Abstract
Background/Aims
The incidence of gastroesophageal reflux disease (GERD) is increasing in Korea. The aim of this study was to evaluate the relationship between GERD symptoms and dietary factors in Korea.
Methods
From January 2007 to April 2008, 162 subjects were enrolled (81 in GERD group and 81 in control group). They were asked to complete the questionnaires about GERD symptoms and dietary habits. The symptom severity score was recorded by visual analogue scale.
Results
Subjects with overweight or obesity had an increased risk for GERD (OR, 2.52; 95% CI, 1.18-5.39). Irregular dietary intake was one of the risk factors for GERD (OR, 2.33; 95% CI, 1.11-4.89). Acid regurgitation was the most suffering (2.85 ± 2.95 by visual analogue scale) and frequent reflux-related symptom (57.5%) in GERD. Noodles (OR, 1.22; 95% CI, 1.12-1.34), spicy foods (OR, 1.09; 95% CI, 1.02-1.16), fatty meals (OR, 1.20; 95% CI, 1.09-1.33), sweets (OR, 1.42; 95% CI, 1.00-2.02), alcohol (OR, 1.16; 95% CI, 1.03-1.31), breads (OR, 1.17; 95% CI, 1.01-1.34), carbonated drinks (OR, 1.69; 95% CI, 1.04-2.74) and caffeinated drinks (OR,1.41; 95% CI, 1.15-1.73) were associated with symptom aggravation in GERD. Among the investigated noodles, ramen (instant noodle) caused reflux-related symptoms most frequently (52.4%).
Conclusions
We found that noodles, spicy foods, fatty meals, sweets, alcohol, breads, carbonated drinks and caffeinated drinks were associated with reflux-related symptoms.
Keywords: Diet, Food habits, Gastroesophageal reflux disease, Symptom
Introduction
Gastroesophageal reflux disease (GERD) is a condition which develops when the reflux of gastric contents cause troublesome symptoms and/or complications.1 A recent systematic review identified a 10%-20% prevalence of GERD, defined by at least weekly heartburn and/or regurgitation in the Western world; while in Asia, the prevalence was less than 5%.2 It has been suggested that there is an increasing trend in the prevalence of GERD over the last 2 decades and that reflux disease is more common in Asian countries than previously recognized.3 For the differences in prevalence rate in different countries, there are several potential explanations; such as lifestyle factors, dietary factors, overweight/obesity and genetic factors. However, the exact pathogenetic role of these factors is still under debate and the beneficial effect of recommending specific modification in lifestyle habits is also controversial.4
GERD is a multi-factorial disease with both environmental and genetic risk factors, and several epidemiological data lend support to this concept.5 Various lifestyle factors are thought to be associated with GERD symptoms, including body weight, nutrition, alcohol consumption, smoking, the intake of NSAIDs and sleeping position.6 There are many patients who are more likely to experience a perceived reflux event when they eat some foods like noodles. It is a common belief that some foods may induce or worsen GERD symptoms. In fact, in daily clinical practice, this belief leads to advising patients to avoid the suspected foods.7 Furthermore, since GERD symptoms are most commonly reported postprandially, the role of dietary components in inducing symptoms has been suggested.7 However, no definitive data exist regarding the role of diet and specific foods or drinks in influencing on GERD symptoms.7 The aim of this study was to evaluate the relationship between GERD symptoms and dietary factors, especially regular meals in Korea.
Materials and Methods
Subjects
From January 2007 to April 2008, patients attending department of medicine in Samsung Medical Center with frequent (more than weekly) typical reflux symptoms such as acid regurgitation or heartburn were recruited as GERD group. All of these patients underwent esophagogastroduodenoscopy (EGD) to confirm erosive esophagitis or other combined disorder. In case of erosive reflux disease, the severity of erosive esophagitis seen on EGD was graded from A to D according to the Los Angeles (LA) classification.8 In the same period, randomly selected subjects attending Seoul National University Hospital Healthcare System Gangnam Center for routine health check-up to be confirmed without erosive esophagitis or hiatal hernia by EGD were recruited as control group. Subjects with typical reflux symptoms more than once a week within the last 1 year were excluded in control group.
