Abstract
Background
The purposes of the present study are to evaluate the subsidence and nonunion that occurred after anterior cervical discectomy and fusion using a stand-alone intervertebral cage and to analyze the risk factors for the complications.
Methods
Thirty-eight patients (47 segments) who underwent anterior cervical fusion using a stand-alone polyetheretherketone (PEEK) cage and an autologous cancellous iliac bone graft from June 2003 to August 2008 were enrolled in this study. The anterior and posterior segmental heights and the distance from the anterior edge of the upper vertebra to the anterior margin of the cage were measured on the plain radiographs. Subsidence was defined as ≥ a 2 mm (minor) or 3 mm (major) decrease of the segmental height at the final follow-up compared to that measured at the immediate postoperative period. Nonunion was evaluated according to the instability being ≥ 2 mm in the interspinous distance on the flexion-extension lateral radiographs.
Results
The anterior and posterior segmental heights decreased from the immediate postoperative period to the final follow-up at 1.33 ± 1.46 mm and 0.81 ± 1.27 mm, respectively. Subsidence ≥ 2 mm and 3 mm were observed in 12 segments (25.5%) and 7 segments (14.9%), respectively. Among the expected risk factors for subsidence, a smaller anteroposterior (AP) diameter (14 mm vs. 12 mm) of cages (p = 0.034; odds ratio [OR], 0.017) and larger intraoperative distraction (p = 0.041; OR, 3.988) had a significantly higher risk of subsidence. Intervertebral nonunion was observed in 7 segments (7/47, 14.9%). Compared with the union group, the nonunion group had a significantly higher ratio of two-level fusion to one-level fusions (p = 0.001).
Conclusions
Anterior cervical fusion using a stand-alone cage with a large AP diameter while preventing anterior intraoperative over-distraction will be helpful to prevent the subsidence of cages. Two-level cervical fusion might require more careful attention for avoiding nonunion.
Keywords: Anterior cervical fusion, PEEK cage, Subsidence, Nonunion
Anterior cervical discectomy and fusion (ACDF) has been performed as the gold standard for the treatment of degenerative cervical disc disease. However, the classic method of Cloward1) and Smith and Robinson2) using an autologous tricortical iliac bone graft has been reported to have problems of donor site morbidity3,4) and subsidence.5,6) In order to overcome those problems, ACDF using an intervertebral cage has been recently used with favorable results. Stand-alone intervertebral cages made of a range of materials such as stainless steel, titanium, carbon fiber and polyetheretherketone (PEEK),7,8) can be effective for restoring the intervertebral disc height and lordosis, providing load-bearing support to the anterior column and preventing graft collapse.7,9) However, nonunion and subsidence into the endplates have been reported as the complications of this procedure,7,8,10-13) which can eventually result in narrowing of the foramen, nerve root compression, pseudoarthrosis due to cervical instability,14,15) and adjacent segment degeneration due to the loss of lordosis.16,17) The purpose of this study is to evaluate the incidence and risk factors of nonunion and subsidence after ACDF using a stand-alone PEEK cage by performing a radiological analysis.
METHODS
One- or two-level ACDF using a stand-alone PEEK cage (Solis®, Stryker Spine, Allendale, NJ, USA) and an autologous cancellous iliac bone graft was performed on 51 patients (63 segments) with degenerative cervical disc disease, including cervical myelopathy and radiculopathy, between June 2003 and August 2008. Of them, 38 patients (47 segments) were enrolled in this study. The exclusion criteria were ≤ a 12 month follow-up period, C7-T1 fusion (insufficient for precise radiological evaluation), anterior fusion on the adjacent segments and additional posterior decompression. The mean age of the patients was 52 years (range, 34 to 75 years). There were 20 males and 18 females. The mean follow-up period was 23.1 months (range, 12 to 57 months). The preoperative diagnosis was radiculopathy in 26 patients and cervical myelopathy in 12. There were 27 one-level fusions and 20 two-level fusions. The two-level fusion involving C7-T1 level in two patients was classified as two-level fusion, but only one segment other than C7-T1 was included in the analysis. There were 2 segments of C3-4 fusion, 6 segments of C4-5 fusion, 28 segments of C5-6 fusion and 11 segments of C6-7 fusion.
