Abstract
Aims: To compare the mortality of female alcoholics randomly assigned to the woman-only programme ‘Early treatment for Women with Alcohol Addiction’ (EWA) versus those who received mixed gender ‘Treatment As Usual’ (TAU). Methods: Randomized controlled trial involving 2-year follow-up by personal interview and mortality register data through 27 years of 200 women first time treated for alcohol use disorder (AUD; EWA, n = 100 and TAU, n = 100), who were consecutively recruited during 1983–1984. Data from the Causes of Death Register were used to test for mortality differences related to group interaction predictors such as age, inpatient versus outpatient status at intake and 2-year drinking outcome. Results: Significantly lower mortality was found among younger women who participated in EWA compared with those who received TAU. This difference lasted nearly 20 years after intake to treatment. For women who only needed outpatient treatment, reduced mortality was found in the EWA group, even for older women. Increased mortality was found for TAU women who did not attend the 2-year follow-up compared with those who attended; no such difference was found for EWA women. This indicates different attrition mechanisms in the two groups. Thus, previously reported treatment effects may have been underestimated. EWA was a more comprehensive programme than TAU while also being single gender. Conclusions: EWA, specifically developed to meet a broad spectrum of problems among women with AUDs, was more effective than TAU, a mixed gender programme. It was not possible to separate whether this was in part because it was a more comprehensive programme, as well as being single gender.
INTRODUCTION
Female alcoholics show a higher mortality risk than male alcoholics and women from the general population (Dahlgren and Myrhed, 1977). The mortality rates reported vary between 3 and 5.6 for treatment samples (Berglund, 1984; Cipriani et al., 2001; Gerdner and Berglund, 1997; Lindberg and Ågren, 1988), while it is only 1.4 for women and men who initiated help seeking for alcohol use disorders (AUDs; Timko et al., 2006). In a previous study, a mortality rate of 2.4 was found for 420 women referred to the programme ‘Early treatment for Women with Alcohol Addiction’ (EWA) compared with matched women from the general population (Haver et al., 2009). In this paper, we present long-term mortality for a subgroup of these women (n = 200) who participated in a randomized controlled trial (RCT) that compared the EWA programme with treatment as usual (TAU).
Treatment variables relevant for mortality are treatment duration, the need of inpatient versus outpatient treatment and duration of outpatient follow-up (James, 2005; Masudomi et al., 2004; Timko et al., 2006). After controlling for background factors, mortality risk is related to compliance with treatment and intervention outcome as measured by abstinence, alcohol consumption, social drinking, relapse and prolonged alcohol misuse after treatment (Barr et al., 1984; Feuerlein et al., 1994; Gerdner and Berglund, 1997; Smith et al., 1983, 1994; Taylor, 1994; Timko et al., 2006). Continuous abstinence may be especially important for survival (Gerdner and Berglund, 1997; Yoshino et al., 1997). However, alcohol-dependent and socially unstable women who had an improved drinking pattern, even while not becoming abstinent, survived longer than the non-improved women (Gerdner and Berglund, 1997).
There are several reasons to expect differences in long-term mortality between the EWA and TAU groups. First, the EWA intervention group did significantly better than the TAU group on treatment compliance and treatment duration, needed less inpatient care because they did not experience relapse drinking following initial treatment, experienced more improved social conditions and work status, and had a lower load of psychiatric symptoms at the 2-year follow-up (Dahlgren and Willander, 1989a). Furthermore, EWA women had a significantly better drinking outcome as assessed by self-reported alcohol consumption measures (e.g. total alcohol consumption, abstinence or meeting the criteria for social drinking versus drinking relapse). Most importantly, this initial study reported a trend towards higher mortality among the TAU women following intake, while the EWA group had a mortality rate as expected among women of the general population (Dahlgren and Willander, 1989b). This important observation needed to be studied for extended time periods since a potentially lower mortality rate over time would be a strong indicator of the effectiveness of the EWA treatment programme.
The preventive effect of an intervention will most likely be stronger directly after the intervention than it will be in the long term (Cuijpers et al., 2004). Consequently, the practice of using the ratio between number of deaths and number of years when comparing results across different study intervals is a problematic procedure (Timko et al., 2006). It is unlikely that the same group differences will be consistent over such a long period of time as 27 years. We expected women in the EWA group to show increased survival relative to women in the TAU group, with the most marked differences early in the follow-up period. Testing such a research problem can be done by testing whether the group difference interacts with time or by dividing the follow-up interval into separate time intervals.
Age should also be taken into account when studying group differences in mortality, especially when there is a wide age range. Increasing age is associated with increased risk of death, and therefore stronger mortality differences are likely between younger and older women over a long follow-up period. This makes the interaction between age and treatment condition (EWA versus TAU) a relevant factor in the analyses. Age can also act as an indirect predictor of mortality because it may correlate with other factors relevant for mortality. For example, older individuals may be less drug dependent at baseline than younger individuals and they may also show longer retention in treatment and thereby are less likely to have close family or friends who encourage alcohol use (Satre et al., 2004); such factors could potentially moderate some of the direct effects of age on mortality.