Subjects were excluded if they have other gastrointestinal diseases (for example, active peptic ulcer disease, infectious conditions of the intestine and gastric malignancy), a history of gastrectomy or severe health problems. Exclusion criteria also contained the subjects who require daily use of NSAIDs, oral steroid or aspirin, on proton pump inhibitors or histamine-2 receptor antagonists over the preceding 4 weeks, and currently pregnant women.
The participants were asked to complete the questionnaires consisted of questions about the patient's demographics, reflux related symptoms and diet factors. Body mass index was calculated as a ratio between weight (kg) and the square of height (m2) and further categorized as follows based on recommended cutoffs: normal (< 23), overweight or obesity (≥ 23). A total of 162 subjects (81 in GERD group and 81 in control group) agreed to complete the questionnaire and were enrolled in this study. Written informed consents were obtained from all participants. This study received approval from the institutional review board of the Samsung Medical Center and Seoul National University Hospital.
Questionnaire
The questionnaire consisted of the following questions:
(1) Questions about dietary habits (large-volume meal, rapid food intake, irregular intake, eating between meals and late-evening meal)
How much do you take each meal?
How long does it take to eat a regular meal?
Do you eat regularly?
Do you eat between meals?
Do you eat in late evening or at night?
(2) Do you suffer from the following symptoms? How often? How severe are the symptoms? (recorded by visual analogue scale [VAS])
Heartburn
Acid regurgitation
Chest discomfort
Chest pain
Hoarseness
Globus sensation
Cough
Epigastric pain
Epigastric soreness
dyspepsia
(3) How long do you suffer from the symptoms?
(4) Did you feel the symptom development or aggravation after eating specific food? What was(were) the food(s)? And how severe were the symptoms? (recorded by VAS)
Diet factors
The questionnaires also asked whether they suffered from reflux-related symptoms with specific food intake. The foods possibly causing reflux-related symptoms were listed in Korean's favorite foods extracted from the Third Korea National Health & Nutrition Examination Survey (KNHANES III).9
Symptom assessment
The severities of reflux related symptoms (heartburn, acid regurgitation, chest discomfort, chest pain, hoarseness, globus sensation, cough, epigastric pain, epigastric soreness and dyspepsia)10 were recorded by 10 cm VAS running from 0 (no symptom) to 10 (maximal symptom expression).
Statistical Methods
Statistic analysis was performed using the Student's t test and Chi-square to compare the differences between the 2 groups. Multivariate logistic regression models were used to assess the potential risk factors of GERD. Age- and sex-adjusted data of dietary habits, reflux-related symptoms and specific foods were also analyzed by multiple logistic regression. All P-values were 2-tailed, and P-values of less than 0.05 were considered statistically significant.
Results
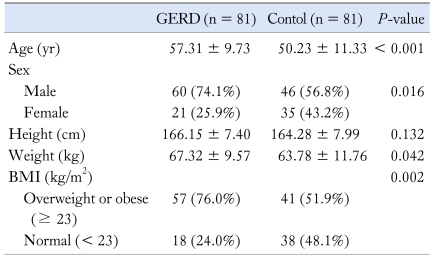
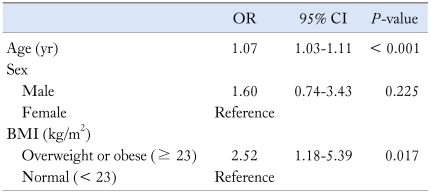
The clinical characteristics of the study subjects are presented in Table 1. Mean ages were 57 years in GERD group and 50 years in control group (P < 0.001). Subjects with overweight or obesity had an increased risk for GERD (OR, 2.52; 95% CI, 1.18-5.39) (Table 2). In GERD group, endoscopic findings were as follows; 13 patients (16.0%) had non-erosive reflux disease, 30 patients (37.0%) were LA-A, 34 patients (42.0%) were LA-B and 4 patients (5.0%) were LA-C. In our study population, there was no patient with LA-D.
