Abstract
Pneumatic dilation (PD) is an effective treatment for achalasia cardia. Outcome of PD, however, varies among different studies. Recently, some groups started considering laparoscopic myotomy to be competitive to PD in treatment of achalasia considering dreaded complication like perforation following the latter therapeutic approach. Therefore, there is need to predict outcome of PD for achalasia, so that appropriate therapy, both for treatment naïve and for treatment failed patients can be chosen. Apart from age and gender, 2 investigations, namely post-PD manometry and timed barium esophagogram are most often used to predict outcome after PD. Even though there are studies available in the literature with regard to these modalities to predict outcome of PD, these are quite few in number, including small number of patients, primarily because of rarity of the disease. In this article, we review the literature predicting outcome of PD for achalasia.
Keywords: Achalasia, Dysphagia, Esophageal dysmotility, Manometry
Introduction
Achalasia cardia is a rare primary esophageal motor disorder, which is diagnosed on the basis of esophageal manometry.1 Typical manometry findings in achalasia are aperistalsis of esophageal body and incomplete relaxation of lower esophageal sphincter (LES).2 Based on average esophageal body amplitude, achalasia is classified into classic (≤ 40 mmHg) and vigorous types (> 40 mmHg).3 Vigorous achalasia is considered as the early stage in the natural history of the disease.4,5 Treatment of achalasia is usually palliative in nature.6 There are 3 main modes of therapy: pneumatic dilation (PD), botulinum toxin injection (both through endoscopic means) and surgery (Heller's cardiomyotomy). Endoscopic PD and surgery are effective in providing long-term remission.7
Pneumatic Dilation
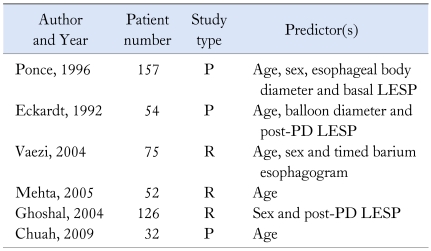
PD is the most popular non-surgical treatment of achalasia. Moreover, it is cost-effective compared to botulinum toxin injection and surgery.8-10 PD can be performed with different dilators of variable balloon compliances. Low compliance polyethylene pneumatic dilator (Rigiflex dilator) is most widely used because of its theoretical advantages over the high compliance balloon dilator.11 Most feared complication of PD is esophageal perforation. Perforation rate varies from less than 1% to 3% in various studies.12-16 Furthermore, PD is effective in 64%-87% patients.12 Also, a proportion of initial responders experience recurrence during long-term follow-up. Therefore, it is important to predict which patient is less likely to respond or develop recurrence following an initial response for the following reasons; (1) to devise treatment strategy in a given patient, (2) to prognosticate, (3) to plan early re-intervention, if required, and (4) to help understand pathophysiology of the disease. Table 1 shows the likely predictors of outcome following PD for achalasia cardia.
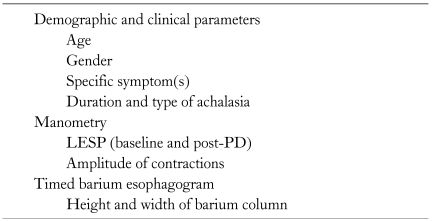
Table 1.
Possible Predictors of Outcome Following Pneumatic Dilation of Achalasia Cardia
LESP, lower esophageal sphincter pressure; PD, pneumatic diation.
The studies published in literature addressing the issue on predictors of outcome of PD (Tables 1-3) differ in type of dilator used, symptom scores used to assess the outcomes (response and recurrence), treatment protocol for management of recurrence and investigations used to predict outcomes etc. In spite of such heterogeneity between the studies, these do provide valuable information, which can guide physician in planning treatment strategy.
Table 3.
Summary of Studies Predicting Outcome of Pneumatic Dilation of Achalasia Cardia
PD, pneumatic dilation; LESP, lower esophageal sphincter pressure; TBE, timed barium esophagogram.