The primary research question was whether the same specific subgroup of women involved in the 2-year RCT, who received the EWA treatment programme, showed reduced mortality risk over time compared with the women who were randomized to TAU (Dahlgren and Willander, 1989a,b). We expected the most marked differences early in the follow-up period and among the younger women.
The secondary research question was whether mortality differences between EWA and TAU were related to the need for inpatient treatment. This is important because inpatient treatment indicates a more serious alcohol problem. A third question was whether women who dropped out of the follow-up study lived as long as those who complied with the follow-up procedure. The mortality register gives a unique opportunity to explore this topic. These analyses can reveal if subjects who drop out are similar to compliant subjects (McKnight et al., 2007; Schafer and Graham, 2002). If such differences are found, this could indicate an over or underestimation of the earlier documented treatment outcome effect (Dahlgren and Willander, 1989a). The fourth research topic was to explore the relationship between short-term drinking outcome and mortality.
MATERIALS AND METHODS
Background
The programme ‘Early treatment for Women with Alcohol Addiction’ was developed in Sweden during the 1980s to improve existing treatment and to reach women early in their addiction career by facilitating treatment entry and making treatment attractive and effective (Dahlgren and Willander, 1989a; Haver and Franck, 1997). The need for a programme that targeted women was made clear by the observations of a general increase in alcohol consumption among women and the poorer treatment results and higher mortality among women alcoholics coming for treatment compared with that of men found in earlier studies (Dahlgren, 1979). The lack of treatment programmes aimed at this specific group of women called for the development of a more complex and adjusted intervention programme (Dahlgren, 1979; Dahlgren and Willander, 1989a; Haver, 2003; Haver and Franck, 1997; Haver et al., 2001). It was assumed that women would benefit from more focus on psychiatric symptoms that complicate the alcohol problem and their relationship with their partner who also frequently had a drinking problem. In addition, the programme addressed their children's needs, the women's work and their social situations (Dahlgren, 1989).
The EWA treatment
The EWA treatment was conducted at the EWA unit, located at Magnus Huss Clinic, at the Karolinska Hospital. The EWA unit was better staffed in general, specifically with more doctors and psychologists, than the units where TAU was delivered. Individualized treatment consisted of detoxification, inpatient treatment when necessary, psychotropic drugs and disulfiram (Antabus) according to initial evaluation, individual and women-only group therapy two or three times a week, regular contact with primarily one of the staff at the hospital for up to 2 years after initial evaluation, work training and physiotherapy. The programme also focused on the woman in her context: family situations and child issues were approached in co-operation with a child psychiatrist. The women's partner was invited to participate in the treatment. Abstinence was the ultimate goal of treatment, though social drinking was considered as an option when abstinence was not possible (Haver and Franck, 1997).
TAU interventions included regular contact with nursing staff and medication administration—first and foremost disulfiram—after detoxification in inpatient or outpatient care. The TAU treatment took place in the regular wards at the same alcoholism treatment centre (Magnus Huss Clinic) or a nearby outpatient clinic. TAU women were given the same comprehensive evaluation of drinking patterns, somatic and mental health status and work and social status at intake. This description of the TAU treatment condition relies upon the original papers (Dahlgren and Willander, 1989a,b) and interviews with two staff members who worked at the ward during the planning phase of this study. The treatment lasted on average 8 months for the EWA women and 5 months for the TAU women (median, P < 0.01), and 36% of the EWA group and 21% of the TAU group continued for 12 months or more (P < 0.05; Dahlgren and Willander, 1989a).
Sample
Two hundred women not previously treated for AUD were consecutively recruited to an RCT during 1983–1984. Women with odd dates of birth were assigned to the EWA programme (n = 100), and women with even dates of birth to a mixed gender setting with no programme specifically developed for women, here called TAU (n = 100). Signs of chronic alcoholism (liver cirrhosis, dementia), previous treatment for alcohol problems, psychotic syndromes and use of narcotic drugs were regarded as exclusion criteria in both treatment groups. Information regarding how many women refused randomization is not available. However, the groups did not differ on important clinical data relevant for outcome. The EWA and TAU women were compared by more than 200 medical and social variables. Three statistically significant differences were found: more EWA than TAU women lived with a male partner and more EWA women reported signs of more advanced alcohol problems. This number of statistically significant differences may be as expected (Dahlgren and Willander, 1989a). In addition, the authors were uncertain about the advantage of these differences regarding the treatment outcome. The mean age at intake to treatment was 42.4 years (SD 9.82) for both groups. The study was approved by the Stockholm Regional Ethical Review Board and the Swedish Data Inspection Board.