Table 1.
Clinical Characteristics
GERD, gastroesophageal reflux disease; BMI, body mass index.
Continuous variables are presented as the mean ± SD and noncontinuous variables as the number (%).
Table 2.
Multivariate Analysis of Risk Factors for Gastroesophageal Reflux Disease
BMI, body mass index.
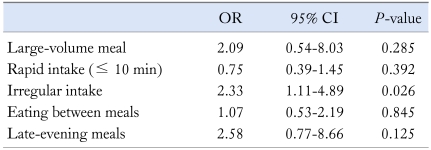
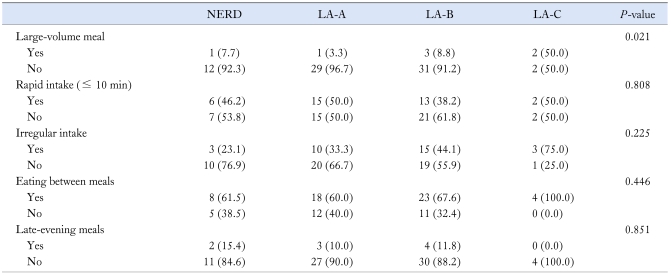
Table 3 shows the relationship between dietary habits and GERD. The odds ratio of irregular dietary intake was 2.33 (95% CI, 1.11-4.89), but other habits (large-volume meal, rapid food intake, eating between meals and late-evening meals) did not show statistical significance. Table 4 shows the comparison of dietary habits according to the endoscopic severity of GERD. Large-volume meal was significantly associated with the grade of erosive esophagitis.
Table 3.
Relationship Between Dietary Habits and Gastroesophageal Reflux Disease
It was adjusted for age and sex.
Table 4.
The Comparison of Dietary Habits According to the Endoscopic Severity of Gastroesophageal Reflux Disease
NERD, non-erosive reflux disease; LA-A, Los Angeles classification A; LA-B, Los Angeles classification B; LA-C, Los Angeles classification C.
Data are presented as the number (%).
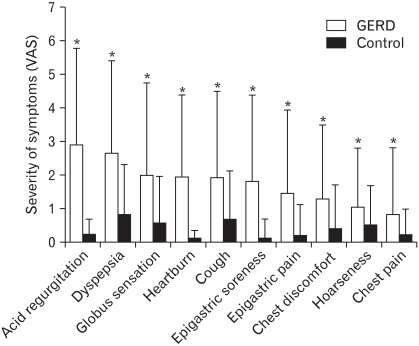
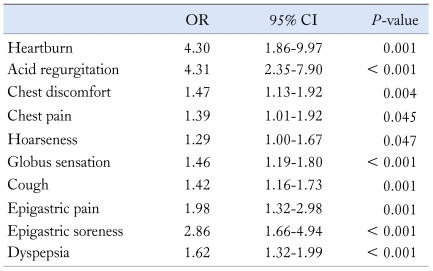
Each reflux-related symptom was assessed by severity and frequency. The severity of symptoms measured by VAS is shown in Figure 1. In GERD group, acid regurgitation was the most suffering symptom (2.85 ± 2.95), whereas dyspepsia was the most suffering symptom (0.76 ± 1.57) in control group. When the data were adjusted for age and sex, the most highly associated symptoms with GERD were acid regurgitation (OR, 4.31; 95% CI, 2.35-7.90) and heartburn (OR, 4.30; 95% CI, 1.86-9.97) (Table 5). Acid regurgitation was the most frequent symptom in GERD group (57.5%), whereas cough was most frequent in control group (16.0%).
Figure 1.
The severity of symptoms related with reflux. The severities of symptoms were measured by visual analogue scale. Acid regurgitation was the most suffering reflux related symptom in gastroesophageal reflux disease (*P < 0.05). GERD, gastroesophageal reflux disease; VAS, visual analogue scale.
Table 5.
The Relationship Between Reflux Related Symptoms and Gastroesophageal Reflux Disease
It was adjusted for age and sex.