Operative Technique
The surgical site was exposed via a standard anterior approach2) and microscopic anterior cervical discectomy was performed. Cartilage was removed with care to avoid damaging the cortical bone of the vertebral endplates. The posterior longitudinal ligament was opened and decompression was carried out. The appropriate cage size was then determined under fluoroscopy guidance. Anterior cervical fusion was performed using a PEEK cage filled with cancellous bone obtained from the anterior iliac crest through a minimal incision. The height of the cage was 6, 7, 8, and 9 mm in 8, 28, 8, and 3 segments, respectively. The anteroposterior (AP) diameter of the cage was 12 and 14 mm in 21 and 26 segments, respectively.
Radiological Evaluation
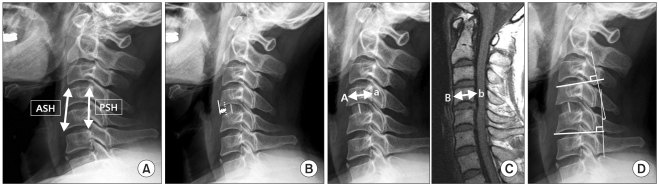
MRI scans were obtained before surgery and the AP and lateral plain radiographs were obtained before surgery, immediately after surgery, at 6 weeks, 3 months, and 6 months after surgery and the last follow-up. Flexion-extension lateral views were also obtained from 3 months after surgery. The anterior segmental height (ASH), posterior segmental height (PSH) (Fig. 1A) and cage distance (CD: the distance from the anterior edge of the upper vertebra to the anterior margin of the cage) (Fig. 1B) were measured on the radiographs. The ratio of the AP diameter at the middle of the upper vertebral body on the radiographs to that on the MRI scans was used to correct for the magnification difference of each image (Fig. 1C). The ASH and PSH values were used to assess the anterior/posterior intraoperative distraction and the anterior/posterior subsidence. The ASH/PSH was measured as the distance between the anterior/posterior margin of the upper end plate of the upper vertebra and the anterior/posterior margin of the lower end plate of the lower vertebra. The anterior/posterior intraoperative distraction was calculated as a difference in the ASH/PSH between before surgery and immediately after surgery. Anterior/posterior subsidence was defined as ≥ a 2 mm (minor subsidence) or 3 mm (major subsidence) reduction in the ASH/PSH between immediately after surgery and the last follow-up. The patients with ≥ 2 mm subsidence were classified as the subsidence group.
Fig. 1.
(A) The anterior segmental height (ASH) and posterior segmental height (PSH) were measured as the distance between the upper end plate of the upper vertebra and the lower end plate of the lower vertebra at the anterior and posterior margins, respectively. (B) The cage distance was measured as the distance between the anterior edge of the upper vertebra and the anterior margin of the cage. (C) Magnification differences were corrected by the ratio between the anteroposterior diameters at the middle of the upper vertebral body on each plain radiograph (A-a) and MRI (B-b). Every length measured on the plain radiographs was multiplied by the ratio (B-b/A-a). (D) Segmental lordosis was measured using Cobb's method.
Segmental lordosis was measured using Cobb's method to assess the sagittal alignment (Fig. 1D). The increase in lordosis from before surgery to immediately after surgery and the decrease in lordosis from immediately after surgery to the last follow-up were recorded.
Nonunion was defined as the appearance of segmental instability with ≥ 2 mm widening of the interspinous distance on the flexion-extension lateral views at the last follow-up.
Radiological assessments were performed by an independent orthopedic surgeon on two occasions with using two PACS digital software systems: a Marosis 5.0 PACS viewer (Marotech, Seoul, Korea) and an Impax CS 5000 (Agfa-Gevaert, Mortsel, Belgium).
Statistical Analysis
The risk factors for cage subsidence were assessed using logistic regression analysis. The decreases of segmental lordosis in the subsidence and nonsubsidence groups were analyzed using independent t-tests. The risk factors for nonunion were analyzed using nonparametric tests: the chi square test and Fisher's exact test for the categorical variables and the Mann-Whitney U test for the continuous variables. All the statistical analyses were conducted using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA). Statistical significance was set at p-values < 0.05 with a confidence interval of 95%.
