Abstract
Ethnic and geographical differences are important factors in studying disease frequencies, because they may highlight the environmental or genetic influences in the etiology. We retrieved the studies which have been published regarding the epidemiologic features of gastroesophageal reflux disease (GERD) in Asia, based on the definitions of GERD, study settings, publication years and geographical regions. From the population-based studies, the prevalence of symptom-based GERD in Eastern Asia was found to be 2.5%-4.8% before 2005 and 5.2%-8.5% from 2005 to 2010. In Southeast and Western Asia, it was 6.3%-18.3% after 2005, which was much higher than those in Eastern Asia. There were robust epidemiologic data of endoscopic reflux esophagitis in medical check-up participants. The prevalence of endoscopic reflux esophagitis in Eastern Asia increased from 3.4%-5.0% before 2000, to 4.3%-15.7% after 2005. Although there were only limited studies, the prevalence of extra-esophageal syndromes in Asia was higher in GERD group than in controls. The prevalence of Barrett's esophagus was 0.06%-0.84% in the health check-up participants, whereas it was 0.31%-2.00% in the referral hospital settings. In summary, the prevalence of symptom-based GERD and endoscopic reflux esophagitis has increased in Asian countries. However, the prevalence of Barrett's esophagus in Asia has not changed and also still rare.
Keywords: Asia, Epidemiology, Gastroesophageal reflux, Prevalence
Introduction
Gastroesophageal reflux disease (GERD) broadly includes the whole spectrum of reflux disease, from intermittent symptoms like heartburn or acid regurgitation to endoscopic reflux esophagitis and Barrett's esophagus.1 It usually gives a considerable impact on the quality of the patient's life not only by the symptoms, but also by the following consultation procedures and medical cares. While GERD is a common disease and also the major upper gastrointestinal problem in Western countries, its prevalence amongst Asian has been reported to be relatively low.2-4
During the recent decade, several studies about prevalence of symptom-based GERD and endoscopic reflux esophagitis have revealed generally higher number of patients compared to other previous Asian studies. Time trend studies have also shown the increase of prevalence both in symptom based-GERD and endoscopic reflux esophagitis.5
Heartburn and acid regurgitation are the characteristic symptoms of GERD. Heartburn is defined as a burning sensation at the retrosternal area. However, different criteria of GERD have been published from all over the world including Asia, with the frequency of its symptoms differing from once a week to even once a year. Furthermore, it also has been attributed to the lack of the exact word for heartburn in some Asian languages, such as Chinese or Korean.6 In addition, there has not been any consensus distinguishing GERD from dyspepsia.
In Asia, endoscopic reflux esophagitis is quite commonly diagnosed because the cost of endoscopic examination is relatively inexpensive. Actually, a lot of asymptomatic people get the upper endoscopic examinations for gastric cancer screening and comprehensive medical check-up. The major limitation of studies with individuals in screening program is that it might not represent the general population. However, such studies have advantages of their large sample size and consistent diagnostic manners.
This paper was aimed to review the epidemiologic aspect of GERD and its related disease manifestations, such as endoscopic reflux esophagitis, Barrett's esophagus and extra-esophageal syndrome, according to various definitions, study settings, publication years and geographical regions in Asia.
Methods
Identification and Eligibility Assessment of Relevant Studies
A systematic PubMed search was performed to identify all of the reports written about the prevalence of GERD, published from January 1995 to October 2010, using combinations of the following index terms: "gastroesophageal reflux disease," "reflux," "gastroesophageal reflux" or "esophagitis" and "prevalence" or "epidemiology." Only the papers published in English were reviewed. Included studies had to meet all of these 3 following criteria: (1) including epidemiologic studies performed with at least 200 subjects gathered by population-based or medical check-up settings; (2) having detailed description of GERD definition or its related manifestations and (3) subjecting any sample type, including subjects from tertiary hospitals, to collect data about extra-esophageal symptoms or Barrett's esophagus.
Data Extraction
Following information was abstracted from each study included: the year of publication, study periods, country of subjects, sample types (the population-based type, subjects who underwent the medical check-up or those from referral hospitals), study design (derived from case-control, cohort or other cross-sectional studies), sample size and prevalence of GERD, reflux esophagitis, Barrett's esophagus or extra-esophageal syndromes of GERD.
All studies were sub-grouped by each geographical region, based on Globocan 2008, the project of the International Agency for Research on Cancer which provides contemporary estimates of the incidence, prevalence and mortality from major types of cancers for all countries over the world.7 The Asian geographic area includes these 4 regions of Eastern (China, Japan, Korea and Taiwan), Southeastern (Malaysia, Singapore and Thailand), South Central (India, Iran and Pakistan) and Western (Israel and Turkey) Asia.
Among a total of 3,440 papers searched by those key words, 1,696 papers were excluded from this study because they were not written by English or their subjects were not adults or human. Only 70 studies were included in the final analysis.
Prevalence of Symptom-Based Gastroesophageal Reflux Disease
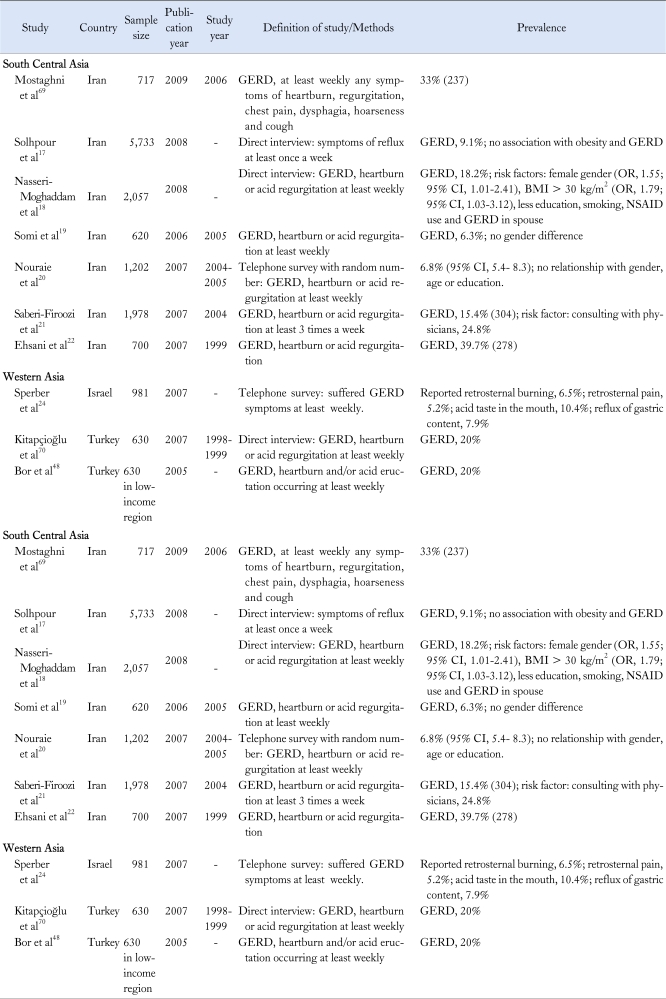
Details of published studies satisfying the inclusion criteria on the symptom-based GERD (ie, symptoms of heartburn or acid regurgitation occurring at least once a week), in the population-based studies are listed in Table 1. They generally used methods of face-to-face or telephone interviews or the postal questionnaires.