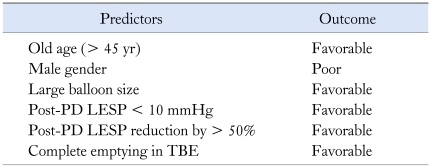
The first large prospective study was done by Ponce et al17 in which 157 patients with achalasia underwent PD with Witzel dilator. Patients who had post-PD lower esophageal sphincter pressure (LESP) < 10 mmHg had a better outcome than others. Using Bayes' theorem, a predictive model was constructed including 5 most discriminating values: age < 20 years, male sex, diameter of esophageal body < 3 cm, basal pressure of esophageal body > 15 mmHg and LESP > 30 mmHg. Jackknife method was used to validate the model. The limitation of this study was lack of use of conventional statistics including multivariate analysis. Furthermore, Witzel dilator has high compliance balloon that is no longer in use.
Mehta et al18 reported a retrospective study on 52 patients using Rigiflex balloon in whom 81% responded to PD. On univariate analysis, non-responders were younger in age (< 40 years), had high baseline LESP (> 50 mmHg) and reduced mid-esophageal contractions (amplitude < 30 mmHg). There was no significant difference in response rates with respect to gender. On multivariate analysis, only young age was associated with poor response, though patients with high baseline LES pressure showed a trend towards poor response. Esophageal manometry was not repeated after PD in this study.
From our center, we reported a retrospective study on 126 patients who had undergone PD for achalasia.12 On univariate analysis, regurgitation, chest pain, pulmonary symptoms and male gender were associated with non-response. Post-PD reduction in LESP by more than 50% was associated with good response. On multivariate analysis, male gender was the only factor, which was associated with worse outcome. This is the largest study in which a low compliance dilator (Rigiflex) was used. But, post-PD manometry was not done in all the patients in this study.
Eckardt et al19,20 reported outcome of management of 54 patients with achalasia cardia with PD. Symptom score and LESP were assessed at baseline and at 4 weeks after PD. Follow-up assessment of symptom score was done at 2 yearly intervals for a median of 13.8 years. Of 35 patients who had relapse, 32 relapsed within 5 years. Long-term outcome was significantly better in patients with age older than 40 years and post-PD LESP < 10 mmHg. Even though this study was prospective with long-term follow-up, the authors have used Brownie Mchardy dilator (high compliance balloon) which is not being used now-a-days.
Farhoomand et al21 reported a retrospective analysis of 75 patients who underwent PD with Rigiflex dilator. Symptom scoring and timed barium esophagogram were done in all the patients at baseline and at 1 month after PD. Among the patients who had undergone PD with 30 mm balloon, retreatment was required less often compared to the patients who had undergone PD with 35 and 40 mm balloon. Especially, early failure rate (within 3 months) was high among those who had undergone PD with 30 mm balloon compared to those in whom larger balloon diameter was used. Also, 22 of 25 patients who had early failure were men. Multivariate Cox proportional hazards model revealed that younger men (< 45 years) required additional therapy more frequently compared to older men and also the difference in response rate between male and female became narrower as age advanced. Thus they concluded that failure was commoner among young men who had undergone PD with 30 mm balloon. Similar to their previous study in which complete barium emptying in timed barium esophagogram was found to strongly correlate with symptomatic improvement, including long-term remission, this study also showed that those who did not require re-treatment more often had complete barium emptying after PD.22 Post-PD manometry was not done in this study. The authors suggested that male patients with achalasia should be treated with 35 mm balloon for even the first session of PD as 30 mm balloon often failed in them and post-PD timed barium esophagogram predicted long-term outcome after PD. A prospective study by Chuah et al23 on 32 patients managed with Rigiflex dilator also concluded that age more than 45 years was the only significant factor predicting favorable outcome.
Even though, some studies evaluated duration of dysphagia and type of achalasia as possible parameters predicting outcome, they were not found important in predicting outcome even in univariate analysis.12,17-19 Post-PD manometry and timed barium esophagogram are the 2 most widely used investigations to predict the outcome after PD. Manometry studies have used various criteria to predict the outcome such as post-PD LESP < 10 mmHg and reduction of LESP by more than 50% of baseline LESP.
