Introduction
Breathe Your Best for School Success (BYB) was a feasibility program of Asthma 411, an initiative developed to improve asthma management in the school setting as part of a Centers for Disease Control and Prevention cooperative agreement awarded to the St. Louis Regional Asthma Consortium (SLRAC). The objective of BYB was to increase the number of current provider-written asthma action plans (AAPs) submitted to the school nurse at the beginning of the school year. The Saint Louis University Institutional Review Board approved implementation and evaluation of Asthma 411 interventions. BYB was a collaborative project among the school districts and SLRAC.
BYB utilized a “passport” which described the three steps to “breathe your best”: (1) obtain an AAP from a health care provider (HCP), (2) fill prescriptions at a pharmacy, and (3) give appropriate medications and the AAP to the school nurse at the beginning of the school year. The passports were designed to be attractive to students and were inserted into plastic cases attached to lanyards for easy transport by students and families. The passport included information describing the importance of each step and included space for signatures from the HCP, pharmacist, and school nurse to verify completion of each step. Incentives were offered to promote participation. To assess reasons for participation or nonparticipation in the BYB program, randomized telephone surveys with parents or guardians of children with asthma were conducted in the fall of 2007.
Implementation
BYB targeted elementary (K–sixth grade) students in two districts and was promoted during the summers preceding the 2005–2006 (one school district, five schools) and 2006–2007 (two school districts, nine schools) school years. Demographic information for the two districts appears in Table 1. To generate awareness, nurses distributed fliers to students and parents, and BYB was promoted in end-of-year school district newsletters. In June, a letter explaining the program, the BYB passport, and a sample AAP were mailed by the schools to parents of elementary students with asthma—196 in 2005 (11% of the student population) and 429 in 2006 (15% of the student population). The letter described the importance of providing an AAP to the school nurse. Lists of students with asthma were provided by the school nurses, identified through school medical forms and/or noting when students brought asthma medication to the nurse’s office. In mid-July, reminder postcards were sent which briefly described the three steps and incentives. Materials were written at a fourth grade reading level.
Table 1.
Demographics for two low-income, urban school districts participating in Breathe Your Best for School Success
| District Aa | District Bb | ||||
|---|---|---|---|---|---|
| Academic year | 2004–2005 | 2005–2006 | 2006–2007 | 2005–2006 | 2006–2007 |
| Total students | 3,212 | 3,543 | 4,013 | 561 | 577 |
| African American (N, %) | 3,135 (97.6) | 3,465 (97.8) | 3,945 (98.3) | 561 (100) | 577 (100) |
| Qualify for free or reduced price lunch (N, %) | 2,582 (80.4) | 2,824 (79.7) | 3,178 (79.2) | 465 (82.8) | 478 (82.8) |
| Students with asthmac (N, %) | 363 (11.3) | 481 (13.5) | 510 (12.7) | 108 (19.3) | 126 (21.8) |
| Students with asthma submitting an asthma action plan (N, %)d | 110 (30.3) | 124 (25.7) | 122 (24.0) | 22 (20.4) | 32 (25.4) |
aDistrict A participated in both 2005–2006 and 2006–2007
bDistrict B participated in 2006–2007 only
cAs identified and provided by school nurses. Children with asthma are identified by the school nurse by either self-reporting on school medical forms or if child brings asthma medication into her office
dPercentages are based on end-of-year information provided by school nurses. Percentages reported in the text are based on beginning-of-year information
Students who gave their AAP to the nurse at the beginning of the school year received a small “goody bag” containing items donated by health organizations, such as rulers, yo-yos, pens, band-aid holders, health pamphlets, Frisbees, and coloring books. School nurses accepted AAPs in any format, as long as they were completed and signed by the HCP. Students who returned completed AAPs to the school nurse with or without a completed passport, as well as students with current AAPs on file, were entered into a grand prize drawing (e.g., tickets to a pro football game or a shopping spree at a department store). Though many items were donated, the annual estimated cost of the BYB program was $9,440, or $1,048 per school. This included $3,560 for printing, materials, and postage; $2,900 for incentives; and $2,980 estimated staff time (for a 0.2 staff time equivalent).