Table 1.
Population-Based Study of Gastroesophageal Reflux Disease in Asia
GERD, gastroesophageal reflux disease; RDQ, Reflux Disease Questionnaire, HRQOL; health-related quality of life; IBS, irritable bowel syndrome; SGER, symptomatic gastroesophageal reflux; BMI, body mass index.
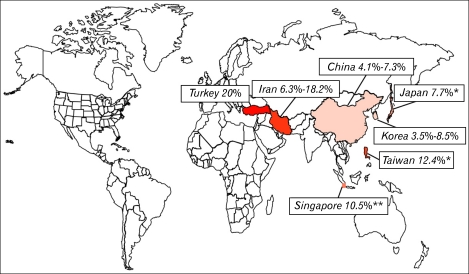
The largest sample group was consisted of Eastern Asia studies, followed by those from South Central Asia (Figure). The prevalence of symptom-based GERD in Eastern Asia was 5.2%-8.5%8-13 from 2005 to 2010, while it was 2.5%-4.8%14-16 before 2005. Most studies in South Central Asia were conducted in Iran. The prevalence of GERD in Iran was 6.3%-18.3%17-20 from 2005 to 2010, which seemed more prevalent than in Eastern Asia. Before 2005, 2 population-based studies from this country with different definitions of GERD also showed similar results.21,22 On the other hand, the time trend of GERD prevalence showed drastic change between 2 cross-sectional surveys of the general population in Singapore in Southeastern Asia. The first survey which was held in 1994 showed the prevalence of GERD by at least monthly symptoms to be around 5.5% ± 1.5%, while it has increased to 10.5% ± 2.0% after 5 years (OR, 2.2; 95% CI, 1.0-5.2; P = 0.05).23 However, the sample size of this study was relatively small and this increased result might also have been attributed to the increased awareness.
Figure.
The prevalence of gastroesophageal reflux disease in Asian population-based study. Gastroesophageal reflux disease (GERD) is defined as having heartburn or acid regurgitation at least weekly. *Study conducted in subjects with medical check-up, **GERD, retrosternal burning sensation or acid regurgitation at least once a month.
The prevalence in Western Asia was found to be the highest among the whole Asian region as represented by 20% in Turkey. One population-based study performed in Israel (2007) also reported the high prevalence of GERD symptoms, including 6.5% of retrosternal burning, 5.2% of retrosternal pain, 10.4% of acid taste in the mouth and 7.9% of the reflux of gastric contents.24
Prevalence of Endoscopic Reflux Esophagitis
The list of studies published regarding the prevalence of endoscopic reflux esophagitis is summarized in Tables 2 and 3. Most endoscopy-based studies were conducted with medical check-up participants or patients having upper gastrointestinal symptoms who visited the referral hospitals. Most of the GERD endoscopic studies were consisted of Eastern Asian studies including Japan, China and Korea. The prevalence of endoscopic reflux esophagitis in Eastern Asia was 3.4%-5.0%25,26 before 2000, with these 2 studies using the definition of reflux esophagitis by Savary-Miller classification, while other 9 studies showed results of 6.6%-15.0%27-31 from 2000 to 2005 and 4.3%-15.7%32-35 after 2005, with the definition by LA classification. However, it is quite uncertain why such a wide range of prevalence has been found for endoscopic reflux esophagitis. There might be some variability in interpreting the endoscopic findings. Furthermore, several studies were conducted in retrospective manner and might have under- or over-estimated the exact prevalence of endoscopic reflux esophagitis.
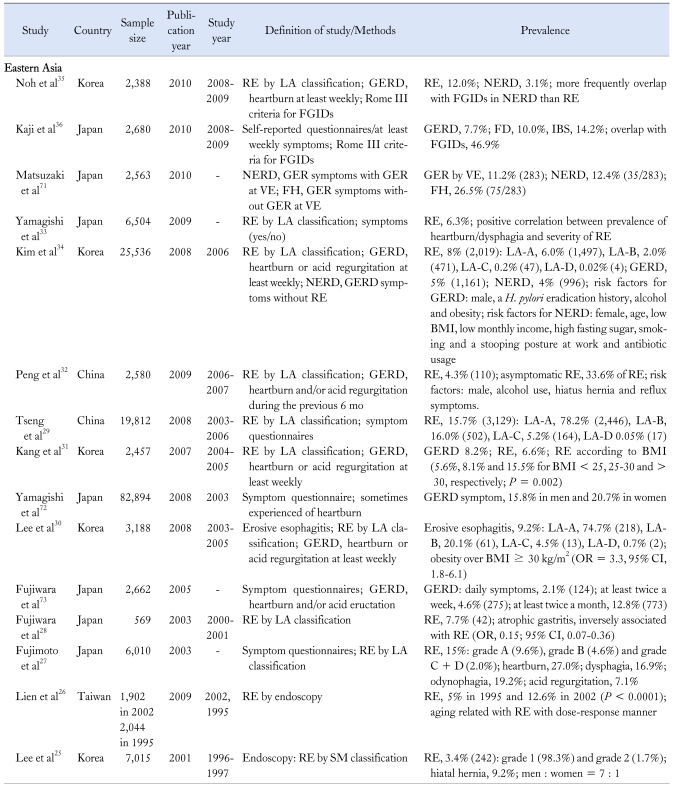
Table 2.
Epidemiology of Gastroesophageal Reflux Disease in Asian Medical Check-up People
RE, reflux esophagitis; LA, Los Angeles; GERD, gastroesophageal reflux disease; FGID, functional gastrointestinal disorder; NERD, non-erosive reflux disease; VE, videoesophagography; FH, functional heartburn; SM, Savary-Miller; FD, functional dyspepsia; IBS, irritable bowel syndrome; H. pylori, Helicobacter pylori.