Andersson et al24 reported a prospective study, in which 51 patients with achalasia were randomized into 2 treatment groups, namely PD and laparoscopic myotomy. Timed barium esophagogram was done at baseline and after treatment. The median follow-up time after the post-treatment timed barium esophagogram was 18 months. They found a significant correlation between barium emptying at 1 minute and symptom scores at the end of follow-up period in both the groups. Patients with less than 50% improvement in this parameter after treatment had a 40% risk of treatment failure on follow-up.
The recently introduced high resolution manometry displays spatiotemporal plots of esophageal body and LESPs.25,26 It also helps us to understand the segmental functional anatomy of esophageal body and LES, which contributes to our understanding of various subsets of achalasia and possibly their difference in response to various modes of treatment. Till now, this attractive research tool has not been studied for predicting the outcome of PD in achalasia.
Why Is Pneumatic Dilation Less Effective in Men?
Explanation for worse outcome of PD among men is unknown. However, one may hypothesize that LES muscles might be stronger among men than women that might be responsible for worse outcome among them. LES tone might be more in younger men than in older men, thus further explaining less favorable outcome in young men. However, this needs to be studied further.
Why Is Old Age a Favorable Predictor?
Apart from some of the above discussed studies, there are many other studies in literature which concluded old age as a predictor of favorable outcome.27-30 Though, the exact reason for this is not known, there are various hypotheses to explain this finding.
Anatomically, LES has 2 components, namely clasp fibers encircling the gastroesophageal junction medially and gastric sling fibers present on left lateral side. In PD, only the clasp fibers are targeted. Hence, it is possible that gastric sling fibers, unaffected by PD, contribute to residual LES tone in these patients after PD. As discussed previously, this tone is likely to be higher in younger patients, thus explaining poor response in young patients.31 Patients with long-standing symptoms often interpret mild improvement in esophageal emptying as dramatic relief from dysphagia.32 Older patients perceive less pain compared to their younger counterparts when balloon is distended in esophagus.33 Also, older patients are expected to have weaker LES muscles that might be easily torn during PD.
Clinical Implications
Young men having persistently high LESP and poor esophageal emptying after PD might be better treated by laparoscopic myotomy rather than persisting with repeated PDs. Similarly, old women after PD having low (or > 50% reduced) LESP and good esophageal emptying may be offered repeated PD in the unlikely event of recurrence. Thirty-five mm instead of 30 mm balloon should be tried for first PD, particularly in males.
Need for Future Research
A prospective study with large number of patients and long-term follow-up is needed. Both timed barium esophagogram and manometry, especially high resolution manometry should be done at baseline and post-PD, so that they can be compared in their value in predicting outcome. Strong statistical methods will add to the strength of evidence.
Conclusion
PD is an effective alternative to surgery. The response to PD depends on age and gender of the patient and size of the balloon used for PD. The long-term response can be predicted with the help of post-PD manometry and timed barium esophagogram. Balloon size has to be chosen according to the gender. Further prospective studies with larger numbers are needed.
Table 2.
Summary of Factors Useful to Predict Outcome of Pneumatic Dilation of Achalasia Cardia as Found in Different Studies
P, prospective study; R, retrospective study; LESP, lower esophageal sphincter pressure; PD, pneumatic dilation.
Footnotes
Financial support: None.
Conflicts of interest: None.
