmentosa
Introduction
Retinal astrocytic hamartomas are rare benign tumours which can arise from any location in the retina, from the optic nerve head and macula to the far periphery. They appear as white nodular masses with patchy calcification overlying the blood vessels. Multifocal and bilateral lesions are likely to be associated with tuberous sclerosis and neurofibromatosis [1, 2]. Solitary astrocytic hamartomas may be seen in otherwise normal patients [3]. We report the evolution of an astrocytic hamartoma of the left optic nerve head over a 2-year follow-up in a patient with retinitis pigmentosa.
Case Report
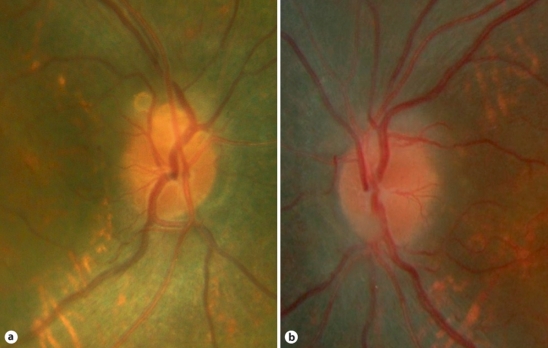
A 14-year-old boy was referred to the medical retina specialists with a history of night blindness over the last 3 years. Best corrected visual acuity was 6/18 in both eyes. There was no significant past ocular and medical history. Also, there was no family history of any retinal disorder. Colour vision tested with Ishihara plates was normal in both eyes and confrontation fields showed mid peripheral constriction. Fundus examination revealed bone spicule pigmentary changes at the retinal mid periphery. The retinal vessels were not significantly attenuated and the optic nerve heads were not pale. Superficial globules at the margins of both optic discs were observed and regarded as optic nerve head drusen (fig. 1).
Fig. 1.
Optic nerve heads of both eyes on presentation.
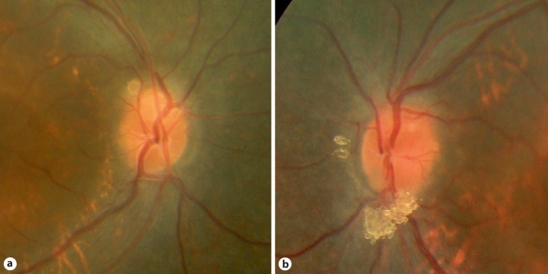
The patient was investigated further with electrodiagnostic tests. Pattern electroretinogram (ERG) P50 components were subnormal bilaterally. Rod-specific and maximal ERGs were severely reduced bilaterally. 30-Hz flicker and transient photopic ERGs were delayed and markedly reduced bilaterally. All the tests confirmed moderately severe rod cone dystrophy with macular involvement bilaterally. A diagnosis of retinitis pigmentosa was confirmed and the patient was followed up yearly. Two years later, the fundus examination revealed evolution of the left optic nerve head lesion with a nodular appearance overlying the optic nerve head vessels (fig. 2). Autofluoresence imaging of the left optic nerve head showed increased autofluorescence of the nodular mass (fig. 3). The remaining examination was unchanged.
Fig. 2.
Optic nerve heads of both eyes 2 years later.
Fig. 3.
Autofluoresence imaging of the left optic nerve head.
Further investigations were recommended to exclude neurofibromatosis and tuberous sclerosis. The patient did not report any symptoms except for night blindness. A detailed family history was negative for any neurological or dermatological disorders. Brain MRI and kidney ultrasound were unremarkable.
Discussion
Astrocytic hamartomas of the optic nerve head are associated with certain types of phakomatoses such as neurofibromatosis and tuberous sclerosis but are also often seen in eyes with retinitis pigmentosa [4, 5]. Although optic nerve head drusen are more common in patients with retinitis pigmentosa [6, 7], they can be difficult to distinguish from an astrocytic hamartoma as illustrated in this case. Optic nerve head drusen are white calcareous deposits. Histopathologically, the drusen contain multiple deposits of calcium crystals that vary in size (5–1,000 μm). These crystals are located in the pre-laminar region of the optic nerve head and are believed to arise from the debris due to long-standing axonal stasis in the nerve fibre layer. They are within the substance of the nerve, whereas disc hamartomas consist of astrocytic cell proliferations in addition to calcifications which overlie the disc and then involve the peripapillary area.