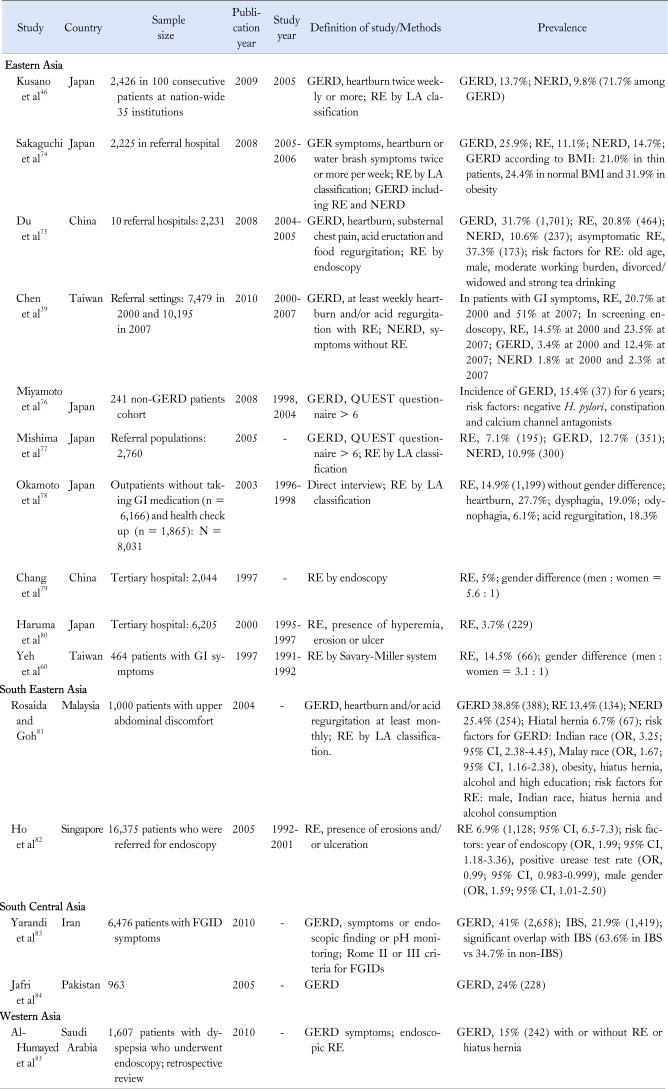
Table 3.
Epidemiology of Gastroesophageal Reflux Disease in Asian Referral Hospital
GERD, gastroesophageal reflux disease; GI, gastrointestinal; FGID, functional gastrointestinal disorder; RE, Reflux esophagitis; LA, Los Angeles; NERD, non-erosive reflux disease; QUEST, questionnaire for the diagnosis of reflux esophagitis; BMI, body mass index; H. pylori, Helicobacter pylori; IBS, irritable bowel syndrome.
The intensity and frequency of reflux induced symptoms are poor predictors for finding the presence or the severity of endoscopic mucosal breaks (erosion or ulcer). In the medical check-up studies, the prevalence of GERD based on symptoms like heartburn or acid regurgitations at least once a week was 5.0%-8.2%,31,34,36 which were similar with those of population-based studies.
Asymptomatic reflux esophagitis was reported in 33.6%-84.0% among the subjects with reflux esophagitis.32,34 This finding might be a true reflection of community or caused by the possible over-diagnosis of endoscopic reflux esophagitis by including mild reflux esophagitis or minimal changes.
Non-erosive reflux disease (NERD) has been commonly defined as the presence of classic GERD symptoms in the absence of esophageal mucosal injury which has been detected during the upper endoscopy.37 NERD is considered as the major subcategory of GERD, which has been assumed with an increasingly important role. The prevalence of NERD in medical check-up studies was reported from 3.1% to 4.0%, comprising about 70%-80% of GERD.34,35 Most studies using questionnaires might have over-estimated the prevalence of NERD because their questions might have failed to distinguish the functional heartburn.38 More precise data regarding the epidemiology of NERD are needed.
In referral hospital settings, the prevalence of GERD showed wide range results as followings: 12.4%-31.7% of symptom-based GERD, 2.3%-14.7% of NERD and 7.1%-20.8% of endoscopic reflux esophagitis. In a time trend study in Chinese tertiary hospitals from 2000 to 2007, the prevalence of endoscopic reflux esophagitis increased from 20.7% to 51.0% with the increased numbers of undergoing endoscopy secondary to GERD from 4.9% in 2000 to 14.1% in 2007. However, the prevalence of concomitant GERD symptoms did not significantly change (range, 13.0%-15.1%) in screening endoscopic studies with no significant interval change in the prevalence of NERD.39 Therefore, those authors have suggested that the actual increase in the prevalence of endoscopic reflux esophagitis might be the result of the increased demand for endoscopic investigation of GERD symptoms in some populations, or the better recognition of reflux esophagitis by endoscopists.
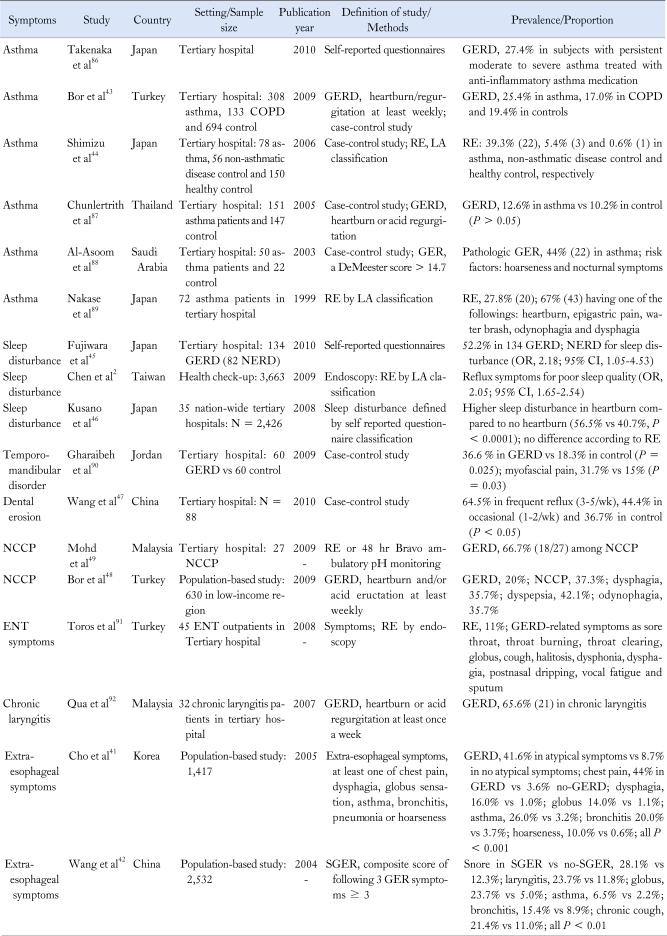
Prevalence of Extra-esophageal Syndromes
Although typical manifestations of GERD are heartburn or acid regurgitation, atypical or extra-esophageal symptoms might also be presented including respiratory symptoms, such as chronic cough, asthma or laryngitis, dental erosions, non-cardiac chest pain (NCCP), sleep disturbance and so on.40 These syndromes are usually considered to be multifactorial with GERD as one of the several potential aggravating cofactors.1 Extra-esophageal syndromes rarely occur with concomitant manifestations of the typical esophageal syndrome. Upper endoscopy and ambulatory pH monitoring were used to diagnose reflux in patients with atypical gastroesophageal reflux symptoms, however, these studies have been proved to have poor diagnostic yield.