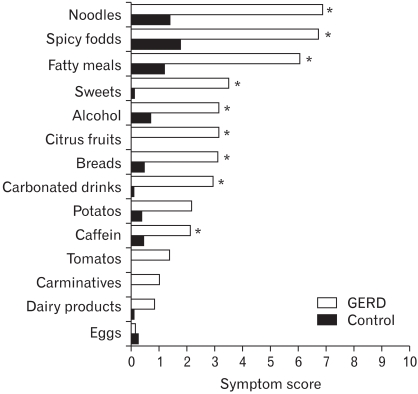
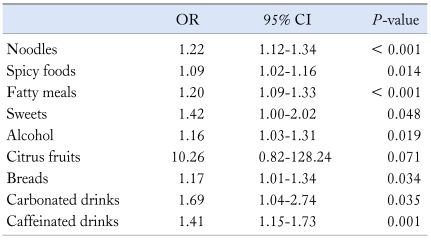
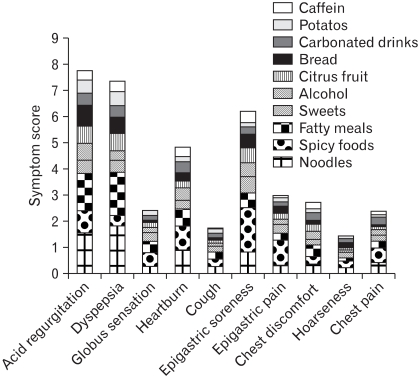
Figure 2 demonstrates several foods and their symptom severity scores in each group. Symptom severity scores were calculated by the sum of each severity (VAS scale) of symptoms. Noodles showed the highest symptom severity score in GERD group, and they were significantly higher than control group. When the data were adjusted for age and sex, noodles (OR, 1.22; 95% CI, 1.12-1.34), spicy foods (OR, 1.09; 95% CI, 1.02-1.16), fatty meals (OR, 1.20; 95% CI, 1.09-1.33), sweets (OR, 1.42; 95% CI, 1.00-2.02), alcohol (OR, 1.16; 95% CI, 1.03-1.31), breads (OR, 1.17; 95% CI, 1.01-1.34), carbonated drinks (OR, 1.69; 95% CI, 1.04-2.74) and caffeinated drinks (OR, 1.41; 95% CI, 1.15-1.74) were associated with symptom aggravation in GERD (Table 6).
Figure 2.
The specific foods and their symptom severity scores in gastroesophageal reflux disease (GERD) and control groups. Noodles, spicy foods, fatty meals, sweets, alcohol, citrus fruits, breads, carbonated drinks and caffeinated drinks were associated with significantly higher symptom severity score in GERD group (*P < 0.05).
Table 6.
The Relationship Between Specific Foods and Symptom Aggravation in Gastroesophageal Reflux Disease
It was adjusted for age and sex.
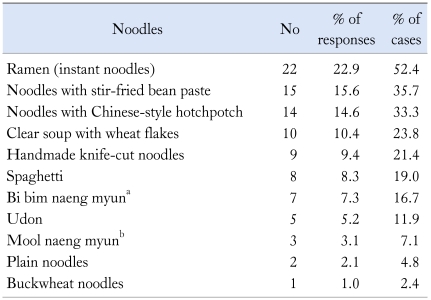
The subjects who answered that reflux related symptoms developed or were aggravated by noodles were asked what kinds of noodles contributed to the symptom. More than half of the responders answered that ramen (instant noodle) caused reflux-related symptoms (Table 7).
Table 7.
The List of Noodles Causing Symptoms: Patients With Symptom Aggravation by Noodles Reported Which Kind Did by Multiple Choice
aCold noodles served with hot and spicy sauce mix, bCold noodles served in cold beef soup.
The relationship between reflux-related symptoms and symptom severity scores aggravated by several foods in GERD is shown in Figure 3. The symptoms of acid regurgitation, dyspepsia, epigastric soreness and heartburn were more aggravated by these foods.
Figure 3.