RESULTS
Cage Subsidence and the Risk Factors
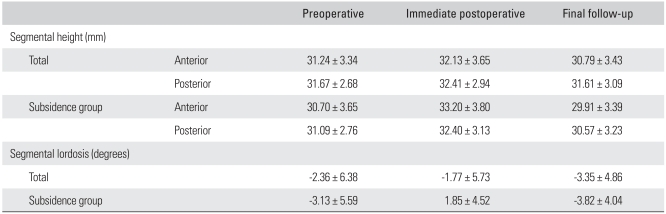
The mean loss of ASH and PSH was 1.33 ± 1.46 mm and 0.81 ± 1.27 mm, respectively, from immediately after surgery to the last follow-up and 0.44 ± 1.42 mm and 0.06 ± 1.34 mm, respectively, from before surgery to the last follow-up (Table 1). Cage subsidence of ≥ 2 mm and ≥ 3 mm occurred in 12 (25.5%) and 7 (14.9%) of the 47 segments, respectively. Among the segments with ≥ 2 mm subsidence, anterior subsidence only and combined anterior and posterior subsidence was observed in 5 segments (42%) and 7 segments (58%) of the 12 segments, respectively, and posterior subsidence only was not noted in any of them. The expected risk factors were gender, the AP diameter of the cage, the cage distance, the intraoperative anterior distraction and the intraoperative increase of segmental lordosis. Of them, the AP diameter of the cage and the intraoperative anterior distraction had statistically significant effects on subsidence: the use of 14 mm-diameter cages led to a significantly less risk for subsidence than did using 12 mm-diameter cages (p = 0.034; odds ratio [OR], 0.017) and larger intraoperative anterior distraction resulted in a significantly greater risk for subsidence (p = 0.041; OR, 3.988) (Table 2).
Table 1.
The Segmental Height and Segmental Lordosis in Total and the Subsidence Group
Table 2.
Logistic Regression Analysis of the Risk Factors for Subsidence
*Statistically significant (p < 0.05).
Loss of Segmental Lordosis
The loss of segmental lordosis from immediately after surgery to the last follow-up averaged 1.58° ± 3.68° and it was ≥ 3° in 14 segments (29.8%). The mean loss from before surgery to the last follow-up was 0.99° ± 4.81° (Table 1). The mean loss of segmental lordosis from immediately after surgery to the last follow-up was 5.67° ± 2.95° in the subsidence group, which was significantly higher compared to 1.77° ± 2.76° in the nonsubsidence group (p < 0.01).
Intervertebral Nonunion and the Risk Factors
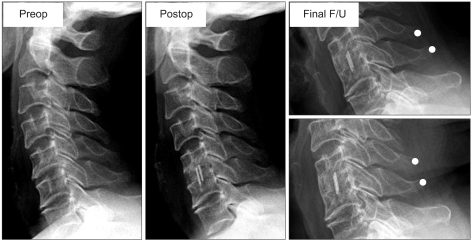
Nonuninon was observed in 7 segments (14.9%). A statistically significant difference between the union and nonunion groups was found only for the number of fused segments (p = 0.001) and not for the other surgical conditions or radiological parameters. Nonunion did not occur in the 27 segments after one-level fusion (0%) whereas it occurred in 7 (35%) of the 20 segments after two-level fusion (p = 0.001). The incidence of subsidence was higher in the nonunion group compared to that in the union group, but the difference was not statistically significant (p = 0.06) (Figs. 2 and 3).
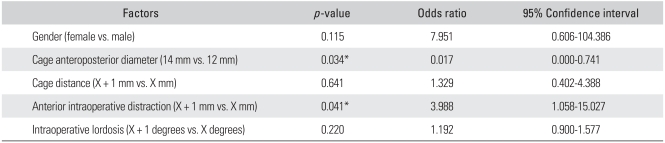
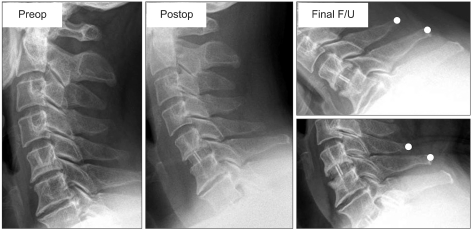
Fig. 2.