Extra-esophageal syndromes of GERD in Asia are summarized in Table 4. These data showed a wide range of prevalence or proportion because of the different definition of disease and different conditions of each study.
Table 4.
Extra-esophageal Syndrome of Gastroesophageal Reflux Disease in Asia
NCCP, non-cardiac chest pain; ENT, ear, nose and throat; COPD, chronic obstructive pulmonary disease; GERD, gastroesophageal reflux disease; NERD, non-erosive reflux disease; RE, reflux esophagitis; LA, Los Angeles; SGER, symptomatic gastroesophageal reflux.
Two population-based studies in Asia have demonstrated the association between extra-esophageal syndrome and GERD.41,42 The proportion of GERD was significantly higher in subjects with atypical symptoms than in controls (41.6% vs 8.7%, P < 0.05).41 Symptoms as chest pain, dysphagia, globus, asthma, bronchitis, chronic cough and hoarseness were more frequently associated with GERD than controls.42
Both asthma and GERD are common conditions and they often coexist. However, several Western epidemiologic studies have revealed that asthma had been found more frequently in subjects with GERD than the general population.1 The prevalence of GERD was higher in the asthma group compared with controls in one large scale study (n = 1,135), performed in Turkey (25.4% vs 19.4%, P < 0.05).43 The proportion of endoscopic reflux esophagitis in patients with asthma was also higher than controls.44 There have been several studies demonstrating the association between sleep disturbance and GERD. The proportion of sleep dysfunction was 52.5%-56.6% among the patients with GERD, and GERD increased the OR of sleep disturbance to about twice than controls.2,45,46
Dental erosion is an acid-induced loss of dental hard tissue without the involvement of bacteria. Direct contact of regurgitated gastric acid is considered to be the main mechanism of dental erosion in patients with GERD.47 In tertiary hospitals, dental erosions were found in 64.5% among patients with frequent reflux symptoms (3-5 times/wk), 44.4% among subjects with occasional symptoms (1-2 times/wk) and 36.7% among controls (P < 0.05).47
NCCP is a heterogeneous and complex disorder with many potential causes including GERD. NCCP has been common in Asia48 and GERD has also been frequently detected in NCCP, even though the proportions were different according to the diagnostic modalities.48,49
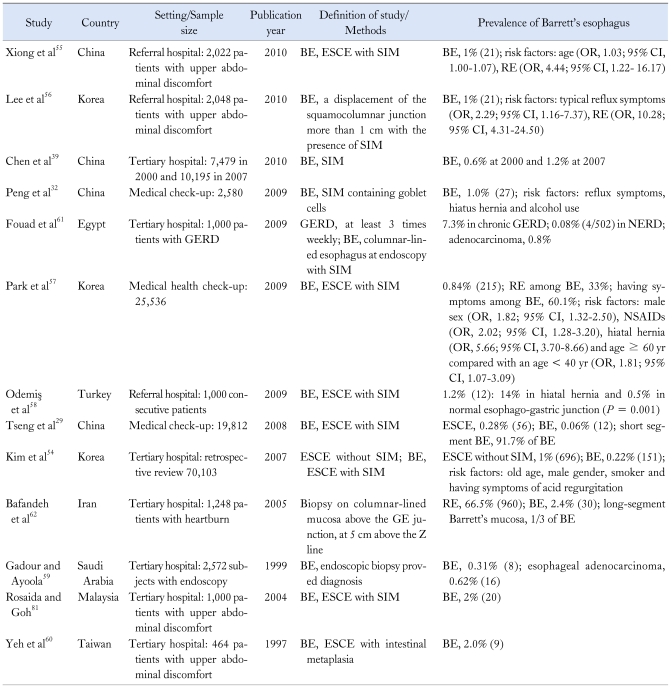
Prevalence of Barrett's Esophagus
Barrett's esophagus is histologically confirmed by specialized intestinal metaplasia.50,51 It is considered to be one of the most important complications of GERD due to its strong association with adenocarcinoma. However, epidemiologic studies have consistently reported that the prevalence of Barrett's esophagus-associated adenocarcinoma is very rare in Asia.52,53 The prevalence of Barrett's esophagus was reported as 0.06%-0.84%29,54 in medical check-up and 0.31%-2.00%39,55-60 in the referral hospital settings (Table 5). The proportion of Barrett's esophagus was 7.3%61 in patients with GERD and 2.4%62 in those with heartburn symptoms. Importantly, esophageal adenocarcinoma is often found even without any medical history of reflux symptoms.63 Although GERD symptoms is considered to be one of the most important risk factors of Barrett's esophagus,54-56 only 60.1% of subjects who had received the medical check-up were found to have GERD symptoms.57
Table 5.
Epidemiology of Barrett's Esophagus in Asia
GERD, gastroesophageal reflux disease; BE, Barrett's esophagus; ESCE, endoscopic suspected columnar epithelium; SIM, specialized intestinal metaplasia; RE, reflux esophagitis; NERD, non-erosive reflux disease.
In the Western world, esophageal adenocarcinoma has become one of the increasing cancers, in parallel with the increased prevalence of GERD and its major determinant, obesity.64,65 Such increase in the occurrence of Barrett's esophagus has not yet been observed in Asia. Epidemiologic changes of GERD in Asia seem to be correlated with economic or environmental effects, Helicobacter pylori infections, nutritional changes, and also the geographic and ethnic differences.53,66 The general low-fat diet of Asian, their smaller body mass and also their higher prevalence of Helicobacter pylori might be related with the lower prevalence of GERD compared to Western peoples.53 However, their rapid economic growth, changes of eating habits and also the growing number of obesity in people would induce many changes in the epidemiology of Barrett's esophagus and esophageal adenocarcinoma in the future.
In conclusion, many robust studies about GERD in Asia have been published during recent decades. Population-based studies showed that the prevalence of GERD has been increased in Eastern Asia, but still lower than those of the Western population. The prevalence of GERD in Southeast and Western Asia was higher than in Eastern Asia. The prevalence of endoscopic reflux esophagitis in Eastern Asia seemed to increase in participants who have received the medical check-up. In Asia, only few and limited studies have been reported regarding the proportion of extra-esophageal syndromes such as asthma, sleep disturbance, non-cardiac chest pain and dental erosion, which was found to be significantly higher in the GERD patient group than controls. On the other hand, the prevalence of Barrett's esophagus was found to be relatively low.
Based on the distinct genetic characteristics compared from the Western people, and rapid changes of socio-economic environments, this kind of study observing and investigating the epidemiologic changes of GERD in Asia would be a good model to understand the underlying pathogenesis of GERD.
Footnotes
Financial support: None.
Conflicts of interest: None.