Attrition
In this study, 25 EWA women and 32 TAU women dropped out at the 2-year personal follow-up, which left a sample of 75 and 68 women, respectively. Reasons for dropout were refusal to participate because the interview would revive unpleasant memories or because the interview would make a new partner who did not know of their earlier problems aware of their past. Furthermore, some had acquired an unregistered address and telephone number, which prevented the research team from locating them. Analyses showed that EWA women with missing observations at follow-up had somewhat higher wine consumption, but lower liquor consumption, at baseline than EWA women with observations at follow-up. No such differences in drinking pattern were found for TAU women. However, TAU women with missing observation at follow-up consumed less psychotropic medication at baseline than TAU women who contributed at both measurement points. The analyses show whether data are ‘missing at random’, but not if data are ‘missing not at random’ (McKnight et al., 2007; Schafer and Graham, 2002). Register data were available for all women, giving a unique opportunity to analyse dropout status versus mortality.
Measures
The variables used in the analyses were age at intake to treatment (continuous variables), inpatient versus outpatient treatment (inpatient treatment needed: 38 of 77 EWA and 25 of 83 TAU women, 40 subjects had missing data in this variable), 2-year treatment outcome and follow-up attrition. Since very few women in our study reported total abstinence during the initial 2-year follow-up period, this factor could not work as a predictor of mortality. Social drinking was defined as drinking in the company of others, drinking limited to a pre-decided quantity, absence of craving, no drinking the following day and consuming <30 g of pure ethanol (about half a bottle of table wine) in 24 h. Drinking patterns not in accordance with the above definition were labelled relapse drinking.
Statistical analysis
Statistical analyses were descriptive statistics, cross tabulation and survival models (Kaplan–Meier, Cox regression). With such a long follow-up period, a simple cross tabulation between group membership and mortality status would most likely not give statistically significant results. This is not primarily related to lack of statistical power, but to the use of analysis that does not take time until death into account. Differences between the groups manifest early in the follow-up period can be expected to even out over time due to more deaths later on in the group with lower mortality—all will die eventually. Nevertheless, the two groups may be very different regarding years of survival. This problem is handled by using statistical analyses that incorporate information about time until death and allow for variance in group differences over time. Thus, the proportional hazard assumption underlying ordinary Cox regression will probably not hold for the 27-year observation period (Schemper, 1992). Cox regression log-minus-log plots and Kaplan–Meier plots for the two groups showed unparallel lines, which indicated that ordinary Cox regression is problematic. Therefore, the factors were entered as time-dependent covariates to allow non-proportional hazards over time. Finding factors to be time-dependent represents additional evidence against the proportional hazard assumption. Thus, estimated hazard ratios (HR) based on a model with both time-independent and time-dependent covariates are presented (Bellera et al., 2010). These results revealed a more limited time interval for further ordinary Cox regression analysis.
All mortality analyses controlled for age and incorporated age and treatment condition interaction. The variable Age was used as a continuous variable in all analyses and was never categorized into age subgroups. To present the interaction effect between treatment and age found in the multivariate Cox regression analyses, survival plots were generated at three arbitrary age levels; here they are presented as plots for women being 30, 40 and 50-years old. Such prediction of outcome values represents standard regression procedure. Re-analysing this interaction model with centred variables or with a residualized interaction term would reduce multi-colinearity between the main predictors and the interaction predictor, but would not change the interpretation of the results (Wu and Zumbo, 2008). In contrast to analyses with the age variable in its original form, a statistically significant effect of age was found when centred variables were used. However, as long as the interaction effect is found to be statistically significant, this shows that the group difference is dependent on the age level (Pedhazur and Schmelkin, 1991). In our study, this was confirmed by identical survival profiles for the different statistical models.
RESULTS
The overall mortality for the total follow-up period of 27 years in the EWA group was 38% and 45% in the TAU group, a difference that is not statistically significant (χ2 = 1.00; P = 0.32). Cox regression with time-dependent covariates showed statistically significant differences in mortality between the two intervention groups, depending on age and time since intake to treatment. Table 1 shows all variables except the main effect of age to be statistically significant.
Table 1.
Cox regression with treatment condition (EWA and TAU), age at intake, interaction effect between age and treatment condition and time interaction covariates for the 27-year follow-up period
| Variable | B | Exp(B) | 95% CI lower | 95% CI upper | P-value |
|---|---|---|---|---|---|
| Treatment (EWA/TAU) | −6.51 | 0.00 | 0.00 | 0.37 | 0.020 |
| Age at intake | −0.02 | 0.98 | 0.92 | 1.04 | 0.495 |
| Age at intake × Treatment | 0.13 | 1.14 | 1.14 | 1.27 | 0.030 |
| Treatment × Time | 0.35 | 1.42 | 1.42 | 1.95 | 0.032 |
| Age at intake × Time | 0.00 | 1.00 | 1.00 | 1.01 | 0.039 |
| Age at intake × Treatment × Time | −0.01 | 0.99 | 0.99 | 1.00 | 0.043 |
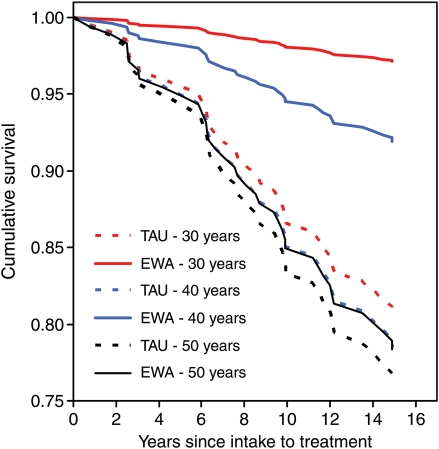
On the basis of these results, Fig. 1 illustrates time-dependent hazard ratios—HR(t). The plot shows equal and increasing HRs developing over time for women who are 50-year old. Differences in mortality were found in favour of the EWA programme for younger women (here shown as predicted estimates for women who are 30-year old) and for extended parts of the observation period. This difference lasted up to 15 years, but levelled out over time, so that no difference existed ∼20 years after intake to treatment.
