Abstract
A once-daily antibiotic regimen for group A β-hemolytic streptococcal pharyngitis (GABHS) could improve compliance and be effective in the prevention of rheumatic fever, a dangerous complication of untreated or poorly treated GABHS. Amoxicillin is ideal for once-daily dosing due to its low cost. Azithromycin, cefadroxil, ceftibuten, cefixime and extended release amoxicillin are also FDA approved to treat GABHS once daily; however, even when taken for short courses, these antibiotics are more expensive compared with a oncedaily dosing of conventional amoxicillin for 10 days. The American Heart Association recently recommended once-daily amoxicillin dosing when treating GABHS, and amoxicillin has been proven to be effective when dosed once daily, with no obvious disadvantage compared with twice-daily dosing or with conventional penicillin treatment 3 to 4 times daily.
Keywords: amoxicillin, once daily, pharyngitis, streptococcal infections
INTRODUCTION
Rheumatic fever is a preventable inflammatory disease that can develop as a result of untreated or poorly treated group A β-hemolytic streptococcal pharyngitis (GABHS).1 Rheumatic fever can lead to rheumatic heart disease, a condition in which heart valves are permanently damaged.1 Symptoms of rheumatic fever include abdominal pain, fever, shortness of breath, chest pain, joint pain and swelling, and skin rash. It is estimated that more than 336,000 children have rheumatic fever annually, with 10 cases per 100,000 people in developed countries.2 Approximately 60% of patients who have rheumatic fever will have rheumatic heart disease,2 making it the leading cause of cardiovascular death in the first 50 years of life in developing countries.1
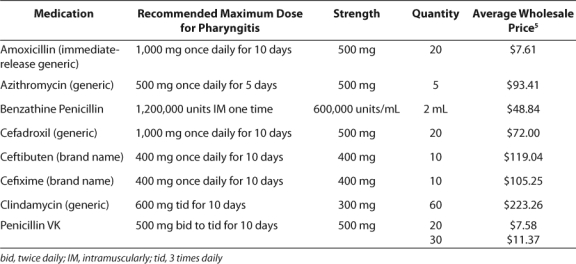
Penicillin given 2 to 4 times daily is considered to be the standard of care when treating streptococcal pharyngitis.3 Amoxicillin is a congener of penicillin with similar antimicrobial activity but a slightly longer half life of 1 to 2 hours compared with 30 minutes for penicillin.4 There are currently 6 Food Drug Administration labeled treatments for GABHS pharyngitis: penicillin, cefadroxil, cefixime, ceftibuten, azithromycin, and extended release amoxicillin (Moxatag). However, these agents are all relatively expensive compared with conventional amoxicillin, as seen in Table 1. A once-daily dosing regimen of generic amoxicillin could improve compliance and be an affordable alternative for treating GABHS. The purpose of this manuscript is to examine claims that once daily amoxicillin is noninferior to other commonly used antibiotic therapies in the treatment of GABHS.
Table 1.
Relative Costs of Treatments for GABHS Pharyngitis
SUPPORTING STUDIES
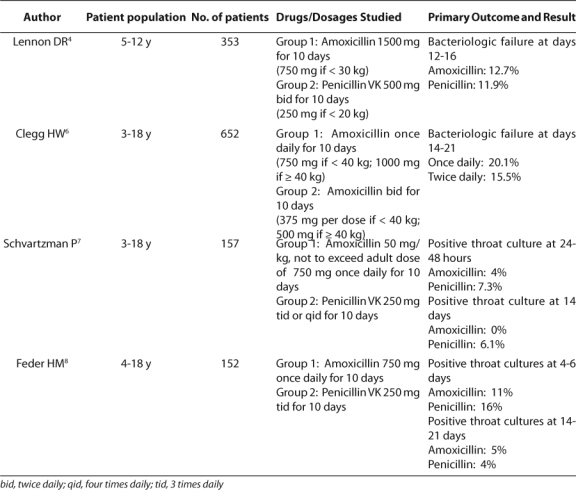
We identified 4 studies in which researchers have examined the efficacy of once-daily amoxi cillin in the treatment of GABHS. Information from these studies is summarized in Table 2. The first of these studies was performed by Lennon and colleagues.4 This study compared once-daily amoxicillin with twice-daily penicillin V potassium (K) in pediatric patients. Children aged 5 to 12 years who had positive results for GABHS were randomized to receive either amoxicillin 1500 mg (750 mg for children ≤ 30 kg) administered orally once daily for 10 days or to receive penicillin VK 500 mg (250 mg for children ≤ 20 kg) twice daily for 10 days. So that compliance could be monitored, children were given supervised doses at school. During the weekend, the children were asked to complete drug diary cards and to return the bottle on Monday. The eradication of GABHS and the clinical course were assessed by using follow-up throat cultures and symptom evaluation within days 3 to 6 (visit 2), days 12 to 16 (visit 3), and days 26 to 36 (visit 4). The primary outcome of bacteriological failure for patients in both medication groups was similar at all 3 visits, with the failure rate for penicillin being 6.2%, 11.9%, and 11.3% and for amoxicillin 5.8%, 12.7%, and 10.7%. No difference in symptom resolution was detected between groups. Adverse events were not monitored or reported in this study. Using the school personnel to administer doses resulted in 97% of amoxicillin and 98% of penicillin VK patients receiving ≥ 80% of their doses. The authors concluded that once-daily amoxicillin for 10 days is noninferior to 10 days of twice-daily penicillin VK in the treatment and elimination of GABHS pharyngitis in children.