References
- 1.Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900–1920. doi: 10.1111/j.1572-0241.2006.00630.x. [DOI] [PubMed] [Google Scholar]
- 2.Chen MJ, Wu MS, Lin JT, et al. Gastroesophageal reflux disease and sleep quality in a Chinese population. J Formos Med Assoc. 2009;108:53–60. doi: 10.1016/S0929-6646(09)60032-2. [DOI] [PubMed] [Google Scholar]
- 3.Kang JY. Systematic review: geographical and ethnic differences in gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2004;20:705–717. doi: 10.1111/j.1365-2036.2004.02165.x. [DOI] [PubMed] [Google Scholar]
- 4.El-Serag HB. Time trends of gastroesophageal reflux disease: a systematic review. Clin Gastroenterol Hepatol. 2007;5:17–26. doi: 10.1016/j.cgh.2006.09.016. [DOI] [PubMed] [Google Scholar]
- 5.Fock KM, Talley NJ, Fass R, et al. Asia-Pacific consensus on the management of gastroesophageal reflux disease: update. J Gastroenterol Hepatol. 2008;23:8–22. doi: 10.1111/j.1440-1746.2007.05249.x. [DOI] [PubMed] [Google Scholar]
- 6.Goh KL, Chang CS, Fock KM, Ke M, Park HJ, Lam SK. Gastrooesophageal reflux disease in Asia. J Gastroenterol Hepatol. 2000;15:230–238. doi: 10.1046/j.1440-1746.2000.02148.x. [DOI] [PubMed] [Google Scholar]
- 7.GLOBOCAN 2008: Cancer incidence and mortality worldwide in 2008. International agency for research on cancer. 2008. Available from http://globocan.iarc.fr.
- 8.He J, Ma X, Zhao Y, et al. A population-based survey of the epidemiology of symptom-defined gastroesophageal reflux disease: the Systematic Investigation of Gastrointestinal Diseases in China. BMC Gastroenterol. 2010;10:94. doi: 10.1186/1471-230X-10-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang R, Yan X, Ma XQ, et al. Burden of gastroesophageal reflux disease in Shanghai, China. Dig Liver Dis. 2009;41:110–115. doi: 10.1016/j.dld.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 10.Lee SY, Lee KJ, Kim SJ, Cho SW. Prevalence and risk factors for overlaps between gastroesophageal reflux disease, dyspepsia, and irritable bowel syndrome: a population-based study. Digestion. 2009;79:196–201. doi: 10.1159/000211715. [DOI] [PubMed] [Google Scholar]
- 11.Yang SY, Lee OY, Bak YT, et al. Prevalence of gastroesophageal reflux disease symptoms and uninvestigated dyspepsia in Korea: a population-based study. Dig Dis Sci. 2008;53:188–193. doi: 10.1007/s10620-007-9842-0. [DOI] [PubMed] [Google Scholar]
- 12.Li YM, Du J, Zhang H, Yu CH. Epidemiological investigation in outpatients with symptomatic gastroesophageal reflux from the Department of Medicine in Zhejiang Province, east China. J Gastroenterol Hepatol. 2008;23:283–289. doi: 10.1111/j.1440-1746.2007.05045.x. [DOI] [PubMed] [Google Scholar]
- 13.Chen M, Xiong L, Chen H, Xu A, He L, Hu P. Prevalence, risk factors and impact of gastroesophageal reflux disease symptoms: a population-based study in South China. Scand J Gastroenterol. 2005;40:759–767. doi: 10.1080/00365520510015610. [DOI] [PubMed] [Google Scholar]
- 14.Wong WM, Lai KC, Lam KF, et al. Prevalence, clinical spectrum and health care utilization of gastro-oesophageal reflux disease in a Chinese population: a population-based study. Aliment Pharmacol Ther. 2003;18:595–604. doi: 10.1046/j.1365-2036.2003.01737.x. [DOI] [PubMed] [Google Scholar]
- 15.Jeong JJ, Choi MG, Cho YS, et al. Chronic gastrointestinal symptoms and quality of life in the Korean population. World J Gastroenterol. 2008;14:6388–6394. doi: 10.3748/wjg.14.6388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cheung TK, Lam KF, Hu WH, et al. Positive association between gastro-oesophageal reflux disease and irritable bowel syndrome in a Chinese population. Aliment Pharmacol Ther. 2007;25:1099–1104. doi: 10.1111/j.1365-2036.2007.03304.x. [DOI] [PubMed] [Google Scholar]
- 17.Solhpour A, Pourhoseingholi MA, Soltani F, et al. Gastro-esophageal reflux symptoms and body mass index: no relation among the Iranian population. Indian J Gastroenterol. 2008;27:153–155. [PubMed] [Google Scholar]
- 18.Nasseri-Moghaddam S, Mofid A, Ghotbi MH, et al. Epidemiological study of gastro-oesophageal reflux disease: reflux in spouse as a risk factor. Aliment Pharmacol Ther. 2008;28:144–153. doi: 10.1111/j.1365-2036.2008.03708.x. [DOI] [PubMed] [Google Scholar]
- 19.Somi MH, Farhang S, Mirinezhad K, et al. Prevalence and precipitating factors of gastroesophageal reflux disease in a young population of Tabriz, Northwest of Iran. Saudi Med J. 2006;27:1878–1881. [PubMed] [Google Scholar]
- 20.Nouraie M, Razjouyan H, Assady M, Malekzadeh R, Nasseri-Moghaddam S. Epidemiology of gastroesophageal reflux symptoms in Tehran, Iran: a population-based telephone survey. Arch Iran Med. 2007;10:289–294. [PubMed] [Google Scholar]
- 21.Saberi-Firoozi M, Khademolhosseini F, Yousefi M, Mehrabani D, Zare N, Heydari ST. Risk factors of gastroesophageal reflux disease in Shiraz, southern Iran. World J Gastroenterol. 2007;13:5486–5491. doi: 10.3748/wjg.v13.i41.5486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ehsani MJ, Maleki I, Mohammadzadeh F, Mashayekh A. Epidemiology of gastroesophageal reflux disease in Tehran, Iran. J Gastroenterol Hepatol. 2007;22:1419–1422. doi: 10.1111/j.1440-1746.2006.04616.x. [DOI] [PubMed] [Google Scholar]
- 23.Lim SL, Goh WT, Lee JM, Ng TP, Ho KY Community Medicine GI Study Group. Changing prevalence of gastroesophageal reflux with changing time: longitudinal study in an Asian population. J Gastroenterol Hepatol. 2005;20:995–1001. doi: 10.1111/j.1440-1746.2005.03887.x. [DOI] [PubMed] [Google Scholar]
- 24.Sperber AD, Halpern Z, Shvartzman P, et al. Prevalence of GERD symptoms in a representative Israeli adult population. J Clin Gastroenterol. 2007;41:457–461. doi: 10.1097/01.mcg.0000225664.68920.96. [DOI] [PubMed] [Google Scholar]