Fig. 1.
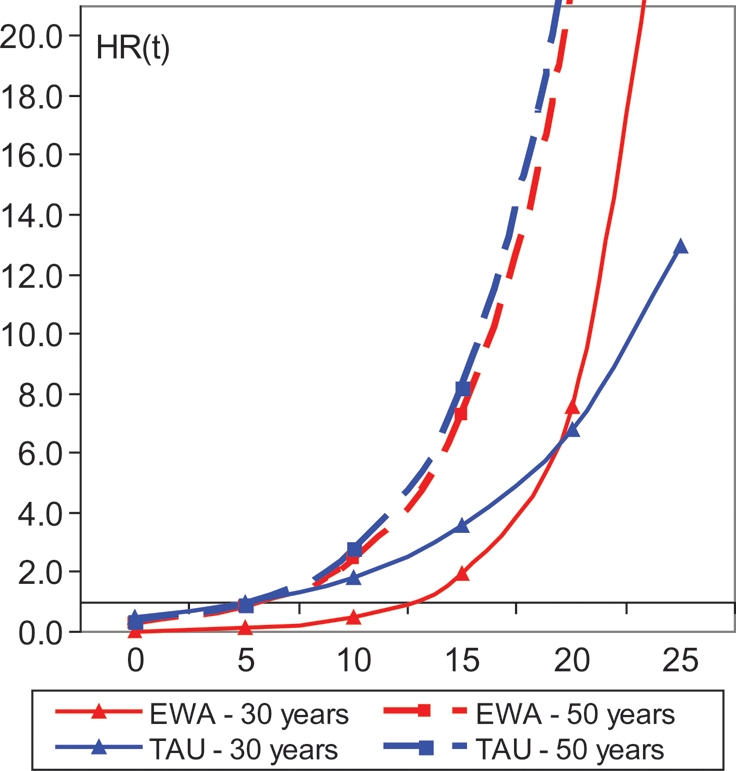
Hazard ratio over time [HR(t)] based on Cox regression with time-dependent covariates (HR(t) = e(−6.51 Group−0.02 Age + 0.13 Group × Age + 0.35 Group × Time + 0.00 Age × Time − 0.01 Age × Group × Time)). Age was treated as a continuous variable. The plot is based on pre-specified values for treatment group condition and age (30 and 50 years), and the interaction between treatment condition and age.
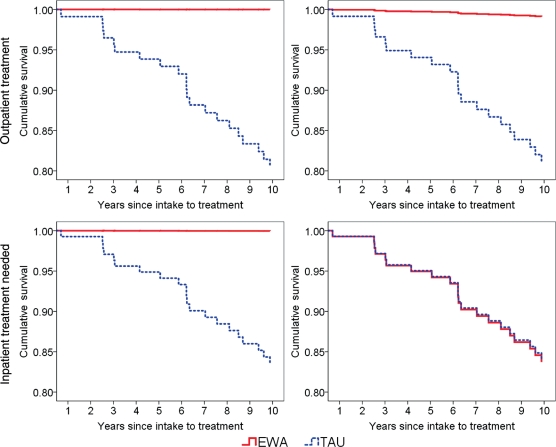
Since differences in mortality were shown for younger women up to and slightly above 15 years after intake, a standard proportional hazard model was analysed for this period to simplify the model. The results confirmed statistically significant effects of treatment condition (EWA versus TAU) and the interaction between treatment condition and age [Age at intake: Exp(B) = 1.01; P = 0.58; Group effect: Exp(B) = 0.01; P = 0.01; Group × Age: Exp(B) = 1.10; P = 0.02]. Survival plots showed that mortality group differences were strongest among younger women, while no difference in survival was found if the women were ∼51-years old as shown in Fig. 2.
Fig. 2.
Survival plots for 15-year follow-up after intake to treatment for two treatment conditions (EWA and TAU) at three different age levels (Cox regression model estimates). Age was treated as a continuous variable.