A case of anterior subsidence without nonunion. The anterior subsidence was 2.8 mm, and segmental stability on the flexion and extension radiographs was observed. Subsidence is not necessarily accompanied with nonunion. F/U: follow-up.
Fig. 3.
A case of nonsubsidence with nonunion. Instability with a difference of 5 mm between the interspinous distances on the flexion and extension radiographs was observed without subsidence. Nonunion can occur without subsidence. F/U: follow-up.
DISCUSSION
ACDF using an intervertebral cage has become a popular alternative to prevent the complications of the classic method using a autologous tricortical iliac bone graft3-6,18) and anterior cervical plating, including screw loosening, screw breakage, screw migration and soft tissue injuries.19-21) ACDF using an intervertebral cage is credited with promoting instant stability, restoration of the neural foraminal height and interbody fusion by providing an environment for bone growth.10,14,22) However, recent studies have shown that cage subsidence is a major complication of ACDF using stand-alone cages regardless of the composite materials (Table 3).7,8,10-13,15,23,24) PEEK cages are currently the most preferred. Compared with titanium and carbon fiber cages, PEEK cages are more biocompatible25) and radiolucent, which allows for precise radiological evaluation of bony union. In addition, PEEK cages are expected to result in lower subsidence rates than that with using metal cages because their modulus of elasticity is similar to that of bone.26) However, various degrees of subsidence have been reported after ACDF using stand-alone PEEK cages (Table 3). This can be partly attributable to the errors from measurement methods and the magnification differences on radiographs. Based on the report that ≤ 2 mm cage subsidence into the vertebral body can occur during the bone remodeling process after ACDF using cages,10) the segments with ≥ a 2 mm decrease in the anterior or posterior segmental height were classified as the subsidence group in this current study. Considering that ≥ a 3 mm11-13,15,23) decrease, as well as ≥ 2 mm7,10,24) decrease, has been used as a criterion for subsidence in many studies, we recorded ≥ 2 mm subsidence (minor subsidence) and ≥ 3 mm subsidence (major subsidence) separately for comparisons with other studies. The segmental height, including the upper and lower vertebral bodies, was measured to assess subsidence instead of measuring the intervertebral disc space height to reduce measurement errors. Indeed, owing to bone formation in the endplates around the cage, adjacent endplates are difficult to identify clearly and a reduction in the distance between endplates may not be distinguishable from subsidence.7,15,18,23,24) With regard to methods to eliminate magnification errors on the radiographs, the ratio of the segmental height to the AP diameter of the vertebral body can be used5) or the ratio of the AP diameter of the verteberal body on MRI scans to that on radiographs can be calculated to correct for the segmental height,7,15) as was done in this study. As a result, ≥ 2 mm subsidence and ≥ 3 mm subsidence was observed in 25.5% and 14.9% of the total segments, respectively. Anterior subsidence only and combined anterior and posterior subsidence occurred in the majority of the subsidence segments and posterior only subsidence was rare, as was reported in other studies.
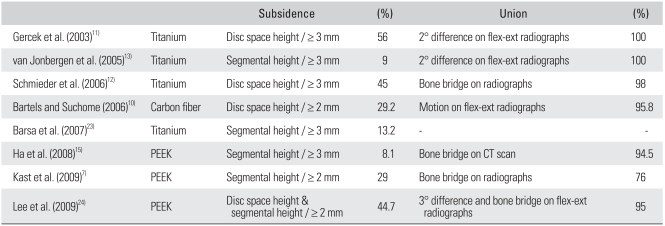
Table 3.
Summary of the Studies on Cage Subsidence and Union
PEEK: polyetheretherketone, flex-ext: flexion-extension.