- 25.Lee SJ, Song CW, Jeen YT, et al. Prevalence of endoscopic reflux esophagitis among Koreans. J Gastroenterol Hepatol. 2001;16:373–376. doi: 10.1046/j.1440-1746.2001.02464.x. [DOI] [PubMed] [Google Scholar]
- 26.Lien HC, Chang CS, Yeh HZ, et al. Increasing prevalence of erosive esophagitis among Taiwanese aged 40 years and above: a comparison between two time periods. J Clin Gastroenterol. 2009;43:926–932. doi: 10.1097/MCG.0b013e318191e9d5. [DOI] [PubMed] [Google Scholar]
- 27.Fujimoto K, Iwakiri R, Okamoto K, et al. Characteristics of gastroesophageal reflux disease in Japan: increased prevalence in elderly women. J Gastroenterol. 2003;38(Suppl 15):3–6. [PubMed] [Google Scholar]
- 28.Fujiwara Y, Higuchi K, Shiba M, et al. Association between gastroesophageal flap valve, reflux esophagitis, Barrett's epithelium, and atrophic gastritis assessed by endoscopy in Japanese patients. J Gastroenterol. 2003;38:533–539. doi: 10.1007/s00535-002-1100-9. [DOI] [PubMed] [Google Scholar]
- 29.Tseng PH, Lee YC, Chiu HM, et al. Prevalence and clinical characteristics of Barrett's esophagus in a Chinese general population. J Clin Gastroenterol. 2008;42:1074–1079. doi: 10.1097/MCG.0b013e31809e7126. [DOI] [PubMed] [Google Scholar]
- 30.Lee HL, Eun CS, Lee OY, et al. Association between GERD-related erosive esophagitis and obesity. J Clin Gastroenterol. 2008;42:672–675. doi: 10.1097/MCG.0b013e31806daf64. [DOI] [PubMed] [Google Scholar]
- 31.Kang MS, Park DI, Oh SY, et al. Abdominal obesity is an independent risk factor for erosive esophagitis in a Korean population. J Gastroenterol Hepatol. 2007;22:1656–1661. doi: 10.1111/j.1440-1746.2006.04518.x. [DOI] [PubMed] [Google Scholar]
- 32.Peng S, Cui Y, Xiao YL, et al. Prevalence of erosive esophagitis and Barrett's esophagus in the adult Chinese population. Endoscopy. 2009;41:1011–1017. doi: 10.1055/s-0029-1215291. [DOI] [PubMed] [Google Scholar]
- 33.Yamagishi H, Koike T, Ohara S, et al. Clinical characteristics of gastroesophageal reflux disease in Japan. Hepatogastroenterology. 2009;56:1032–1034. [PubMed] [Google Scholar]
- 34.Kim N, Lee SW, Cho SI, et al. The prevalence of and risk factors for erosive oesophagitis and non-erosive reflux disease: a nationwide multicentre prospective study in Korea. Aliment Pharmacol Ther. 2008;27:173–185. doi: 10.1111/j.1365-2036.2007.03561.x. [DOI] [PubMed] [Google Scholar]
- 35.Noh YW, Jung HK, Kim SE, Jung SA. Overlap of erosive and non-erosive reflux diseases with functional gastrointestinal disorders according to Rome III criteria. J Neurogastroenterol Motil. 2010;16:148–156. doi: 10.5056/jnm.2010.16.2.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kaji M, Fujiwara Y, Shiba M, et al. Prevalence of overlaps between GERD, FD and IBS and impact on health-related quality of life. J Gastroenterol Hepatol. 2010;25:1151–1156. doi: 10.1111/j.1440-1746.2010.06249.x. [DOI] [PubMed] [Google Scholar]
- 37.Hershcovici T, Fass R. Nonerosive reflux disease (NERD) - an update. J Neurogastroenterol Motil. 2010;16:8–21. doi: 10.5056/jnm.2010.16.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Modlin IM, Hunt RH, Malfertheiner P, et al. Non-erosive reflux disease - defining the entity and delineating the management. Digestion. 2008;78(Suppl 1):1–5. doi: 10.1159/000151248. [DOI] [PubMed] [Google Scholar]
- 39.Chen MJ, Lee YC, Chiu HM, Wu MS, Wang HP, Lin JT. Time trends of endoscopic and pathological diagnoses related to gastroesophageal reflux disease in a Chinese population: eight years single institution experience. Dis Esophagus. 2010;23:201–207. doi: 10.1111/j.1442-2050.2009.01012.x. [DOI] [PubMed] [Google Scholar]
- 40.Koop H, Schepp W, Müller-Lissner S, et al. Consensus conference of the DGVS on gastroesophageal reflux. Z Gastroenterol. 2005;43:163–164. doi: 10.1055/s-2005-857870. [DOI] [PubMed] [Google Scholar]
- 41.Cho YS, Choi MG, Jeong JJ, et al. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Asan-si, Korea. Am J Gastroenterol. 2005;100:747–753. doi: 10.1111/j.1572-0241.2005.41245.x. [DOI] [PubMed] [Google Scholar]
- 42.Wang JH, Luo JY, Dong L, Gong J, Tong M. Epidemiology of gastroesophageal reflux disease: a general population-based study in Xi'an of Northwest China. World J Gastroenterol. 2004;10:1647–1651. doi: 10.3748/wjg.v10.i11.1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bor S, Kitapcioglu G, Solak ZA, Ertilav M, Erdinc M. Prevalence of gastroesophageal reflux disease in patients with asthma and chronic obstructive pulmonary disease. J Gastroenterol Hepatol. 2010;25:309–313. doi: 10.1111/j.1440-1746.2009.06035.x. [DOI] [PubMed] [Google Scholar]
- 44.Shimizu Y, Dobashi K, Kobayashi S, et al. High prevalence of gastroesophageal reflux disease with minimal mucosal change in asthmatic patients. Tohoku J Exp Med. 2006;209:329–336. doi: 10.1620/tjem.209.329. [DOI] [PubMed] [Google Scholar]
- 45.Fujiwara Y, Kohata Y, Kaji M, et al. Sleep dysfunction in Japanese patients with gastroesophageal reflux disease: prevalence, risk factors, and efficacy of rabeprazole. Digestion. 2010;81:135–141. doi: 10.1159/000253849. [DOI] [PubMed] [Google Scholar]
- 46.Kusano M, Kouzu T, Kawano T, Ohara S. Nationwide epidemiological study on gastroesophageal reflux disease and sleep disorders in the Japanese population. J Gastroenterol. 2008;43:833–841. doi: 10.1007/s00535-008-2235-0. [DOI] [PubMed] [Google Scholar]