No differences between the two treatment conditions were found for inpatients versus outpatients over the first 15 years of observation. A further restriction of the follow-up interval to 10 years revealed statistically significant interaction effects of both age and outpatient versus inpatient status with treatment condition [EWA and TAU; Age × Treatment Condition: Exp(B) = 1.36; P = 0.007; Treatment condition × Inpatient versus Outpatient status: Exp(B) = 23.96; P = 0.025]. In addition, the main effect of treatment condition was statistically significant [Exp(B) = 0.00; P = 0.006]. Fig. 3 shows survival plots for the treatment condition, dependent on inpatient versus outpatient status, and age at intake, with two age levels to facilitate the illustration. This figure illustrates the reduced mortality risk among younger EWA women, both in outpatient and inpatient settings, and among middle-aged EWA women who received outpatient treatment only.
Fig. 3.
Survival plots for 10-year follow-up after intake to treatment for two treatment conditions (EWA and TAU) at two age levels, separated by inpatient versus outpatient status at intake (Cox regression model estimates). Age was treated as a continuous variable.
In the TAU group, Kaplan–Meier analyses showed higher mortality for women (n = 32) who did not complete the 2-year follow-up compared with those who did (n = 68; Generalized Wilcoxon χ2 = 14.46; P = 0.000), with estimated mean survival 16.74 and 23.52, respectively. No such survival difference was found among EWA women non-completers versus completers (n = 25 of 75; 22.64 and 21.84 years, respectively, χ2 = 0.06; P = 0.81).
A social drinking pattern during 1 or 2 years after intake was obtained by almost half the EWA group (47.9%), while the frequency in the TAU group was only 19.1%, a statistically significant difference (χ2 = 13.03; P = 0.000). However, we did not find statistically significant relationships between social drinking outcome and mortality for the total group of women who completed the 2-year follow-up (n = 143; χ2 = .076; P = 0.38). For those women who did not attain a social drinking pattern, we nevertheless found that the EWA women had lower mortality [Age at intake: Exp(B) = 0.97; P = 0.396; Group effect: Exp(B) = 0.00; P = 0.000; Group × Age: Exp(B) = 1.56; P = 0.002].
DISCUSSION
Reduced mortality was found in the EWA group compared with the TAU group, with a stronger difference between younger women in the two groups and with the greatest difference in the initial period of the total 27-year follow-up time. This difference was reduced to zero ∼20 years after intake to treatment. Since the two samples were found to be equal concerning important clinical data relevant for outcome (Dahlgren and Willander, 1989a), this finding supports the interpretation that the EWA treatment programme was more effective than the TAU programme. Few treatment programmes for female alcoholics have been tested within a long-term follow-up design, and none to our knowledge with a randomized controlled design (Greenfield et al., 2007a, b). The present study thereby represents unique data on comparative effectiveness of the two types of interventions. Since mortality is a common prognostic and treatment outcome variable for disorders, improved survival for the younger women up to ∼20 years after the start of treatment is an important finding.
This finding could be attributed to the fact that the EWA intervention programme focused on several risk factors for premature death, such as premature treatment closure (Berglund et al., 2003; Costello, 2006), level of alcohol consumption, binge drinking and severity of alcohol dependence symptoms (Timko et al., 2006). The EWA programme also focused on medical problems, history and presence of mental health problems, coping strategies and relapse prevention and interpersonal stressors such as work-related problems and living with a partner who is a heavy drinker. These and other factors, like co-habitant status, socio-demographic status and unemployment, are found to be related to mortality in the general population and also among female alcoholics (Feuerlein et al., 1994; Greenfield et al., 2002, 2007a; Lantz et al., 1998; Mann et al., 2004; Masudomi et al., 2004; Satre et al., 2004; Schneider et al., 1995; Timko et al., 2006). We believe that longer treatment duration, more stable contact with treatment staff, targeting premature treatment attrition, focus on medical and psychiatric problems and the improved short-term outcome are important factors for the long-term results regarding mortality among EWA women. Accepting the individual woman's drinking goal—without pushing total abstinence as the one and only acceptable outcome—might have enhanced treatment compliance, and thereby duration of treatment. On the other hand, the TAU treatment only included supportive counselling in combination with social interventions, and sometimes also medication. Specific interventions targeting psychiatric co-morbidity were not generally available outside the EWA programme at that time, and this aspect of treatment was later shown to be important for the outcome (Berglund et al., 2003; Greenfield et al., 2007a; Schneider et al., 1995). In sum, the EWA treatment programme was more comprehensive and intensive than the TAU treatment and this difference was important for survival.
Treatment seeking and compliance were facilitated by attending a woman-only programme (Haver and Franck, 1997); however, the impact of this aspect of treatment setting on the outcome cannot be measured using the present design; nevertheless, it is noteworthy that EWA women reported that meeting other women with drinking problems was the most important factor related to positive change (Swedenhammar and Franck, 1995). Another interesting finding from the original follow-up study is that TAU women more often changed partners during the first 2 years after intake to treatment, which might be a result of easier access to men with drinking problems. This aspect of mixed gender programmes has previously been related to a poorer outcome for women alcoholics (Greenfield et al., 2002).