Table 2.
Studies Evaluating Once-Daily Amoxicillin for GABHS
In their adequately powered study, Lennon and colleagues enrolled patients for 80% power to demonstrate noninferiority, but the study was not designed to determine whether one treatment is superior to another. Using school personnel to deliver doses likely enhanced compliance, allowing for comparisons of medication efficacy but limiting the generalizability of the study to the home environment.
Clegg and colleagues evaluated once-daily amoxicillin therapy in patients aged 3 to 18 years who had GABHS.6 These patients were stratified by weight and randomly assigned to receive amoxicillin for 10 days either once daily (750 mg for patients < 40 kg or 1000 mg for patients ≥ 40 kg) or twice daily (375 mg for patients < 40 kg or 500 mg for patients ≥ 40 kg). To assess compliance, drug diaries were used, along with routine inspection of the medication bottles. Bacteriologic failure was determined by throat swabs taken between days 14 to 21 (visit 2) and days 28 to 35 (visit 3). At visit 2, the failure rate for the once-daily group was 20.1%, and the failure rate for the twice-daily group was 15.5%. These percentages were within the prespecified acceptable variation between the groups of less than 10%. At visit 3, the failure rate was 2.8% for the once-daily group and 7.1% for the twice-daily group; however, at the discretion of the study physician, patients with failure at visit 2 were started on a different medication. The frequency of adverse events did not differ between groups. Gastrointestinal symptoms and rash were the most common adverse effects. Rash occurred in 10% of patients in both treatment groups and was present more often in those less than 40 kg. Only 1% of the patients had a rash that was considered allergic in nature. The treatment groups had similar adherence rates with 4% of patients in the once-daily and 5% of patients in the twice-daily groups receiving fewer than 10 days of therapy. The authors concluded that oncedaily amoxicillin is noninferior to twice-daily amoxicillin dosing.
Clegg et al. enrolled sufficient patients for 90% power to demonstrate noninferiority of oncedaily amoxicillin to twice-daily amoxicillin. The failure rates in the study were higher than those reported in other studies with no reason for high failure rates identified. No data exist to determine whether the doses chosen by the authors or the use of a 40-kg weight cut-off to determine the dose results in optimal outcomes.
In another analysis, Shvartzman and colleagues studied once-daily amoxicillin treatment in pediatric patients 3 years and older.7 A group of 82 patients received 250 mg of penicillin VK 3 or 4 times daily for 10 days, and a group of 75 patients received once-daily amoxicillin (50 mg/kg, not to exceed 750 mg) for 10 days. Neither adverse effects nor compliance were reported in this study. The researchers found that patients receiving once-daily amoxicillin had significantly fewer bacteriologic treatment failures (0%) 14 days after completing the therapy compared with patients who received penicillin VK (6.1%). The finding was considered statistically significant. No difference existed between groups in symptom resolution. The course of treatment for the 3 amoxicillin-treated patients who had positive throat cultures at 24 to 48 hours was changed to penicillin VK for 10 days, making it difficult to determine whether the 14-day results were influenced by the antibiotic change.
In still another study, Feder and colleagues enrolled pediatric patients aged 4 to 18 years who presented with symptoms of GABHS.8 Patients were randomly assigned to a 10-day course of either 750 mg of amoxicillin once daily or 250 mg of penicillin VK 3 times daily. Patients were then asked to return for follow-up at 18 to 24 hours, 4 to 6 days, and 14 to 21 days. Treatment failure was defined as the presence of the same serotype of GABHS on a follow-up culture as on the initial culture. Compliance was assessed by having the parent dip a strip of filter paper in the patient's urine on the 7th day of therapy. The strip was mailed to the University of Connecticut Health Center, where it was assayed for antimicrobial therapy. The researchers concluded that no statistically significant differences existed in the treatments at any of the 3 follow-up swabs, with the failure rates being 11% for amoxicillin vs 16% for penicillin at 4 to 6 days and 5% vs 4% at days 14 to 21. Among the 79 patients treated with amoxicillin, 2 patients had rashes, 3 had diarrhea, and 3 complained of abdominal pain. Of the 73 who completed the penicillin therapy, 1 patient had urticaria, 2 had diarrhea, and 1 complained of abdominal pain. These symptoms resolved within 24 hours of discontinuing the antibiotic. Thus, the study concluded that amoxicillin given once daily is as effective as penicillin VK given 3 times daily. This study reported no statistical analysis in the methods or results.