- 47.Wang GR, Zhang H, Wang ZG, Jiang GS, Guo CH. Relationship between dental erosion and respiratory symptoms in patients with gastro-oesophageal reflux disease. J Dent. 2010;38:892–898. doi: 10.1016/j.jdent.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 48.Bor S, Mandiracioglu A, Kitapcioglu G, Caymaz-Bor C, Gilbert RJ. Gastroesophageal reflux disease in a low-income region in Turkey. Am J Gastroenterol. 2005;100:759–765. doi: 10.1111/j.1572-0241.2005.41065.x. [DOI] [PubMed] [Google Scholar]
- 49.Mohd H, Qua CS, Wong CH, Azman W, Goh KL. Non-cardiac chest pain: prevalence of reflux disease and response to acid suppression in an Asian population. J Gastroenterol Hepatol. 2009;24:288–293. doi: 10.1111/j.1440-1746.2008.05702.x. [DOI] [PubMed] [Google Scholar]
- 50.Hirota WK, Loughney TM, Lazas DJ, Maydonovitch CL, Rholl V, Wong RK. Specialized intestinal metaplasia, dysplasia, and cancer of the esophagus and esophagogastric junction: prevalence and clinical data. Gastroenterology. 1999;116:277–285. doi: 10.1016/s0016-5085(99)70123-x. [DOI] [PubMed] [Google Scholar]
- 51.Spechler SJ. The columnar-lined esophagus. History, terminology, and clinical issues. Gastroenterol Clin North Am. 1997;26:455–466. doi: 10.1016/s0889-8553(05)70306-x. [DOI] [PubMed] [Google Scholar]
- 52.Tu CH, Lee CT, Perng DS, Chang CC, Hsu CH, Lee YC. Esophageal adenocarcinoma arising from Barrett's epithelium in Taiwan. J Formos Med Assoc. 2007;106:664–668. doi: 10.1016/S0929-6646(08)60024-8. [DOI] [PubMed] [Google Scholar]
- 53.Hongo M, Nagasaki Y, Shoji T. Epidemiology of esophageal cancer: Orient to Occident. Effects of chronology, geography and ethnicity. J Gastroenterol Hepatol. 2009;24:729–735. doi: 10.1111/j.1440-1746.2009.05824.x. [DOI] [PubMed] [Google Scholar]
- 54.Kim JH, Rhee PL, Lee JH, et al. Prevalence and risk factors of Barrett's esophagus in Korea. J Gastroenterol Hepatol. 2007;22:908–912. doi: 10.1111/j.1440-1746.2006.04448.x. [DOI] [PubMed] [Google Scholar]
- 55.Xiong LS, Cui Y, Wang JP, et al. Prevalence and risk factors of Barrett's esophagus in patients undergoing endoscopy for upper gastrointestinal symptoms. J Dig Dis. 2010;11:83–87. doi: 10.1111/j.1751-2980.2010.00419.x. [DOI] [PubMed] [Google Scholar]
- 56.Lee IS, Choi SC, Shim KN, et al. Prevalence of Barrett's esophagus remains low in the Korean population: nationwide cross-sectional prospective multicenter study. Dig Dis Sci. 2010;55:1932–1939. doi: 10.1007/s10620-009-0984-0. [DOI] [PubMed] [Google Scholar]
- 57.Park JJ, Kim JW, Kim HJ, et al. The prevalence of and risk factors for Barrett's esophagus in a Korean population: a nationwide multicenter prospective study. J Clin Gastroenterol. 2009;43:907–914. doi: 10.1097/MCG.0b013e318196bd11. [DOI] [PubMed] [Google Scholar]
- 58.Odemiş B, Ciçek B, Zengin NI, et al. Barrett's esophagus and endoscopically assessed esophagogastric junction integrity in 1000 consecutive Turkish patients undergoing endoscopy: a prospective study. Dis Esophagus. 2009;22:649–655. doi: 10.1111/j.1442-2050.2009.00982.x. [DOI] [PubMed] [Google Scholar]
- 59.Gadour MO, Ayoola EA. Barrett's oesophagus and oesophageal cancer in Saudi Arabia. Trop Gastroenterol. 1999;20:111–115. [PubMed] [Google Scholar]
- 60.Yeh C, Hsu CT, Ho AS, Sampliner RE, Fass R. Erosive esophagitis and Barrett's esophagus in Taiwan: a higher frequency than expected. Dig Dis Sci. 1997;42:702–706. doi: 10.1023/a:1018835324210. [DOI] [PubMed] [Google Scholar]
- 61.Fouad YM, Makhlouf MM, Tawfik HM, el-Amin H, Ghany WA, el-Khayat HR. Barrett's esophagus: prevalence and risk factors in patients with chronic GERD in Upper Egypt. World J Gastroenterol. 2009;15:3511–3515. doi: 10.3748/wjg.15.3511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bafandeh Y, Esmaili H, Aharizad S. Endoscopic and histologic findings in Iranian patients with heartburn. Indian J Gastroenterol. 2005;24:236–238. [PubMed] [Google Scholar]
- 63.Bytzer P, Christensen PB, Damkier P, Vinding K, Seersholm N. Adenocarcinoma of the esophagus and Barrett's esophagus: a population-based study. Am J Gastroenterol. 1999;94:86–91. doi: 10.1111/j.1572-0241.1999.00776.x. [DOI] [PubMed] [Google Scholar]
- 64.Blot WJ, Devesa SS, Kneller RW, Fraumeni JF., Jr Rising incidence of adenocarcinoma of the esophagus and gastric cardia. JAMA. 1991;265:1287–1289. [PubMed] [Google Scholar]
- 65.Devesa SS, Blot WJ, Fraumeni JF., Jr Changing patterns in the incidence of esophageal and gastric carcinoma in the United States. Cancer. 1998;83:2049–2053. [PubMed] [Google Scholar]
- 66.Blaser MJ. Hypothesis: the changing relationships of Helicobacter pylori and humans: implications for health and disease. J Infect Dis. 1999;179:1523–1530. doi: 10.1086/314785. [DOI] [PubMed] [Google Scholar]
- 67.Ma XQ, Cao Y, Wang R, et al. Prevalence of, and factors associated with, gastroesophageal reflux disease: a population-based study in Shanghai, China. Dis Esophagus. 2009;22:317–322. doi: 10.1111/j.1442-2050.2008.00904.x. [DOI] [PubMed] [Google Scholar]
- 68.Ho KY, Kang JY, Seow A. Prevalence of gastrointestinal symptoms in a multiracial Asian population, with particular reference to reflux-type symptoms. Am J Gastroenterol. 1998;93:1816–1822. doi: 10.1111/j.1572-0241.1998.00526.x. [DOI] [PubMed] [Google Scholar]
- 69.Mostaghni A, Mehrabani D, Khademolhosseini F, et al. Prevalence and risk factors of gastroesophageal reflux disease in Qashqai migrating nomads, southern Iran. World J Gastroenterol. 2009;15:961–965. doi: 10.3748/wjg.15.961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kitapçioğlu G, Mandiracioğlu A, Caymaz Bor C, Bor S. Overlap of symptoms of dyspepsia and gastroesophageal reflux in the community. Turk J Gastroenterol. 2007;18:14–19. [PubMed] [Google Scholar]