The main effect of age over the total observation period was not statistically significant in several analyses; however, this is of no importance as long as the interaction between age and treatment condition was found to be statistically significant (Pedhazur and Schmelkin, 1991). As expected, this interaction effect showed that the women's age was a relevant mortality predictor (Satre et al., 2004; Timko et al., 2006), but to a different degree for the two groups. Of particular importance is that the EWA programme improved survival among younger women, since more years lost to life were thereby saved. Because mortality differences will level out over time, we used survival analysis with time-dependent covariates to analyse differences between the two treatment conditions. Otherwise, the long-observation period would have concealed important group differences (Cuijpers et al., 2004; Schemper, 1992). This procedure also tests the presence of the proportional hazard assumption, which is not often verified in research (Bellera et al., 2010), thereby revealing the important results reported above.
Another finding was related to inpatient versus outpatient status at intake. Even when initial inpatient treatment was used, a positive effect of the EWA intervention was found. In general, the need for inpatient treatment is assumed to reflect problem severity among female alcoholics (James, 2005; Timko et al., 2006). In the EWA study, missing data, different practices and availability of inpatient beds between the EWA and TAU programme make the interpretation of these results uncertain. For patients who received outpatient treatment only, a lower mortality risk was observed both among younger and older EWA women, which shows that the EWA programme also worked for older women.
Regarding attrition, we found some interesting survival differences between women who attended the 2-year follow-up versus those who did not. In the TAU group, women who dropped out of the study had a higher mortality compared with those who participated at follow-up. This indicates that TAU women dropping out of the study were less well functioning during the observation period. Also, these findings indicate different attrition mechanisms in the two groups. We cannot explain this difference because there is no data for the 2-year follow-up for women who dropped out of the study. Several factors may be involved: alcohol relapses, reduced social support systems, meeting new heavy-drinking partners and ineffective coping strategies. No such mortality difference was found among the EWA women. Thus, follow-up attrition was probably ‘not random’ in the TAU group as opposed to the EWA group. In spite of the increasing focus on missing data theory and methodology, it is still not often implemented in research beyond reporting missing percentages and correlations between missingness and variables in the study (McKnight et al., 2007; Schafer and Graham, 2002). Clearly, missing data have implications for representativeness and generalizations of the 2-year outcome results. The present results reveal that the findings reported from the original 2-year follow-up study probably represent an underestimation of the actual initial outcome differences between the EWA and the TAU samples (Dahlgren and Willander, 1989a).
The importance of drinking outcome for overall mortality has been addressed by several authors (Barr et al., 1984; Feuerlein et al., 1994; Gerdner and Berglund, 1997; Smith et al., 1994; Taylor, 1994; Timko et al., 2006). In the present study, relapse drinking during the first 2 years after the start of treatment did not affect mortality for either the EWA or TAU group. This could mean that the initial drinking patterns reported are unreliable (Dahlgren and Willander, 1989a). Alternatively, changing drinking patterns during long-term follow-up is an expected outcome, which makes the initial drinking outcome an unstable predictor of long-term mortality. In addition, no difference regarding mortality was found for women who managed to achieve a socially acceptable drinking pattern. For those women who did not attain a social drinking pattern, we nevertheless found that the EWA programme positively affected mortality. However, these findings are uncertain due to the reported different attrition mechanisms at the 2-year's follow-up.
CONCLUSIONS
These results suggest that a woman-only programme specifically developed to meet a broad spectrum of problems among women with AUDs could have a major impact on the lives of these women. The EWA programme had a significant effect on mortality over a time period up to 15–20 years after intake to treatment, especially among younger women, compared with women who participated in a mixed gender ‘Treatment-As-Usual’ programme.
Funding
The project was funded by the Norwegian Research Foundation (NFR), The Swedish Research Council (grant 14645) and the Alcohol Research Council of the Swedish Retail Monopoly.