DISCUSSION
The studies discussed demonstrate the efficacy and safety of once-daily amoxicillin eradicating GABHS from the oropharynx. In none of the studies were patients evaluated for emergence of rheumatic fever as a complication of GABHSpositive pharyngitis. However, when the organism is eradicated, the risk for rheumatic fever is eliminated. Each of these studies suggests that a once-daily treatment strategy will be effective and that gastrointestinal and other events did not occur at more frequent rates with the once-daily dosing regimen. The doses used in the studies were variable, and no studies have compared the different dosages, making it difficult to determine the best dosing strategy to use. In addition, we found no studies that determined whether there is an advantage of the delayed-release amoxicillin product over immediate-release products.
In February 2009, updated guidelines were released by the American Heart Association regarding the prevention of rheumatic fever and the diagnosis and treatment of acute streptococcal pharyngitis. These guidelines outlined the accepted therapies for the treatment of GABHS pharyngitis. According to the guidelines, amoxicillin 50 mg/kg once daily (not to exceed 1000 mg) and penicillin 40 mg/kg (not to exceed 750 mg) divided 3 times a day are the oral antibiotics of choice.1
CONCLUSIONS
Once-daily administration of amoxicillin in patients aged 3 years and older has been proven to be noninferior to multiple daily dosing for group A β-hemolytic streptococcal pharyngitis. The recommendation made by the American Heart Association in February 2009 is 50 mg/kg/day up to 1000 mg for 10 days.1 This once-daily regimen not only can help improve adherence, but it is a cheaper once-daily alternative for the patient.
ABBREVIATIONS
- GABHS
group A β-hemolytic streptococcal pharyngitis
- K
potassium
Footnotes
DISCLOSURE The authors declare no conflicts or financial interests in any product or service mentioned in the manuscript, including grants, equipment, medications, employment, gifts, and honoraria.
REFERENCES
- 1.Gerber MA, Baltimore RS, Eaton CB, et al. Prevention of Rheumatic Fever and Diagnosis and Treatment of Acute Streptococcal Pharyngitis: A Scientific Statement From the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee of the Council on Cardiovascular Disease in the Young, the Interdisciplinary Council on Functional Genomics and Translational Biology, and the Interdisciplinary Council on Quality of Care and Outcomes Research: Endorsed by the American Academy of Pediatrics. Circulation. 2009;119:1541–1551. doi: 10.1161/CIRCULATIONAHA.109.191959. [DOI] [PubMed] [Google Scholar]
- 2.Carapetis JR, Steer AC, Mulholland EK, Weber M. The global burden of group A streptococcal diseases. Lancet Infect Dis. 2005;5:685–694. doi: 10.1016/S1473-3099(05)70267-X. [DOI] [PubMed] [Google Scholar]
- 3.Kahliq Y, Forgie S, Zhanel G. Upper respiratory tract infections. In: DiPiro JT, Talbert RL, Yee GC, et al., editors. Pharmacotherapy: a pathophysiologic approach. New York: Elsevier; 2008. pp. 1779–1790. [Google Scholar]
- 4.Lennon DR, Farrell E, Martin DR, Stewart JM. Once-daily amoxicillin versus twicedaily penicillin V in group A beta-hemolytic streptococcal pharyngitis. Arch Dis Child. 2008;93:474–478. doi: 10.1136/adc.2006.113506. [DOI] [PubMed] [Google Scholar]
- 5.Red Book: Pharmacy's Fundamental Resource. Thomson Healthcare; Montvale, NJ: 2008. [Google Scholar]
- 6.Clegg HW, Ryan AG, Dallas SD, et al. Treatment of streptococcal pharyngitis with once-daily compared with twice-daily amoxicillin: a noninferiority trial. Pediatr Infect Dis J. 2006;25:761–767. doi: 10.1097/01.inf.0000235678.46805.92. [DOI] [PubMed] [Google Scholar]
- 7.Shvartzman P, Tabenkin H, Rosentwaig A, et al. Treatment of streptococcal pharyngitis with amoxicillin once a day. Br Med J. 1993;306:1170–1172. doi: 10.1136/bmj.306.6886.1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feder HM, Jr., Gerber MA, Randolph MF, et al. Once-daily therapy for streptococcal pharyngitis with amoxicillin. Pediatrics. 1999;103:47–51. doi: 10.1542/peds.103.1.47. [DOI] [PubMed] [Google Scholar]
- 9.American Heart Association. Rheumatic Heart Disease/Rheumatic Fever. http://circ.ahajournals.org/cgi/reprint/CIRCULATIONAHA.109.191959 www.americanheart.org (accessed August 15, 2010)