In the past, when the distinction between astrocytic hamartoma and optic nerve head drusen was not clear, many patients with retinitis pigmentosa were presumed to have optic disc drusen [8]. Subsequent analysis of these patients revealed that some of them had astrocytic hamartomas [9]. Differential diagnoses should also include papilloedema, optic disc hemangiomas, retinoblastomas, meningiomas, metastatic tumours, combined hamartomas of the retina and retinal pigment epithelium and granulomas of different aetiologies [10]. B-scan, autofluorescence, fluorescein angiography, optical coherence tomography and computed tomography of the brain could be very helpful in differentiating the optic nerve head lesions.
In our case, the lesion in the left optic nerve head was presumed to be a drusen on clinical examination in the first instance, but the examination 2 years later showed a change in the size and the appearance with characteristics suggestive of optic nerve head astrocytic hamartoma. Autofluoresence and optical coherence tomography confirmed the diagnosis of optic nerve head hamartoma. This is the first time in our knowledge that such an evolution is documented photographically in a patient with retinitis pigmentosa.
Footnotes
This is an Open Access article licensed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs 3.0 License (www.karger.com/OA-license), applicable to the online version of the article only. Distribution for non-commercial purposes only.
The authors have no proprietary interest. No financial support was received for the study.
References
- 1.Williams R, Taylor D. Tuberous sclerosis. Surv Ophthalmol. 1985;30:143–154. doi: 10.1016/0039-6257(85)90058-x. [DOI] [PubMed] [Google Scholar]
- 2.Ulbright TM, Fulling KH, Helveston EM. Astrocytic tumours of the retina. Differentiation of sporadic tumours from phakomatoses-associated tumours. Arch Pathol Lab Med. 1984;108:160–163. [PubMed] [Google Scholar]
- 3.Reeser FH, Aaberg TM, Van Horn DL. Astrocytic hamartoma of the retina not associated with tuberous sclerosis. Am J Ophthalmol. 1978;86:688–698. doi: 10.1016/0002-9394(78)90192-7. [DOI] [PubMed] [Google Scholar]
- 4.Bec P, Mathis A, Adam P, Maillard P, Alberge Y. Retinitis pigmentosa associated with astrocytic hamartomas of the optic disc. Ophthalmologica. 1984;189:135–138. doi: 10.1159/000309399. [DOI] [PubMed] [Google Scholar]
- 5.Pillai S, Limaye S, Saimovici LB. Optic disc hamartoma associated with retinitis pigmentosa. Retina. 1983;3:24–26. [Google Scholar]
- 6.Grover S, Fishman GA, Brown J., Jr Frequency of optic disc or parapapillary nerve fiber layer drusen in retinitis pigmentosa. Ophthalmology. 1997;104:295–298. doi: 10.1016/s0161-6420(97)30321-2. [DOI] [PubMed] [Google Scholar]
- 7.Lorentzen DW. Drusen of the optic disc. Acta Ophthalmol. 1966;(suppl 90):1–180. [PubMed] [Google Scholar]
- 8.De Bustros S, Miller NR, Finkelstein D, Massof R. Bilateral astrocytic hamartomas of the optic nerve heads in retinitis pigmentosa. Retina. 1983;3:21–23. [Google Scholar]
- 9.Robertson DM. Hamartomas of the optic disc with retinitis pigmentosa. Am J Ophthalmol. 1972;74:526–531. doi: 10.1016/0002-9394(72)90921-x. [DOI] [PubMed] [Google Scholar]
- 10.Brown GC, Shields JA. Tumors of the optic nerve head. Surv Ophthalmol. 1985;29:239–264. [PubMed] [Google Scholar]