References
- 1.Farrokhi F, Vaezi MF. Idiopathic (primary) achalasia. Orphanet J Rare Dis. 2007;2:38–46. doi: 10.1186/1750-1172-2-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eckardt AJ, Eckardt VF. Current clinical approach to achalasia. World J Gastroenterol. 2009;15:3969–3975. doi: 10.3748/wjg.15.3969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goldenberg SP, Burrell M, Fette GG, Vos C, Traube M. Classic and vigorous achalasia: a comparison of manometric, radiographic, and clinical fingings. Gastroenterology. 1991;101:743–748. doi: 10.1016/0016-5085(91)90534-r. [DOI] [PubMed] [Google Scholar]
- 4.Misra A, Chourasia D, Ghoshal UC. Manometric and symptomatic spectrum of motor dysphagia in a tertiary referral center in northern India. Indian J Gastroenterol. 2010;29:12–16. doi: 10.1007/s12664-010-0002-7. [DOI] [PubMed] [Google Scholar]
- 5.Park W, Vaezi MF. Etiology and pathogenesis of achalasia: the current understanding. Am J Gastroenterol. 2005;100:1404–1414. doi: 10.1111/j.1572-0241.2005.41775.x. [DOI] [PubMed] [Google Scholar]
- 6.Chuah SK, Wu KL, Hu TH, Tai WC, Changchien CS. Endoscope guided pneumatic dilation for treatment of esophageal achalasia. World J Gastroenterol. 2010;16:411–417. doi: 10.3748/wjg.v16.i4.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lopushinsky SR, Urbach DR. Pneumatic dilatation and surgical myotomy for achalasia. JAMA. 2006;296:2227–2233. doi: 10.1001/jama.296.18.2227. [DOI] [PubMed] [Google Scholar]
- 8.Ghoshal UC, Aggarwal R, Kumar S, Naik SR. Pneumatic dilation versus intrasphincteric botulinum toxin injection in the treatment of achalasia cardia in India: an economic analysis. Indian J Gastroenterol. 2002;21:193–196. [PubMed] [Google Scholar]
- 9.Parkman HP, Reynolds JC, Ouyang A, Rosato EF, Eisenberg JM, Cohen S. Pneumatic dilatation or oesophagomyotomy treatment for idiopathic achalasia: clinical outcomes and cost analysis. Dig Dis Sci. 1993;38:75–85. doi: 10.1007/BF01296777. [DOI] [PubMed] [Google Scholar]
- 10.Richter JE. Comparison and cost analysis of different treatment strategies in achalasia. Gastrointest Endosc Clin N Am. 2001;11:359–370. [PubMed] [Google Scholar]
- 11.Stark GA, Castell DO, Richter JE, Wu WC. Prospective randomized comparison of Brown-McHardy and microvasive balloon dilators in treatment of achalasia. Am J Gastroenterol. 1990;85:1322–1326. [PubMed] [Google Scholar]
- 12.Ghoshal UC, Kumar S, Saraswat VA, Aggarwal R, Misra A, Choudhuri G. Long-term follow-up after pneumatic dilation for achalasia cardia: factors associated with treatment failure and recurrence. Am J Gastroenterol. 2004;99:2304–2310. doi: 10.1111/j.1572-0241.2004.40099.x. [DOI] [PubMed] [Google Scholar]
- 13.Khan AA, Shah WH, Alam A, Butt AK, Shafqat F. Sixteen years of follow up of achalasia: a prospective study of graded dilatation using Rigiflex balloon. Dis Esophagus. 2005;18:41–45. doi: 10.1111/j.1442-2050.2005.00448.x. [DOI] [PubMed] [Google Scholar]
- 14.Vela MF, Richter JE, Wachsberger D, Connor J, Rice TW. Complexities of managing achalasia at a tertiary referral centre: use of pneumatic dilatation, Heller myotomy, and botulinum toxin injection. Am J Gastroenterol. 2004;99:1029–1036. doi: 10.1111/j.1572-0241.2004.30199.x. [DOI] [PubMed] [Google Scholar]
- 15.Metman EH, Lagasse JP, d'Alteroche L, Picon L, Scotto B, Barbieux JP. Risk factors for immediate complications after progressive pneumatic dilation for achalasia. Am J Gastroenterol. 1999;94:1179–1185. doi: 10.1111/j.1572-0241.1999.01062.x. [DOI] [PubMed] [Google Scholar]
- 16.Bittinger M, Wienbeck M. Pneumatic dilation in achalasia. Can J Gastroenterol. 2001;15:195–199. doi: 10.1155/2001/593657. [DOI] [PubMed] [Google Scholar]