Processes and Outcomes
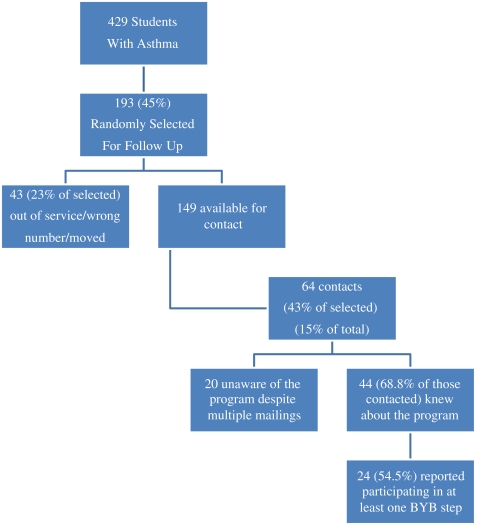
During the 2005–2006 and 2006–2007 school years, only 26 (13.3%) and 27 (6.3%) students with asthma returned completed BYB passports to the school nurse, respectively. In addition, school nurses saw no increase in the total number of current AAPs following the promotion of BYB for either school year. To assess reasons for participation or nonparticipation in the BYB program, school representatives conducted phone interviews in the fall of 2007 with a sample of families randomly selected (N = 193) from the master list of students with asthma who were mailed BYB information (N = 429). Of the 193 selected, 43 had either moved out of the district (as reported by the person who answered the phone) or had inoperable numbers on file, leaving 149 available for interview (Figure 1). Up to three calling attempts per phone number were made in an effort to reach 15% of those mailed BYB information, resulting in 64 successful contacts and interviews. Of those interviewed, 44 (68.8%) reported knowledge of the BYB program. Just over half of these (n = 24) reported participating in at least one or more BYB steps and 92% (n = 22) said they participated because they wanted to stay current on their child’s asthma management. Of those who participated, 75% (n = 18) reported visiting a HCP (the most frequent step reported as completed), while only 13 (54%) reported turning in an AAP to the school nurse as a result of BYB. Reasons for nonparticipation among those who were aware of the program (n = 20) included insufficient time (n = 9), perception that the child’s asthma was under control (n = 6), failure to receive the materials (n = 3), and lack of transportation or a HCP (n = 2).
FIGURE 1.
Evaluation phone calls.
Discussion
Breathe Your Best for School Success was created as a fun, incentive-based program to help encourage students and their families to obtain a current, health care provider-written AAP, and then to provide these to schools. Despite the low participation rate, school nurses were enthusiastic about the program, expressing interest in providing BYB again. Participating school districts reported rates of AAPs on file for students with asthma at 20–30% (Table 1). While these rates were not enhanced by the BYB program, they still may be higher in the participating districts than in other districts with similar demographics and asthma prevalence. Possible reasons for this include that the schools have been involved in Asthma 411 prior to the BYB program, nurses were provided with continuing asthma education and training, and school nurses prioritized the pursuit of up-to-date AAPs. Similarly, 92% of the parents reporting participation indicated that they found the BYB materials informative and a good reminder for staying current on asthma management. Only one respondent in the telephone survey stated that the incentive was the motivating reason to participate in BYB. These positive responses by nurses and parents suggest that a program such as BYB might promote asthma care-related awareness and action; however, the low participation rate warrants exploration into barriers to participation and potential program modifications.
School nurse feedback indicated that outcomes might be improved by conducting programs like BYB throughout the entire academic year. Although this would add to nurses’ workloads, a nonsummer schedule is also likely to be more convenient for them. (It might furthermore increase parent exposure to the program and student involvement in it.) BYB was facilitated by Asthma 411 staff in collaboration with the school nurses to minimize additional work for the nurses. However, BYB planning and implementation proved to be labor and time intensive, and the program might be too costly and time-consuming for school nurses without additional assistance from the district or other community organizations.
Many parents may not have perceived participating in BYB to be a priority. Even though an asthma action plan was included in the materials mailed to parents, responses during the phone calls indicated that many were still unaware of the importance of obtaining a provider-written AAP, or submitting a copy to the school. Additionally, approximately 13 (54%) of the parents who did participate reported that they turned in an AAP to the school nurse—a number inconsistent with school nurse records, which indicated that only nine (37.5%) had in fact turned in an AAP. This inconsistency may illustrate a lack of understanding related to the AAP. There are many health forms required by the schools, but the AAP is not among them. Many parents may have assumed they had given an AAP to the school nurse, confusing it with one of the other, required health forms. Providing parents with thorough information about the use of an AAP may improve this discrepancy. Furthermore, there was a large gap between the number of children visiting a HCP (n = 18), as reported by parents, and the number of AAPs returned in conjunction with a passport (n = 9), as reported by the school nurses. While parents were not asked if the HCP filled out an AAP during the child’s visit, this gap could indicate that either health care providers were not providing AAPs, or that parents were not following through and providing the AAP to the school nurse. This lack of understanding indicates parents’ and HCPs’ need for additional education about AAPs and the steps to asthma management.
The low participation also suggests that the goody bags and the grand prize drawings for football tickets and shopping sprees did not offer sufficient incentive for parents and students. Likewise, it is unclear whether the incentives provided any motivation to the families that did participate. BYB may have been successful at engaging those students and families who were already participating in positive health behaviors, or who were more motivated to do so, and it may have been able to accomplish this without the added incentives.
Conclusion
An incentive-based intervention may provide a novel way to increase provider-written AAPs within the school setting, but other barriers in the participating districts appeared to limit the intervention’s success. Although no significant changes were seen, this type of intervention may help to raise awareness of the need for provider-written AAPs. Based on parent responses, it was and can be a useful method of informing and reminding parents about the key components of asthma management. Modifications such as implementing the program over the course of an entire school year and providing education for parents, students, and HCPs may improve the outcomes of BYB.
Acknowledgments
The authors would like to thank Theresa Prosser, Pharm.D., BCPS, Tricia Berry, Pharm.D., BCPS, the schools, and school nurses for their assistance in developing and implementing Breathe Your Best for School Success.
Footnotes
This project was supported in part through a cooperative agreement with the Centers for Disease Control and Prevention, U.S. Department of Health and Human Services under program announcement 03030. All human subject activities were approved by the Saint Louis University Institutional Review Board.