Relationship between reflux-related symptoms and symptom severity scores aggravated by several foods in gastroesophageal reflux disease. The symptoms of acid regurgitation, dyspepsia, epigastric soreness and heartburn were more aggravated by these foods.
Discussion
The most common symptom in GERD patients is heartburn in Western countries.11 Several studies have reported the prevalence of heartburn as 21%-37% to experience heartburn at least once a month and as 13%-25% to experience at least once a week or more frequently.12-14 In this study, however, the most frequent and bothersome symptom of GERD patients was acid regurgitation. This may be attributed to cultural and linguistic differences in symptom perception and interpretation. The term "heartburn" is not universally understood and there is no direct translation of the word "heartburn" in Chinese, Swedish, Malay or Korean.3 A multiethnic study showed that the term "heartburn" was understood by only 35% of white American subjects and the figure dropped to 13% for Asian patients.15
The present study showed that subjects with overweight or obesity had an increased risk for GERD. These results are in agreement with those of previous studies which reported that body mass index may be associated with symptomatic gastroesophageal reflux, independent of diet and exercise.16,17
It is a common belief that some dietary habits would aggravate GERD-related symptoms, such as large-volume meal, rapid food intake, irregular food intake, eating between meals or late-evening meals. Physicians often advise patients with GERD to change their dietary habit and lifestyle. However, the evidence to support such recommendations of lifestyle modification has not been well substantiated. In several studies investigating the effect of dietary habits on gastroesophageal reflux, the results have not been consistent.18-22 In our study, the odds ratio for relative risk of irregular dietary intake was 2.33, while other habits (large-volume meal, rapid food intake, eating between meals and late-evening meals) did not show statistical significance. The reasons for these results might be considered in that the proportion of severe erosive esophagitis was too small in this study population. In Korea, however, the distribution of erosive esophagitis based on the LA classification is quite different from other countries. Severe esophagitis such as LA-C or LA-D accounts for only 3% in Korea,23 which is the reason why our study population was so deviated.
In this study, we showed that noodles induced severe symptom aggravation in GERD group. Noodles are one of the most favorite meals in Korea. To our knowledge, this is the first study to suggest that noodles may be refluxogenic to GERD patients. A possible explanation is the high carbohydrate content of noodles. A recent study showed that very low-carbohydrate diet in individuals with GERD significantly reduces distal esophageal acid exposure and improves symptoms.24 A second explanation for our findings is that noodles are generally made by wheat, which is more likely to precipitate the reflux related symptoms than rice.25 Other possible explanation is the high salt intake. It has been demonstrated that salt intake seems to be a risk factor for reflux symptoms.26 In our results, the most "refluxogenic" noodles, such as ramen and noodles with stir-fried bean paste, contain high salt content.
We also found that reflux-related symptoms were associated with spicy foods, fatty meals, sweets, alcohol, carbonated drinks and caffeinated drinks. These results are consistent with several physiological studies which have shown a decrease in lower esophageal pressure and an increase in esophageal acid exposure in response to ingestion of a variety of food items.27-29
There are several limitations that should be acknowledged. First, unmatched control group with ambiguous criteria may have resulted in a selection bias. The second limitation of this study was a relatively small number of subjects.
In summary, subjects with overweight or obesity had an increased risk for GERD. Irregular dietary intake was one of the risk factors for GERD. Acid regurgitation was the most suffering and most frequent reflux-related symptom in GERD. Noodles, spicy foods, fatty meals, sweets, alcohol, breads, carbonated drinks and caffeinated drinks were associated with symptom aggravation in GERD. Among the investigated noodles, ramen caused reflux-related symptoms most frequently.
In conclusion, this is the first study in Korea to suggest that noodles may be refluxogenic to GERD patients. Large prospective controlled trials are warranted to recommend more precise dietary and lifestyle modifications in the treatment of GERD.
Footnotes
Financial support: None.
Conflicts of interest: None.