- 17.Ponce J, Garrigues V, Pertejo V, Sala T, Berenguer J. Individual prediction of response to pneumatic dilation in patients with achalasia. Dig Dis Sci. 1996;41:2135–2141. doi: 10.1007/BF02071392. [DOI] [PubMed] [Google Scholar]
- 18.Mehta R, John A, Sadasivan S, et al. Factors determining successful outcome following pneumatic balloon dilation in achalasia cardia. Indian J Gastroenterol. 2005;24:243–245. [PubMed] [Google Scholar]
- 19.Eckardt VF, Aignherr C, Bernhard G. Predictors of outcome in patients with achalasia treated by pneumatic dilation. Gastroenterology. 1992;103:1732–1738. doi: 10.1016/0016-5085(92)91428-7. [DOI] [PubMed] [Google Scholar]
- 20.Eckardt VF, Gockel I, Bernhard G. Pneumatic dilation for achalasia: late results of a prospective follow up investigation. Gut. 2004;53:629–633. doi: 10.1136/gut.2003.029298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Farhoomand K, Connor JT, Richter JE, Achkar E, Vaezi MF. Predictors of outcome of pneumatic dilation in achalasia. Clin Gastroenterol Hepatol. 2004;2:389–394. doi: 10.1016/s1542-3565(04)00123-5. [DOI] [PubMed] [Google Scholar]
- 22.Vaezi MF, Baker ME, Achkar E, Richter JE. Timed barium oesophagram: better predictor of long term success after pneumatic dilation in achalasia than symptom assessment. Gut. 2002;50:765–770. doi: 10.1136/gut.50.6.765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chuah SK, Hu TH, Wu KL, et al. Clinical remission in endoscope-guided pneumatic dilation for the treatment of esophageal achalasia: 7-year follow-up results of a prospective investigation. J Gastrointest Surg. 2009;13:862–867. doi: 10.1007/s11605-009-0804-z. [DOI] [PubMed] [Google Scholar]
- 24.Andersson M, Lundell L, Kostic S, et al. Evaluation of the response to treatment in patients with idiopathic achalasia by the timed barium esophagogram: results from a randomized clinical trial. Dis Esophagus. 2009;22:264–273. doi: 10.1111/j.1442-2050.2008.00914.x. [DOI] [PubMed] [Google Scholar]
- 25.Fox MR, Bredenoord AJ. Oesophageal high-resolution manometry: moving from research into clinical practice. Gut. 2008;57:405–423. doi: 10.1136/gut.2007.127993. [DOI] [PubMed] [Google Scholar]
- 26.Pandolfino JE, Kwiatek MA, Nealis T, Bulsiewicz W, Post J, Kahrilas PJ. Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology. 2008;135:1526–1533. doi: 10.1053/j.gastro.2008.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fellows IW, Ogilvie AL, Atkinson M. Pneumatic dilation in achalasia. Gut. 1983;24:1020–1023. doi: 10.1136/gut.24.11.1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vantrappen G, Hellemans J, Deloof W, Valembois P, Vandenbrouke J. Treatment of achalasia with pneumatic dilations. Gut. 1971;12:268–275. doi: 10.1136/gut.12.4.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dağli U, Kuran S, Savaş N, et al. Factors predicting outcome of balloon dilatation in achalasia. Dig Dis Sci. 2009;54:1237–1242. doi: 10.1007/s10620-008-0493-6. [DOI] [PubMed] [Google Scholar]
- 30.Tanaka Y, Iwakiri K, Kawami N, et al. Predictors of a better outcome of pneumatic dilatation in patients with primary achalasia. J Gastroenterol. 2010;45:153–158. doi: 10.1007/s00535-009-0145-4. [DOI] [PubMed] [Google Scholar]
- 31.Pehlivanov N, Pasricha PJ. Medical and endoscopic management of achalasia. GI Motility online. 2006 www.nature.com/gimo/contents/pt1/full/gimo52.html. [Google Scholar]
- 32.Gelfand MD, Kozarek RA. An experience with polyethylene balloons for pneumatic dilation in achalasia. Am J Gastroenterol. 1989;84:924–927. [PubMed] [Google Scholar]
- 33.Lasch H, Castell DO, Castell JA. Evidence for diminished visceral pain with aging: studies using graded intraesophageal balloon distension. Am J Physiol. 1997;272:G1–G3. doi: 10.1152/ajpgi.1997.272.1.G1. [DOI] [PubMed] [Google Scholar]