REFERENCES
- Barr HL, Antes D, Ottenberg DJ, et al. Mortality of treated alcoholics and drug addicts: the benefits of abstinence. J Stud Alcohol. 1984;45:440–52. doi: 10.15288/jsa.1984.45.440. [DOI] [PubMed] [Google Scholar]
- Bellera CAC, MacGrogan GG, Debled MM, et al. Variables with time-varying effects and the Cox model: some statistical concepts illustrated with a prognostic factor study in breast cancer. BMC Med Res Methodol. 2010;10:20. doi: 10.1186/1471-2288-10-20. doi:10.1186/1471-2288-10-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berglund M. Mortality in alcoholics related to clinical state at first admission. A study of 537 deaths. Acta Psychiatr Scand. 1984;70:407–16. doi: 10.1111/j.1600-0447.1984.tb01228.x. doi:10.1111/j.1600-0447.1984.tb01228.x. [DOI] [PubMed] [Google Scholar]
- Berglund M, Thelander S, Salaspuro M, et al. Treatment of alcohol abuse: an evidence-based review. Alcohol Clin Exp Res. 2003;27:1645–56. doi: 10.1097/01.ALC.0000090144.99832.19. doi:10.1097/01.ALC.0000090144.99832.19. [DOI] [PubMed] [Google Scholar]
- Cipriani F, Landucci S, Bloomfield K. Alcohol-related mortality in Europe: a tentative analysis from the EU Project “alcohol consumption and alcohol problems among women in European countries”. Subst Abuse. 2001;22:55–67. doi: 10.1080/08897070109511445. [DOI] [PubMed] [Google Scholar]
- Costello RM. Long-term mortality from alcoholism: a descriptive analysis. J Stud Alcohol. 2006;67:694–9. doi: 10.15288/jsa.2006.67.694. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Riper H, Lemmers L. The effects on mortality of brief interventions for problem drinking: a meta-analysis. Addiction. 2004;99:839–45. doi: 10.1111/j.1360-0443.2004.00778.x. doi:10.1111/j.1360-0443.2004.00778.x. [DOI] [PubMed] [Google Scholar]
- Dahlgren L. Female Alcoholics. A psychiatric and Social Study. Stockholm: Karolinska Institute; 1979. [Google Scholar]
- Dahlgren L. Alcoholism in women: hidden abuse. Nord Med. 1989;104:212–3. [PubMed] [Google Scholar]
- Dahlgren L, Myrhed M. Alcoholic females. II. Causes of death with reference to sex difference. Acta psychiatr Scand. 1977;56:81–91. doi: 10.1111/j.1600-0447.1977.tb06668.x. doi:10.1111/j.1600-0447.1977.tb06668.x. [DOI] [PubMed] [Google Scholar]
- Dahlgren L, Willander A. Are special treatment facilities for female alcoholics needed? A controlled 2-year follow-up study from a specialized female unit (EWA) versus a mixed male/female treatment facility. Alcohol Clin Exp Res. 1989a;13:499–504. doi: 10.1111/j.1530-0277.1989.tb00366.x. doi:10.1111/j.1530-0277.1989.tb00366.x. [DOI] [PubMed] [Google Scholar]
- Dahlgren L, Willander A. Hög dödlighet bland kvinnor utan behandling för alkoholproblem [A study of abusers at the EWA unit: women not treated for their alcohol problems have an increased mortality rate] Läkartidningen. 1989b;86:1898–900. [PubMed] [Google Scholar]
- Feuerlein W, Küfner H, Flohrschütz T. Mortality in alcoholic patients given inpatient treatment. Addiction. 1994;89:841–9. doi: 10.1111/j.1360-0443.1994.tb00987.x. doi:10.1111/j.1360-0443.1994.tb00987.x. [DOI] [PubMed] [Google Scholar]
- Gerdner A, Berglund M. Mortality of treated alcoholics after eight years in relation to short-term outcome. Alcohol Alcohol. 1997;32:573–9. doi: 10.1093/oxfordjournals.alcalc.a008298. [DOI] [PubMed] [Google Scholar]
- Greenfield TK, Rehm J, Rogers JD. Effects of depression and social integration on the relationship between alcohol consumption and all-cause mortality. Addiction. 2002;97:29–38. doi: 10.1046/j.1360-0443.2002.00065.x. doi:10.1046/j.1360-0443.2002.00065.x. [DOI] [PubMed] [Google Scholar]
- Greenfield SF, Brooks AJ, Gordon SM, et al. Substance abuse treatment entry, retention, and outcome in women: a review of the literature. Drug Alcohol Depend. 2007a;86:1–21. doi: 10.1016/j.drugalcdep.2006.05.012. doi:10.1016/j.drugalcdep.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield SF, Trucco EM, McHugh RK, et al. The women's recovery group study: a Stage I trial of women-focused group therapy for substance use disorders versus mixed-gender group drug counseling. Drug Alcohol Depend. 2007b;90:39–47. doi: 10.1016/j.drugalcdep.2007.02.009. doi:10.1016/j.drugalcdep.2007.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haver B. Comorbid psychiatric disorders predict and influence treatment outcome in female alcoholics. Eur Addict Res. 2003;9:39–44. doi: 10.1159/000067735. doi:10.1159/000067735. [DOI] [PubMed] [Google Scholar]