References
- 1.Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900–1920. doi: 10.1111/j.1572-0241.2006.00630.x. [DOI] [PubMed] [Google Scholar]
- 2.Dent J, El-Serag HB, Wallander MA, Johansson S. Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2005;54:710–717. doi: 10.1136/gut.2004.051821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sharma P, Wani S, Romero Y, Johnson D, Hamilton F. Racial and geographic issues in gastroesophageal reflux disease. Am J Gastroenterol. 2008;103:2669–2680. doi: 10.1111/j.1572-0241.2008.02089.x. [DOI] [PubMed] [Google Scholar]
- 4.Kaltenbach T, Crockett S, Gerson LB. Are lifestyle measures effective in patients with gastroesophageal reflux disease? An evidence-based approach. Arch Intern Med. 2006;166:965–971. doi: 10.1001/archinte.166.9.965. [DOI] [PubMed] [Google Scholar]
- 5.Belhocine K, Galmiche JP. Epidemiology of the complications of gastroesophageal reflux disease. Dig Dis. 2009;27:7–13. doi: 10.1159/000210097. [DOI] [PubMed] [Google Scholar]
- 6.Nocon M, Labenz J, Willich SN. Lifestyle factors and symptoms of gastro-oesophageal reflux - a population-based study. Aliment Pharmacol Ther. 2006;23:169–174. doi: 10.1111/j.1365-2036.2006.02727.x. [DOI] [PubMed] [Google Scholar]
- 7.Festi D, Scaioli E, Baldi F, et al. Body weight, lifestyle, dietary habits and gastroesophageal reflux disease. World J Gastroenterol. 2009;15:1690–1701. doi: 10.3748/wjg.15.1690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Armstrong D, Bennett JR, Blum AL, et al. The endoscopic assessment of esophagitis: a progress report on observer agreement. Gastroenterology. 1996;111:85–92. doi: 10.1053/gast.1996.v111.pm8698230. [DOI] [PubMed] [Google Scholar]
- 9.The Third Korea National Health & Nutrition Examination Survey (KNHANES III), 2005 - Nutrition survey (1): Ministry of Health and Welfare, Korea Health Industry Development Institute. 2006. [Google Scholar]
- 10.Hwang JK, Kim J, Hong SG, et al. [A prospective multicenter study on the prevalence and symptoms of erosive reflux esophagitis in secondary and tertiary hospitals in Korea] . Korean J Gastroenterol. 2009;53:283–291. doi: 10.4166/kjg.2009.53.5.283. [Korean] [DOI] [PubMed] [Google Scholar]
- 11.Rothman M, Farup C, Stewart W, Helbers L, Zeldis J. Symptoms associated with gastroesophageal reflux disease: development of a questionnaire for use in clinical trials. Dig Dis Sci. 2001;46:1540–1549. doi: 10.1023/a:1010660425522. [DOI] [PubMed] [Google Scholar]
- 12.Talley NJ, Zinsmeister AR, Schleck CD, Melton LJ., 3rd Dyspepsia and dyspepsia subgroups: a population-based study. Gastroenterology. 1992;102:1259–1268. [PubMed] [Google Scholar]
- 13.El-Serag HB, Petersen NJ, Carter J, et al. Gastroesophageal reflux among different racial groups in the United States. Gastroenterology. 2004;126:1692–1699. doi: 10.1053/j.gastro.2004.03.077. [DOI] [PubMed] [Google Scholar]
- 14.Mohammed I, Nightingale P, Trudgill NJ. Risk factors for gastrooesophageal reflux disease symptoms: a community study. Aliment Pharmacol Ther. 2005;21:821–827. doi: 10.1111/j.1365-2036.2005.02426.x. [DOI] [PubMed] [Google Scholar]
- 15.Spechler SJ, Jain SK, Tendler DA, Parker RA. Racial differences in the frequency of symptoms and complications of gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2002;16:1795–1800. doi: 10.1046/j.1365-2036.2002.01351.x. [DOI] [PubMed] [Google Scholar]