Cage subsidence is a concern in that the decrease of the foraminal volume, cervical spine instability and loss of segmental lordosis can lead to adjacent segment degeneration.14-16) On the contrary, Schmieder et al.12) reported that the height of the foramen was well maintained among the subsidence cases and the occurrence of kyphosis was either rare or it did not result in notable clinical differences. However, in this study, the segmental height at the last follow-up was even lower than the preoperative segmental height in the subsidence group when it was insufficient immediately after surgery, indicating the possibility of the decrease of the foraminal volume due to subsidence. Furthermore, kyphosis was noted in 67% of the subsidence group at the last follow-up and the loss of segmental lordosis in the subsidence group was significantly higher compared to that of the nonsubsidence group, indicating the possibility of progression of adjacent segment degeneration due to subsidence.
The risk factors for cage subsidence have been statistically analyzed in a few previous studies. The logistic regression analysis by Bartels et al.10) showed that the incidence of cage subsidence was significantly higher for C6-7 fusion level than that for the other fusion levels. Barsa and Suchomel23) reported that the distance from the anterior rim of the upper vertebra to the cage was significantly larger and the contact surface ratio of the cage versus the endplate was significantly smaller in the subsidence group. The expected risk factors included in our logistic regression analysis were also among a variety of major ones described in the literature. Proper surgical preparation of the upper and lower endplates to reduce bone structure damage was not included because the amount of damage of the bony structure could not be assessed on plain radiographs. Vertebral body bone density was excluded as well because it was difficult to measure this in all the patients. Instead, gender was included, which allowed us to estimate the impact of bone density in older-age women with osteoporosis.10) The distance from the anterior edge of the upper vertebra to the anterior margin of the cage was included as an expected risk factor based on the report of Barsa and Suchomel23) that the anterior vertebral osteophyte provides biomechanical support to the interbody cage and the distance from the cage to the anterior vertebral rim was correlated with the incidence of subsidence. The results of the analysis showed that the ratio of the AP diameter of the upper endplate to the diameter of the cage had no statistically significant correlation with the incidence of subsidence (Pearson's correlation coefficient, 0.22) and there was also no significant difference between the subsidence and nonsubsidence groups when comparing the means (p = 0.188). The contact surface ratio of the cage versus the endplate was not included in the analysis because precise measurement of the width of the endplate was difficult to obtain on the plain AP radiographs. Instead, the absolute values of the AP diameter of the cages (14 mm vs. 12 mm) were examined on the risk factor analysis. The results showed that the risk of subsidence was significantly lower when a 14 mm-diameter cage rather than a 12 mm-diameter cage was used and when the anterior intraoperative distraction was smaller (Table 2). Accordingly, the contact surface between the cage and the vertebral body, and the anterior intraoperative distraction were confirmed as the risk factors for cage subsidence. Therefore, it is recommend to use a cage with a large AP diameter, to perform interbody distraction prior to anterior longitudinal ligament resection with using caution to avoid over-distraction and to choose a cage with a proper height in order not to have to apply excessive force during cage insertion.10)
Intervertebral union was observed in ≥ 90% of the cases after ACDF using stand-alone cages in most of the previous studies, except for the 6-month follow-up study of Kast et al.7) (Table 3). However, the union rates of the previous studies might have been overestimated due to measurement errors. Indeed, accurate assessment of the bone bridge formation on radiographs and precise angular measurement of motion on the flexion-extension lateral radiographs are difficult to achieve. It is desirable to assess both the bone bridge formation on CT scans and the stability on the flexion-extension lateral radiographs. Unfortunately, it is not feasible to perform CT scans on all patients. Based on the report that the interspinous distance was more reliable in terms of reproducibility and accuracy than the Cobb angle on the flexion-extension lateral radiographs, the segments with ≥ a 2 mm difference of the interspinous distance on the flexion-extension lateral radiographs were classified as nonunion,27) which was found in 14.9% of the total segments in our study. The risk factors for nonunion were evaluated by comparing the union and nonunion groups using nonparametric tests. The number of segments in the nonunion group was not sufficient for logistic regression analysis. A significant difference was found in the number of fused segments, that is, one-level fusion vs. two-level fusion (Fisher's exact test, p = 0.001). The incidence of nonunion was 0% and 35% after one-level fusion and two-level fusion, respectively, indicating a significantly higher rate of nonunion in two-level fusion (Fisher's exact test, p = 0.001). Van Jonbergen et al.13) reported that union was achieved in all cases at the sixth postoperative month after one-level, two-level, three-level and even four-level fusions. However, our results revealed that more caution should be taken to prevent nonunion during two-level fusion than that during one-level fusion.