- Haver B, Franck J. The Karolinska Project for Early Treatment of Women with Alcohol Addiction. A review of a unique research program. Eur Addict Res. 1997;3:30–6. doi:10.1159/000259144. [Google Scholar]
- Haver B, Dahlgren L, Willander A. A 2-year follow-up of 120 Swedish female alcoholics treated early in their drinking career: prediction of drinking outcome. Alcohol Clin Exp Res. 2001;25:1586–93. doi:10.1111/j.1530-0277.2001.tb02165.x. [PubMed] [Google Scholar]
- Haver B, Gjestad R, Lindberg S, et al. Mortality risk up to 25 years after initiation of treatment among 420 Swedish women with alcohol addiction. Addiction. 2009;104:413–9. doi: 10.1111/j.1360-0443.2008.02479.x. doi:10.1111/j.1360-0443.2008.02479.x. [DOI] [PubMed] [Google Scholar]
- James RM. Is there a case for extended interventions for alcohol and drug use disorders? Addiction. 2005;100:1594–610. doi: 10.1111/j.1360-0443.2005.01208.x. doi:10.1111/j.1360-0443.2005.01208.x. [DOI] [PubMed] [Google Scholar]
- Lantz PM, Hous JS, Lepkowsk JM, et al. Socioeconomic factors, health behaviors, and mortality: results from a nationally representative prospective study of US adults. JAMA. 1998;279:1703–8. doi: 10.1001/jama.279.21.1703. doi:10.1001/jama.279.21.1703. [DOI] [PubMed] [Google Scholar]
- Lindberg S, Ågren G. Mortality among male and female hospitalized alcoholics in stockholm 1962–1983. Addiction. 1988;83:1193–200. doi: 10.1111/j.1360-0443.1988.tb03026.x. doi:10.1111/j.1360-0443.1988.tb03026.x. [DOI] [PubMed] [Google Scholar]
- Mann K, Hintz T, Jung M. Does psychiatric comorbidity in alcohol-dependent patients affect treatment outcome? Eur Arch Psychiatry Clin Neurosci. 2004;254:172–81. doi: 10.1007/s00406-004-0465-6. [DOI] [PubMed] [Google Scholar]
- Masudomi I, Isse K, Uchiyama M, et al. Self-help groups reduce mortality risk: a 5-year follow-up study of alcoholics in the Tokyo metropolitan area. Psychiatry Clin Neurosci. 2004;58:551–7. doi: 10.1111/j.1440-1819.2004.01299.x. doi:10.1111/j.1440-1819.2004.01299.x. [DOI] [PubMed] [Google Scholar]
- McKnight PE, McKnight KM, Sidani S, et al. Missing Data: A Gentle Introduction. New York: Guilford Press; 2007. [Google Scholar]
- Pedhazur EJ, Schmelkin LP. Measurement, Design, and Analysis: An Integrated Approach. Hillsdale, NJ: Lawrence Erlbaum Associates; 1991. [Google Scholar]
- Satre DD, Mertens JR, Areán PA, et al. Five-year alcohol and drug treatment outcomes of older adults versus middle-aged and younger adults in a managed care program. Addiction. 2004;99:1286–97. doi: 10.1111/j.1360-0443.2004.00831.x. doi:10.1111/j.1360-0443.2004.00831.x. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychol Methods. 2002;7:147–77. doi:10.1037/1082-989X.7.2.147. [PubMed] [Google Scholar]
- Schemper M. Cox analysis of survival data with non-proportional hazard functions. Statistician. 1992;41:455–65. [Google Scholar]
- Schneider KM, Kviz FJ, Isola ML, et al. Evaluating multiple outcomes and gender differences in alcoholism treatment. Addict Behav. 1995;20:1–21. doi: 10.1016/0306-4603(94)00037-y. doi:10.1016/0306-4603(94)00037-Y. [DOI] [PubMed] [Google Scholar]
- Smith EM, Cloninger CR, Bradford S. Predictors of mortality in alcoholic women: prospective follow-up study. Alcohol Clin Exp Res. 1983;7:237–43. doi: 10.1111/j.1530-0277.1983.tb05449.x. doi:10.1111/j.1530-0277.1983.tb05449.x. [DOI] [PubMed] [Google Scholar]
- Smith EM, Lewis CE, Kercher C, et al. Predictors of mortality in alcoholic women: a 20-year follow-up study. Alcohol Clin Exp Res. 1994;18:1177–86. doi: 10.1111/j.1530-0277.1994.tb00101.x. doi:10.1111/j.1530-0277.1994.tb00101.x. [DOI] [PubMed] [Google Scholar]
- Swedenhammar R, Franck J. Så ser missbrukaren på sin egen behandling. Läkartidningen. 1995;92:1593–6. [PubMed] [Google Scholar]
- Taylor C. What happens over the long-term? Br Med Bull. 1994;50:50–66. doi: 10.1093/oxfordjournals.bmb.a072884. [DOI] [PubMed] [Google Scholar]
- Timko C, DeBenedetti A, Moos BS, et al. Predictors of 16-year mortality among individuals initiating help-seeking for an alcoholic use disorder. Alcohol Clin Exp Res. 2006;30:1711–20. doi: 10.1111/j.1530-0277.2006.00206.x. doi:10.1111/j.1530-0277.2006.00206.x. [DOI] [PubMed] [Google Scholar]
- Wu A, Zumbo B. Understanding and using mediators and moderators. Soc Indic Res. 2008;87:367–92. doi:10.1007/s11205-007-9143-1. [Google Scholar]
- Yoshino A, Kato M, Yoshimasu H, et al. Which relapse criteria best predict the mortality risk of treated alcoholics? Alcohol Clin Exp Res. 1997;21:1374–8. [PubMed] [Google Scholar]