- 16.El-Serag HB, Graham DY, Satia JA, Rabeneck L. Obesity is an independent risk factor for GERD symptoms and erosive esophagitis. Am J Gastroenterol. 2005;100:1243–1250. doi: 10.1111/j.1572-0241.2005.41703.x. [DOI] [PubMed] [Google Scholar]
- 17.Nandurkar S, Locke GR, 3rd, Fett S, Zinsmeister AR, Cameron AJ, Talley NJ. Relationship between body mass index, diet, exercise and gastro-oesophageal reflux symptoms in a community. Aliment Pharmacol Ther. 2004;20:497–505. doi: 10.1111/j.1365-2036.2004.02156.x. [DOI] [PubMed] [Google Scholar]
- 18.Iwakiri K, Kobayashi M, Kotoyori M, Yamada H, Sugiura T, Nakagawa Y. Relationship between postprandial esophageal acid exposure and meal volume and fat content. Dig Dis Sci. 1996;41:926–930. doi: 10.1007/BF02091532. [DOI] [PubMed] [Google Scholar]
- 19.Dore MP, Maragkoudakis E, Fraley K, et al. Diet, lifestyle and gender in gastro-esophageal reflux disease. Dig Dis Sci. 2008;53:2027–2032. doi: 10.1007/s10620-007-0108-7. [DOI] [PubMed] [Google Scholar]
- 20.Orr WC, Harnish MJ. Sleep-related gastro-oesophageal reflux: provocation with a late evening meal and treatment with acid suppression. Aliment Pharmacol Ther. 1998;12:1033–1038. doi: 10.1046/j.1365-2036.1998.00407.x. [DOI] [PubMed] [Google Scholar]
- 21.Fujiwara Y, Machida A, Watanabe Y, et al. Association between dinner-to-bed time and gastro-esophageal reflux disease. Am J Gastroenterol. 2005;100:2633–2636. doi: 10.1111/j.1572-0241.2005.00354.x. [DOI] [PubMed] [Google Scholar]
- 22.Wildi SM, Tutuian R, Castell DO. The influence of rapid food intake on postprandial reflux: studies in healthy volunteers. Am J Gastroenterol. 2004;99:1645–1651. doi: 10.1111/j.1572-0241.2004.30273.x. [DOI] [PubMed] [Google Scholar]
- 23.Kim N, Lee SW, Cho SI, et al. The prevalence of and risk factors for erosive oesophagitis and non-erosive reflux disease: a nationwide multicentre prospective study in Korea. Aliment Pharmacol Ther. 2008;27:173–185. doi: 10.1111/j.1365-2036.2007.03561.x. [DOI] [PubMed] [Google Scholar]
- 24.Austin GL, Thiny MT, Westman EC, Yancy WS, Jr, Shaheen NJ. A very low-carbohydrate diet improves gastroesophageal reflux and its symptoms. Dig Dis Sci. 2006;51:1307–1312. doi: 10.1007/s10620-005-9027-7. [DOI] [PubMed] [Google Scholar]
- 25.Sohn SM, Song CW, Koo JS, et al. [Gastroesophageal acid reflux according to different meals: flour cake vs rice cake] Korean J Gastrointest Motil. 2001;7:181–187. [Korean] [Google Scholar]
- 26.Nilsson M, Johnsen R, Ye W, Hveem K, Lagergren J. Lifestyle related risk factors in the aetiology of gastro-oesophageal reflux. Gut. 2004;53:1730–1735. doi: 10.1136/gut.2004.043265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Becker DJ, Sinclair J, Castell DO, Wu WC. A comparison of high and low fat meals on postprandial esophageal acid exposure. Am J Gastroenterol. 1989;84:782–786. [PubMed] [Google Scholar]
- 28.Hamoui N, Lord RV, Hagen JA, Theisen J, Demeester TR, Crookes PF. Response of the lower esophageal sphincter to gastric distention by carbonated beverages. J Gastrointest Surg. 2006;10:870–877. doi: 10.1016/j.gassur.2005.11.010. [DOI] [PubMed] [Google Scholar]
- 29.Murphy DW, Castell DO. Chocolate and heartburn: evidence of increased esophageal acid exposure after chocolate ingestion. Am J Gastroenterol. 1988;83:633–636. [PubMed] [Google Scholar]