This study evaluated the radiological findings regarding subsidence and nonunion after ACDF using a stand-alone PEEK cage. Future studies need to examine the relationships between the radiological findings and the clinical outcomes to determine the clinical implications of the complications.
In conclusion, ACDF using a stand-alone cage and an autologous cancellous iliac bone graft can lead to anterior subsidence only or combined anterior and posterior subsidence, which all eventually results in kyphotic malalignment. It can be helpful to use a stand-alone cage with a large AP diameter and to avoid intraoperative anterior over-distraction so as to prevent cage subsidence. Furthermore, greater care should be taken in cases of two-level fusion to avoid nonunion, which is another major complication of the procedure.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15(6):602–617. doi: 10.3171/jns.1958.15.6.0602. [DOI] [PubMed] [Google Scholar]
- 2.Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958;40(3):607–624. [PubMed] [Google Scholar]
- 3.Banwart JC, Asher MA, Hassanein RS. Iliac crest bone graft harvest donor site morbidity: a statistical evaluation. Spine (Phila Pa 1976) 1995;20(9):1055–1060. doi: 10.1097/00007632-199505000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Silber JS, Anderson DG, Daffner SD, et al. Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 2003;28(2):134–139. doi: 10.1097/00007632-200301150-00008. [DOI] [PubMed] [Google Scholar]
- 5.Siddiqui AA, Jackowski A. Cage versus tricortical graft for cervical interbody fusion: a prospective randomised study. J Bone Joint Surg Br. 2003;85(7):1019–1025. doi: 10.1302/0301-620x.85b7.13398. [DOI] [PubMed] [Google Scholar]
- 6.Vavruch L, Hedlund R, Javid D, Leszniewski W, Shalabi A. A prospective randomized comparison between the cloward procedure and a carbon fiber cage in the cervical spine: a clinical and radiologic study. Spine (Phila Pa 1976) 2002;27(16):1694–1701. doi: 10.1097/00007632-200208150-00003. [DOI] [PubMed] [Google Scholar]
- 7.Kast E, Derakhshani S, Bothmann M, Oberle J. Subsidence after anterior cervical inter-body fusion: a randomized prospective clinical trial. Neurosurg Rev. 2009;32(2):207–214. doi: 10.1007/s10143-008-0168-y. [DOI] [PubMed] [Google Scholar]
- 8.Kulkarni AG, Hee HT, Wong HK. Solis cage (PEEK) for anterior cervical fusion: preliminary radiological results with emphasis on fusion and subsidence. Spine J. 2007;7(2):205–209. doi: 10.1016/j.spinee.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 9.Kandziora F, Pflugmacher R, Schafer J, et al. Biomechanical comparison of cervical spine interbody fusion cages. Spine (Phila Pa 1976) 2001;26(17):1850–1857. doi: 10.1097/00007632-200109010-00007. [DOI] [PubMed] [Google Scholar]
- 10.Bartels RH, Donk RD, Feuth T. Subsidence of stand-alone cervical carbon fiber cages. Neurosurgery. 2006;58(3):502–508. doi: 10.1227/01.NEU.0000197258.30821.50. [DOI] [PubMed] [Google Scholar]
- 11.Gercek E, Arlet V, Delisle J, Marchesi D. Subsidence of stand-alone cervical cages in anterior interbody fusion: warning. Eur Spine J. 2003;12(5):513–516. doi: 10.1007/s00586-003-0539-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schmieder K, Wolzik-Grossmann M, Pechlivanis I, Engelhardt M, Scholz M, Harders A. Subsidence of the wing titanium cage after anterior cervical interbody fusion: 2-year follow-up study. J Neurosurg Spine. 2006;4(6):447–453. doi: 10.3171/spi.2006.4.6.447. [DOI] [PubMed] [Google Scholar]