- 71.Matsuzaki J, Suzuki H, Iwasaki E, Yokoyama H, Sugino Y, Hibi T. Serum lipid levels are positively associated with non-erosive reflux disease, but not with functional heartburn. Neurogastroenterol Motil. 2010;22:965–970. e251. doi: 10.1111/j.1365-2982.2010.01518.x. [DOI] [PubMed] [Google Scholar]
- 72.Yamagishi H, Koike T, Ohara S, et al. Prevalence of gastroesophageal reflux symptoms in a large unselected general population in Japan. World J Gastroenterol. 2008;14:1358–1364. doi: 10.3748/wjg.14.1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Fujiwara Y, Higuchi K, Watanabe Y, et al. Prevalence of gastroesophageal reflux disease and gastroesophageal reflux disease symptoms in Japan. J Gastroenterol Hepatol. 2005;20:26–29. doi: 10.1111/j.1440-1746.2004.03521.x. [DOI] [PubMed] [Google Scholar]
- 74.Sakaguchi M, Oka H, Hashimoto T, et al. Obesity as a risk factor for GERD in Japan. J Gastroenterol. 2008;43:57–62. doi: 10.1007/s00535-007-2128-7. [DOI] [PubMed] [Google Scholar]
- 75.Du J, Liu J, Zhang H, Yu CH, Li YM. Risk factors for gastroesophageal reflux disease, reflux esophagitis and non-erosive reflux disease among Chinese patients undergoing upper gastrointestinal endoscopic examination. World J Gastroenterol. 2007;13:6009–6015. doi: 10.3748/wjg.v13.45.6009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Miyamoto M, Haruma K, Kuwabara M, Nagano M, Okamoto T, Tanaka M. High incidence of newly-developed gastroesophageal reflux disease in the Japanese community: a 6-year follow-up study. J Gastroenterol Hepatol. 2008;23:393–397. doi: 10.1111/j.1440-1746.2007.05043.x. [DOI] [PubMed] [Google Scholar]
- 77.Mishima I, Adachi K, Arima N, et al. Prevalence of endoscopically negative and positive gastroesophageal reflux disease in the Japanese. Scand J Gastroenterol. 2005;40:1005–1009. doi: 10.1080/00365520510023260. [DOI] [PubMed] [Google Scholar]
- 78.Okamoto K, Iwakiri R, Mori M, et al. Clinical symptoms in endoscopic reflux esophagitis: evaluation in 8031 adult subjects. Dig Dis Sci. 2003;48:2237–2241. doi: 10.1023/b:ddas.0000007857.15694.15. [DOI] [PubMed] [Google Scholar]
- 79.Chang CS, Poon SK, Lien HC, Chen GH. The incidence of reflux esophagitis among the Chinese. Am J Gastroenterol. 1997;92:668–671. [PubMed] [Google Scholar]
- 80.Haruma K, Hamada H, Mihara M, et al. Negative association between Helicobacter pylori infection and reflux esophagitis in older patients: case-control study in Japan. Helicobacter. 2000;5:24–29. doi: 10.1046/j.1523-5378.2000.00003.x. [DOI] [PubMed] [Google Scholar]
- 81.Rosaida MS, Goh KL. Gastro-oesophageal reflux disease, reflux oesophagitis and non-erosive reflux disease in a multiracial Asian population: a prospective, endoscopy based study. Eur J Gastroenterol Hepatol. 2004;16:495–501. doi: 10.1097/00042737-200405000-00010. [DOI] [PubMed] [Google Scholar]
- 82.Ho KY, Chan YH, Kang JY. Increasing trend of reflux esophagitis and decreasing trend of Helicobacter pylori infection in patients from a multiethnic Asian country. Am J Gastroenterol. 2005;100:1923–1928. doi: 10.1111/j.1572-0241.2005.50138.x. [DOI] [PubMed] [Google Scholar]
- 83.Yarandi SS, Nasseri-Moghaddam S, Mostajabi P, Malekzadeh R. Overlapping gastroesophageal reflux disease and irritable bowel syndrome: increased dysfunctional symptoms. World J Gastroenterol. 2010;16:1232–1238. doi: 10.3748/wjg.v16.i9.1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Jafri N, Yakoob J, Islam M, Manzoor S, Jalil A, Hashmi F. Perception of gastroesophageal reflux disease in urban population in Pakistan. J Coll Physicians Surg Pak. 2005;15:532–534. [PubMed] [Google Scholar]
- 85.Al-Humayed SM, Mohamed-Elbagir AK, Al-Wabel AA, Argobi YA. The changing pattern of upper gastro-intestinal lesions in southern Saudi Arabia: an endoscopic study. Saudi J Gastroenterol. 2010;16:35–37. doi: 10.4103/1319-3767.58766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Takenaka R, Matsuno O, Kitajima K, et al. The use of frequency scale for the symptoms of GERD in assessment of gastro-oesophageal reflex symptoms in asthma. Allergol Immunopathol (Madr) 2010;38:20–24. doi: 10.1016/j.aller.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 87.Chunlertrith K, Boonsawat W, Zaeoue U. Prevalence of gastroesophageal reflux symptoms in asthma patients at Srinagarind Hospital. J Med Assoc Thai. 2005;88:668–671. [PubMed] [Google Scholar]
- 88.Al-Asoom L, Al-Rubaish AM, El-Munshid HA, Al-Nafaie AN, Bukharie HA, Abdulrahman IS. Gastroesophageal reflux in bronchial asthma patients. A clinical note. Saudi Med J. 2003;24:1364–1369. [PubMed] [Google Scholar]
- 89.Nakase H, Itani T, Mimura J, et al. Relationship between asthma and gastro-oesophageal reflux: significance of endoscopic grade of reflux oesophagitis in adult asthmatics. J Gastroenterol Hepatol. 1999;14:715–722. doi: 10.1046/j.1440-1746.1999.01939.x. [DOI] [PubMed] [Google Scholar]
- 90.Gharaibeh TM, Jadallah K, Jadayel FA. Prevalence of temporomandibular disorders in patients with gastroesophageal reflux disease: a case-controlled study. J Oral Maxillofac Surg. 2010;68:1560–1564. doi: 10.1016/j.joms.2009.06.027. [DOI] [PubMed] [Google Scholar]
- 91.Toros SZ, Toros AB, Yüksel OD, Ozel L, Akkaynak C, Naiboglu B. Association of laryngopharyngeal manifestations and gastroesophageal reflux. Eur Arch Otorhinolaryngol. 2009;266:403–409. doi: 10.1007/s00405-008-0761-2. [DOI] [PubMed] [Google Scholar]
- 92.Qua CS, Wong CH, Gopala K, Goh KL. Gastro-oesophageal reflux disease in chronic laryngitis: prevalence and response to acid-suppressive therapy. Aliment Pharmacol Ther. 2007;25:287–295. doi: 10.1111/j.1365-2036.2006.03185.x. [DOI] [PubMed] [Google Scholar]