- 13.van Jonbergen HP, Spruit M, Anderson PG, Pavlov PW. Anterior cervical interbody fusion with a titanium box cage: early radiological assessment of fusion and subsidence. Spine J. 2005;5(6):645–649. doi: 10.1016/j.spinee.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 14.Bartels RH, Donk R, van Azn RD. Height of cervical foramina after anterior discectomy and implantation of a carbon fiber cage. J Neurosurg. 2001;95(1 Suppl):40–42. doi: 10.3171/spi.2001.95.1.0040. [DOI] [PubMed] [Google Scholar]
- 15.Ha SK, Park JY, Kim SH, Lim DJ, Kim SD, Lee SK. Radiologic assessment of subsidence in stand-alone cervical polyetheretherketone (PEEK) cage. J Korean Neurosurg Soc. 2008;44(6):370–374. doi: 10.3340/jkns.2008.44.6.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Katsuura A, Hukuda S, Saruhashi Y, Mori K. Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J. 2001;10(4):320–324. doi: 10.1007/s005860000243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Oda I, Cunningham BW, Buckley RA, et al. Does spinal kyphotic deformity influence the biomechanical characteristics of the adjacent motion segments? An in vivo animal model. Spine (Phila Pa 1976) 1999;24(20):2139–2146. doi: 10.1097/00007632-199910150-00014. [DOI] [PubMed] [Google Scholar]
- 18.Shad A, Leach JC, Teddy PJ, Cadoux-Hudson TA. Use of the Solis cage and local autologous bone graft for anterior cervical discectomy and fusion: early technical experience. J Neurosurg Spine. 2005;2(2):116–122. doi: 10.3171/spi.2005.2.2.0116. [DOI] [PubMed] [Google Scholar]
- 19.Paramore CG, Dickman CA, Sonntag VK. Radiographic and clinical follow-up review of Caspar plates in 49 patients. J Neurosurg. 1996;84(6):957–961. doi: 10.3171/jns.1996.84.6.0957. [DOI] [PubMed] [Google Scholar]
- 20.Bose B. Anterior cervical fusion using Caspar plating: analysis of results and review of the literature. Surg Neurol. 1998;49(1):25–31. doi: 10.1016/s0090-3019(97)00306-6. [DOI] [PubMed] [Google Scholar]
- 21.Gaudinez RF, English GM, Gebhard JS, Brugman JL, Donaldson DH, Brown CW. Esophageal perforations after anterior cervical surgery. J Spinal Disord. 2000;13(1):77–84. doi: 10.1097/00002517-200002000-00015. [DOI] [PubMed] [Google Scholar]
- 22.Steffen T, Tsantrizos A, Fruth I, Aebi M. Cages: designs and concepts. Eur Spine J. 2000;9(Suppl 1):S89–S94. doi: 10.1007/PL00010027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barsa P, Suchomel P. Factors affecting sagittal malalignment due to cage subsidence in standalone cage assisted anterior cervical fusion. Eur Spine J. 2007;16(9):1395–1400. doi: 10.1007/s00586-006-0284-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee SH, Suk KS, Kim KT, Lee JH, Seo EM, Im YS. Outcome analysis of single level anterior cervical fusion using interbody PEEK cage with autologous iliac bone graft. J Korean Orthop Assoc. 2009;44(1):93–101. [Google Scholar]
- 25.Toth JM, Wang M, Estes BT, Scifert JL, Seim HB, 3rd, Turner AS. Polyetheretherketone as a biomaterial for spinal applications. Biomaterials. 2006;27(3):324–334. doi: 10.1016/j.biomaterials.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 26.Wenz LM, Merritt K, Brown SA, Moet A, Steffee AD. In vitro biocompatibility of polyetheretherketone and polysulfone composites. J Biomed Mater Res. 1990;24(2):207–215. doi: 10.1002/jbm.820240207. [DOI] [PubMed] [Google Scholar]
- 27.Cannada LK, Scherping SC, Yoo JU, Jones PK, Emery SE. Pseudoarthrosis of the cervical spine: a comparison of radiographic diagnostic measures. Spine (Phila Pa 1976) 2003;28(1):46–51. doi: 10.1097/00007632-200301010-00012. [DOI] [PubMed] [Google Scholar]